Abstract
Pneumatic otoscopy is the recommended diagnostic method for middle ear infections. Physicians use a pneumatic otoscope to assess the position of the eardrum (bulging or retraction) as well as the eardrum mobility while an insufflation bulb is squeezed to generate air pressure changes in a sealed ear canal. While pneumatic otoscopy provides increased sensitivity and specificity by detecting decreased eardrum mobility, there exist many challenges to correctly perform and interpret results. For example, the ear canal must be sealed using a specialized ear speculum to deliver sufficiently large pressure changes that can induce visible movements of an eardrum. To overcome this challenge, video motion magnification is proposed to amplify pneumatic-induced motions of the eardrum without sealing of the ear canal. Pneumatic otoscopy is performed on adult subjects using a smartphone camera with an otoscope attachment at 60 frames per second, with pressure inputs at 5 Hz. Phase-based Eulerian motion magnification is applied to magnify spatiotemporal dependent motions in the video. As a result, the motion magnification of unsealed pneumatic otoscopy reveals comparable eardrum motions as in standard pneumatic otoscopy with a sealed ear canal. Furthermore, the estimated motions (in pixels) are quantified to examine the spatial and the temporal variations of the eardrum motions. The motion magnification may avoid the need for sealing the ear canal as well as decrease patient discomfort in pneumatic otoscopy, improving the capability and the usability as a point-of-care diagnostic tool in primary care and otology.
Keywords: Pneumatic otoscopy, eardrum mobility, motion magnification, video processing, middle ear infection
1. Introduction
A middle ear infection, or otitis media, is a leading cause of primary care visits worldwide during childhood. Middle ear infections occur when an inflammation is established within the middle ear, primarily due to bacterial or viral pathogens 1. More than 80% of children before the age of 4 have at least one episode 2, and its financial burden remains substantial, estimated to be around $5 billion 3,4. A middle ear infection is clinically characterized by the presence of accumulated middle ear fluid, known as a middle ear effusion (MEE), in a normally air-filled middle ear cavity. Persistent MEEs may lead to conductive hearing loss and developmental delays, as the eardrum vibrations will not effectively be transmitted to the inner ear.
Clinical diagnosis of middle ear infections can be difficult due to the anatomical location of middle ear. In order to establish a diagnosis, physicians must identify the presence of a MEE, located behind the eardrum. The standard method to diagnose middle ear infections is to use an otoscope, a tool that provides a magnified surface view of the eardrum. Otoscopic features, including bulging and opacity of the eardrum, can be non-invasively examined. Nonetheless, otoscopy alone may not be sufficient for the diagnosis unless the presence of a MEE is clearly visualized behind the eardrum 5–7. Clinical guidelines therefore recommend the examination of eardrum mobility via pneumatic otoscopy 6,7. A pneumatic otoscope combines a standard otoscope with an insufflation bulb to generate variations in air pressure. The presence of a MEE will significantly decrease the eardrum mobility. Many studies have shown that pneumatic otoscopy provides increased sensitivity and specificity among middle ear diagnostic tools, such as standard otoscopy, tympanometry, and acoustic reflectometry, but only if performed and interpreted correctly 8–10. Pneumatic otoscopy is often described as being difficult to perform correctly, and as a result, is rarely used in practice 8,11,12.
To correctly perform pneumatic otoscopy, the ear canal must first be sealed using a specialized ear speculum (specula with rubber rings) in order to deliver variations in air pressure to the eardrum. Second, the magnitude of the pressure should be large enough so that the eardrum movement can be visualized by otoscopy, yet safe enough to prevent any rupture of the eardrum. Third, the air pressure from the pneumatic bulb should provide both negative and positive pressure to generate bidirectional movement of the eardrum. In addition, due to the pressure changes in the sealed ear canal, pneumatic otoscopy can often lead to patient discomfort 8. Lastly, one must ensure that the pneumatic otoscope itself does not have a pressure leak. To interpret the results from pneumatic otoscopy, physicians must detect subtle (< 1 mm) and fast (< 1 second) movement of an eardrum. When a MEE is present, eardrum mobility will be decreased and disrupted. However, decreased eardrum mobility will also be observed when the ear canal is not properly sealed, thereby compromising the diagnostic potential of this technique.
Motion magnification is a video processing technique that amplifies subtle motions in the video. By amplifying the spatiotemporal changes between frames, one study reconstructed magnified motion from the human pulse, oscillating guitar strings, and other visibly subtle motion 13. This linear Eulerian video magnification captures the small changes in color intensity values over time, at the frequency of interest. Although linear Eulerian video processing can magnify subtle motion without heavy computation, this method can be affected by noise, especially with larger magnification 14. Recently, a Eulerian approach was developed based on phase (complex-valued) changes in images 14. This method employs the fact that phase variations in one domain are equivalent to spatial translations in another domain via the Fourier shift theorem. As a result, phase-based Eulerian video processing amplifies subtle motion while suppressing noise, compared to the linear Eulerian processing method.
Motion magnification has great potential in biomedicine by identifying and visualizing motions that are not easily visible with the naked eye. For example, one study applied linear Eulerian video magnification to improve free flap monitoring during surgery 15. Based on subtle color changes in arteries and veins, blood supply and blockages can be monitored during surgery with motions magnified at frequencies around the heart rate (1.2–1.4 Hz). Furthermore, vibration patterns of a membrane exposed to acoustic stimuli have been visualized through motion magnification 16, showing the potential of this algorithm for applications in remote hearing or monitoring. Phase-based Eulerian motion magnification has recently been applied to a healthy adult subject to visualize eardrum vibration from a sound signal at 60 Hz 17. However, detecting the acoustic mobility of the eardrum was essentially limited by the frame rate of the camera, since audible frequencies range from 20 to 20,000 Hz for humans.
