Abstract
An understanding of the influence of sex (biological attributes) and gender (socially constructed roles, behaviours, expressions, identities) factors on the risk of infection, hospitalization and death is of urgent importance in the COVID-19 pandemic response effort. Despite similar global rates of infection with Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2, the virus responsible for the COVID-19 pandemic), hospitalizations and mortality are higher in men than in women. Females may be less vulnerable to viral infection due to sex-based differences in immune responses and renin-angiotensin system activity. The response and side effects of currently studied potential therapies for COVID-19, such as hydroxychloroquine, likely differ by sex. Women form the majority of the health care workforce and a uniform approach to sizing of personal protective equipment may provide differing levels of protection from viral infection to health care workers of varying shapes and sizes. Important gender differences exist in the response to public health measures to prevent and contain spread of COVID-19, as well as presentation for testing and medical care, which may inadvertently propagate viral spread. Targeted approaches that consider both sex and gender, as well as measures of intersectionality, are urgently needed in the response efforts against COVID-19.
Keywords: Sex, Gender, COVID-19, Infection, Mortality, Policy
Résumé
Il est d’une importance primordiale, pour riposter à la pandémie de COVID-19, de comprendre l’influence des facteurs liés au sexe (les attributs biologiques) et au genre (les rôles, comportements, expressions et identités socialement construits) sur les risques d’infection, d’hospitalisation et de décès. Malgré la similarité mondiale des taux d’infection par le coronavirus du syndrome respiratoire aigu sévère 2 (SRAS-Cov-2, le virus responsable de la pandémie de COVID-19), les hospitalisations et la mortalité sont plus élevées chez les hommes que chez les femmes. Celles-ci pourraient être moins vulnérables à l’infection virale en raison de différences sexuelles dans les réponses immunitaires et dans l’activité du système rénine-angiotensine. Les réactions et les effets secondaires aux traitements possibles de la COVID-19 actuellement à l’étude, comme l’hydroxychloroquine, diffèrent probablement selon le sexe. Comme les femmes composent la majorité de la main-d’œuvre des soins de santé, les tailles uniformes de l’équipement de protection individuelle offrent peut-être des niveaux de protection inégaux contre l’infection virale aux travailleurs de la santé de formes et de tailles différentes. Il existe des différences importantes entre les genres dans les réactions aux mesures de santé publique visant à prévenir et à contenir la propagation de la COVID-19 et dans la présentation aux tests et aux soins médicaux, ce qui pourrait par inadvertance favoriser la propagation virale. Dans la riposte à la COVID-19, il devient urgent d’adopter des approches ciblées, qui tiennent compte à la fois du sexe et du genre, ainsi que des mesures de l’intersectionnalité.
Mots-clés: Sexe, genre, COVID-19, infection, mortalité, politique (principe)
Global data suggest that despite similar rates of infection with Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2), the virus responsible for the COVID-19 pandemic, hospitalizations and mortality are higher in men than in women across all age groups in confirmed cases (Global Health 50/50. COVID-19 Sex-disaggregated Data Tracker 2020). Whether sex- (biological attributes) or gender- (socially constructed roles, behaviours, expressions, identities) related factors are shaping this outcome is unknown. An understanding of the influence of each on risk of infection, hospitalization and death is of urgent importance in the COVID-19 pandemic response effort (Fig. 1).
Fig. 1.
