Abstract
Congenital pseudarthrosis of the tibia (CPT) is a rare congenital malformation. It is characterized by a tibial anterior bowing deformity or specific types of non-union, which typically result from abnormal development of the tibia, leading to the formation of local pseudarthrosis. The treatment of CPT is very challenging. The advent of 3D printing and computer-assisted techniques in recent years has provided a new ancillary technique for treatment planning and implementation. This case report describes the successful surgical treatment of a 14-year-old male that presented with a shortened limb deformity. Ahead of elective surgery, 3D printing and computer-assisted techniques were used to provide a 1:1 model of his left tibia, fibula and ankle joint to precisely determine the surgical procedure. The first surgery did not result in complete calcification of the tibial extension area, so a second proximal tibia iliac bone graft and internal fixation surgery was undertaken. Following regular follow-up and rehabilitation, by the 18-month follow-up, the proximal tibial bone graft had healed and the patient had resumed walking with a normal gait. This case report describes in detail the successful use of unilateral external fixation using the Ilizarov technique, 3D printing and computer-assisted orthopaedic surgery in the planning of treatment for CPT.
Keywords: Case study, congenital pseudarthrosis of the tibia, digital orthopaedic, surgery
Introduction
Congenital pseudarthrosis of the tibia (CPT) is difficult to treat in paediatric patients. Some patients eventually undergo amputation because of incorrect treatment and repeated fractures.1 CPT was first described in 1709 by Hatzoecher. It is characterized by a tibial anterior bowing deformity or specific types of nonunion that typically result from abnormal development of the tibia, which results in the formation of local pseudarthrosis. Pathologically, in CPT, the affected tibia exhibits insufficient mechanical strength and osteogenic capability.2 An abnormal highly cellular fibrovascular tissue grows at the expense of the bony cortex.2 As it encroaches on the bony cortex, it promotes incoordinate osteoclastic bone resorption that does not have a normal bone modelling purpose.2 Reactive changes simultaneously occur at the medullary aspect leading to deposition of excess trabecular bone and hence medullary sclerosis.2 Excessive bone resorption accounts for intracortical cysts. Impaired vascularization can result in decreased osteogenic capabilities.2 A fibrous hamartoma surrounds the bone at the congenital pseudarthrosis of the tibia site.3 In the past, healing after bone graft surgery was slow and frequently associated with limb shortening.4 These cases also tended to require proximal bone extension for bone shortening and osteotomy for distal pseudarthrosis resection with the Ilizarov technique.5 However, the surgical treatment of such diseases remains a challenge for orthopaedic surgeons and a variety of surgical methods are often combined for CPT.5 The advent of 3D printing and computer-assisted techniques in recent years has provided a new auxiliary technique for treatment planning and implementation.6 This current case report is a description of how the use of 3D printing and computer-assisted techniques can provide a 1:1 model of the tibia and fibula including any ankle joint deformity to precisely plan the surgical procedure. The successful use of unilateral external fixation using the Ilizarov technique, 3D printing and computer-assisted orthopaedic surgery in the planning of the treatment of CPT is described.
Case report
A 14-year-old male presented at the Department of Traumatology, The Zhanjiang Central People's Hospital, Zhanjiang, Guangdong Province, China in July 2015 with a shortened limb deformity and multiple cafe-au-lait spots (Figure 1a). The patient showed severe left ankle valgus that had worsened with age and left lower limb shortening of approximately 3.0 cm (Figure 1b). The patient had shown evidence of the condition for approximately 11 years. He was unable to walk normally and was suffering from complete non-union with extensive bone defects. Both clinical and radiographic assessment (Figure 1c) led to a diagnosis of Crawford type 2 CPT.7
Figure 1.
A 14-year-old male child presented with a shortened limb deformity of 11 years duration and multiple cafe-au-lait spots: (a) cafe-au-lait spots on the body; (b) the appearance of the left calf deformity; (c) X-ray radiography of the crus. The colour version of this figure is available at: http://imr.sagepub.com.
Before surgery, the patient’s left calf was scanned using a 64-slice spiral computed tomography (CT) scanner (Aquilion 64; Toshiba, Otawara, Japan). The Digital Imaging and Communications in Medicine data were extracted and input into Mimics software version 10.0 (Materialise, Leuven, Belgium) to create a 3D reconstruction of the left tibia and fibula including the ankle joint.