In this paper, motion magnification is employed to visualize pneumatic-induced motion of the human eardrum without sealing the ear canal. Sealing the ear canal is one of the main challenges and barriers to the wide-spread practical use of pneumatic otoscopy, since a special ear speculum is required to seal the ear canal. Nonetheless, pneumatic otoscopy has the capability of non-invasively examining the eardrum mobility, enhancing the diagnostic accuracy of middle ear infections. Phase-based Eulerian motion magnification developed by Wadhwa et al. 14 is applied to the videos acquired from a high frame-rate smartphone camera with an otoscope attachment. Furthermore, quantitative analysis is performed to compare motions from different regions on the eardrum. If the pneumatic-induced motions of eardrums can be identified and assessed without sealing the ear canal, pneumatic otoscopy will become a more reliable and accessible point-of-care diagnostic method in primary care, pediatrics, and otology.
2. Methods
2.1. Principles of phase-based Eulerian motion magnification
Phase-based Eulerian motion magnification was developed by Wadhwa et al. based on earlier works in Eulerian motion magnification 13. Eulerian motion magnification utilizes spatial decomposition of each frame in the input video, and a temporal filter is applied to select the motions at the frequency of interests. Then, the filtered motion signals are multiplied with a pre-defined number to amplify the small motions.
To mathematically describe the motion magnification algorithm, an image I(x) in one dimensional (1D) space is assumed. The 1D image I(x) has a small motion at time i, described by m(t). From the input with true motion, I(x + m(t)), we want to generate the output with magnified motions at a certain frequency. First, the 1D image with the true motion can be spatially decomposed using Fourier series decomposition and complex sinusoids with frequency ω,
| Equation (1) |
The term on the right side of the equation (1) indicates a sum of complex sinusoids, where the exponential term (phase) contains the motion information from the input image. From the Fourier shift theorem, we know that the time shifting in one domain (motions) is equal to the multiplication of the phase term in another domain. Thus, by modifying this phase term at a specific frequency, one can amplify the motions of interest.
In order to amplify only the motions of interest, a filter is applied to select the frequencies of interest. Assuming that we know a range of frequencies in the motion, m(t), the phase ωx + ωm(t) can be bandpass filtered to remove the DC component ωx, resulting in
| Equation (2) |
Then, the specific motion can be magnified in each term by an amplification factor, a, in Equation (1) as,
| Equation (3) |
Equation (3) shows the input with only motion m(t) amplified by the factor 1 + α. This process can be scaled up for two dimensional (2D) datasets or images. It is also noted that the changes in motions at different locations in 2D are computed by the same process as described for equations (1) through (3).
For the case of phase-based motion magnification, the spatial decomposition is performed using a complex steerable pyramid, a technique in signal processing and computer vision to understand an image with a range of scales and orientations 18. In addition, the phase is separated (Equation (1)) from the amplitude in each frame of multi-scale and multi-orientation. The spatiotemporal changes in the phase are analyzed by applying temporal filters to select the motions of interest (Equation (2)). Then, the bandpass filtered motions are magnified (Equation (3)) and combined with the amplitude to reconstruct the magnified video. More details about the algorithm can be found in Wadhwa et al. 14. In summary, each frame of a video is decomposed based on a wide range of complex values, and the temporally band-passed phase is modified to magnify spatial motion.
2.2. Experimental methods
To investigate a feasibility of the motion magnification algorithm to amplify the motions of the human eardrum, three adult volunteers were recruited at the Beckman Institute for Advanced Science and Technology (Urbana, IL) under a protocol approved by the institutional review board (IRB) at the University of Illinois at Urbana-Champaign. A standard 226 Hz tympanometry (TM286 AutoTymp, Welch-Sllyn) was used to measure the compliance of an eardrum and the middle ear pressure. Pneumatic video otoscopy and tympanometry were performed in a typical exam room. The subjects were asked to lie down on an examination bed for stable measurements during pneumatic video otoscopy. The subjects with the normal condition of the middle ear (n = 2) did not have any previous or recent middle ear disease or symptoms. These two subjects’ tympanograms revealed a type ‘A’ tympanogram showing a narrow, peak acoustic compliance. One adult volunteer complained of “ear fullness” obtained a type ‘As’ tympanogram, indicating decreased eardrum mobility. This subject also had previous middle ear infections as a child.
