Abstract
Background
In a previous randomised controlled trial (RCT) in hospital healthcare workers (HCWs), cloth masks resulted in a higher risk of respiratory infections compared with medical masks. This was the only published RCT of cloth masks at the time of the COVID-19 pandemic.
Objective
To do a post hoc analysis of unpublished data on mask washing and mask contamination from the original RCT to further understand poor performance of the two-layered cotton cloth mask used by HCWs in that RCT.
Setting
14 secondary-level/tertiary-level hospitals in Hanoi, Vietnam.
Participants
A subgroup of 607 HCWs aged ≥18 years working full time in selected high-risk wards, who used a two-layered cloth mask and were part of a randomised controlled clinical trial comparing medical masks and cloth masks.
Intervention
Washing method for cloth masks (self-washing or hospital laundry). A substudy of contamination of a sample of 15 cloth and medical masks was also conducted.
Outcome measure
Infection rate over 4 weeks of follow up and viral contamination of masks tested by multiplex PCR.
Results
Viral contamination with rhinovirus was identified on both used medical and cloth masks. Most HCW (77% of daily washing) self-washed their masks by hand. The risk of infection was more than double among HCW self-washing their masks compared with the hospital laundry (HR 2.04 (95% CI 1.03 to 4.00); p=0.04). There was no significant difference in infection between HCW who wore cloth masks washed in the hospital laundry compared with medical masks (p=0.5).
Conclusions
Using self-reported method of washing, we showed double the risk of infection with seasonal respiratory viruses if masks were self-washed by hand by HCWs. The majority of HCWs in the study reported hand-washing their mask themselves. This could explain the poor performance of two layered cloth masks, if the self-washing was inadequate. Cloth masks washed in the hospital laundry were as protective as medical masks. Both cloth and medical masks were contaminated, but only cloth masks were reused in the study, reiterating the importance of daily washing of reusable cloth masks using proper method. A well-washed cloth mask can be as protective as a medical mask.
Trial resgistration number
ACTRN12610000887077.
Keywords: infectious diseases, infection control, respiratory infections
Strengths and limitations of this study.
Unpublished data on washing and contamination of the cloth masks was available for post hoc analysis of an original published randomised controlled trial (RCT), which allowed further understanding of reasons for the poor performance of cloth masks in the RCT.
The method and frequency of washing of cloth masks was self-reported by health workers, which could be subject to recall bias or misreporting.
The contamination study showed contamination of both medical and cloth masks but had a small sample.
The data are specific for the two-layered cloth mask used in the study and do not preclude better protection from a well-designed cloth mask that is washed daily.
Introduction
Global shortages of masks and respirators have resulted in agencies such as the US Centers for Disease Control recommending cloth masks for healthcare workers (HCWs) when disposable masks or respirators are not available.1 We conducted the only randomised controlled clinical trial (RCT) of cloth face masks available at the time of the COVID-19 pandemic, published in 2015.2 This RCT showed that cloth masks resulted in a higher risk of infection than medical masks and also higher than the control arm. The rate of infection in the cloth mask arm was 1.67 times higher for laboratory confirmed viral illness and 13 times higher for clinical influenza-like illness.2 In testing for water resistance, we also showed almost complete penetration of the cloth masks by sodium chloride droplets, more than double the penetration of medical masks. During the COVID-19 pandemic, where no medical grade mask was available, this RCT has raised concern about the safety of cloth masks as an alternative for HCWs.
In the RCT, over 90% of participants reported washing their masks daily.2 On average, HCWs worked most days during the 4-week trial period and reported washing their cloth masks on 92% of all days. They reported self-washing (80%), combined self-washing and hospital laundry (16%) and only hospital laundry (4%) as their method of washing.
We postulated that the poor performance of cloth masks may be due the design of the mask, which was a two-layered cotton mask manufactured in Vietnam, and possibly due to inadequate washing.2 It was also possible that different distribution of cloth masks versus medical masks by ward type may have caused an apparently higher rate of infection in cloth mask users. Given the urgency around the safety of cloth masks and the controversy caused by the results of our RCT, we analysed unpublished data on cleaning of the cloth masks and ward allocation from the 2015 trial, as well as unpublished data from a substudy on viral contamination of cloth and medical masks.
Aims
To determine the relationship of washing of masks to infection risk in cloth mask users. The secondary aim was to determine contamination with viral pathogens on the surface of cloth and medical masks.
