Abstract
Although total confinement has not been adopted by the government of Cameroon, the COVID-19 pandemic is keeping geriatric patients out of hospital, despite a decline in their health status. In addition, the pandemic might have a significant effect on their general well-being. This study aimed to examine the effects of the COVID-19 pandemic on the follow-up and well-being of older outpatients seen at geriatric consultation in Cameroon. We carried out a telephone survey of patients who did not attend an appointment at our geriatrics outpatient clinic on April 2020. Overall, 30 participants were recruited of whom 70% were female (n = 21) with a median age of 74 years (IQR 68.8–85). Most patients (73%, n = 22) did not attend their appointment because of fear of being infected by SARS-CoV-2 at hospital. Approximately 23% (n = 7) of participants reported a decline of their functional status since the last geriatric visit. Loss of appetite and weight loss were both reported in 30% (n = 9) of patients. Half of participants (n = 15) self-rated their health status as bad and three of them died in private health facilities. Strategies to ensure a continuum of care for this vulnerable population during this pandemic are highly needed in our setting.
Keywords: COVID-19, older adults, outpatients, effects
Introduction
The outbreak of COVID-19 has turned into a pandemic since the World Health Organization (WHO) statement on March 11, 2020. It has spread rapidly throughout the world, and according to WHO, the global mortality rate is around 3.4% (Archived: WHO Timeline-COVID-19, 2020; Coronavirus mortality rate, 2020). Many countries have therefore adopted total confinement as a major response to the pandemic, in addition to other barrier measures.
Since the first case detected in Cameroon a country in Central Africa, on March 6, the government has chosen not to apply a total confinement of the population. The authorities adopted barrier measures to limit the spread of virus including closure of international borders and educational facilities, hygiene measures, social distancing as well as compulsory mask wearing in public spaces. Despite these measures, Cameroon is currently one of the most affected countries in Africa with 15,173 confirmed cases and 359 deaths as of July 12, 2020 (COVID-19 Coronavirus pandemic, 2020).
As this health crisis impacts our country, no restrictions on movement were introduced in the government’s response to COVID-19 mainly for economic reasons. Thus, while planning interventions to fight against COVID-19, health facilities in Cameroon had to maintain usual medical activities to address the needs of all patients, SARS-Cov-2 positive or not, during the pandemic. As a result, outpatients clinics, elective surgical interventions and other non-urgent procedures have been maintained in most healthcare facilities.
Despite these efforts to provide almost normal service in the hospital, we have noticed a significant decrease in geriatric consultations at the Yaounde Central Hospital. In fact, most patients expected in routine consultation did not attend their appointments. Furthermore, we have not recorded any new geriatric consultations since March 19, 2020. Hence, this study aimed to examine the effects of the COVID-19 pandemic on the follow-up and well-being of geriatrics outpatients seen at the Yaounde Central Hospital.
Methods
Study Setting, Design, and Participants
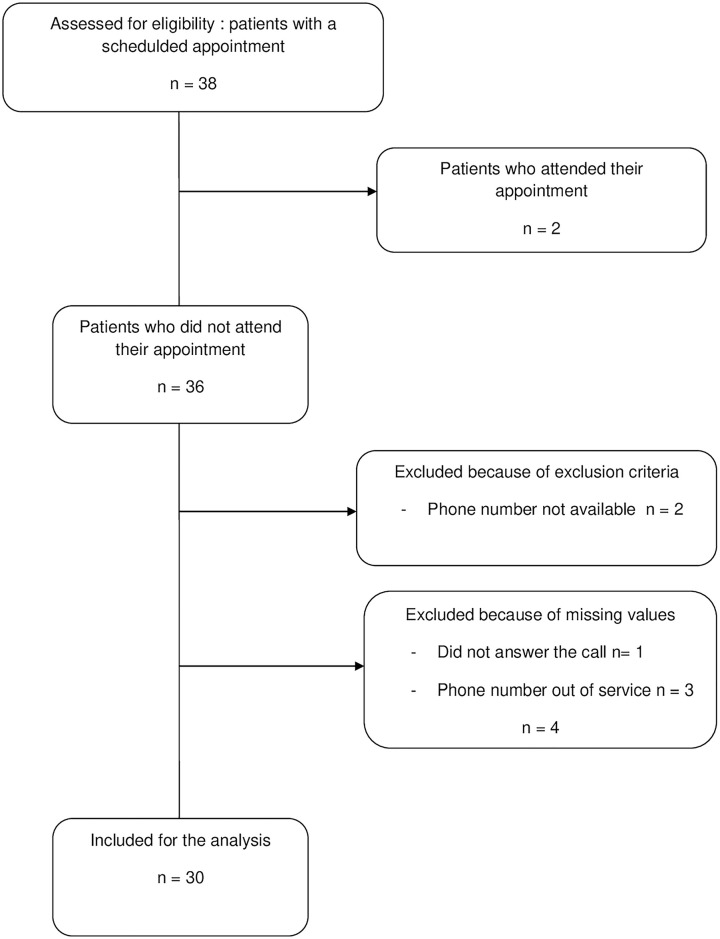
