Abstract
The impact of COVID-19 on food security can best be understood from the downturn on agricultural and other related economic activities which were almost brought to a total halt during the pandemic. The restriction of movement/lockdown policy instituted by various governments heavily affected local and national food production as farmers could not go to their farmlands. More so, there was price gouging on raw food items as local farmers were reducing cultivation and harvest because of their safety. The lockdown also affected the transportation of food products from farms and local companies to the market and across inter-state/province borders. Additionally, many human infections traceable to disease outbreak from animal origin suggest a great risk of exposure to infectious agents by live animal farmers. In combating this menace, local food production needs to be encouraged more, while measures should be put in place to facilitate farmer's participation in government regulations on enforcing biosecurity, health standards, disease monitoring, and surveillance practices.
Keywords: Agricultural produce, Animal production, COVID-19, Food security, Public health, Risk assessment
Résumé
L’impact de la COVID-19 sur la sécurité alimentaire peut être mieux compris à partir du ralentissement des activités agricoles, et autres activités économiques connexes, qui ont été presque totalement interrompues pendant la pandémie. La restriction des déplacements et le verrouillage institué par les différents gouvernements ont fortement affecté la production alimentaire locale et nationale, les agriculteurs ne pouvant plus se rendre sur leurs terres. De plus, les prix des produits alimentaires bruts ont été réduits, car les agriculteurs locaux ont réduit leurs cultures et leurs récoltes en raison de leur sécurité. Le blocage a également affecté le transport des produits alimentaires des fermes et des entreprises locales vers le marché et au-delà des frontières entre les États et les provinces. En outre, de nombreuses infections humaines, dont on peut retracer l’origine animale, suggèrent un grand risque d’exposition des éleveurs d’animaux vivants à des agents infectieux. Pour lutter contre cette menace, il convient d’encourager davantage la production alimentaire locale, tout en mettant en place des mesures visant à faciliter la participation des agriculteurs aux réglementations gouvernementales relatives à l’application de la biosécurité, des normes sanitaires, du suivi des maladies et des pratiques de surveillance.
Mots clés: Produits agricoles, COVID-19, Sécurité alimentaire, Santé publique, Évaluation des risques
Introduction
Food security is one of the major challenges being faced by the fast-rising African population even though she is blessed with diverse human and natural resources [1]. Since the first confirmed case of COVID-19 in Africa was recorded in Egypt on 14 February 2020 [2], all hands have been on deck to forestall tension and reduce panic on her citizens. Amongst other measures that were put in place in combating the global menace, the Government in African countries like every other government in Europe, Asia, America, etc. instituted a total lockdown and restriction to human movements across their countries [3] without having adequate measures in place to combat the impending food crisis.
Due to the lockdown measures, food security became a thug of war as there was an incessant hike in the price of foodstuffs whilst there was no change in economic capabilities. The restriction on movement which resulted in the unavailability of labor made it difficult for farming activities to be carried out. Furthermore, companies involved in the production and processing of food products were also affected, i.e. many stopped been operational. Even those that were working, their production/operation capacity were reduced in adherence to the directives instituted by the government. Consequently, there was a high demand for food and foodstuffs due to a significant drop in supply which led to product scarcity and a reduction in the purchasing power of individuals. Therefore, only a little food item could be bought with a large sum of money; making it difficult to derive maximum value for the money spent.
More so, due to the long period of the lockdown, many homes and families undoubtedly did not have enough physical and economic access to sufficient, safe, and nutritious food that meets the daily dietary needs and food preferences for an active and healthy life based on individual's nutritional requirement and dietary considerations. The majority of the populace is currently out of job (no work, no pay), so they are not currently earning an income, thus affecting their standard of living [4]. Although the government policies do not affect the general availability of food commodities, but daily and/or low-income earners who live below the poverty line were greatly affected, as they began to weep and fear for the “hunger virus” rather than the dreaded coronavirus. Additionally, the government relief packages were only palliatives and could not go round because they were insufficient in supply.