Methods
We selected all subjects who wore a cloth mask from the published RCT of cloth masks versus medical masks,2 which included subjects allocated to the cloth mask arm (n=569) as well as anyone in the control arm wearing only a cloth mask (38/458). This provided 607 subjects for further analysis of infection risk by washing and cleaning of cloth masks. The cloth mask used in the study was manufactured locally in Vietnam and widely used in the secondary hospitals and also in tertiary hospitals (see figure 1). The cloth mask studied was made of cotton and cotton blend fabric with two layers (inner and outer layer), without a filter layer and with four strings in four corners of the mask as pictured in figure 1. HCWs were provided five masks and asked to wash their mask daily and use a clean one each day. They could hand-wash the masks themselves in the hospital with soap and tap water and hang them out to dry in a space provided for HCWs (figure 1), or they could get the masks laundered in the hospital laundry in an automatic washing machine with detergent and hot water, if available in their hospital. They were provided written instructions on washing the mask themselves and self-reported their washing practices daily. They reused the masks after self-washing or using the hospital laundry system. The study was an epidemiological analysis of unpublished data on contamination and washing of cloth masks, collected during the original RCT. We also looked at the distribution of HCWs by ward type to see if there was any difference between the cloth and medical mask groups that could explain the higher rate of infection in the cloth mask group.
Figure 1.

Cloth mask used in the study.
The outcome of interest was infection, using a composite outcome variable measured in the study (clinical respiratory illness, influenza-like illness and laboratory confirmation of one or multiple respiratory viruses).2 In the study, 85% (58/68 positive RT-PCR tests) were for rhinovirus.2
The data on the method of washing (self-washing or hospital laundry) as well as daily diary data on frequency of washing were analysed. Self-reported daily cleaning data from daily diary cards were analysed, as participants may have varied the cleaning frequency and type by day over the 4-week follow-up period. Person-days of mask washing were used as denominator data for analysis. Follow-up data were censored when infection occurred. We compared cloth masks that were self-washed by hand, with cloth masks that were washed in the hospital laundry and medical masks. Data on ward type (intensive care, infectious diseases, paediatrics, cancer and haematology, emergency and other) cleaning method and frequency of cleaning were analysed against infection risk.
Statistical analysis
To determine the association, we adopted a survival analysis technique with time-varying covariates. The data were arranged in ‘counting process format’,3 where for each participant there were same number of records as the number of days of follow-up. The outcome and study factor (mask cleaning) were assessed daily as binary variables. We generated Kaplan-Meier survival plots to compare the survival experience by mask cleaning practices and fitted the Cox proportional hazards model to estimate the hazard ratios (HRs). We also examined infection rate by type of ward using a Pearson’s χ2 test.
Substudy of contamination of masks
A total of 117 masks samples were collected: 102 from subjects with clinical respiratory illness in participating hospitals and 15 from a substudy as described further. All participants at this time also had a swab of their nose and throat collected for lab testing.
For the substudy of mask contamination, 15 mask samples were collected from two purposively selected wards in Thanh Nhan General Hospital (a city hospital in Hanoi) between 28 March and 8 April 2011. Intervention arms were cluster randomised by ward, so staff on each ward used the same type of mask. Nine participants were randomly selected from the cloth mask group (intensive care unit (ICU)), and six were randomly selected from medical masks group (paediatric ward). In the cloth mask group, three participants were given five clean cloth mask per person, along with daily washing instructions, and masks were collected after 1 month. Three participants were requested to provide their cloth masks for testing after use. The remaining three participants were asked to provide their cloth masks that they used for previous 4 weeks.
In the medical mask group, three randomly selected participants were given one new medical mask per person in the morning by the study team, and the masks were collected the same day after 1 hour of use. The remaining three participants were given one new medical mask per person in the morning by the survey team, and the masks were collected after 4 hours of use.
Mask testing
The mask testing method is shown in figure 2. Mask samples were collected after use by HCWs. They were folded in double vertically. They were cut at the central part of the mask into 3×5 cm rectangles and separated into different layers: three layers for medical masks and two with cloth masks. Masks were cut and placed in a tube (as described in figure 2) and sent to the lab for testing as described in the original study.2 Each layer was put into different viral transport medium (VTM) tube and labelled, using a sterilised bamboo stick to push the layer deep into the media. Testing was performed using both normal and concentrated samples. A multiplex respiratory viral RT-PCR test was done for SVA/B, influenza A/H3N2, A/H1N1 and B viruses, and hMPV (reaction mix 1); parainfluenza viruses 1–4 (reaction mix 2); rhinoviruses, influenza C virus, SARS-CoV (reaction mix 3); coronaviruses OC43, 229E, NL63 and HKU1 (reaction mix 4); and adenoviruses and hBoV (reaction mix 5), as described in the original trial.2
Figure 2.