This retrospective study was carried out in May 2020, at the geriatric unit of the Yaounde Central Hospital. This 650-bedded hospital is located in the capital of Cameroon and has the lone Geriatrics-dedicated unit in Cameroon. On 2019, 202 patients have been hospitalized in the Geriatric unit and 339 have consulted at the outpatients clinic. Participants were recruited on the basis of the consultation logbook. We conducted a telephone survey with all the patients aged 65 and over who had an appointment between the 1st and the 30th April, who provided a phone number and who did not attend their visit with the geriatrician (Figure 1). The interview consisted on brief interviews of 10 min with closed-ended questions and was conducted with the patient or a family member in case of inability for the patient to communicate. A verbal consent was obtained from the patient or his family member if the former was not able to communicate.
Figure 1.
Patients flow diagram.
Data Collection
Data collected in the consultation logbook included age and gender, baseline functional status, and comorbidities such as hypertension, diabetes mellitus, cerebrovascular disease, dementia, cancer, heart failure, human immunodeficiency virus (HIV), hepatitis B and C infections. We collected information given during the interviews: main reasons for non consultation, self-rated health status, functional status, self-rated loss of appetite and weight loss. Functional status was assessed by the Katz Index of Independence in Activities of Daily Living (ADL). The Katz Index of independence in ADL is widely used to assess the older patient ability to perform basic activities of daily living by measuring six functions: bathing, dressing, toileting, transferring, continence, and feeding (Katz, 1983). Health status was assessed by self-rating it as “bad” or “good.”
Data Analysis
Data were coded, entered and analyzed with the Statistical Package for Social Sciences (SPSS 23.0) for Windows (SPSS, Chicago, Illinois, USA). Quantitative variables are described using section median and interquartile range (IQR) and categorical variables with frequencies and proportions.
Results
Thirty-eight patients had a scheduled appointment at our geriatric outpatient clinic and 36 (94.7%) dropped out consultation. Thirty (83.3%) patients responded to the interview (Figure 1).
Characteristics of Participants
Overall, 30 participants were recruited for the study of whom 70% were female (n = 21). Fourteen patients (46.6%) responded themselves to the interview. The median age of participants was 74 (IQR 68.8–85), with 40% (n = 12) aged ≥80 years. More than 90% (n = 27) of patients had at least one chronic medical condition, the commonest being hypertension (86.7%, n = 26), diabetes mellitus (23.3%, n = 7), cerebrovascular disease (16.7%, n = 5), dementia (13.3%, n = 4), and hepatitis C (13.3%, n = 4).
Effects of COVID-19 on Older Outpatients Follow-Up and Well-Being
As presented in Table 1, most patients (73.3%, n = 22) did not attend their appointment because of fear of being infected by SARS-CoV-2 at the hospital. Other reasons for non consultation were reported: absence of complaints in 50% (n = 15) and financial issues in 26% (n = 8). Thirteen participants (43%) reported they had not gone out of home since the beginning of pandemic but none declared being isolated at home. On the other hand, about 57% (n = 17) of patients reported that they had continued going out of their home for purposes other than attending their medical appointments; about half of them (n = 7) did not always wear a mask.
Table 1.