Furthermore, in Africa, the COVID-19 pandemic is occurring amid other societal threats and existing shocks such as desert locust infestations in East Africa, adverse climatic effects in Zimbabwe and northern Mozambique, civil unrest in South Sudan, northern Nigeria, and the Sahel; thus, the coronavirus pandemic exacerbated the threats to food security and the vulnerabilities faced by the agricultural sector [5], [6]. From the foregoing, it could be affirmed that the COVID-19 crisis had contributed adversely to increased food insecurity in Africa as livestock supply chains are currently experiencing disruptions, including limited access to inputs and services, transport and roadblocks, restricted labor movements, and heightened credit financing or poor liquidity, with the resultant increase in food prices. Driven by disruptions to market activities prices continue to rise substantially in Zimbabwe, Sudan, and South Sudan, among other African countries [7]. It has been estimated that agricultural production would contract by 2.6 percent optimistically and by 7 percent with trade blockages [8].
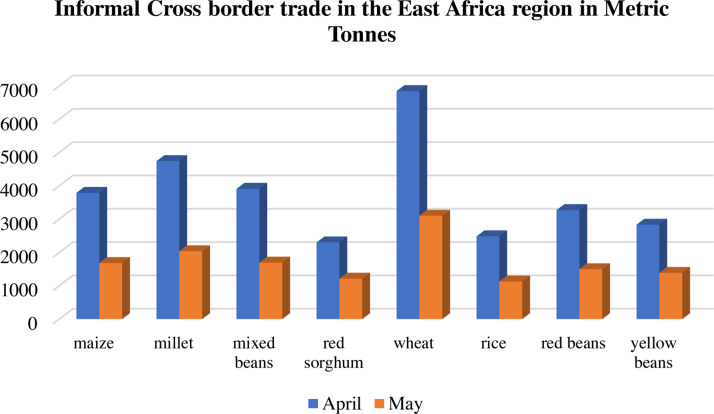
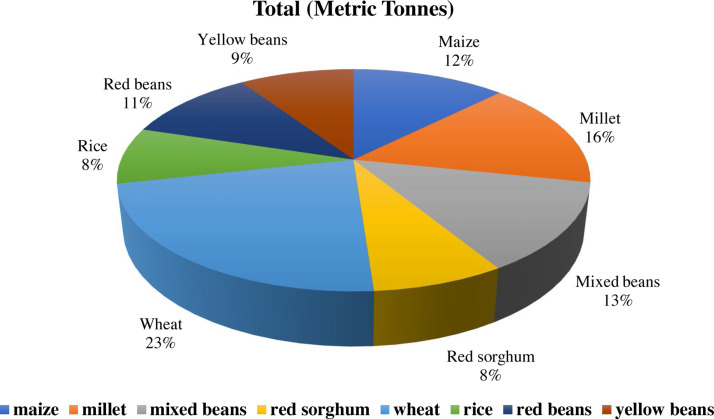
The rising cases of COVID-19 in the African region have restricted cross border movement and trade, especially for truck drivers hauling agricultural products. About 75% reduction occurred in informal cross border trade compared to January and February, during the first quarter of 2020 [9]. The commodity flow for grain markets between April and May 2020, across selected borders of East African countries such as Tanzania, Burundi, Rwanda, Uganda, Kenya, Somalia, Djibouti, Ethiopia, Sudan, and South Sudan and DRC is given in Figure 1, Figure 2 .
Figure 1.
Informal cross border trade in the East Africa regions between April–May, 2020. Adapted from [9].
Commerce transfrontalier informel dans les régions d’Afrique de l’Est entre avril et mai 2020. Adapté de [9].
Figure 2.
Total informal cross border trade in the East African Grain Markets. Adapted from [9].
Total du commerce transfrontalier informel sur les marchés céréaliers d’Afrique de l’Est. Adapté de [9].