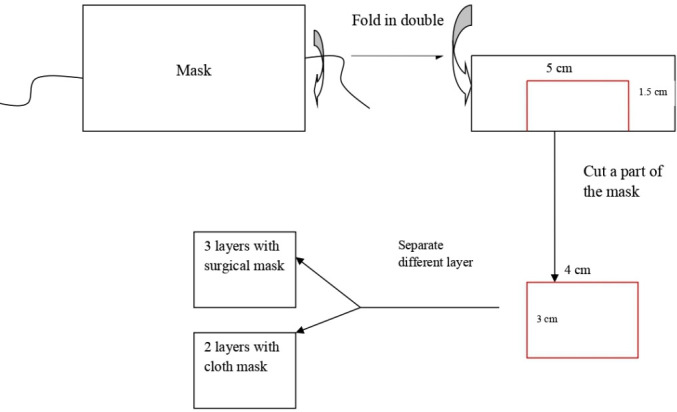
Mask testing.
Patient and public involvement
There was no patient or public involvement.
Results
There were 607 subjects with 9253 person-days of follow-up who wore a cloth mask during the study. The highest rates of infection among cloth mask users was in the emergency department (ED) (12%) and ICU (10%). There was a similar distribution of participants between the ward types, in the medical mask and cloth mask arms with 138 medical mask users and 180 cloth mask users in ICU; and 163 medical mask users and 143 cloth mask users in the ED.
We also compared the infection rate of ICU and ED combined with other wards (paediatrics, infectious diseases, internal medicine and others). In the ICU and ED wards, there were 36 (11.2%) infections among 323 cloth mask users and in all other wards there were 16 (5.6%) infections among 284 subjects. This difference was statistically significant (p=0.015). There was no significant difference in infection rate between any ward types for medical masks, which was 5.33% overall (range 3.8%–6.9%). In ICU, medical masks had 8/138 (5.8%) infections, while in ED, medical masks had 7/163 (4.2%) infections.
The most common method of cleaning each day was self-washing by hand (77%,) followed by hospital laundry (13%). Some HCWs used both methods at different times. Over 90% (8396/9253 person-day observations) reported washing their mask daily. Only 15 subjects reported cleaning their mask <50% of the time over the 4 weeks of follow-up. There were 7091/9253 person-days of self-washing reported and 1177/9253 person-days of hospital laundry washing. Rates of infection among HCWs who self-washed their cloth masks by hand and who used the hospital laundry were 2/100 person days (110/5417 person days) and 0.85 per 100 person days (9/1052 person days), respectively. The rate of infection among HCWs who wore a medical mask was 0.85 per 100 person days (139/16 284 person days). The risk of infection was just over double for HCWs who self-washed their cloth masks by hand compared with using the hospital laundry. The HR of infection for self-washing was 2.04 (95% CI 1.03 to 4.00); p=0.04.
There was no significant difference in infection rate between cloth masks washed in the hospital laundry and medical masks (p=0.5). Figure 3 shows that hospital laundry was superior to self-washing in the survival analysis.
Figure 3.
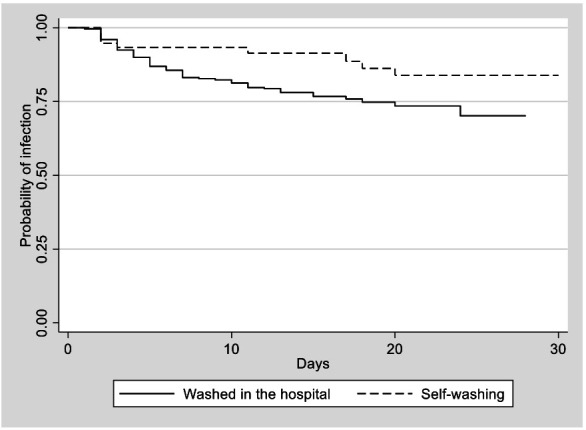
Survival analysis of infection by mask washing location (hospital laundry vs self-washing).
Mask testing results
In standard testing, 2% (2/117) of masks samples were positive for virus. Rhinoviruses were isolated from the internal layer and external layers respectively of one medical mask sample each.
In concentrated testing, around 4% (4/117) mask samples were positive—two medical masks and two cloth masks. Rhinoviruses were isolated from internal and external layers of two medical masks and only the internal layer of two cloth mask samples. Paired nose and throat swabs of these same subjects were also positive for rhinoviruses.
