Abstract
Objective:
Migraine is a common recurrent headache disorder affecting 14% American adults. Although weather and air pollution are ofte reported by patients with migraine as precipitating factors, previous studies have had mixed results.
Methods:
We prospectively collected migraine headache onset using electronic questionnaires from 98 adults in the Greater Boston area with episodic migraine (2016–2017). Each participant was followed for an average of 45 days for a total of 4406 days of observation. Temperature, relative humidity, and barometric pressure data were obtained from local weather station. Daily average fine particulate matter, daily maximum 1-hour sulfur dioxide, daily maximum 1-hour nitrogen dioxide, daily maximum 8-hour ozone, and daily maximum 8-hour carbon monoxide from local air pollution monitors. We conducted a repeated measures analysis using fixed effects logistic regression models. In the models we adjusted for day of week, a natural cubic spline term of day of the year with 4 degrees of freedom, and a participant identifier. We additionally adjusted for linear terms of temperature and relative humidity in the air pollution analyses. We also applied logistic regression models with generalized estimating equation (GEE) with autoregressive correlation structure in the sensitivity analysis.
Results:
The mean age was 35 years and 88% were women. Mean temperature was 56.9°F, relative humidity 67.3%, and fine particulate matter 7.3 μg/m3. Higher relative humidity was associated with higher odds of migraine headache, but the association was only observed in warm season (April-September). Higher daily of maximum 8-hour ozone and daily maximum 8-hour carbon monoxide appeared to be associated with higher odds of migraine headache onset in cold season (October-March). Although the associations for O3 and relative humidity were attenuated and no longer statistically significant in the overall GEE analysis, the differing associations by season remained.
Conclusions:
We found that higher relative humidity was associated with higher odds of migraine headache onset in the warm season, and traffic-related gaseous pollutants may be associated with higher odds of migraine headache onset in the cold season.
Keywords: Air Pollution, Cohort Study, Headache, Migraine Disorders, Precipitating Factors, Weather
1. Introduction
Migraine is a recurrent headache disorder characterized by symptoms such as headache, nausea, vomiting, photophobia, and phonophobia (International Headache Society 2018). According to the Global Burden of Disease Study 2016, in 2016, the global age-standardized prevalence was 14.4%; 1.04 billion individuals were estimated to have migraine, and migraine attributed to an estimation of 45.1 million years of life lived with disability (GBD 2016 Headache Collaborators 2018). In the U.S., migraine and severe headaches affect approximately about 1 in every 7 adults (Burch et al. 2015) and are associated with high societal cost: the annual societal costs were estimated at about $2,649 U.S. dollars (2013) per person per year for patients with episodic migraine, and about $8,243 U.S. dollars (2013) per person per year for those with chronic migraine (Messali et al. 2016).
Weather is perceived by patients with migraine as a common trigger of migraine headache (Andress-Rothrock et al. 2010; Pellegrino et al. 2018; Peroutka 2014), however, findings from epidemiologic studies remain inconclusive. Studies from several decades ago compared headache frequencies among participants during or after different weather conditions and have had mixed results (Cull 1981; Gomersall and Stuart 1973; Osterman et al. 1981; Schulman et al. 1980; Wilkinson and Woodrow 1979). Findings from more recent studies suggest that there may be a subgroup of patients with migraine who are susceptible to weather (Hoffmann et al. 2011; Hoffmann et al. 2015; Prince et al. 2004; Yang et al. 2015), with two of these studies reporting associations between lower temperature and higher number of migraine headaches among the “weather sensitive” participants (Hoffmann et al. 2011; Yang et al. 2015). Some larger scale epidemiologic studies obtained data from emergency department visits and have found generally positive associations between daily average temperature and number of visits for migraine headache (Mukamal et al. 2009; Vodonos et al. 2015; Yilmaz et al. 2015), but not all (Villeneuve et al. 2006). Findings for relative humidity or barometric pressure are also inconsistent (Mukamal et al. 2009; Villeneuve et al. 2006; Yilmaz et al. 2015). In a recent prospective diary-based study, a ridge of high pressure was associated with headache attacks but not with migraine (Zebenholzer et al. 2011). Last, few studies have quantitatively examined the magnitude of these associations (Mukamal et al. 2009; Vodonos et al. 2015).
Ambient air pollution is another potential risk factor for headache onset among patients with migraine. The majority of past studies have found associations between higher levels of ambient air pollution and more frequent emergency department visits or clinic visits due to migraine headache (Chen et al. 2015; Chiu et al. 2015; Chiu and Yang 2015; Dales et al. 2009; Lee et al. 2018; Szyszkowicz 2008; Szyszkowicz and Porada 2012; Szyszkowicz et al. 2009), but not all (Mukamal et al. 2009). For example, in a very large study of daily hospitalization records for headache in 7 Chilean urban centers, Dales et al. found that higher levels of fine particulate matter (PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), and carbon monoxide (CO) were associated with higher number of hospitalization for migraine headache (Dales et al. 2009).