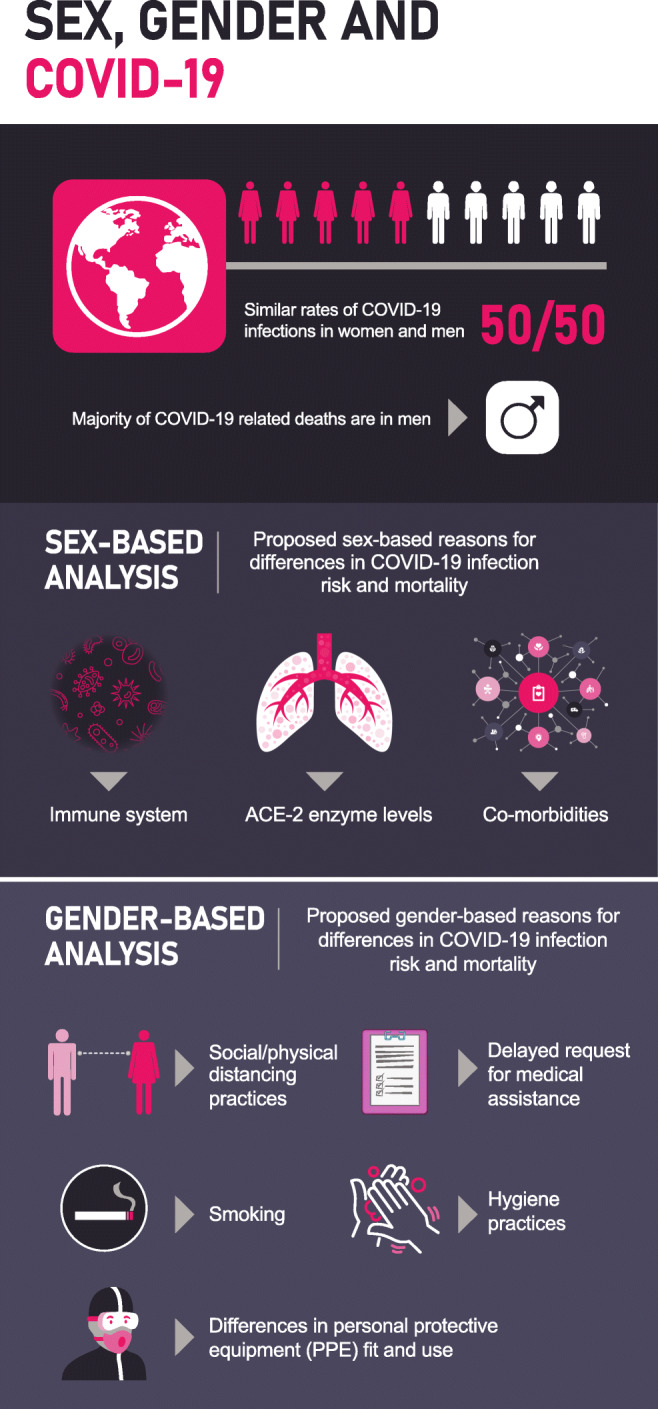
Sex and gender factors associated with SARS-CoV-2 infection and outcomes
Potential sex-related factors influencing SARS-CoV-2 infection
There are well-established sex-based reasons for a greater infection risk in males, with females being at significant immunological advantage. Females demonstrate stronger innate and humoral immune responses than males and are consequently less vulnerable to many bacterial, fungal, parasitic and viral infections (Schurz et al. 2019). Viral infections such as influenza, SARS-CoV and Middle Eastern Respiratory Syndrome Coronavirus exhibit sex-biased incidence and case-fatality rates with a male bias.
Globally, women make up 70% of frontline health care workers (Boniol et al. 2019), and thus, one would expect that women would have greater exposure to the virus in health care settings and would statistically represent a greater proportion of people infected with SARS-CoV-2. In countries with available data, female health care workers appear to be infected in greater numbers compared with their male counterparts (Global Health 50/50. COVID-19 Sex-disaggregated data tracker 2020). However, in countries that report sex- or gender-stratified data, general population infection rates are similar by sex (Global Health 50/50. COVID-19 Sex-disaggregated data tracker 2020). This suggests that either men are more likely to contract the virus for a given exposure or that men may be exposed to the virus more frequently in a non-health care setting.
Angiotensin-converting enzyme 2 (ACE2), an integral part of the human renin-angiotensin-aldosterone system (RAAS), is the functional receptor that allows SARS-CoV-2 to invade human alveolar epithelial cells (Zhou et al. 2020). While it is a subject of debate as to whether ACE2 expression is harmful or beneficial in patients infected with the virus, and specific sex differences in ACE2 expression are not clear, males demonstrate greater RAAS activity compared with females overall (Zalucky et al. 2014). Mortality risk in SARS-CoV-2 is increased in those with greater cardiovascular disease burden and elevated D-Dimer (Yang et al. 2020), and it has been speculated that a higher rate of cardiovascular disease and thrombosis in men may be contributing to increased mortality in this population. However, studies to date have not reported sex-stratified comorbidities of COVID-19 patients or RAAS antagonist use so it is not possible to comment on these potential contributors.
Among intubated patients, male patients are more likely than female patients to acquire ventilator-associated pneumonia (Cook and Kollef 1998), which may contribute to the higher mortality observed with COVID-19 in males. Prone positioning, a promising intervention among intubated patients, may reduce mortality among selected patients with severe acute respiratory distress syndrome, and trials are ongoing in those patients with SARS-CoV-2. While we are not aware of any literature suggesting that there is a sex difference in benefit or risk of this intervention, significant sex differences in airway structure and respiratory control (LoMauro and Aliverti 2018) exist, suggesting this is an important factor to consider when interpreting results.