Additionally, over the past months of April and May 2020, with a steading rise of confirmed cases across African countries, grain prices have increased owing to the depletion of stocks gotten from the previous harvest [10]. The disparity in lockdown protocols and measures by different governments has impacted grain trades across African countries. The increment in costs of agricultural inputs, logistic challenges, and reduced cross border transactions have facilitated peaks in food prices across the regions [10], [11].
Food security and safety concerns in animal production
COVID-19 is a respiratory illness that can spread from person to person through direct contact or by droplets released by an infected person through coughing or sneezing, etc. [12]. However, the WHO and the U.S. Centers for Disease Control and Prevention suggest that populaces with amplified hazard for complexities; including aged persons and people with constant health issues, for example, coronary illness, diabetes, and lung ailment, and so forth should avoid potential risk to their health [13].
While home sanitation and individual cleanliness are consistently significant, regular hand washing with soap and fast running water for a minimum of 20 seconds has been heavily encouraged in reducing the spread of the disease [13]. Other practices, like frequent sanitizing and cleaning different surfaces, can likewise serve as an extra defensive measure just as proper hygiene [14].
According to the U.S. Food and Drug Administration, the Centers for Disease Control and Prevention, and the U.S. Department of Agriculture, there is at present no proof to propose that COVID-19 can be transmitted through food consumption or food bundling, but food safety practices are highly encouraged [15].
Nevertheless, a large number of chemicals in consumer food products have been suspected and identified to be endocrine-disrupting chemicals (EDCs), which are potential contributors to reducing human and animals immunity against diseases and also the development of many of these chronic diseases [16]. Such chemical compounds (e.g. polycyclic aromatic hydrocarbons, PAHs, and polychlorinated biphenyls, PCBs) are widespread in processed foods and food packaging materials and are exacerbating health challenges, and also in the case of COVID-19 pandemics. Furthermore, the poor nutrition obtained in most processed foodstuffs along sides the EDCs in food and food bundling materials such as bisphenol A (BPA), could prompt the interruption of proper regulation of glucose/blood sugar, insulin resistance, and cell brokenness coming about in inflammation [17]. As a consequence, the ingestion of these chemical compounds beyond permissible limit endangers one and makes one susceptible to infectious disease as a result of impaired immunity.
It is noteworthy to note that hurtful food microorganisms develop quickly at a mild temperature range of 41 °F to 140 °F [18]. Thus, some households tend to cook food at a higher temperature thereby bringing about food burn. However, food processing techniques such as cooking, drying, grilling, roasting, frying, and smoking, etc. at high temperatures are major sources of PAHs [19], [20].
Bioaccumulation of these ubiquitous organic pollutants in plants and animals constitute a serious health threat. PAHs are a large category of varied organic compounds, each of them having a minimum of two fused aromatic rings containing mainly carbon and hydrogen atoms in its skeletal structure. PAH generally occur in complex mixtures, which may consist of hundreds of compounds. They are principally framed by deficient ignition or pyrolysis of organic material and during various industrial processes and food handling procedures [21], [22]. These groups of compounds have potentially hazardous effects on the environment and health, as the majority of them are carcinogenic, teratogenic and mutagenic [23], [24]. Some studies have reported the mean daily intake of the total PAH fraction to be between 4 ng/kg per day (low estimate) and 10 ng/kg per day (high estimate) [25].
Additionally, plants and exposed foodstuffs could get in contact with PAHs essentially via climatic depositions on vegetables, fruits, grains, etc. particularly those with broad leaves, and through take-up from contaminated water and soil [26]. Gomes et al. [27] reported that vegetation in urbanized zones, particularly those with proximity to roads and huge industrial activities tend to have higher concentrations of PAHs. More so, seafood such as fish, mussels, shellfish, and shrimp have polluted enroute the absorption of polluted surface waters and are responsible for an important proportion of food-borne illnesses and outbreaks [28]. The degree of accumulation and withholding of PAHs in aquatic lives are subjected by some components, such as PAHs profile, PAHs availability, biota physiology among others [29], [30].