Most of the previous studies were conducted outside of the U.S. (Chen et al. 2015; Chiu and Yang 2015; Dales et al. 2009; Hoffmann et al. 2011; Hoffmann et al. 2015; Lee et al. 2018; Szyszkowicz 2008; Szyszkowicz and Porada 2012; Szyszkowicz et al. 2009; Villeneuve et al. 2006; Vodonos et al. 2015; Yang et al. 2015; Yilmaz et al. 2015; Zebenholzer et al. 2011). However, weather conditions and air pollution levels may be influenced by regional climate and/or pollution sources. Moreover, data from emergency department visits records may be affected by factors that may influence patients’ decision to visit the emergency department, such as migraine headache severity, duration, and health care access. We therefore conducted a prospective diary-based cohort study to examine the associations of temperature, relative humidity, barometric pressure, and ambient air pollutants with migraine headache onset among 98 patients with episodic migraine in the Greater Boston area, Massachusetts, U.S..
2. Methods
2.1. Study sample
The study period was from March 2016 to October 2017. We identified potential participants by accessing the patient and research repositories at Beth Israel Deaconess Medical Center and the clinical research registries at the Massachusetts General Hospital and the Brigham and Women’s Hospital; posting flyers in public areas and in the neurology and primary care clinics at Beth Israel Deaconess Medical Center; and physician’s referral. We recruited participants who were 18 years and older, able to communicate in English, had reported history of migraine for at least 3 years, and had reported at least 2 headache days per month. No potential participants were excluded based on criteria of current episode of major depressive disorder as assessed during the clinical interview by a study physician. At the time of enrollment, we excluded potential participants who: 1) reported chronic pain or chronic opioid use; 2) were at high risk for obstructive sleep apnea, assessed by the Berlin questionnaire or with untreated moderate or severe sleep apnea; 3) were pregnant; 4) failed to complete diaries for 4 of 7 days during a run-in period; or 5) reported 15 or more headache days per month during the past 3 months. A total of 131 participants completed the screening and 101 met the inclusion criteria and were enrolled in the cohort study. Of these 101 enrolled participants, three participants were excluded from the analysis because they contributed fewer than 21 days of diary data. In the end, we included data from 98 participants in the analysis. Each participant was followed for an average of 45 days for a total of 4406 days of observation.
At baseline, each participant first completed a baseline questionnaire that collected data on demographics, medication use, lifestyle factors, and measures of psychological factors. Participants were also asked to identify their perceived headache triggers, such as sleep, weather, and caffeinated beverage intake. Participants then completed an online diary each morning and evening for the subsequent 6 weeks. The electronic data were collected by the Research Data Capture (REDCap) tools hosted by Beth Israel Deaconess Medical Center (Harris et al. 2009). All participants provided written informed consent and the study protocol was approved by the Committee on Clinical Investigations at Beth Israel Deaconess Medical Center.
2.2. Migraine headaches
Participants completed both morning and evening diaries to report the presence of migraine headache since their prior diary completion. If a migraine headache was reported, participants were then asked to record the time of headache, whether the headache was ongoing, or whether the headache resolved. If the participants reported that the headache was resolved, additional questions were asked regarding the intensity, duration, use of migraine medication, associated symptoms, and similarities to their usual migraine headaches. A study physician reviewed the reported headaches after the study completion.
We considered headache onset reported within one calendar day of a prior headache’s resolution as a relapse. For a migraine headache that lasted for multiple days, the day of migraine headache onset was defined as the event day, whereas the days with continuing migraine headache and the day on which the migraine headache ended were considered as time with a prevalent headache and therefore the participants were not at risk of having a new headache begin during this time. The follow-up period for each participant was up to 2 months.
2.3. Weather and air pollution
We calculated daily averages of ambient temperature, relative humidity, and barometric pressure from hourly measures that were obtained from the Boston Logan Airport Weather Station. The data are publicly accessible at: https://www.ncdc.noaa.gov/cdo-web/datasets/LCD/stations/WBAN:14739/detail (Accessed on August 31, 2018). We obtained daily measures of air pollutants from U.S. Environment Protection Agency’s Air Quality System: daily mean fine particulate matter (PM2.5) was measured from Roxbury (Site ID: 250250042), North End (Site ID: 250250043), and Von Hillern (Site ID: 250250044) sites; daily maximum 1-hour SO2 was measured from Kenmore (Site ID: 250250002) and Roxbury sites; daily maximum 1-hour NO2 was measured from Kenmore, Roxbury, and Von Hillern sites; daily maximum 8-hour O3 was measured from Roxbury site; and daily maximum 8-hour CO was measured from Roxbury and Von Hillern sites. Data can be downloaded at: https://www.epa.gov/outdoor-air-quality-data/download-daily-data (Accessed on August 31, 2018).