Treatments aimed at reducing morbidity and mortality would benefit from sex-based stratification of results. Multiple randomized controlled trials are ongoing to assess the efficacy of hydroxychloroquine in the treatment of SARS-CoV-2. Given the known potential for cardiac arrhythmias with this medication (WHO Evidence Review Group Meeting: The cardiotoxicity of antimalarials 2017), as well as sex-based differences in cardiac electrophysiology, interpretation of results via a sex lens is warranted.
Potential gender-related factors influencing SARS-CoV-2 infection
Gendered factors may also play a role in the risk of infection, hospitalization and death due to SARS-CoV-2. As recommended by health authorities worldwide, handwashing with soap is one of the most effective means of preventing infection with SARS-CoV-2. Reported hand hygiene practices during the COVID-19 pandemic appear to differ by gender (Guzek et al. 2020); a previous study reported that men were less likely to engage in handwashing with soap in public restrooms compared with women (Johnson et al. 2003). Interestingly, the presence of a visual behaviour prompt in the form of a sign increased rates of handwashing with soap in women by over 30%, but was not associated with a change in handwashing behaviour in men (Johnson et al. 2003), highlighting the importance of incorporating gender norms, roles and relations in how public health measures are communicated and disseminated. Similarly, the Kaiser Family Foundation Coronavirus and Health Tracking Polls demonstrated important differences in how women and men are experiencing the pandemic, with men less likely to report taking protective actions (Hamel and Salganicoff 2020) as recommended by governmental advisories. These telephone surveys show that while self-reported social distancing measures have increased significantly for everyone, men are less likely than women to report staying home instead of going to work or other regular activities (69% vs. 81%), changing or cancelling travel plans (66% vs. 72%), or remaining sheltered in place (76% vs. 88%). It is possible that current gender-neutral or gender-blind approaches to transmission of information in the COVID-19 pandemic are failing to reach specific aspects of society. Moreover, measures for the prevention and control of the COVID 19 pandemic have been criticized as being designed for a Western capitalist society without accounting for impact on other cultures, including that of Indigenous peoples (Junior et al. 2020), with important gendered health implications in these communities (Levesque and Quesnel-Vallee 2019).
Personal protective equipment (PPE) is an essential form of workplace safety in the health care setting, and numerous jurisdictions have reported inadequate PPE supplies for their workers during the COVID-19 pandemic. PPE has been primarily developed based on measurements taken from white American military male recruits during the 1950s to 1970s, which is not reflective of the increasing gender and ethnic diversity of the health care workforce. Previous data have suggested that alternative-size PPE fitting a range of body shapes and sizes is not always readily available (Flynn et al. 2017), and poor fit may, in addition to increasing the risk of infection, discourage proper use, further increasing the risk of viral transmission. Whether appropriately sized PPE is in use during the COVID-19 pandemic, and whether this differs by sex or gender, is unknown.
Across health conditions, women are more likely to seek medical attention compared with men for the same concern (Thompson et al. 2016), suggesting that men may present later in the course of the illness or disease. Members of the LGBTQ community may be less likely to seek medical attention for health concerns due to concerns of discrimination and stigmatization (Mule et al. 2009). Testing for SARS-CoV-2 is performed at the discretion of treating health care providers, and testing practices and capabilities vary widely across providers, facilities and jurisdictions around the world. In the United States, more women than men have been tested for SARS-CoV-2 (Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Briefing: April 9, 2020. 2020); it is unknown if there are sex or gender differences in the global rates of testing for SARS-CoV-2, only that the sex ratio of confirmed cases is similar (Global Health 50/50. COVID-19 Sex-disaggregated data tracker 2020). Gender differences in timing of presentation to a health care provider may provide some explanation for the higher rates of hospitalization of men with COVID-19 on a global scale, as men may present for testing and medical evaluation later and sicker.
Globally, men are more likely to smoke and thus have the potential for poorer respiratory outcomes in SARS-Cov-2 infection, though this remains speculative as gender-stratified smoking rates have not been specifically reported in the published COVID-19 literature.
Numerous factors, including age, ethnicity, race, socio-economic position, geographic location, health status and occupation, intersect with sex and gender to shape an individual’s vulnerability to the impacts of COVID-19. Targeted approaches that consider both sex and gender, as well as these important intersecting factors, are urgently needed in the fight against COVID-19. We strongly urge policymakers, scientists, health care providers and governments to incorporate sex and gender into all aspects of prevention, testing and treatment to achieve the most effective and equitable pandemic response.