Studies have postulated that PAHs could aggregate on item surfaces, due to their lipophilicity; additionally, the dispersion can occur to internal layers [31] where water movement and fat substance have a major role in relocation rate [32]. On the other hand, the presence of obstructions, for example, the packages of smoked sausages and the skin of bacon [33], [34] can meddle with PAHs movement into products inner layers. According to the European Food Safety Authority [35], meat and meat items are one of the food categories contributing most to dietary admission of PAHs every day.
Furthermore, PCBs, have been reported to be one of the man-made chlorinated compounds gotten from a biphenyl ring with 1 to 10 chlorine atoms attached on each of the phenyl ring resulting in 209 congeners [36], [37]. PCBs are non-ionizable, largely non-polar, and highly hydrophobic in nature. Investigations have shown that human beings are largely exposed to PCBs during food ingestion, and seldom, via occupation. Thus, they can bind tightly and be deposited into fatty tissues, organs, and glands [38], [39]. PCBs are also known suppressors of immune system function, increase the risk of diabetes, causes cardiovascular diseases, decreased verbal learning, increased depression, hypo-reflexia, neurobehavioral disturbances, reproductive disorders, etc. [37], [40], [41].
Risk assessment and impact of food ethics on public health
Human risk assessment has been investigated to find out the potential hazard resulting from human exposure to poisonous substances present in various foodstuffs and environmental matrices. These investigations are generally used to help with meeting guidelines like those specified by administrative bodies like WHO and numerous others [42]. The major point of human risk evaluation is, to ensure the protection of consumers against the impacts of poisons in water or foods. Thus, it is important to guarantee that contaminants of interest in food or water don’t surpass the normal daily intake.
The incidence of PAHs in a significant number of our day-by-day food substances represents a grave risk to humans. Human exposure to high concentrations of PAHs via food consumption may bring about injurious and harmful impacts [43]. Contaminants in food have been accounted for by numerous researchers and every one of the potential contaminants can be connected to an assortment of harmful impacts. Every adverse effect observed relies upon various components, like exposure intensity, rate or frequency, duration, route and dose, and/or concentration; subtleties of the individual like age and health status [44], [45], [46]. Most PAHs are capable of causing cancer that accounts for the significant effect of the risk characterizations. However, it is often hard to attribute a given health effect in epidemiological studies to a particular PAH compound since PAHs exist as a mixture of different PAH compounds [47]. In general, the higher molecular weight PAHs are more hydrophobic, toxic and recalcitrant [48].
The discoveries of some epidemiological studies on PAHs provides a superior appreciation of the dangers of polar PAHs to people and other organisms, particularly as the harmfulness of PAHs is regularly through the impacts of exceptionally receptive polar genotoxic metabolites instead of direct impacts of PAHs [49]. In many case-control investigations, loss of ovarian capacities, the decrease in lung capacities, advancement of diseases, early stage of menopause, male infertility, and frequencies of diabetes are other health effects of PAHs exposure [50].
Impact of COVID-19 on livestock production and animal health
In Africa, livestock production occupies an important facet in nutrition, food security, livelihood, socio-economic roles and significantly contributes to household income generation. Livestock products are estimated to contribute about 30% of the agricultural GDP in Africa [51]. In West African countries, the livestock sector contributes substantially, such as 5% in Côte d’Ivoire, 44% in Mali, 40% in Sahel countries, 15% in Mauritania, and 3% in Nigeria to the agricultural GDP [52]. This contribution to rural agricultural development forms an integral drive towards food security, poverty alleviation, and national stability [51].