2.4. Statistical methods
We calculated the 1-, 2-, and 3-day moving averages of the daily levels of weather conditions and air pollution levels. The 1-day moving average was defined as the daily average values of each exposure variable on the day of migraine headache onset. We evaluated the goodness-of-fit for non-linear models where weather conditions were modeled as natural cubic spline terms (anova() function), and did not find statistically significant deviation from linearity (all P>0.6). Therefore we modeled weather conditions as linear terms in the analyses.
We used fixed effects logistic regression model and examined the associations for each moving average of weather conditions and air pollutants separately, adjusting for day of week, a participant identifier, and seasonality by using a natural cubic spline function of day of the year (range: 1 to 366) with 4 degrees of freedom (ns() function in R). For analyses of air pollutants, we additionally adjusted for corresponding moving averages of temperature and relative humidity. This was because weather conditions may affect both measured levels of air pollutants and the risk of having migraine headache. Therefore, we considered weather as a potential upstream common cause of both air pollution and migraine headache.
For sensitivity analyses: 1) we applied logistic regression models with generalized estimating equation (GEE) and specified the autoregressive correlation structure to account for the potential correlations between nearby migraine headache onsets within each study participant; 2) we excluded the 2 calendar days after a migraine headache ended; 3) we used a two-exposure model by including both temperature and relative humidity in the same model; 4) we used a two-exposure model by including both NO2 and O3 in the same model; 5) we examined the associations for air pollutants by additionally adjusting for PM2.5 in the models; 6) we examined the associations for air pollutants without adjusting for temperature and relative humidity in the models; and 7) we examined whether the associations differ between warm season (April to September) and cold season (October to March) or differ between participants who reported weather change as a potential trigger of their migraine headache and those who did not by using interaction terms. Since we found positive associations between relative humidity and migraine headache onset, we conducted a post-hoc analysis and examined the associations for daily average precipitation.
Parameter estimates from the temperature analyses were scaled to a 10°F (5.6°C) increment. We also scaled the results for relative humidity (26.5%), barometric pressure (0.3 inHg), PM2.5 (3.6 μg/m3), NO2 (11.7 ppb), SO2 (0.6 ppb), O3 (14 ppb), and CO (150 ppb); these scale factors were selected to approximate the interquartile range of the daily measures. We then reported scaled odds ratios (ORs) and 95% confidence intervals (CIs). A two-tailed P<0.05 was used to determine the statistical significance when applicable. Main analyses were performed using the glm() function in R-3.5.3 (R Core Team 2019), and analyses with GEE were performed using the geeglm() function in the R package “geepack” (Højsgaard et al. 2005). Plots were generated using STATA 13.0 (StataCorp, College Station, TX).
3. Results
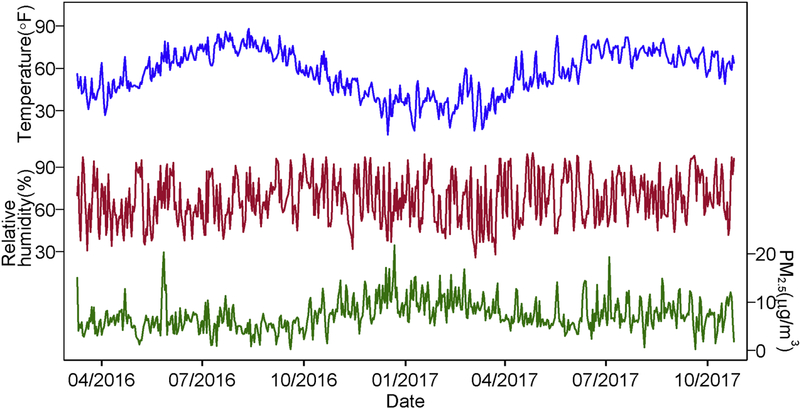
We enrolled 98 patients and collected data on a total of 4406 days, including 870 episodes of migraine headache. On average, participants reported 9 migraine headaches (range: 1 to 22). The mean age was 35 (standard deviation: 12) and 86 (88%) were women. 81 (83%) participants were white and 68 (79%) of the 86 female participants were premenopausal (Table 1). Characteristics of temperature, relative humidity, barometric pressure, and air pollutants are listed in Table 2. The daily mean temperature during the study period was 56.9°F (13.8°C) (standard deviation: 16.0°F (8.9°C)), and the mean PM2.5 levels during the period was 7.3 μg/m3 (standard deviation: 3.2 μg/m3). Figure 1 shows the levels of daily average temperature, relative humidity, and PM2.5 during the study period.