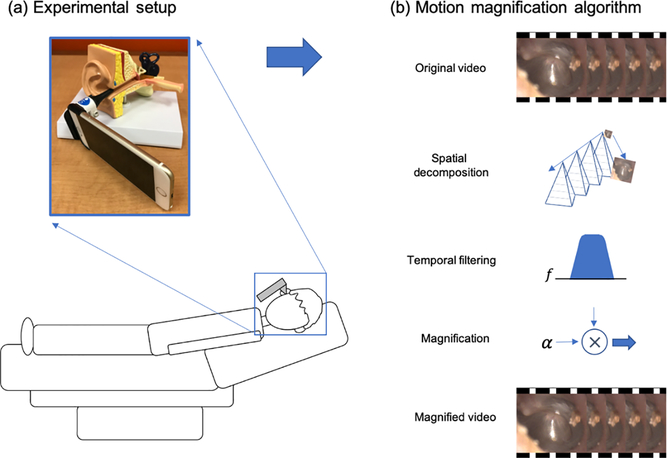
A smartphone (iPhone 6, Apple, Cupertino, CA) with an otoscope attachment (OTO, CellScope) was used to acquire videos of the pneumatic-induced motions of the eardrums at a frame rate of 60 Hz and with 720p resolution. The otoscope attachment contained an insufflation port for pneumatic otoscopy. Standard disposable otoscope specula were used during imaging under non-sealed conditions. In order to verify the processed motions, systematic and consistent pressure inputs were utilized. A custom-designed pressure generator based on a voice coil and bellow was employed from a previous study 19. The sinusoidal pressure (peak amplitude of ± 150 daPa, when properly sealed) at 5 Hz was applied via plastic tubing connected to the insufflation port. A frequency of 5 Hz was selected to avoid potential motion artifacts and motion due to the heart rate, which occurs around 1 Hz. For comparison to standard pneumatic otoscopy with a sealed ear canal, a silicone earbud was used with a speculum to form a proper seal of the ear canal. As a baseline measurement, videos of motion without sealing of the ear canal, and without any pressure inputs, were also acquired. Since the measurement is in a video format, one video measurement contains multiple repeats of movements, depending on the frequency of the induced pressure transient and the length of the video. The number of repeats can be adjusted by taking a longer measurement. In general, around 5 separate video measurements were taken for the study. A schematic diagram describing the experimental method is shown in Figure 1.
Figure 1.
Schematic diagram of (a) the experimental setup and (b) a graphical illustration of the motion magnification algorithm.
2.3. Applying phase-based Eulerian motion magnification
The acquired videos were cropped to select the region of interests. The start and the end of the videos were not used for the magnification algorithm to avoid potential motion artifacts. No stabilization of the videos was performed. Phase-based Eulerian motion magnification was performed on acquired videos in MATLAB (R2017b, MathWorks, MA) on a personal computer (Alienware i9 with 32 GB RAM). An octave-bandwidth pyramid with two orientations was used to decrease the processing time. Motions in the frequency range of 4.9 – 5.1 Hz were chosen to be amplified. The magnification factor (α) was set empirically to 15 for videos with an unsealed ear canal, and to 10 for videos with a sealed ear canal for visualization purposes. All parameters were consistent between measurements and subjects.
2.4. Analytical methods
A spatiotemporal slice is an effective two-dimensional representation of the video results. In order to quantify and compare the pneumatic motion, a spatiotemporal slice was generated for a line of interest over 100 frames (duration of 1.68 seconds with 60 Hz acquisition). The slice can validate the motion frequency, as well as the relative amplitude of the motion. In addition, the spatiotemporal slices at different spatial locations were examined to investigate the spatial and temporal dependence of the pneumatic mobility.
From the spatiotemporal slices, the amplitudes of the motions (in pixels) can be extracted. Each spatiotemporal slice was converted into a binary image, and the motions of interest in each spatiotemporal slice were segmented and quantified to determine the amplitudes. By comparing different regions, the spatial and temporal variations of pneumatic eardrum mobility can be investigated. No averaging was performed during the quantification.
3. Results
3.1. Pneumatic eardrum motion with a sealed ear canal
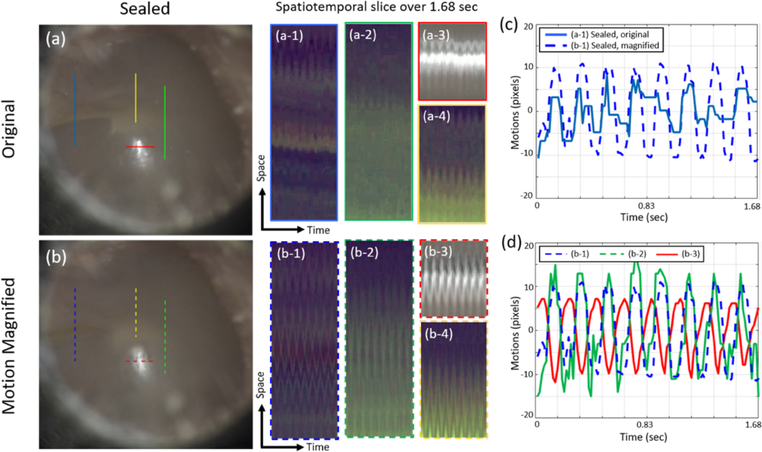
First, pneumatic-induced motion of an eardrum with a sealed ear canal, as in standard pneumatic otoscopy, is amplified to validate the motion magnification algorithm. Representative frames from the original (unmagnified) video and the motion magnified video are shown in Figure 2 (a) and (b), respectively. Multiple regions of interest are selected to represent different areas and features on the eardrum. The spatiotemporal slices on the lines of interest over 1.68 seconds (100 frames total) are displayed in Figure 2 (a-1) through (a-4) and Figure 2 (b-1) through (b-4).
Figure 2.
Comparison of (a) original and (b) motion magnified results showing pneumatic-induced motion of an eardrum with a sealed ear canal. The spatiotemporal slices for the blue, green, red, and yellow lines are shown in (a-1 through a-4 and b-1 through b-4, respectively). Note that around 8 peaks of the cyclical motion are visible from the spatiotemporal slice. (c) Comparison of motions at the blue line of interest between original and motion magnified results. (d) Spatial and temporal variations of eardrum mobility can be examined after the motion is amplified. This dataset was acquired from a healthy adult volunteer, subject 1. The original and the motion magnified video results can be found in Video 1.