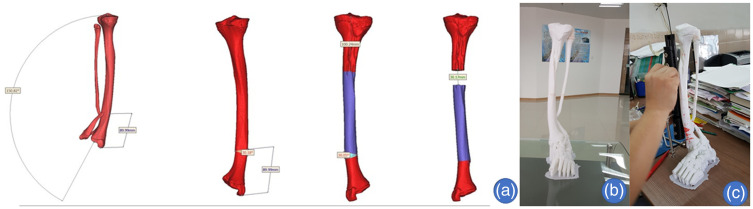
A computer simulation was used to design the surgery plan (Figure 2a). A computer was used to measure a distal tibial anterior bow angle of approximately 30°, with left lower limb shortening of approximately 3.0 cm. The design of the angle and position of the osteotomy at the anterior bow of the distal tibia were completed using the computer. The distance between the proximal osteotomy plane and the end of the malleolus medialis was approximately 9.0 cm. The distance between the proximal tibial transverse subperiosteal truncation and the knee joint line was approximately 10 cm. The output STL file was fed into the 3D printer, which produced a 1:1 3D model of the left tibia and fibula including the ankle joint (Figure 2b). There was a pseudarthrosis in the distal fibula model. The position and angle of the anteromedial wedge osteotomy in the distal sections of the tibia were marked on the model. The location of the unilateral external fixator for the proximal tibial bone lengthening was determined (Figure 2c).
Figure 2.
A computer simulation was used to design the surgery plan: (a) the surgery plan as designed by the computer; (b) a 3D printed 1:1 model of the left tibia and fibula including the ankle joint and foot of the 14-year-old male child; (c) the osteotomous position and angle of the anteromedial wedge osteotomy in the distal sections of the tibia were marked on the 3D model. The colour version of this figure is available at: http://imr.sagepub.com.
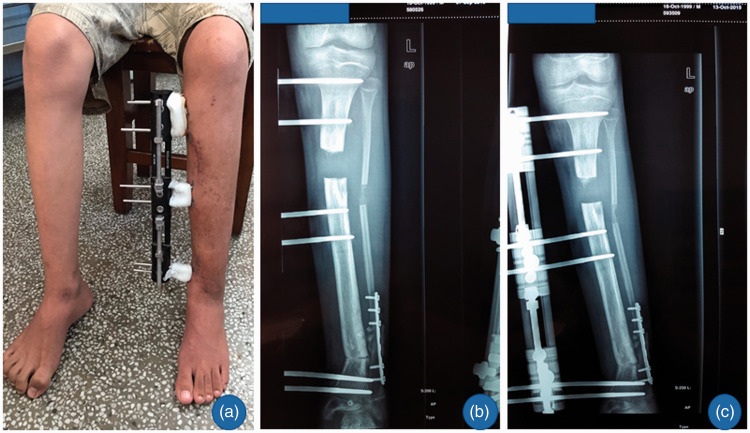
The patient was placed in a supine position and anaesthetized by general anaesthetic. The area was swabbed and a 3-cm medial longitudinal incision was made on the distal left lower leg. According to the preoperative 3D model, anteromedial 30° wedge osteotomy at the apex of the anterior bow of the distal tibia was performed. Next, an 8-cm lateral longitudinal incision was made along the distal left lower leg and the pseudarthrosis of the fibula was resected. The defect of the fibula was repaired with allograft bone and fixed with a 7-hole reconstruction fixation plate. At 10 cm under the left knee joint line, transverse subperiosteal truncation was made to the proximal tibia and fibula, and a unilateral external fixator was fitted and nailed at proximal and distal points (Figure 3a). The section of distal tibial osteotomy was compressed and the section of proximal osteotomy was elongated with the unilateral external fixation using the Ilizarov technique (Figure 3b).
Figure 3.
Representative imaging of the surgical procedure: (a) distal tibia bone cutting and proximal tibia bone lengthening with external fixation during the first stage; (b) X-ray of the left tibiofibular 1 week after the surgery. The colour version of this figure is available at: http://imr.sagepub.com.
At 1 week after surgery, the left calf and ankle joint were fixed with orthopaedic braces. The patient showed neither bleeding nor infection, with a good blood supply and sensory and motor function to the left lower limb. Bone extension commenced 10 days after surgery, extending the length of the bone by 1 mm per day, with adjustments made four times a day. At the 1-month follow-up, a tibial extension of approximately 3.0 cm had been achieved, with satisfactory recovery of the left lower limb length (Figure 4a). There was minor calcification at the tibial extension area, but satisfactory at the fibular extension area (Figure 4b). As a result, further bone elongation was ceased. At the 2-month follow-up, there were higher rates of calcification at the tibial extension area and satisfactory calcification at the fibular extension area (Figure 4c).
Figure 4.