Table 1.
Characteristics of the Included 98 Participants With Migraine in the Greater Boston Area, Massachusetts, 2016–2017.
| N(%) or Mean (SD) | |
|---|---|
| Age, years | 35(12) |
| Women | 86 (88%) |
| Race, White | 81 (83%) |
| Ethnicity, Not Hispanic or Latino | 83 (86%) |
| Post-menopausala | 11 (13%) |
| Pre-menopausala | 68 (79%) |
| Current smoker | 2 (2%) |
| Former smoker | 13 (14%) |
| Report weather triggers migraine | 48 (49%) |
Abbreviation: SD, standard deviation.
Among 86 women.
Table 2.
Characteristics of Weather Factors and Air Pollutants in Greater Boston Area, Massachusetts, March, 2016-October, 2017.
| Mean (SD) | IQR | Pearson Correlation Coefficients |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Relative humidity | Pressure | PM2.5 | NO2 | SO2 | O3 | CO | |||
| Temperature, °F | 56.9 (16.0) | 26.0 | 0.06 | −0.15 | −0.25 | −0.27 | −0.13 | 0.40 | −0.13 |
| Relative humidity, % | 67.3 (16.7) | 26.5 | −0.09 | −0.15 | −0.03 | 0.01 | −0.39 | 0.05 | |
| Barometric pressure, inHg | 30.0 (0.2) | 0.3 | 0.16 | 0.19 | 0.19 | −0.06 | 0.12 | ||
| Fine particulate matter (PM2.5), μg/m3 | 7.3 (3.2) | 3.6 | 0.49 | 0.41 | 0.12 | 0.52 | |||
| Nitrogen dioxide (NO2), ppb | 24.5 (9.1) | 11.7 | 0.58 | −0.06 | 0.61 | ||||
| Sulfur dioxide (SO2)a, ppb | 0.9 (0.7) | 0.6 | −0.16 | 0.65 | |||||
| Ozone (O3)b, ppb | 33.7 (10.4) | 14.0 | −0.14 | ||||||
| Carbon monoxide (CO)c, ppb | 337.2 (122.2) | 150.0 | |||||||
Abbreviations: SD, standard deviation; IQR, interquartile range.
1 day missing.
6 days missing.
4 days missing.
Figure 1.
Characteristics of temperature, relative humidity, and fine particulate matter (PM2.5) in the Greater Boston area, Massachusetts, March, 2016-October, 2017.
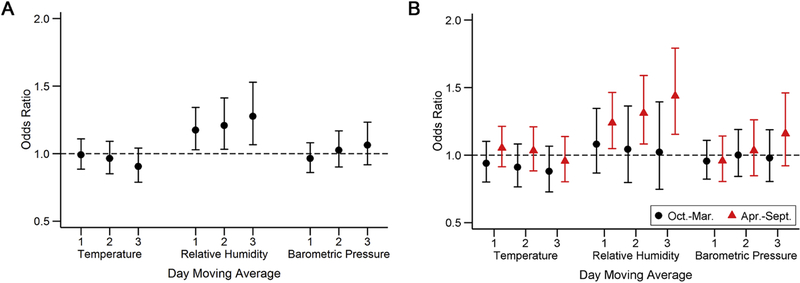
Higher relative humidity was associated with higher odds of migraine headache onset (Figure 2A). For example, a 26.5% increase in the 3-day moving average of relative humidity was associated with a 28% (95% confidence interval: 1.07, 1.53) higher odds of having a migraine headache onset. The associations of temperature or barometric pressure with migraine headache onset were generally null (Figure 2A). Furthermore, relative humidity and migraine headache onset appeared to be positive associated only in the warm season (Figure 2B).
Figure 2.
Associations of weather with migraine headaches overall (A) and by season (B) among participants with migraine in the Greater Boston area, Massachusetts, 2016–2017. Models were adjusted for day of week, a natural cubic spline function of day of year, and a participant identifier.