The virus responsible for the COVID-19 disease, SARS-CoV-2 is zoonotic in origin, as such can infect humans and animals [53]. Farmers have been considered particularly vulnerable to infections due to their proximity to animals, and the zoonotic risk associated with the COVID-19 virus [54]. Earlier reports of human infections were traceable to wet markets, as such, suggesting the greater risk by which live animal farmers may be exposed to infectious agents [55]. Reported cases of infected pets such as dogs, and cats, have raised concerns regarding transmission between livestock and farmers. Besides, research has postulated that some farm animals including pigs, ducks, and chickens were not susceptible, to the SARS-CoV-2 virus; but are carriers of other pathogenic organisms, that may pose a potential threat to humans and can reduce human immunity and pose an imminent risk to human health [56], [57]. Although still under investigation, there is a need to further validate these findings under commercial livestock conditions. Alongside this, on-farm disease surveillance, and health care services are either unavailable or inadequate, thus, putting the health and safety of the farmers at risk. Also, the problem of farm and job security arises following infection of workers and economic disruptions in the livestock value chain, as all stages, from production, processing, marketing, distribution, and consumption have been affected and may lead to layoffs of the workforce, thus creating massive unemployment and loss of income [58].
During pandemics, the livestock sector often accounts for significant economic losses, with implications for food security, especially in regions that are heavily dependent on this sector. With the emergence of COVID-19, the limitations enforced on the animal-human interface has resulted in adverse impacts for both livestock production and associated livelihoods [5].
In a bid to curtail the risk of COVID-19 disease transmission, policy responses to limit inter-human contacts and complete shut-down of human activities in severely affected regions have resulted in concomitant drastic effects on animal production, farm outputs, and supplies to markets. Proper management of farm animals allows for their daily access to feed, water, medication, and other production supplies as necessary. The inability of farmers to freely conduct their rearing activities or possibly have access to farm inputs would culminate in affecting not only the welfare of farm animals, but the farmer's livelihood, and consumer's access to goods and services.
Nomadic/pastoral herdsmen are particularly affected by movement restriction since their farming activities are heavily reliant on movement across grasslands in search of natural resources. The ease of access to extension services and technical experts to troubleshoot farm problems is hampered especially in rural areas with inadequate access to digital service for ready access to information. Regular on-farm visitation by extension agents is therefore difficult to navigate considering that this may be a possible route for farm-to-farm transmission of diseases.
Reduced access to market stalls and farmer's markets arising from movement restrictions impacts negatively on-farm productivity, increasing wastage and post-harvest losses of livestock products especially due to their relatively short shelf life. Fresh food supply chains may be hampered with restrictions on trading routes, furthermore, increasing deterioration, and wastage [59]. The disruptions to livestock products demand and supply, and losses in farm products, further poses discouragement and disincentives for continued production, processing, and marketing of livestock and animal products. Closures of communal and territorial markets as seen in Kenya and Nigeria have also increased the extent of post-harvest losses since a large proportion of small-scale farmers, especially women, rely on these local markets for sales [60]. Direct sales to restaurants, hotels, and food service vendors have also suffered major setbacks due to low patronage. Following the limitations in airfreights and cargo deliveries of imported goods into the countries, market activities are lulled. The heavy dependence of the livestock sector for imported feed ingredients, medication, and technical experts poses significant constraints on livestock production in African countries. A substantial decline in food imports, between 13 to 25 percent, has been reported in African countries as a result of higher transaction costs and decreased domestic demand [8].
Conclusion and mitigation strategies
The recent COVID-19 pandemic is an eye-opener to what is most salient: food and health. Therefore, it is pertinent that a total restructuring of the food sub-sector of the economy to achieve sustainable development. Most African nations depend heavily on imported food items, raw materials, and packing resources [61]; but the recent ban of imported food items and the current temporary shutdown of all borders due to COVID-19. Therefore, serious attention needs to be diverted into reviving locally made food and raw materials. Although the production power is insufficient to sustain her population, the cash empowerment of the masses with regards to the financial assistance to help raise the standard of living is necessary for the government at all levels to effectively contain food security and animal production issues.