Since some regions (inferior) of the eardrum do not exhibit obvious structural features at the original dynamic range of the camera, the contrast of colors (RGB) is adjusted to visualize subtle features. With sinusoidal pressure inputs at 5 Hz, around 8 cycles of pneumatic-induced motion over 1.68 seconds was expected. It is noted that both the motion magnified results and the original video show consistent pneumatic motion at 5 Hz, since the ear canal was properly sealed and sufficiently large pressure amplitudes were delivered. After motion magnification, exaggerated motions of the eardrum are visualized in Figure 2 (b).
In Figure 2 (c), the amplitudes of the motions on the blue lines of interest are compared after motion magnification. The magnification captures the same pneumatic-induced motion detected by the original video, but with a greater amplitude. Note that this amplitude can be adjusted using the magnification factor, a. In addition, more consistent and clearer temporal motions are identified after the motion is magnified. The magnified motions allow spatial and temporal comparison of the pneumatic-induced motion, as shown in Figure 2 (d). The smallest motions are identified around the light reflex region (b-3), whereas the larger motions are identified in the upper region (posterior). The light reflex region refers to a consistent region on the eardrum that reflects the most amount of the incident light from the ear canal. This feature is often used as a guide to examine the eardrum. Such spatial variations in the pneumatic mobility agreed with a previous study based on computed tomography (CT) images and finite element modeling (FEM) 20. Furthermore, a temporal delay is also observed among different regions of the eardrum. There was a temporal difference of around 80 msec between the motion captured from the light reflex region compared to the motion captured from the superior region of the eardrum.
3.2. Pneumatic-induced eardrum motion with an unsealed ear canal
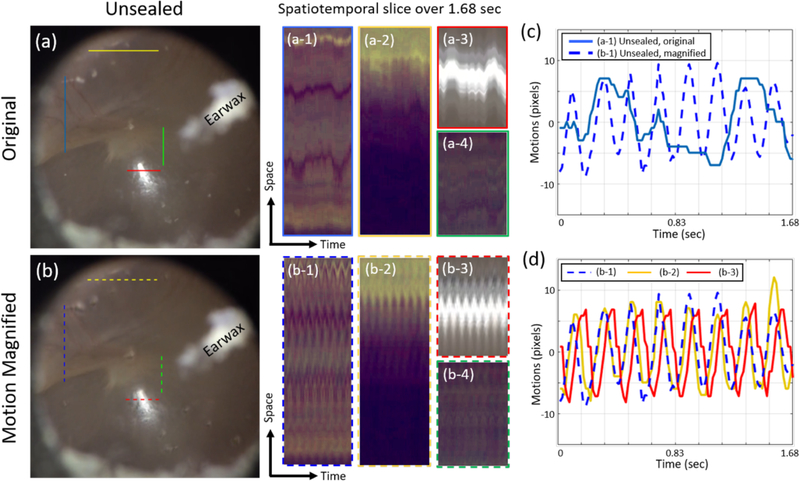
In general, pneumatic-induced motion of the eardrum is not visible with the naked eye without sealing the ear canal, because an insufficient pressure amplitude is delivered to the eardrum to induce large motion. Here, motion magnification is applied to the video acquired from pneumatic otoscopy without sealing the ear canal in order to visualize subtle motions on the eardrum. Representative frames from the original and the motion magnified videos for the case of an unsealed canal are shown in Figure 3, along with the spatiotemporal slices of interest. The slices in Figure 3 indicate that the motion at 5 Hz can be clearly visualized only after the motion magnification is applied. In Figure 3 (c), the motions on the blue line of interest are plotted after the magnification. Interestingly, subtle motions at 5 Hz are visualized from the original video, but greater motions at around 1 Hz (possibly due to heart rate) dominate the overall movement, concealing other smaller amplitude motions. After the motion at 5 Hz is magnified, however, the pneumatic-induced motion is identified. Similar to Figure 3 (d), the spatial and temporal variations of eardrum mobility can be examined without sealing of the ear canal. In this example, there was a temporal difference of around 60 msec between the motion captured from the region of the light reflex compared to the motion captured near the Pars flaccida (upper region, yellow) of the eardrum.
Figure 3.
Comparison of (a) original and (b) motion magnified results showing pneumatic-induced motion of an eardrum without sealing the ear canal. The spatiotemporal slices for the blue, green, red, and yellow lines are shown in (a-1 through a-4 and b-1 through b-4, respectively). Note that the motion magnification reveals around 8 peaks of the cyclical motion. (c) Comparison of motions at blue line of interest between the original and motion magnified results. (d) Spatial and temporal variations of the eardrum mobility can be examined after motion is amplified. This dataset was acquired from a healthy adult volunteer, subject 1. The original and the motion magnified video results can be found in Video 2.
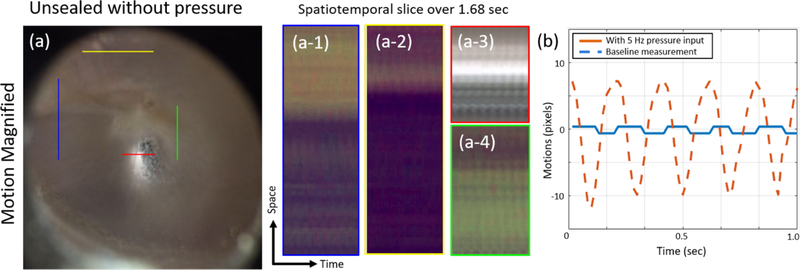
Baseline or background measurements are important since noise is often composed of a wide range of frequencies, with some potentially overlapping with the frequencies of interest. To validate that the motion magnification captures true movement, a control experiment was conducted without sealing the ear canal, and without any pressure input. Note that the measurements in Figures 2 and 3 were taken from the same healthy adult volunteer, for direct comparison of the sealing conditions and the baseline measurements. The motion magnification algorithm was applied to this control video using the same parameters as in previous cases (frequency range from 4.9 to 5.1 Hz to be amplified with an amplification factor of 15). A representative frame from the baseline/background measurement is shown in Figure 4. Note that there exist small fluctuations in the baseline measurement without pressure changes. This baseline noise is from minimal movements of the subject during the measurement, and contains a rage of frequencies. Since the algorithm is set to amplify any 5 Hz phase variations and the subject cannot be immobile, any inherent noise is magnified, as visualized in Figure 4 (b). However, the peak-to-peak amplitude of the pneumatic-induced motion is around 8 to 10 times greater than that of the noise (Figure 4 (b)). This validates that phase-based Eulerian motion magnification amplifies the true pneumatic-induced motion of an eardrum, but that background noise is present.