Representative postoperative imaging: (a) the length of the left lower limb was satisfactory after 1-month follow-up; (b) ossification of the extended part of the left tibia was normal after the 1-month follow-up; (c) At the 2-month follow-up, there were higher rates of calcification at the tibial extension area and satisfactory calcification at the fibular extension area.
At 8 months after surgery, calcification of the tibial extension area was incomplete and the two ends were still not united. The healing of the distal tibial osteotomy was satisfactory. The healing of the area of pseudarthrosis and extension of the fibula was completed. A decision was made to undertake a second proximal tibia iliac bone graft and internal fixation surgery (Figure 5a). In the second surgery, the unilateral external fixator maintained the length of the left calf, and after the bone graft was internally fixed, the external fixation was dismantled (Figure 5b). With regular follow-up and rehabilitation, at the 18-month follow-up, the proximal tibial bone graft had healed (Figure 5c) and the patient had resumed walking with a normal gait (Figure 5d).
Figure 5.
Representative imaging during and after a second proximal tibia iliac bone graft and internal fixation surgery at 8 months after the original surgery: (a) there was no continuous callus in the ossification of the extended part after the 8-month follow-up so a second surgery was undertaken; (b) completed bone grafting and internal fixation operation during the second surgery; (c) the bone grafting had healed at the 18-month follow-up; (d) the patient was able to walk with a normal gait after the 18-month follow-up.
The study protocol was approved by the Institutional Review Board at The Zhanjiang Central People's Hospital, Zhanjiang, Guangdong Province, China (no. KY-SB-2018-005). Written informed consent was obtained from the patient’s legal guardians for publication of this study and any accompanying images.
Discussion
Ilizarov was the first to use the external circular fixation technique, which can be adapted to the type of pseudarthrosis found in CPT.8 Usually, an intramedullary rod is used for CPT.5,9 Despite the variety of surgical procedures for the treatment of CPT,10–12 the choice of surgical approach centres on three basic premises: (i) union of the pseudarthrosis; (ii) prevention of fractures; and (iii) the correction of any limb deformities. This current case report describes an approach to the treatment of CPT that used unilateral external fixation based on the Ilizarov technique, 3D printing and computer-assisted orthopaedic surgery. Unilateral fixators provide stability and much improved patient comfort compared with circular fixators.13 When compared with circular fixators, the unilateral designs are less awkward.13 Their reduced bulk facilitates the maintenance of good hygiene and accommodates the use of greater clothing options.13 In this current case, the area of distal tibial osteotomy was compressed, so it was not different from the traditional Ilizarov technique. However, this case study suggests that it is good for healing.
The clinical application of 3D printing and computer-assisted technology has become a model of cross-discipline cooperation and scientific research transformation in the field of medicine.14 As this current case demonstrates, with the use of computer-assisted technology and a 3D model of the limb, surgeons can more precisely design the angle and position of the osteotomy and have a more extensive understanding of the anatomy of CPT prior to surgery.
Congenital pseudarthrosis of the tibia is often associated with neurofibromatosis or neurotrophic malnutrition.15 Neurotrophic malnutrition is a possible cause of the non-union of CPT. Neural regulation plays an important role in fracture healing.16 There are now a variety of ways to treat bone defects.17 The Ilizarov technique is widely used for bone and soft-tissue defects.18 In this current case, however, early bone lengthening surgery was undertaken using unilateral external fixation, so a bone graft internal fixation surgery was necessary. Considering the use of allogeneic or autogenous bone for grafting, autogenous bone has a higher survival rate. Transplanting fibula anastomosed with nourishing blood vessels has the highest rate of success.19 Nonetheless, the operation was complicated. This current case involved an iliac bone grafting and internal fixation operation for the proximal tibial bone defect. At the 18-month follow-up, the proximal tibial bone graft had healed. Iliac bone grafting is suitable for the bone defects associated with CPT, which have the characteristics of large quantity, shallow position and simple operation.
There are several key advantages associated with unilateral external fixation using a 3D printed model and computer-assisted technology in the surgical treatment of CPT: (i) when assessing the deformity and creating a plan for the surgical approach, the 1:1 CPT model printed with 3D printing technology is more informative than trying to reconstruct the bone using CT images; (iii) the 3D printing-assisted external fixation technology allows for more minimally invasive, personalized and precise surgical procedures, which should achieve better surgical results in the long term; (iii) when considering CPT in patients with neurodevelopmental disorder, the treatment of CPT may need a second proximal tibia iliac bone graft and internal fixation operation.