Acknowledgements
We thank Alexa Desjarlais for graphic design.
Author contributions
All authors had access to the data and a role in writing the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Boniol M, McIsaac M, Xu L, Wuliji T, Diallo K, Campbell J. Gender equity in the health workforce: analysis of 104 countries. Working paper 1. Geneva: World Health Organization; 2019. [Google Scholar]
- Cook DJ, Kollef MH. Risk factors for ICU-acquired pneumonia. JAMA. 1998;279(20):1605–1606. doi: 10.1001/jama.279.20.1605. [DOI] [PubMed] [Google Scholar]
- Flynn MA, Keller B, DeLaney SC. Promotion of alternative-sized personal protective equipment. Journal of Safety Research. 2017;63:43–46. doi: 10.1016/j.jsr.2017.08.004. [DOI] [PubMed] [Google Scholar]
- Global Health 50/50. COVID-19 Sex-disaggregated data tracker (2020). https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/. Accessed 25 August 2020.
- Guzek, D., Skolmowska, D., Głąbska, D. (2020). Analysis of gender-dependent personal protective behaviors in a national sample: Polish Adolescents’ COVID-19 Experience (PLACE-19) study. International Journal of Environmental Research and Public Health, 17(16), 5770. 10.3390/ijerph17165770. [DOI] [PMC free article] [PubMed]
- Hamel, L., & Salganicoff, A. (2020). Is there a widening gender gap in coronavirus stress? https://www.kff.org/coronavirus-policy-watch/is-there-widening-gender-gap-in-coronavirus-stress/. Accessed 11 April 2020.
- Johnson HD, Sholcosky D, Gabello K, Ragni R, Ogonosky N. Sex differences in public restroom handwashing behavior associated with visual behavior prompts. Perceptual and Motor Skills. 2003;97(3 Pt 1):805–810. doi: 10.2466/pms.2003.97.3.805. [DOI] [PubMed] [Google Scholar]
- Junior JG, Moreira MM, Pinheiro WR, de Amorim LM, Lima CKT, da Silva CGL, et al. The mental health of those whose rights have been taken away: an essay on the mental health of indigenous peoples in the face of the 2019 Coronavirus (2019-nCoV) outbreak. Psychiatry Research. 2020;289:113094. doi: 10.1016/j.psychres.2020.113094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levesque A, Quesnel-Vallee A. Gender variations in the relationship between social capital and mental health outcomes among the Indigenous populations of Canada. International Journal for Equity in Health. 2019;18(1):124. doi: 10.1186/s12939-019-1028-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoMauro A, Aliverti A. Sex differences in respiratory function. Breathe (Sheffield, England) 2018;14(2):131–140. doi: 10.1183/20734735.000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mule NJ, Ross LE, Deeprose B, Jackson BE, Daley A, Travers A, et al. Promoting LGBT health and wellbeing through inclusive policy development. International Journal for Equity in Health. 2009;8:18. doi: 10.1186/1475-9276-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remarks by President Trump, Vice President Pence, and Members of the Coronavirus Task Force in Press Briefing: April 9, 2020 (2020). https://www.whitehouse.gov/briefings-statements/remarks-president-trump-vice-president-pence-members-coronavirus-task-force-press-briefing-23/. Accessed 18 April 2020.
- Schurz H, Salie M, Tromp G, Hoal EG, Kinnear CJ, Moller M. The X chromosome and sex-specific effects in infectious disease susceptibility. Human Genomics. 2019;13(1):2. doi: 10.1186/s40246-018-0185-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Family Practice. 2016;17:38. doi: 10.1186/s12875-016-0440-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Evidence Review Group Meeting: The cardiotoxicity of antimalarials (2017). https://www.who.int/malaria/mpac/mpac-mar2017-erg-cardiotoxicity-report-session2.pdf. Accessed 18 April 2020.
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International Journal of Infectious Diseases. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalucky, A. A., Nicholl, D. D. M., Mann, M. C., Hemmelgarn, B. R., Turin, T. C., MacRae, J. M., Sola, D. Y., Ahmed S. B. (2014). Sex influences the effect of body mass index on the vascular response to angiotensin II in humans. Obesity 22(3), 739–746. 10.1002/oby.20608. [DOI] [PubMed]
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