Figure 4.
Baseline motion magnified results from the video acquired with no pressure inputs and without sealing the ear canal. Note that although the algorithm captures noise at 5 Hz, the motions are subtle and much less compared to Figure 1 and 2. (b) Plot comparing the amplitudes of the motions with 5 Hz pressure input and the baseline measurement. This dataset was acquired from a healthy adult volunteer, subject 1.
3.3. Comparison of motions from sealed and unsealed ear canals
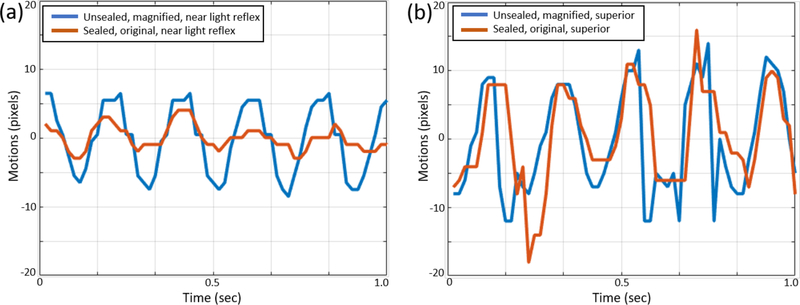
Ultimately, it is essential to determine if unsealed pneumatic otoscopy with motion magnification can produce similar results as properly sealed standard pneumatic otoscopy. The magnified motions without sealing the ear canal are compared with the original (unmagnified) pneumatic motions after sealing the ear canal. In Figure 5 (a), unsealed pneumatic otoscopy with motion magnification reveals a sinusoidal 5 Hz signal from the light reflex region as in standard pneumatic otoscopy, but with increased amplitude of the motion. In addition, Figure 5 (b) shows similar 5 Hz motion from the superior region on the eardrum with comparable amplitudes. The relative amplitudes of the magnified motions from the light reflex region were less than those in the posterior-superior region of the eardrum, as expected from previous results 20. Thus, depending on the eardrum region, motion magnification can generate greater or comparable pneumatic motion images or signals as in standard pneumatic otoscopy. Additional video datasets comparing properly sealed pneumatic otoscopy and unsealed pneumatic otoscopy with motion magnification can be found in Video 3. Video 3 was acquired from a second healthy adult volunteer, subject 2.
Figure 5.
Comparison of magnified eardrum motions with an unsealed ear canal versus the original eardrum motions with a sealed ear canal. (a) Comparison of motions near the light reflex region. (b) Comparison of motions near the posterior-superior regions on the eardrum.
3.4. Pneumatic-induced eardrum motion with decreased eardrum mobility
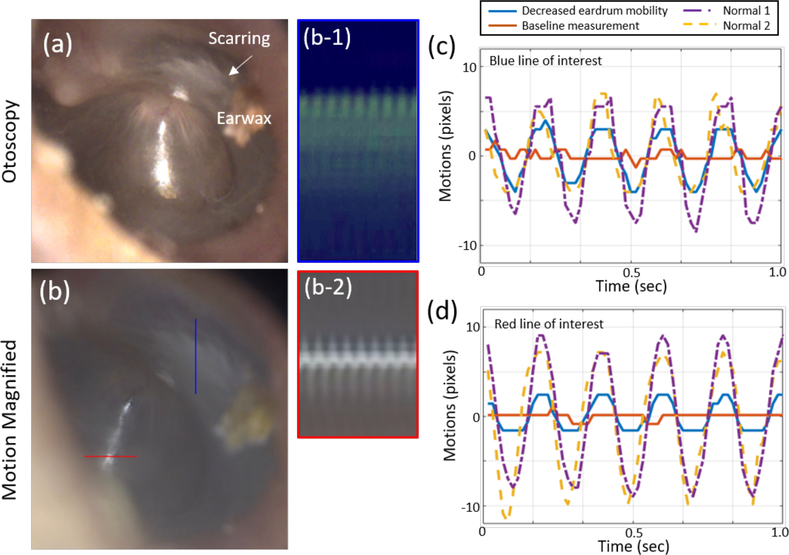
In order to assess decreased eardrum mobility with the motion magnification algorithm, unsealed pneumatic otoscopy was performed on an adult volunteer who complained of “ear fullness”. The subject had a type ‘As’ tympanogram with a compliance of 0.1 cm3. In general, a compliance of 0.3 cm3 or above is considered as normal. The middle ear pressure and the ear canal volume were determined to be −40 daPa and 0.9 cm3, respectively, and both values are within a normal range. The subject had slightly bulging eardrums as well as scarring on the eardrums, shown in Figure 6 (a). For unsealed pneumatic otoscopy, the magnitude and frequency of sinusoidal pressure inputs as well as the parameters for the motion magnification algorithm remained the same as those employed in the normal cases. Figure 6 (b) shows the motion magnified results with spatiotemporal slices showing 5 Hz motion. Figure 6 (c) and (d) describe the cyclical motion, compared with the motion from two healthy subjects. The two normal eardrums had a compliance of 0.5 cm3 and 0.4 cm3, determined from tympanometry. The peak-to-peak motion amplitude of the normal middle ear was around 2 to 4 times greater than that of the less compliant eardrum, depending on the region. Interestingly, there was much less (around 0 to 20 msec) temporal difference of motions between the two regions (blue and red line) of interest. This might be due to an increased stiffness of the eardrum in response to the pressure changes. The video dataset comparing the normal eardrum and the eardrum with decreased mobility is shown in Video 4.
