Abstract
Background
Vulvar lichen sclerosus (LS) is a chronic dermatosis for which the true prevalence is not well established. LS remains an underrecognized and undertreated disease, and treatment patterns and differences among various specialties that care for patients with LS are largely unknown.
Objective
This study sought to determine the prevalence of diagnosed vulvar LS, demographic characteristics, and diagnostic and treatment patterns in the United States.
Methods
A database comprising >21.7 million women with commercial insurance in the United States was analyzed, and the largest cohort of patients with LS in the United States to date was identified.
Results
We found that obstetricians/gynecologists are diagnosing and managing approximately half of women with LS, and regardless of specialty, the majority of providers are appropriately prescribing high-potency topical steroids.
Conclusion
Our results suggest that LS may truly be underrecognized and underdiagnosed, especially in younger women.
Keywords: Lichen sclerosus, Vulvar lichen sclerosus, Prevalence, Treatment
Introduction
Vulvar lichen sclerosus (LS) is a chronic inflammatory dermatosis with poorly established etiology. Traditional teaching is that there is a bimodal onset in prepubertal children and in postmenopausal women (Cooper et al., 2008, Fistarol and Itin, 2013, Schlosser and Mirowski, 2015). However, recent studies suggest that LS may also occur more commonly at other ages than previously thought. One group from London reported that approximately 20% of patients develop LS during their reproductive years (Trokoudes and Lewis, 2019), and a group in Beijing found that 75.2% of their sample of 129 women developed LS during the childbearing period (Yang et al., 2018). The true incidence and prevalence of LS are unknown and difficult to estimate because affected patients, if they choose to see a physician for their potentially embarrassing symptoms, present to various specialists (Pugliese et al., 2007). It has been suggested that women in urban settings, with stronger health awareness and better access to health care, may present more frequently (Yang et al., 2018), potentially creating geographic differences.
In our experience and that of our colleagues, LS remains an underrecognized and undertreated disease. Estimated prevalence ranges from 0.1% to 0.33% in a community-based dermatology department to 1.7% in a private gynecology practice, suggesting a higher rate of presentation to gynecologists than dermatologists (Goldstein et al., 2005). Variations in treatment patterns between specialties are unknown. This study sought to determine the prevalence of diagnosed LS, demographic characteristics, and diagnostic and treatment patterns in the United States.
Methods
The study population included patients in the IBM MarketScan Commercial Claims and Encounters Databases from 2015 to 2017 with ≥2 independent diagnoses of LS (International Classification of Diseases, 10th Revision, Clinical Modification code L90.0). This database comprises >21.7 million women with commercial insurance in the United States. The study population was compared with a control population of women without LS. Patient age and geographic region, provider type, biopsy preferences, and treatment prescribed were examined.
Results
We identified 10,004 women with a diagnosis of LS between 2015 and 2017 in the United States, which is a prevalence of 0.05%. The demographics of patients and controls are shown in Table 1. Seventy-nine percent of women in our data set were between the ages of 45 and 65 years, with an average age of 50.8 years (standard deviation: 13.6 years). Sixteen percent of patients with LS were age 18 to 44 years. In pediatric patients (age: 0–17 years), disease prevalence was 0.01%.
Table 1.
Descriptive characteristics of sample.
| Age, years, % (n) | Lichen sclerosus population | Control population |
| 0–17 | 4.93 (493) | 23.4 (5,077,773) |
| 18–34 | 6.35 (635) | 29.2 (6,352,078) |
| 35–44 | 9.68 (968) | 15.8 (3,432,717) |
| 45–54 | 26.01 (2602) | 16.5 (3,591,622) |
| 55–65 | 53.04 (5306) | 15.1 (3,270,708) |
| Region, % (n) | ||
| Northeast | 20.5 (2053) | 16.5 (3,567,608) |
| North Central | 24.1 (2406) | 19.8 (4,297,275) |
| South | 38.3 (3834) | 46.1 (9,988,061) |
| West | 16.95 (1690) | 17.3 (3,739,029) |
| Unknown | 0.21 (21) | 0.4 (80,043) |
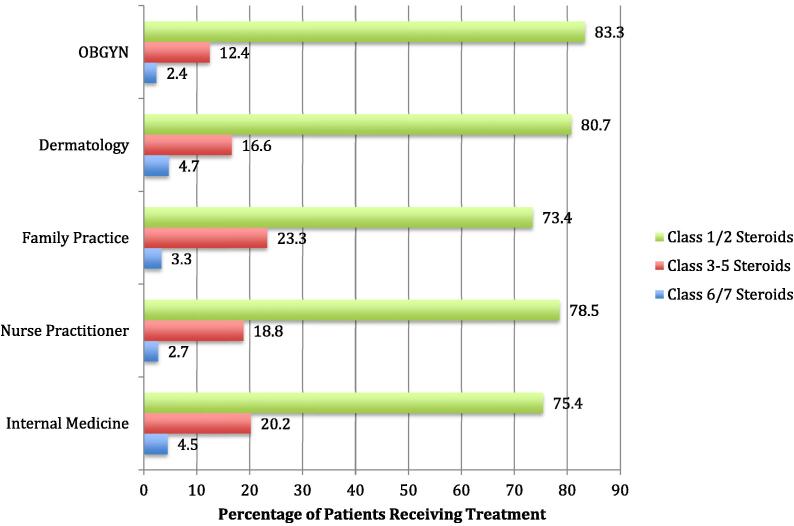
Obstetricians/gynecologists (Ob/Gyns) and dermatologists made up the majority of diagnosing clinicians: 52.4% (n = 5245) and 14.5% (n = 1450), respectively. Other clinicians included family medicine physicians (6.5%; n = 650), nurse practitioners (2.5%; n = 246), and internal medicine physicians (0.4%; n = 42). Twenty-two percent of patients (n = 2238) had a biopsy. Treatments prescribed are shown in Fig. 1. Among patients who saw an Ob/Gyn or dermatologist, 83% and 80%, respectively, received high-potency (Class 1 or 2) topical corticosteroids. Although slightly less than Ob/Gyn and dermatologists, >70% of all other clinician categories also prescribed high-potency steroids (Fig. 1).