This current case report describes satisfactory clinical results in a child with CPT, which suggests that unilateral external fixation using 3D printing and computer-assisted technology is a novel and successful surgical method worthy of clinical application.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This work was supported by grants from the Natural Science Foundation of Guangdong Province (No. 2014A030307012), the Zhan Jiang Key Laboratory of Orthopaedic Technology and Trauma Care (No. 2015A06011) and the Science and Technology Planning Project of Zhanjiang (No. 2018A01033).
ORCID iD
Hua Zhong https://orcid.org/0000-0002-8507-9533
References
- 1.Kong LD, Cheng HX, Nie T. Treat the congenital pseudarthrosis of the Tibia with Ilizarov technology: Case report. Medicine (Baltimore) 2018; 97: e13384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah H, Rousset M, Canavese F. Congenital pseudarthrosis of the tibia: Management and complications. Indian J Orthop 2012; 46: 616–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Rosasy MA. Congenital pseudarthrosis of the tibia: the outcome of a pathology-oriented classification system and treatment protocol. J Pediatr Orthop B 2020; 29: 337–347. [DOI] [PubMed] [Google Scholar]
- 4.Zumiotti A, Ferreira MC. Treatment of congenital pseudarthrosis of the tibia by microsurgical fibula transfer. Microsurgery 1994; 15: 37–43. [DOI] [PubMed] [Google Scholar]
- 5.Zhu GH, Mei HB, He RG, et al. Combination of intramedullary rod, wrapping bone grafting and Ilizarov's fixator for the treatment of Crawford type IV congenital pseudarthrosis of the tibia: mid-term follow up of 56 cases. BMC Musculoskelet Disord 2016; 17: 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoang D, Perrault D, Stevanovic M, et al. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med 2016; 4: 456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford AH, Jr, Bagamery N. Osseous manifestations of neurofibromatosis in childhood. J Pediatr Orthop 1986; 6: 72–88. [DOI] [PubMed] [Google Scholar]
- 8.Gubin AV, Borzunov DY, Marchenkova LO, et al. Contribution of G.A. Ilizarov to bone reconstruction: historical achievements and state of the art. Strategies Trauma Limb Reconstr 2016; 11: 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su YP, Wang MN, Chang WN. Successful treatment of congenital pseudarthrosis of the tibia with long segment fibular allografting in a young child. J Formosan Medical Association 2007; 106: S44–S49. [DOI] [PubMed] [Google Scholar]
- 10.Chalopin A, Pesenti S, Peltier E, et al. Transplantar intramedullary locking nailing in childhood congenital pseudarthrosis of the tibia: A report of 3 cases. Orthop Traumatol Surg Res 2016; 102: 521–524. [DOI] [PubMed] [Google Scholar]
- 11.Pollon T, Sales De Gauzy J, Pham T, et al. Salvage of congenital pseudarthrosis of the tibia by the induced membrane technique followed by a motorised lengthening nail. Orthop Traumatol Surg Res 2018; 104: 147–153. [DOI] [PubMed] [Google Scholar]
- 12.Vukasinović Z, Spasovski D, Seslija I, et al. Congenital pseudarthrosis of lower leg treated by almost outdated method–case report. Srp Arh Celok Lek 2014; 142: 89–93 [Article in Serbian, English abstract]. [DOI] [PubMed] [Google Scholar]
- 13.Fragomen AT, Rozbruch SR. The mechanics of external fixation. HSS J 2007; 3: 13–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cai H. Application of 3D printing in orthopedics: status quo and opportunities in China. Ann Transl Med 2015; 3: S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatton MJ, Ly T, Noor S, et al. Delayed presentation of congenital tibial pseudarthrosis and neurofibromatosis: a difficult union. Asian Biomed 2014; 8: 111–118. [Google Scholar]
- 16.Lei SH, Guo L, Yue HY, et al. Marrow stromal stem cell autologous transplantation in denervated fracture healing: an experimental study in rats. Orthop Surg 2013; 5: 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vidal L, Kampleitner C, Brennan MÁ, et al. Reconstruction of Large Skeletal Defects: Current Clinical Therapeutic Strategies and Future Directions Using 3D Printing. Front Bioeng Biotechnol 2020; 8: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tetsworth K, Paley D, Sen C, et al. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 2017; 48: 2276–2284. [DOI] [PubMed] [Google Scholar]
- 19.Hu B, Gao D, He Y. Efficacy of fibula fixation in the early treatment of osteonecrosis of the femoral head and its effects on local microcirculation, articular surface collapse, joint pain and function. J Musculoskelet Neuronal Interact 2018; 18: 55–61. [PMC free article] [PubMed] [Google Scholar]