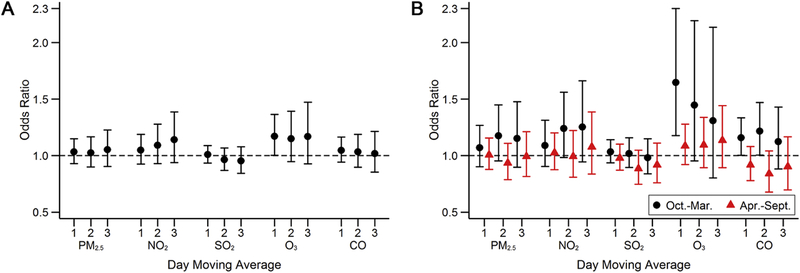
The associations between ambient air pollutants and migraine headache onset were also generally null, except for O3: a 14 ppb higher 1-day moving average of daily maximum 8-hour O3 was associated with higher odds of migraine headache onset (odds ratio=1.17, 95% confidence interval: 1.002, 1.36) (Figure 3A). For longer moving averages of O3, the associations appeared to be positive but the 95% confidence intervals crossed the null. The positive associations were also observed in cold seasons. Additionally, although the associations for NO2 and CO and were generally null in the main analyses, higher 2- and 3-day moving averages of daily maximum 1-hour NO2 and 1- and 2-day moving averages of daily maximum 8-hour CO were associated with higher odds of migraine headache onset in cold season (Figure 3B).
Figure 3.
Associations of ambient air pollutants with migraine headaches overall (A) and by season (B) among participants with migraine in the Greater Boston area, Massachusetts, 2016–2017. Models were adjusted for day of week, a natural cubic spline function of day of year, a participant identifier, temperature, and relative humidity.
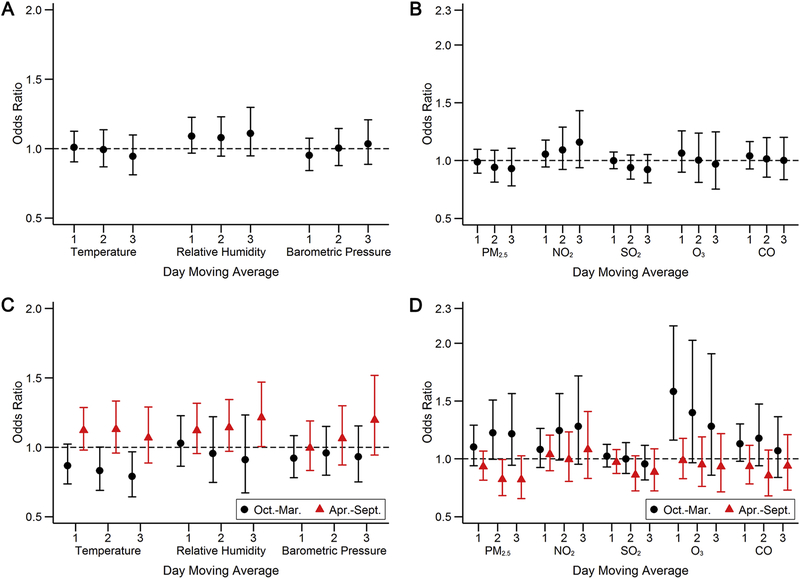
Using logistic regression models with GEE and autoregressive correlation structure led to attenuated results that were no longer statistically significant for relative humidity and O3. However, the observed differing associations by season remained (Figure 4). Adjusting for temperature and relative humidity in the same model, adjusting for NO2 and O3 in the same model, and adjusting for PM2.5 in the models for other pollutants did not alter our results substantially.
Figure 4.
Associations of weather and ambient air pollutants with migraine headaches overall (A and B) and by season (C and D) among participants with migraine in the Greater Boston area, Massachusetts, 2016–2017. We used logistic regression models with generalized estimating equation (GEE), and specified autoregressive correlation structure. Models were adjusted for day of week and a natural cubic spline function of day of year. Models for air pollution (B and D) were additionally adjusted for temperature and relative humidity.
Excluding the two calendar days after a migraine headache ended led to attenuated associations for relative humidity and NO2 (Supplemental Figure S1). Leaving temperature and relative humidity out of the models for air pollution led to attenuated results for O3 (Supplemental Figure S2). However, since we believe that weather conditions are likely confounders for the association between air pollution and migraine, the observed attenuated results without adjusting for temperature and relative humidity could be confounded. We did not find differing associations between participants who believed weather change is a trigger of their migraine headache and those did not (Supplemental Figure S3). And daily average precipitation was not associated with migraine headache onset (Supplemental Figure S4).
4. Discussion
In this prospective study of 98 migraine patients with 4406 days of data, we found that higher relative humidity and higher O3 were associated with higher odds of migraine headache onset. The associations for relative humidity were apparent during the warm season. And there appeared to be weak positive associations of higher daily maximum 1-hour NO2, daily maximum 8-hour O3, and daily maximum 8-hour CO with higher odds of migraine headache onset in the cold season. Although the associations for O3 and relative humidity were attenuated and no longer statistically significant in the overall GEE analysis, the differing associations by season remained. The current study is among the first studies in the U.S. that prospectively collected migraine headache data using daily electronic diaries to investigate and quantify these associations.