Characteristics of Participants, Reasons for Non Consultation and Effects on Well-Being.
| Variables | Women n = 21 (70%) | Men n = 9 (30%) | All participants n = 30 (100%) |
|---|---|---|---|
| Age groups | |||
| 65–69 | 5 (23.8) | 3 (33.3) | 8 (26.7) |
| 70–74 | 6 (28.6) | 2 (22.2) | 8 (26.7) |
| 75–79 | 2 (9.5) | 0 (0) | 2 (6.6) |
| 80+ | 8 (38.1) | 4 (44.4) | 12 (40) |
| Respondent | |||
| Patient | 10 (47.6) | 4 (44.4) | 14 (46.7) |
| Family member | 11 (52.4) | 5 (55.6) | 16 (53.3) |
| Reasons for non consultation | |||
| Fear of contracting COVID-19 in hospital | 15 (71.4) | 7 (77.8) | 22 (73.3) |
| Financial issues | 6 (28.6) | 2 (22.2) | 8 (26.7) |
| No complaint | 11 (52.4) | 4 (44.4) | 15 (50) |
| Continue going out from home for other purposes | |||
| Yes | 12 (57.1) | 5 (55.6) | 17 (56.7) |
| No | 9 (42.9) | 4 (44.4) | 13 (43.3) |
| Not systematically wear a mask outside | 6 (28.6) | 1 (11.1) | 7 (23.3) |
| Self-rated health status | |||
| Good | 11 (52.4) | 4 (44.5) | 15 (50) |
| Bad | 10 (47.6) | 5 (55.5) | 15 (50) |
| Functional decline | |||
| Yes | 4 (19) | 3 (33.3) | 7 (23.3) |
| Loss of appetite | |||
| Yes | 4 (19) | 5 (55.6) | 9 (30) |
| Weight loss | |||
| Yes | 5 (23.8) | 4 (44.4) | 9 (30) |
| Feel isolated at home | |||
| No | 21 (100) | 9 (100) | 30 (100) |
| Consultated in private hospital | |||
| Yes | 7 (33.3) | 2 (22.2) | 9 (30) |
Note. COVID-19: Coronavirus disease 2019.
As regards functional status, seven participants (23.3%) had a decline in their functional status since the last geriatric consultation in comparison with their baseline ADL. Most declared a decline on transferring (71.2%, n = 5) and continence (42.9%, n = 3). Loss of appetite and weight loss were both reported in nine participants (30%).
Half of participants (n = 15) self-rated their health as bad since their last geriatric consultation. Among them, 30% (n = 9) had consulted at a private health center. The most frequent complaints were arthralgia (53.3%, n = 8), confusion (33.3%, n = 5) and dry cough (13.3%, n = 2). Three (20%) participants with bad health status died.
Discussion
Cameroon reported an increase in life expectancy by 10 years between 1950 and 2015. The healthcare demand in this aging population is increasing, but health system is ill-prepared to meet their needs. Those with frailty, multimorbidity, and physical dependence are particularly vulnerable to COVID-19 and are less likely to benefit from intensive medical treatment if they become unwell. Total confinement has not been adopted as a compulsory measure to prevent SARS-Cov-2 spreading in our country. Recommendations to avoid social gatherings and limit movements for older people were difficult to apply in this context.
Our study revealed that most patients did not attend their outpatient visit because of fear of being infected by SARS-CoV-2 at the hospital. Half of patients self-rated their health as bad since their last consultation and 30% decided to consult private health facilities. This could be explained by the fact that in Cameroon some public health facilities were requisitioned to create COVID-19 units and the Yaounde Central hospital set up the first COVID-19 dedicated unit of the country in March 2020. Hence this hospital was considered by the general population as a COVID-19 dedicated hospital, resulting in a drastic drop in attendance by patients with other health issues. However, the fear of contracting SARS-CoV-2 in the hospital contrasts with the fact that more than 50% of our patients continue to go out for other purposes like family and religious events. They are compliant to confinement rules only when it comes to going to the hospital, forgetting at the same time that the virus is present in the community. Thus, it is difficult to prevent older people from exposure to virus, but it is a bigger challenge to prevent them from other worst health effects such as functional decline or decompensation of chronic medical conditions at home. Although many older adults are vigorous, most of them suffer from comorbidities making them more vulnerable to severe COVID-19 and associated death (Chen et al., 2020). The current clinical data sufficiently show that older people are at higher risk of severe illness, 8 out of 10 deaths from the infection have been in adults 65 years of age and older (Morbidity and Mortality Weekly Report, 2020). It is therefore important to strengthen awareness that SARS-CoV-2 can be contracted in the community and emphasize that while respecting the other preventive measures, total confinement is advisable for older people in the current situation even if it has not been adopted by our government mainly for economic reasons.