Also, there is a need for strategic and systematic dissemination of important information as well as education about nutritional values and general health care to the masses. More so, valid and documented regulations to make sure foodstuffs and essential commodities not to be hoarded and unnecessary price hike to earn more profit at the detriment of the common man need to be strictly enacted. Additionally, adequate budgetary allocations to local manufacturers and agriculture particularly the food crop and animal production sub-sectors, and enunciation of appropriate policies need to be revisited. These will help to support locally produced items and aid the export of surplus resources.
Need to say, Africa has been opportune to thrive through previous crises such as the Ebola epidemic (2014–2015) and the food crisis of 2008–2009, thus giving the continent a leveraging ground for pandemic preparedness and response. As part of the COVID-19 response, the African Development Bank has designed the Feed Africa Response to COVID-19 (also known as FAREC), to support farmers, governments other individuals, in building resilience, sustainability, and food sufficiency in the agriculture value chain. Key needs outlined by farmers in countries such as Niger, Nigeria, Senegal, Ghana, and Burkina Faso, to combat the COVID-19 outbreak included virtual learning platforms, digital extension services, electronic payments, and fund transfers, and digital marketing tools [62]. Alternate marketing strategies such as “green channels”, direct sales from farms, and online marketing should be facilitated to safely connect livestock producers with consumers. Changes to infrastructure and investment in cold chains would allow for fresh food processing, storage, and distribution, thus, curbing farm losses. Proper sanitary and biosecurity practices should be adopted in farms and slaughterhouses. However, disease control technologies, such as vaccinations against virulent diseases – Newcastle disease, avian influenza, and African swine fever, should be deployed to safeguard livestock and livelihoods of vulnerable communities.
There still exists a wide gap in information dissemination and the wrongly held belief of the COVID-19 disease as a “speculation” by several rural households in Africa. This bridge can only be exterminated with proper awareness, and sensitization on COVID-19 safety measures for individuals involved in animal production, handling, processing, marketing, and distribution. Prioritizing investment in small-scale farmers and strengthening animal processing and storage facilities would further strengthen access to food as a response against food insecurity. Measures to facilitate farmer's participation in enforcing biosecurity and health standards, disease monitoring and surveillance practices are imminent [60]. Likewise, the inter-relatedness of humans, animals, and the environment is an important linkage in understanding and tackling existing threats to food systems, agricultural production, and livelihoods [63]. Therefore, in tackling the current COVID-19 pandemic and in preparedness for future disease epidemics, the FAO recommends a “One Health approach”, which can holistically address the health of an animal, human and environmental in concert, to achieve the best results [64]. Furthermore, since there is currently no existing reports linking the ingestion of toxic organic pollutants (PAH, PCBs, BPA, etc.) due to COVID-19 and lockdown measure, there is still a need to pay strict attention to food processing guidelines and procedures to reduce the intake of these compounds to boost immunity against diseases and future pandemic outbreaks.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgments
The authors greatly acknowledge the support of the Organization of African Academic Doctors in China.