Figure 6.
Motion magnified pneumatic-induced motion of the subject with decreased eardrum mobility. This subject obtained a type ‘As’ tympanogram with a peak compliance of 0.1 cm3. (a,b) High-resolution otoscopy images of the eardrum, where scarring and slight bulging of the eardrum are identified. (c,d) Plots of cyclical motion from the blue and red lines of interest (around light reflex), respectively. The amplitudes of the motion are around 2–4 times less than those from the two normal middle ear conditions.
4. Discussion
4.1. Capability of motion magnification for assessing eardrum mobility
Non-invasive assessment of eardrum mobility is challenging. Pneumatic otoscopy is the standard method to examine the pneumatic-induced mobility of human ear for the diagnosis of otitis media (an ear infection). However, it is difficult to perform and results are difficult to interpret due to several reasons. The complex and dynamic motions of the eardrum contain both lateral and axial (in and out of plane) movements, which require information in three dimensions for the appropriate assessment. While features on the eardrum can be used to help track these motions, the visible surface features of the eardrum are largely limited to only the light reflex (cone of light), the umbo, and the malleus. A few studies have been performed using quantitative pneumatic otoscopy, where videos of mobility are quantified and analyzed based on the locations and angles of the malleus and the umbo 21,22. However, the difficulties associated with the preparation and manipulation of pneumatic otoscopy remain the same, hindering the broader applicability of such quantitative analysis. More advanced research tools can quantitatively and accurately measure the pneumatic eardrum mobility. For example, optical coherence tomography (OCT) can measure pneumatic mobility of human eardrums in vivo 19,23. However, OCT is not currently used in clinics, and is more expensive compared to a standard or pneumatic otoscope.
Motion magnification can be a valuable add-on tool for pneumatic otoscopy since this processing algorithm can avoid the need for sealing the ear canal, can provide quantitative measures of the eardrum motions, and is affordable. We demonstrated that the video magnification can amplify eardrum motions in pneumatic otoscopy with and without sealing of the ear canal. The amplified eardrum motions show different spatial and temporal responses, which may be useful for studying different middle ear diseases. In the normal middle ear, we observed that the superior regions on the eardrum have greater displacements than the region near the light reflex. There was also a temporal variation between the eardrum motion from different regions of the eardrum. From the middle ear with low compliance, we observed around 2 to 4 less peak-to-peak amplitudes of magnified motion compared with that of the normal middle ear. In addition, much less temporal variation between regions of the eardrum was determined, emphasizing the potential of this technique to differentiate diseased from normal middle ear conditions. Although this study used a smartphone with an otoscope attachment, similar results can be obtained from a readily available video otoscope (Welch-Allyn Digital Macroview) that offers a sufficient camera frame-rate of 30 Hz for capturing motions around 2 to 5 Hz, a typical frequency range of pressure inputs by physicians using pneumatic otoscopy 24.
4.2. Significance of seeing pneumatic-induced eardrum motions with an unsealed ear canal
According to a recent study from 370 clinicians (70% of which were pediatricians and 30% of which were otorhinolaryngologists), around 90% of clinicians regularly use standard otoscopy, whereas only 17% of clinicians use pneumatic otoscopy 12. The reasons include that the instrument was absent in clinics (92.4%), that pneumatic otoscopy was considered useless (2.4%), and that the physicians had inadequate experience for its use (5.1%) 12. All of these responses were in spite of the established guidelines 6,7,11 that pneumatic otoscopy should be used for the diagnosis of otitis media. The standard instrument for diagnosis includes an otoscope with a pneumatic port, an insufflation bulb, and a specialized ear speculum with a rubber ring to pressure-seal the ear canal. The limited adoption and use suggest that developing experience and skills to manipulate a pneumatic otoscope to obtain and maintain a pressure seal of the ear canal is the critical barrier for physicians to perform pneumatic otoscopy in practice 11,12.
When the ear canal is properly sealed with a special ear speculum, and the seal is maintained (often in the presence of a fidgety infant who may be in pain from their ear infection), pneumatic motions are estimated to be around a few hundreds of micrometers, which are visible with the naked eye during otoscopy. During the diagnostic procedure, the subject can feel the pressure-induced movement of his/her eardrum, and may also feel uncomfortable during the measurement. Thus, magnification of eardrum motions without having to seal the ear canal not only simplifies this method for clinicians, but also minimizes the discomfort for patients 8.
In this paper, we showed that motion magnification can amplify subtle pneumatic-induced motions of the eardrum without a specialized ear speculum, and can visualize even larger-amplitude motions than pneumatic otoscopy with a sealed ear canal (Figure 5). Furthermore, the algorithm allows quantitative analysis of the pneumatic motions themselves. Lastly, it is worthwhile to emphasize that the motion magnification algorithm does not create the observed movements, and the magnified background noise is noticeably different compared with those from the pneumatic-induced motions (Figure 4). Because a standard ear speculum partially fills and seals the ear canal, it is therefore possible to deliver much less pressure to the ear canal and then magnify eardrum motions, compared to the need to fully seal the ear canal and deliver larger pressure amplitudes in order to visualize eardrum motions with the naked eye.