Discussion
HCWs whose cloth masks were laundered in the hospital laundry were protected as well as those who wore disposable medical masks, highlighting that a cloth mask can be protective if well washed. However, HCWs who self-washed their masks in the hospital by hand had double the risk of infection than those who used the hospital laundry. Self-washing was by far the most common method of washing (77% of cloth mask users), which could explain the poor performance of cloth masks in the intention-to-treat analysis in the original RCT and reiterates the importance of daily washing of these products.2
While the majority of participants reported washing their mask daily, it appears that the hand washing was not adequate or that a proportion who reported daily washing did not actually do so every day. Hand washing in the hospital is usually done in the available wash basins, some of which do not have hot water, which may reduce the effectiveness of washing. This may have been an important factor in the poor performance of cloth masks in those who self-washed. The WHO recommends machine washing with warm water at 60–90°C and laundry detergent.4
We showed that both cloth and medical mask can become contaminated. There was no difference in contamination between medical and cloth masks; however, the sample size was very small. The majority of participants in the trial who had a confirmed viral infection had rhinovirus, and this was the only virus identified on mask samples, on both the inner and outer layers in medical masks and on the inner layer of cloth masks. More research is needed to quantify longitudinal contamination of unwashed cloth masks over time and by usage frequency.
On a practical level, the difference in clinical outcomes in the trial may be explained by the fact the medical mask users received a new mask daily, whereas cloth mask users received five masks to wash and reuse. The principle of a reusable cloth mask is that a user has at least two masks so they can be washed daily to ensure a clean mask each day. However, for medical mask users the simple fact of being provided a clean mask daily may be a key factor in reducing risk of infection, whereas busy health workers may forget to wash a cloth mask daily or wash them inadequately, as it is an added burden on their workload. We do not recommend cloth masks for health workers, but if used as a last resort where no other options are available, health facilities should provide clean masks daily to health workers and also launder them in the hospital laundry. Placing the burden of cleaning on an HCW may increase the risk of unsafe use and infection. If laundry facilities are not available, using steam sterilisation may be a safer alternative to hand washing.5
A meta-analysis of mask use for severe acute respiratory syndrome, SARS-CoV-2 and Middle East respiratory syndrome coronavirus showed that masks were 85% protective and that a 12-layered cloth mask is as protective as a medical mask.6 There are no data on other combinations of layers, except that single-layered masks are not protective.6 Our original RCT suggests that even a two-layered cotton and cotton blend mask is not protective.2 However, this does not preclude more protective cloth mask designs, especially if washing is done daily according to WHO recommendations.4
Cotton is not a suitable fabric for the outer layer of a mask, as it is absorbent, can become damp and pose a risk of contamination if not washed daily or if washed inadequately.7 The principles of a safer cloth mask would include at least three layers, water-resistant fabric for the outer layer, fine weave, high thread count, fit around the face and ties instead of ear loops, which the latter has been reported to reduce fit.8 They should also be washed daily in soap and water, and the design should allow frequent washing without compromising the design features. The WHO changed its recommendation on community mask use in June 2020 and provided guidance on optimal design of a cloth mask.9
The distribution of trial participants between ward types was similar, so this did not contribute to the poor performance of cloth masks. Furthermore, infection rates were not significantly different by ward type for medical masks—only for cloth masks, which had a significantly higher infection risk for ICU and emergency wards. ICU and emergency wards are recognised as high-risk, high-transmission settings, with documented aerosolised viruses such as influenza and COVID-19,10–12 so a cloth mask may not be adequate in these wards.
We conclude that two-layered cotton masks as used in the original RCT are not a safe option for HCWs if they are held responsible for their own washing, especially in ICU or emergency wards. A respirator provides 96% protection for health workers, compared with 67% with a medical mask,6 and should be the standard for health workers treating patients with COVID-19.13 This does not preclude the use of well-designed cloth masks in the community, as there has been unprecedented efforts in development and research into novel reusable cloth masks during the pandemic.6 However, countries should take responsibility for scaling up manufacturing of medical masks and respirators for health workers, instead of forcing them to work in suboptimal personal protective equipment.14
In summary, the poor performance of cloth masks in our RCT may reflect inadequate washing. Daily washing of cloth masks at the recommended temperature of 60°C–90°C in whatever setting they are used, including the community, is essential for safety. Reports of self-washing may have overestimated the frequency of washing, and there may have been variability in the quality of washing. The additional burden of being responsible for cleaning of a mask for busy HCWs in the midst of a pandemic may compromise safety, if workers forget to wash the mask. Removing this responsibility from HCWs and minimising the burden on them for their own protection by providing daily clean masks is the safest option in hospitals. If cloth masks are used, cleaning in the hospital laundry and daily provision of clean masks is safer than self-washing. The data from our RCT are specific to a two-layered cotton mask and cannot be generalised to all cloth masks. The trial was conducted in 2011, at a time when cloth masks were not well researched and not even mentioned in PPE guidelines despite being used widely in Asia. As a result of the COVID-19 pandemic, unprecedented research on cloth mask design is being conducted, which will result in better designs. Well-designed cloth masks may provide protection in the community,5 8 15 but design is only one aspect of the safety and effectiveness of a cloth mask. Daily washing as recommended by the WHO is also necessary. This study shows that a well-washed cloth mask is as protective as a medical mask.