A large number of studies have been conducted to identify triggering factors of migraine, however, the majority relied on participants’ self-reported perception regarding potential triggers of migraine headaches (Pellegrino et al. 2018; Peroutka 2014). Several epidemiological studies objectively measured weather data and prospective collected migraine headache events by headache diary (Cull 1981; Gomersall and Stuart 1973; Hoffmann et al. 2011; Hoffmann et al. 2015; Osterman et al. 1981; Prince et al. 2004; Schulman et al. 1980; Yang et al. 2015; Zebenholzer et al. 2011): while earlier studies were limited by analytic methods (Cull 1981; Gomersall and Stuart 1973; Osterman et al. 1981; Schulman et al. 1980), studies in the past two decades generally agreed that a subgroup of patients with migraine are “weather sensitive” (Hoffmann et al. 2011; Hoffmann et al. 2015; Prince et al. 2004; Yang et al. 2015), usually by investigating the associations within each individual (Hoffmann et al. 2011; Hoffmann et al. 2015; Prince et al. 2004). To some extent, our findings for the temperature and relative humidity agreed with two of these previous studies that lower relative humidity were associated with lower risk of migraine headache attack (Hoffmann et al. 2011; Yang et al. 2015). However, the two previous studies did not conduct season-specific analyses and were conducted outside of the U.S. (Hoffmann et al. 2011; Yang et al. 2015).
The observed generally null associations for barometric pressure with migraine headache onset also agreed with the majority of previous studies (Gomersall and Stuart 1973; Hoffmann et al. 2011; Mukamal et al. 2009; Osterman et al. 1981; Schulman et al. 1980; Villeneuve et al. 2006; Wilkinson and Woodrow 1979; Yilmaz et al. 2015). One earlier study found a smaller number of migraine attacks in days with lower barometric pressure (Cull 1981), one recent study found inconsistent directions of the association among 4 of the 13 identified “weather sensitive” participants by using an individual-wise approach (Hoffmann et al. 2015), and in a prospective diary-based study, Zebenholzer et al. found an association between a ridge of high pressure and headache attacks but not with migraine (Zebenholzer et al. 2011). Overall, the association between barometric pressure and migraine headache was not well-supported by the previous studies.
In a large-scale study conducted in Israel, Yilmaz et al. found that higher daily relative humidity was associated with a lower number of visits to the emergency department among 3491 patients (Yilmaz et al. 2015), whereas two other large case-crossover studies in the U.S. and Canada found generally null associations (Mukamal et al. 2009; Villeneuve et al. 2006). Higher daily temperature has also been associated with higher number of emergency department visits in previous larger-scale studies (Mukamal et al. 2009; Vodonos et al. 2015; Yilmaz et al. 2015). In the current study, we found associations of higher daily relative humidity with higher odds of migraine onset. One possible explanation for the discrepancy between the current study and these previous studies is that diary and emergency department visits records are likely measures of migraine headaches with different characteristics. For example, patients may only visit emergency departments for more severe or long-lasting headaches, or if they lack access to routine healthcare or medications. Moreover, it is usually difficult to verify whether there were headaches in days that the patients did not visit the hospitals or clinics.
A number of recent studies examined the associations between ambient air pollutants and number of visits to emergency departments or clinics and have found generally positive associations (Chen et al. 2015; Chiu and Yang 2015; Dales et al. 2009; Lee et al. 2018; Szyszkowicz 2008; Szyszkowicz and Porada 2012; Szyszkowicz et al. 2009; Vodonos et al. 2015). However, we found generally null association for air pollutants with migraine headache onset in the current study, consistent with a previous large-scale study in our region (Mukamal et al. 2009). Moreover, we found some weak evidence that suggested positive associations of NO2, O3, and CO with migraine headache onset in cold season, which is to some extent consistent with a few previous studies (Chiu and Yang 2015; Dales et al. 2009; Szyszkowicz 2008; Vodonos et al. 2015). Since NO2, O3, and CO are related to traffic emissions, our finding may indicate potential associations between traffic-related pollutants and migraine headache onset. The current study was conducted in a region where the air pollution level is in compliance with the current U.S. National Ambient Air Quality Standards. Moreover, the air pollution levels in the current study are generally lower than previous studies except NO2 and O3 (Chen et al. 2015; Chiu et al. 2015; Dales et al. 2009; Szyszkowicz 2008; Szyszkowicz et al. 2009; Vodonos et al. 2015).
In the GEE analysis, the observed associations for O3 and relative humidity were attenuated and no longer statistically significant, however, we still observed differing associations by season. While it is possible that the attenuation was due to better control for the correlation structure in the data in the GEE model, another possible reason for the discrepancy could be better control of confounding in the fixed effects model. Furthermore, it is important to note that the GEE analysis estimates “population-averaged effect” while the fixed effects model estimates “subject-specific effect”, which more directly addresses the hypothesis in this study.