4.3. Limitations and future work
While motion magnification without the need to seal the ear canal provides a new method to examine the pneumatic-induced mobility of an eardrum, this study has several limitations for determining its diagnostic utility. First, the subject (patient) is required to remain still during the measurement, since large physical movements of the head or body can cause motion artifacts. Having subjects lie down on an exam bed, as was done in this study, can help with stabilization. The effect of the noise is also illustrated in Figure 5. Second, consistent pressure inputs (both amplitude and frequency) from a custom-built pressure system were used in this study, which would not be immediately accessible in clinics. However, the frequency range of interest for the motion magnification algorithm can be adjusted by the user. The frequency of pressure inputs by a hand-squeezed insufflation bulb varies between clinicians, and can range from 2 to 5 Hz 24. Third, although quantitative analysis was performed based on the relative amplitudes of the motions, the absolute amount of eardrum displacement cannot be measured with a pneumatic otoscope due to the axial movements of the eardrum. Recent advances in the use of OCT for imaging and quantifying the eardrum and its dynamics, however, would enable quantitative displacement measures on the micron scale 19,23. Fourth, the number of datasets presented in this initial study was limited, as the focus was on assessing the feasibility of motion magnification in pneumatic otoscopy. A future study will not only include a larger number of subjects to assess statistically different conditions, but will also include both normal and various pathological ear conditions to determine how magnified motions can be used for clinical diagnosis of different ear diseases.
In addition, the absolute amplitudes of the amplified motions may not be used for direct comparisons between different optical imaging systems and between adults and pediatric subjects. Imaging systems can have different parameters, such as magnification, pixel resolution, and frame rate. In this study, the magnification was kept constant (auto-focus lock feature) during motions. The standard otoscope tips that we used in the study behave as a mechanical spacer, since the shape of the tip prevents it from being inserted deeper into the ear canal. Nonetheless, the imaging distance and magnification are dependent on the length and anatomy of each individual ear canal, just as in standard otoscopy. We believe that the shorter distance between the speculum and the eardrum may give more accurate measurements. A higher frame rate and better pixel resolution may also provide more reliable measurements. For further investigations, more standardized tests are necessary to generate a normalized range for healthy eardrum movements that can be used between different optical imaging systems.
A video stabilization technique that does not affect the motion magnification will be helpful in order to apply this method to pediatric subjects. In addition, a recent work of amplitude-based filtering for video motion magnification by Wu et al. 25 may improve the accuracy of detecting pneumatic-induced motions even in the presence of larger motion. Lastly, a standardized, objective system for pneumatic otoscopy needs to be developed with a user-friendly, embedded platform for practical use of the motion magnification algorithm.
Motion magnification of video-based image data has other applications in biomedical imaging. Here, motion magnification was used to amplify subtle (sub-millimeter scale) motions visualized from a standard smartphone camera. If this algorithm is combined with more advanced and sensitive phase-based optical imaging systems that capture nanometer-scale eardrum motions, as in phase-resolved OCT 26, the motion magnification may reveal the nano-scale displacements of the eardrum associated with hearing.
5. Conclusion
Examining pneumatic-induced eardrum mobility is important for the diagnosis of middle ear infections. However, sealing the ear canal is required in order to observe the eardrum motions via otoscopy, since visible motions (few hundreds of micrometers) of the eardrum must be induced by the pressure. In this study, motion magnification based on the spatiotemporal changes in phase is employed to amplify subtle pneumatic-induced motions of the eardrum without having to seal the ear canal. The magnified motions were visualized with amplitudes comparable to those generated by standard pneumatic otoscopy. Furthermore, much less motion was identified after the motion magnification in the case of decreased eardrum mobility. Quantification and comparison of the relative amplitude and temporal response of the motions were performed for different regions of the eardrum, which may be useful for detecting the disrupted eardrum mobility that occurs during middle ear infections.
Acknowledgements
The authors would like to acknowledge Neal Wadhwa, Michael Rubinstein, Fredo Durand, and William T. Freeman for sharing phase-based video motion processing codes in MATLAB. The authors would also like to recognize and express their appreciation for the support provided by the McGinnis Medical Innovation Fellowship. The work is funded in part by NIH/NIBIB (R01EB013723 and R01EB028615 S.A.B.). Additional information can be found at http://biophotonics.illinois.edu.