Supplementary Material
Acknowledgments
We would like to acknowledge the participating hospitals and staff in Hanoi, Vietnam.
Footnotes
Twitter: @hollyseale
Contributors: CRM conceived, designed study, developed data analysis plan and wrote the manuscript. BR and AAC analysed the data and wrote and reviewed the manuscript. TCD reviewed original data and reviewed and wrote the manuscript. HS reviewed the analysis and wrote the manuscript.
Funding: CRM is supported by a National Health and Medical Research Council (NHMRC) Principal Research Fellowship, grant number 1 137 582. The original randomised controlled trial (RCT) was funded by the Australian Research Council.
Competing interests: TCD works for the Vietnam Ministry of Health.
Patient consent for publication: Not required.
Ethics approval: Ethics approval for the study was granted by National Institute for Hygiene and Epidemiology (NIHE), Vietnam (approval number 05 IRB) and the Human Research Ethics Committee of the University of New South Wales (UNSW), Australia (HREC approval number 10306).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available. The data are not available for sharing under the conditions of ethics approval from Vietnam.
References
- 1.Centers for Disease Control and Prevention Strategies for optimizing the supply of Facemasks. USA: CDC, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html [Google Scholar]
- 2.MacIntyre CR, Seale H, Dung TC, et al. . A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open 2015;5:e006577 10.1136/bmjopen-2014-006577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kleinbaum DGK. Survival Analysis : Mitchell GS JM, Statistics for biology and health. Switzerland: Springer, 2012: 1431–8776. https://www.springer.com/gp/book/9781441966452 [Google Scholar]
- 4.World Health Organization Water, sanitation, hygiene, and waste management for the COVID-19 virus: interim guidance, 2020. Available: https://www.who.int/publications/i/item/water-sanitation-hygiene-and-waste-management-for-covid-19
- 5.Ma Q-X SH, Zhang C-M, Zhang H-L, et al. . Decontamination of face masks with steam for mask reuse in fighting the pandemic COVID-19: experimental supports. J Med Virol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu DK, Akl EA, Duda S, et al. . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet 2020;395:1973–87. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chughtai AA, Seale H, Macintyre CR. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis 2020;26:eid2610.200948. 10.3201/eid2610.200948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacIntyre CRC, Dung A, Seale HS. Covid-19: should cloth masks be used by healthcare workers as a last resort?BMJ, 2020. Available: https://blogs.bmj.com/bmj/2020/04/09/covid-19-should-cloth-masks-be-used-byhealthcare-workers-as-a-last-resort/
- 9.World Health Organization Coronavirus disease (COVID-19) advice for the public: when and how to use masks. Geneva, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks [Google Scholar]
- 10.Blachere FM, Lindsley WG, Pearce TA, et al. . Measurement of airborne influenza virus in a hospital emergency department. Clinical Infectious Diseases 2009;48:438–40. 10.1086/596478 [DOI] [PubMed] [Google Scholar]
- 11.Santarpia JL, Rivera DN, Herrera V, et al. . "Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center.". medRxiv 2020;2020. [Google Scholar]
- 12.Guo ZDW, Zhang SF. (2020). "Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China. Emerg Infect Dis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacIntyre CR, Wang Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. The Lancet 2020;395:1950–1. 10.1016/S0140-6736(20)31183-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T, Schmid MB, Czypionka T, et al. . Face masks for the public during the covid-19 crisis. BMJ 2020;369:m1435. 10.1136/bmj.m1435 [DOI] [PubMed] [Google Scholar]
- 15.Bhattacharjee S, Bahl P, Chughtai AA, et al. . Last-resort strategies during mask shortages: optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic. BMJ Open Respir Res 2020;7:e000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