Our study has a few limitations. First, the current study enrolled only 98 patients with episodic migraine. The air pollution levels in the study regions was generally low and there were relatively small variations in exposure levels during the follow-up for each participant. Second, the study participants were predominantly women with European ancestry, which may limit the generalizability of our findings to other study samples. Third, weather conditions were measured at one fixed station and air pollution levels were measured at several local fixed stations, which may induce non-differential measurement errors that may have attenuated the statistical power.
There are also strengths. First, we used fixed effect models that accounted for participants’ time-invariant conditions during the relatively short follow-up period, such as age, sex, and socioeconomic position. We conducted sensitivity analyses using logistic regression models with GEE and specified autoregressive correlation structure to account for potential correlations between headache onsets that were close to each other. Second, we conducted several sensitivity analyses to demonstrate the robustness of our findings. Third, the weather conditions and air pollution levels were measured by National Oceanic and Atmospheric Administration (NOAA) and U.S. Environmental Protection Agency (EPA), independent of ascertainment of migraine headache onset. It is also unlikely that the participants recorded their migraine headache onset based on the weather conditions or air pollution levels.
5. Conclusions
Our findings suggest an association between higher relative humidity and onset of migraine headache, especially in the warm season; and higher levels of ambient O3 may be associated with higher risk of having migraine, particularly in cold season. Weak positive associations were also found for other traffic-related air pollutants in cold season. Although the associations for O3 and relative humidity were not observed in the overall GEE analysis, the differing associations by season remained. Future larger-scale studies with headache diaries and longer follow-up time are warranted to confirm or refute our findings.
Supplementary Material
Highlights:
Migraine is a common recurrent headache disorder affecting 14% American adults
Weather and air pollution are often reported as precipitating factors by patients
We prospectively collected migraine headache data using daily electronic diaries
Relative humidity is associated with migraine headache onset in warm season
Traffic-related pollutants are associated with migraine headache onset in cold season
Acknowledgements
Funding: This work was supported by American Sleep Medicine Foundation, the National Institute of Health grant 1R21NS091627–01A1, and Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Declarations of interest: Dr.Bertisch have received/receive research funding from Merck, Apnimed, and Lockheed Martin (DARPA is primary funder).
Abbreviation:
- CO
carbon monoxide
- NO2
nitrogen dioxide
- O3
ozone
- PM2.5
fine particulate matter
- SO2
sulfur dioxide
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andress-Rothrock D; King W; Rothrock J An analysis of migraine triggers in a clinic-based population. Headache 2010;50:1366–1370. 10.1111/j.1526-4610.2010.01753.x [DOI] [PubMed] [Google Scholar]
- Burch RC; Loder S; Loder E; Smitherman TA The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache 2015;55:21–34. 10.1111/head.12482 [DOI] [PubMed] [Google Scholar]
- Chen CC; Tsai SS; Yang CY Association between Fine Particulate Air Pollution and Daily Clinic Visits for Migraine in a Subtropical City: Taipei, Taiwan. Int J Environ Res Public Health 2015;12:4697–4708. 10.3390/ijerph120504697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu HF; Weng YH; Chiu YW; Yang CY Air pollution and daily clinic visits for headache in a subtropical city: Taipei, Taiwan. Int J Environ Res Public Health 2015;12:2277–2288. 10.3390/ijerph120202277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu HF; Yang CY Air pollution and daily clinic visits for migraine in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A 2015;78:549–558. 10.1080/15287394.2015.983218 [DOI] [PubMed] [Google Scholar]
- Cull RE Barometric pressure and other factors in migraine. Headache 1981;21:102–103. 10.1111/j.1526-4610.1981.hed2103102.x [DOI] [PubMed] [Google Scholar]
- Dales RE; Cakmak S; Vidal CB Air pollution and hospitalization for headache in Chile. Am J Epidemiol 2009;170:1057–1066. 10.1093/aje/kwp217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2018;17:954–976. 10.1016/S1474-4422(18)30322-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomersall JD; Stuart A Variations in migraine attacks with changes in weather conditions. International Journal of Biometeorology 1973;17:285–299. 10.1007/bf01804622 [DOI] [PubMed] [Google Scholar]