References
- 1.Massa HM, Cripps AW, Lehmann D. Otitis media: Viruses, bacteria, biofilms and vaccines. Med J Aust. 2009;191(9):S44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kubba H, Birchall JP, Pearson JP. The aetiology of otitis media with effusion: A review. Clin Otolaryngol Allied Sci. 2000;25(3):181–194. doi: 10.1046/j.1365-2273.2000.00350.x [DOI] [PubMed] [Google Scholar]
- 3.Monasta L, Ronfani L, Marchetti F, et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS One. 2012;7(4):e36226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tong S, Amand C, Kieffer A, Kyaw MH. Trends in healthcare utilization and costs associated with acute otitis media in the United States during 2008–2014. BMC Health Serv Res. 2018;18(318):1–10. doi: 10.1186/s12913-018-3139-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sassen ML, Van Aarem A, Grote JJ. Validity of tympanometry in the diagnosis of middle ear effusion. Clin Otolaryngol Allied Sci. 1994;19(3):185–189. doi: 10.1111/j.1365-2273.1994.tb01211.x [DOI] [PubMed] [Google Scholar]
- 6.Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practice guidelines: otitis media with effusion (update). Otolaryngol Head Neck Surg. 2016;154(1S):S1–S41. [DOI] [PubMed] [Google Scholar]
- 7.Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964–999. [DOI] [PubMed] [Google Scholar]
- 8.Abbott P, Rosenkranz S, Hu W, Gunasekera H, Reath J. The effect and acceptability of tympanometry and pneumatic otoscopy in general practitioner diagnosis and management of childhood ear disease. BMC Fam Pract. 2014;15:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris PK, Hutchinson KM, Moravec J. The use of tympanometry and pneumatic otoscopy for predicting middle ear disease. Am J Audiol. 2005;14(1):3–13. doi: 10.1044/1059-0889(2005/002) [DOI] [PubMed] [Google Scholar]
- 10.Jones WS, Kaleida PH. How helpful is pneumatic otoscopy in improving diagnostic accuracy? Pediatrics. 2003;112:510–513. [DOI] [PubMed] [Google Scholar]
- 11.Harvey M, Bowe SN, Laury AM. Clinical practice guidelines: Whose practice are we guiding? Otolaryngol - Head Neck Surg (United States). 2016;155(3):373–375. doi: 10.1177/0194599816655145 [DOI] [PubMed] [Google Scholar]
- 12.Cullas Ilarslan EN, Gunay F, Topcu S, Ciftci E. Evaluation of clinical approaches and physician adherence to guidelines for otitis media with effusion. Int J Pediatr Otorhinolaryngol. 2018;112(June):97–103. doi: 10.1016/j.ijporl.2018.06.040 [DOI] [PubMed] [Google Scholar]
- 13.Wu HY, Rubinstein M, Shih E, Guttag J, Durand F, Freeman W. Eulerian video magnification for revealing subtle changes in the world. ACM Trans Graph. 2012;31(4 (Proc. SIGGRAPH)). doi: 10.1145/2185520.2185561 [DOI] [Google Scholar]
- 14.Wadhwa N, Rubinstein M, Durand F, Freeman WT. Phase-based video motion processing. ACM Trans Graph. 2013;32(4 (Proc. SIGGRAPH)). doi: 10.1145/2461912.2461966 [DOI] [Google Scholar]
- 15.Liu YF, Vuong C, Walker PC, et al. Noninvasive free flap monitoring using Eulerian video magnification. Case Rep Otolaryngol. 2016;2016:1–4. doi: 10.1155/2016/9471696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis A, Rubinstein M, Wadhwa N, Mysore GJ, Durand F, Freeman WT. The visual microphone: Passive recovery of sound from video. ACM Trans Graph. 2014;33(4). doi: 10.1145/2601097.2601119 [DOI] [Google Scholar]
- 17.Janatka M, Ramdoo KS, Tatla T, Pachtrachai K, Elson DS, Stoyanov D. Examining in vivo tympanic membrane mobility using smart phone video-otoscopy and phase-based Eulerian video magnification. Proc SPIE 10134, Med Imaging 2017 Comput Diagnosis. 2017;10134(March 2017):101341Y. doi: 10.1117/12.2253729 [DOI] [Google Scholar]
- 18.Simoncelli EP, Freeman WT. The steerable pyramid: a flexible architecture for multi-scale derivative computation. 2nd IEEE Int Conf Image Process. 1995; 111:444–447. doi: 10.1109/ICIP.1995.537667 [DOI] [Google Scholar]
- 19.Won J, Monroy GL, Huang P-C, et al. Pneumatic low-coherence interferometry otoscope to quantify tympanic membrane mobility and middle ear pressure. Biomed Opt Express. 2018;9(2):83–94. doi: 10.1364/BOE.9.000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gentil F, Parente M, Martins P, et al. Effects of the fibers distribution in the human eardrum: A biomechanical study. J Biomech. 2016;49(9):1518–1523. doi: 10.1016/j.jbiomech.2016.03.030 [DOI] [PubMed] [Google Scholar]
- 21.Cho Y-S, Lee D-K, Lee C-K, Ko MH, Lee H-S. Video pneumatic otoscopy for the diagnosis of otitis media with effusion: a quantitative approach. Eur Arch Otorhinolaryngol. 2009;266(7):967–973. [DOI] [PubMed] [Google Scholar]
- 22.Lee JK, Cho YS, Ko MH, et al. Video pneumatic otoscopy for the diagnosis of conductive hearing loss with normal tympanic membranes. Otolaryngol - Head Neck Surg. 2011;144(1):67–72. doi: 10.1177/0194599810390917 [DOI] [PubMed] [Google Scholar]
- 23.Shelton RL, Nolan RM, Monroy GL, et al. Quantitative pneumatic otoscopy using a light-based ranging technique. J Assoc Res Otolaryngol. 2017;18(4):555–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clarke LR, Wiederhold ML, Gates GA. Quatitation of pneumatic otoscopy. Otolaryngol Head Neck Surg. 1987;96(2):119–124. [DOI] [PubMed] [Google Scholar]
- 25.Wu X, Yang X, Jin J, Yang Z. Amplitude-based filtering for video magnification in presence of large motion. Sensors. 2018;18(7):12–14. doi: 10.3390/s18072312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang PC, Chaney EJ, Shelton RL, Boppart SA. Magnetomotive displacement of the tympanic membrane using magnetic nanoparticles: toward enhancement of sound perception. IEEE Trans Biomed Eng. 2018;65(12):2837–2846. doi: 10.1109/TBME.2018.2819649 [DOI] [PMC free article] [PubMed] [Google Scholar]