Fig. 1.
Treatments prescribed by top five specialties/types of providers treating lichen sclerosus.
Discussion
Our study found LS to have a claims-based prevalence of 0.05%, using a definition of ≥2 claims, a lower prevalence than previously reported which suggests significant underdiagnosis. Of note, 16% of diagnoses were in women between the ages of 18 and 44 years, which may represent underdiagnosis in this age group based on recent studies (Trokoudes and Lewis, 2019, Yang et al., 2018). The low prevalence among pediatric patients may be attributable to several factors, including relative rarity and variability in pediatric clinicians’ familiarity with LS and in patients’ clinical symptoms (Lagerstedt et al., 2013). The majority of cases are diagnosed by dermatologists and Ob/Gyn; however, family practice and internal medicine physicians, as well as nurse practitioners, are also seeing relatively high percentages of cases. Biopsies are not performed in the majority of cases. There does not appear to be geographic variation in diagnosis, although our data did not compare urban and nonurban settings specifically.
Clinicians are appropriately prescribing high-potency steroids, although we do not know if frequency or duration of treatment is appropriate. Internal and family medicine physicians prescribe high-potency steroids at slightly lower rates than Ob/Gyns and dermatologists. Therefore, educational efforts directed at these clinicians may be warranted.
Study limitations include coding errors and the inability to know whether biopsies or prescriptions were ordered for LS or a concurrent diagnosis. LS has a specific International Classification of Diseases, 10th Revision, code used most commonly by experts, strengthening the reliability of diagnoses, but this also limits our ability to capture those correctly diagnosed but incorrectly coded and those potentially misdiagnosed. In our data, disease predominates in women aged 45 to 65 years; however, women aged >65 years, individuals who lack private insurance, and those covered by Medicare are not represented. This may affect the case number, given that LS is more symptomatic when estrogen is low, which tends to occur more commonly later in life.
Conclusion
This study identified the largest cohort of patients with LS in the United States to date. Our results support that this condition may truly be underrecognized and underdiagnosed, especially in younger, fertile women. Ob/Gyns are diagnosing and managing approximately half of women with LS; however, women may present to a variety of provider types. Regardless of specialty, the majority of providers are appropriately prescribing high-potency topical steroids. Future studies examining these diagnostic and treatment trends in older populations, as well as those without private insurance, are warranted. Understanding the current management of LS is important given that un- or undertreated disease can significantly affect patients’ quality of life, lead to increased lower urinary tract symptoms and irreversible architectural changes (Lagerstedt et al., 2013), and predispose women to squamous cell carcinoma.
Conflict of Interest
None.
Funding
This project was accomplished through a generous gift from The Louis and Rachel Rudin Foundation, Inc., which supports the research education of residents at NYU Langone Health’s Ronald O. Perelman Department of Dermatology.
Study Approval
N/A.
Financial disclosures
Dr. Miriam Kelz Pomeranz serves on the scientific advisory board for Procter and Gamble and receives royalties from UptoDate.
References
- Cooper S.M., Ali I., Baldo M., Wojnarowska F. The association of lichen sclerosus and erosive lichen planus of the vulva with autoimmune disease: a case-control study. Arch Dermatol. 2008;144(11):1432–1435. doi: 10.1001/archderm.144.11.1432. [DOI] [PubMed] [Google Scholar]
- Fistarol S.K., Itin P.H. Diagnosis and treatment of lichen sclerosus: an update. Am J Clin Dermatol. 2013;14(1):27–47. doi: 10.1007/s40257-012-0006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A.T., Marinoff S.C., Christopher K., Srodon M. Prevalence of vulvar lichen sclerosus in a general gynecology practice. J Reprod Med. 2005;50(7):477–480. [PubMed] [Google Scholar]
- Lagerstedt M., Karvinen K., Joki-Erkkila M., Huotari-Orava R., Snellman E., Laasanen S.L. Childhood lichen sclerosus–a challenge for clinicians. Pediatr Dermatol. 2013;30(4):444–450. doi: 10.1111/pde.12109. [DOI] [PubMed] [Google Scholar]
- Pugliese J.M., Morey A.F., Peterson A.C. Lichen sclerosus: review of the literature and current recommendations for management. J Urol. 2007;178(6):2268–2276. doi: 10.1016/j.juro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- Schlosser B.J., Mirowski G.W. Lichen sclerosus and lichen planus in women and girls. Clin Obstet Gynecol. 2015;58(1):125–142. doi: 10.1097/GRF.0000000000000090. [DOI] [PubMed] [Google Scholar]
- Trokoudes D., Lewis F.M. Lichen sclerosus - the course during pregnancy and effect on delivery. J Eur Acad Dermatol Venereol. 2019;33(12):e466–e468. doi: 10.1111/jdv.15788. [DOI] [PubMed] [Google Scholar]
- Yang M., Wen W., Chang J. Vulvar lichen sclerosus: a single-center retrospective study in China. J Dermatol. 2018;45(9):1101–1104. doi: 10.1111/1346-8138.14533. [DOI] [PubMed] [Google Scholar]