About 23% of patients declared at least one difficulty in performing ADL compared to their baseline functional status, with transferring and continence being the most affected. Functional status is an independent predictor of morbidity and mortality in older adults (Silva et al., 2009). Since the beginning of the pandemic, social restrictions have been proposed to protect older people from the virus. Despite their comorbidities, functional decline can be exacerbated by low levels of physical activity as well as low frequency of social interactions. In developed countries, many older people are experiencing social isolation and functional decline at home. To address their needs, online technologies are used to maintain virtual socialization and access to resources including purchasing food and drugs. Social isolation is not frequent in our setting because most older people live with their children and grandchildren. It is important to raise awareness of family caregivers to the fact that confinement does not mean isolation and to propose moderate intensity physical activities to older people to avoid functional decline. We must also be aware of the risk of depression and various types of abuse on those who are abandoned by their relatives. While we strongly emphasize on social restrictions and other barrier measures, we should develop strategies to continue taking care of our older people and manage their chronic medical conditions to avoid decompensation at home. Telephone consultations can be used to continue keeping in touch with our patients during the pandemic and thus recommend a visit at the hospital only in case of serious health issues. In some cases, we can also suggest visits at home with a dedicated staff.
Conclusion
Our survey demonstrates that in a context where total confinement has not been adopted, older patients drop out of routine geriatric consultations due to fear of the hospital milieu. While it is important to continue to raise awareness on barrier measures against COVID-19, we must urgently put in place measures to follow-up geriatric patients at home. Telephone interviews could be a quick and simple way to inquire about their well-being and thus limit movements for the most vulnerable alongside regulating hospital attendance.
What Is Already Known on This Topic
The current data suggest that older people, particularly those with serious underlying health conditions are at higher risk of severe COVID-19 and related deaths. As a result of the total confinement in developed countries, many older people suffer from negative effects of social restrictions including isolation, functional decline, and worsening of their chronic medical conditions.
What This Study Adds
This study gives information on effects of COVID-19 pandemic on follow-up and well-being of older patients, in a resource-limited setting where confinement has not been adopted as a compulsory measure mainly for economic reasons. Many older people continue to go out for other purposes than their medical visits and most present with functional decline at home. This suggests that while providing advices to social restrictions to protect them from virus, we should develop strategies to continue taking care of them at home.
Limitations
As a retrospective study with a small sample size, our findings might not be generalized. Weight loss and health status assessment was not accurate due to self-rating by participants.
Acknowledgments
The authors thank the patients and their advisers for accepting to participate in the interview and for authorizing the authors to analyze those informations.
Footnotes
Author Contributions: MJNE, VN, and GA conceived the study. MJNE and MZO performed data collection. MJNE, VN, ES, and GA supervised data collection. MJNE and VN and analyzed data. MJNE and VN drafted the manuscript. JJN, LC, ES, and GA critically revised the manuscript. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval was not sought for the present study because we retrospectively reviewed the consultation logbook to collect the information given by the patients.
ORCID iDs: Marie Josiane Ntsama Essomba  https://orcid.org/0000-0002-3417-3351
https://orcid.org/0000-0002-3417-3351
Laura Ciaffi  https://orcid.org/0000-0003-4829-0935
https://orcid.org/0000-0003-4829-0935
References
- Archived: WHO Timeline-COVID-19. (2020). https://www.who.int/news-room/detail/27-04-2020-who-timeline—covid-19
- Chen R., Liang W., Jiang M., Guan W., Zhan C., Wang T., Tang C., Sang L., Liu J., Ni Z., Hu Y., Liu L., Shan H., Lei C., Peng Y., Wei L., Liu Y., Hu Y., Peng P., Wang J., . . . Medical Treatment Expert Group for COVID-19. (2020). Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest, 158(1), 97–105. https://doi.org10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronavirus (COVID-19) mortality rate. (2020). https://www.worldometers.info/coronavirus/coronavirus-death-rate/
- COVID-19 Coronavirus pandemic. (2020). https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1?%22#countries
- Katz S. (1983). Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society, 31(12), 721–727. 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- Morbidity and Mortality Weekly Report. (2020). Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm#contribAff [DOI] [PMC free article] [PubMed]
- Silva T. J., Jerussalmy C. S., Farfel J. M., Curiati J. A., Jacob-Filho W. (2009). Predictors of in-hospital mortality among older patients. Clinics, 64(7), 613–618. 10.1590/S1807-59322009000700002. [DOI] [PMC free article] [PubMed] [Google Scholar]