- Harris PA; Taylor R; Thielke R; Payne J; Gonzalez N; Conde JG Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann J; Lo H; Neeb L; Martus P; Reuter U Weather sensitivity in migraineurs. J Neurol 2011;258:596–602. 10.1007/s00415-010-5798-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann J; Schirra T; Lo H; Neeb L; Reuter U; Martus P The influence of weather on migraine - are migraine attacks predictable? Ann Clin Transl Neurol 2015;2:22–28. 10.1002/acn3.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Højsgaard S; Halekoh U; Yan J The R Package geepack for Generalized Estimating Equations 2005 2005;15:11 10.18637/jss.v015.i02 [DOI] [Google Scholar]
- International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia; 2018;38:1–211. 10.1177/0333102417738202 [DOI] [PubMed] [Google Scholar]
- Lee H; Myung W; Cheong HK; Yi SM; Hong YC; Cho SI; Kim H Ambient air pollution exposure and risk of migraine: Synergistic effect with high temperature. Environ Int 2018;121:383–391. 10.1016/j.envint.2018.09.022 [DOI] [PubMed] [Google Scholar]
- Messali A; Sanderson JC; Blumenfeld AM; Goadsby PJ; Buse DC; Varon SF; Stokes M; Lipton RB Direct and Indirect Costs of Chronic and Episodic Migraine in the United States: A Web-Based Survey. Headache 2016;56:306–322. 10.1111/head.12755 [DOI] [PubMed] [Google Scholar]
- Mukamal KJ; Wellenius GA; Suh HH; Mittleman MA Weather and air pollution as triggers of severe headaches. Neurology 2009;72:922–927. 10.1212/01.wnl.0000344152.56020.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterman PO; Lovstrand KG; Lundberg PO; Lundquist S; Muhr C Weekly headache periodicity and the effect of weather changes on headache. Int J Biometeorol 1981;25:39–45. 10.1007/bf02184436 [DOI] [PubMed] [Google Scholar]
- Pellegrino ABW; Davis-Martin RE; Houle TT; Turner DP; Smitherman TA Perceived triggers of primary headache disorders: A meta-analysis. Cephalalgia 2018;38:1188–1198. 10.1177/0333102417727535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peroutka SJ What turns on a migraine? A systematic review of migraine precipitating factors. Curr Pain Headache Rep 2014;18:454 10.1007/s11916-014-0454-z [DOI] [PubMed] [Google Scholar]
- Prince PB; Rapoport AM; Sheftell FD; Tepper SJ; Bigal ME The effect of weather on headache. Headache 2004;44:596–602. 10.1111/j.1526-4610.2004.446008.x [DOI] [PubMed] [Google Scholar]
- Schulman J; Leviton A; Slack W; Porter D; Graham JR The relationship of headache occurrence to barometric pressure. Int J Biometeorol 1980;24:263–269. 10.1007/bf02249796 [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M Ambient air pollution and daily emergency department visits for headache in Ottawa, Canada. Headache 2008;48:1076–1081. 10.1111/j.1526-4610.2007.01039.x [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M; Porada E Ambient Sulphur Dioxide and Female ED Visits for Migraine. ISRN Neurol 2012;2012:279051 10.5402/2012/279051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyszkowicz M; Stieb DM; Rowe BH Air pollution and daily ED visits for migraine and headache in Edmonton, Canada. Am J Emerg Med 2009;27:391–396. 10.1016/j.ajem.2008.03.013 [DOI] [PubMed] [Google Scholar]
- Villeneuve PJ; Szyszkowicz M; Stieb D; Bourque DA Weather and emergency room visits for migraine headaches in Ottawa, Canada. Headache 2006;46:64–72. 10.1111/j.1526-4610.2006.00322.x [DOI] [PubMed] [Google Scholar]
- Vodonos A; Novack V; Zlotnik Y; Ifergane G Ambient air pollution, weather and daily emergency department visits for headache. Cephalalgia 2015;35:1085–1091. 10.1177/0333102415570300 [DOI] [PubMed] [Google Scholar]
- Wilkinson M; Woodrow J Migraine and weather. Headache 1979;19:375–378. 10.1111/j.1526-4610.1979.hed1907375.x [DOI] [PubMed] [Google Scholar]
- Yang AC; Fuh JL; Huang NE; Shia BC; Wang SJ Patients with migraine are right about their perception of temperature as a trigger: time series analysis of headache diary data. J Headache Pain 2015;16:533 10.1186/s10194-015-0533-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz M; Gurger M; Atescelik M; Yildiz M; Gurbuz S Meteorologic parameters and migraine headache: ED study. Am J Emerg Med 2015;33:409–413. 10.1016/j.ajem.2014.12.056 [DOI] [PubMed] [Google Scholar]
- Zebenholzer K; Rudel E; Frantal S; Brannath W; Schmidt K; Wober-Bingol C; Wober C Migraine and weather: a prospective diary-based analysis. Cephalalgia 2011;31:391–400. 10.1177/0333102410385580 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.