References
- 1.Matemilola S., Elegbede I. The challenges of food security in Nigeria. Open Access Libr J. 2017;04:1–22. [Google Scholar]
- 2.WHO . World Health Organization; Africa: 2020. COVID-19 cases top 10 000 in Africa. [Cited 2020 Jul 20. Available from: https://www.afro.who.int/news/covid-19-cases-top-10-000-africa#:∼:text=Reaching the continent through travellers, countries have reported cases] [Google Scholar]
- 3.Oyeniran O.I., Chia T. Novel Coronavirus disease 2019 (COVID-19) outbreak in Nigeria: how effective are government interventions? Ethics Med Public Heal. 2020:100515. doi: 10.1016/j.jemep.2020.100515%0A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Francis N.N., Pegg S. Socially distanced school-based nutrition program feeding under COVID 19 in the rural Niger Delta. Extr Ind Soc. 2020 doi: 10.1016/j.exis.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.FAO . 2020. Coronavirus disease 2019 (COVID-19) Addressing the impacts of COVID-19 in food crises April–December 2020. [Available from: http://www.fao.org/3/ca8497en/ca8497en.pdf] [Google Scholar]
- 6.Pais G., Jayaram K., van Wamelen A. McKinsey and Company; 2020. Safeguarding Africa's food systems through and beyond the crisis. [Cited 2020 Jul 14. Available from: https://www.mckinsey.com/featured-insights/middle-east-and-africa/safeguarding-africas-food-systems-through-and-beyond-the-crisis] [Google Scholar]
- 7.Blanke J. Brookings; 2020. Economic impact of COVID-19: protecting Africa's food systems from farm to fork. [Cited 2020 Jul 14. Available from: https://www.brookings.edu/blog/africa-in-focus/2020/06/19/economic-impact-of-covid-19-protecting-africas-food-systems-from-farm-to-fork/] [Google Scholar]
- 8.Calderon C., Kambou G., Zebaze Djiofack C., Korman V., Kubota M., Cantu Canales C. 2020. Africa's pulse: assessing the economic impact of Covid-19 and policy responses in Sub-Saharan Africa. [Available from: https://s3-eu-west-1.amazonaws.com/s3.sourceafrica.net/documents/119870/Africa-s-Pulse-Assessing-the-Economic-Impact-of.pdf] [Google Scholar]
- 9.RATIN . 2020. Eastern Africa grain markets and trade – Price & trade bulletin. Grain watch monthly April & May 2020 Update; pp. 1–6. [Google Scholar]
- 10.FSNWG-MAS Prices for seclected commodities in East Africa in first quarter of 2020. East Africa Crossborder Trade Bulletin 29. 2020 [Google Scholar]
- 11.Kipkogei O., Mwesigwa J. IGAD Climate Prediction And Applications Centre (ICPAC); 2020. Agriculture and food security situation analysis and measures taken to minimize impacts of march to may 2020 season; pp. 1–6. [Google Scholar]
- 12.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC . Centers for Disease Control and Prevention; 2020. Food Safety and Coronavirus Disease 2019 (COVID-19) [Cited 2020 Jul 23. Available from: https://www.cdc.gov/foodsafety/newsletter/food-safety-and-Coronavirus.html] [Google Scholar]
- 14.Academy of Nutrition Dietetics Concerns Regarding COVID-19. Eat Right. 2020 [Cited 2020 Jul 23. Available from: https://www.eatright.org/coronavirus] [Google Scholar]
- 15.Ciccone J.K. Ohio State News Contributor; 2020. Food safety during the COVID-19 outbreak. [Cited 2020 Jul 21. Available from: https://news.osu.edu/food-safety-during-the-covid-19-outbreak/] [Google Scholar]
- 16.Diamanti-Kandarakis E., Bourguignon J.P., Giudice L.C., Hauser R., Prins G.S., Soto A.M. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr Rev. 2009;30:293–342. doi: 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boucher J. Food Packaging Forum; 2020. Article discusses toxic chemical exposure and COVID-19. [Cited 2020 Jul 23. Available from: https://www.foodpackagingforum.org/news/article-discusses-toxic-chemical-exposure-and-covid-19] [Google Scholar]
- 18.CDC . Centres for Disease Control and Prevention; 2020. Food and coronavirus disease 2019 (COVID-19) [Cited 2020 Jul 23. Available from: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/food-and-COVID-19.html] [Google Scholar]
- 19.Zelinkova Z., Wenzl T. The occurrence of 16 EPA PAHs in food – A review. Polycycl Aromat Compd. 2015;35:248–284. doi: 10.1080/10406638.2014.918550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh L., Varshney J.G., Agarwal T. Polycyclic aromatic hydrocarbons’ formation and occurrence in processed food. Food Chem. 2016;199:768–781. doi: 10.1016/j.foodchem.2015.12.074. [DOI] [PubMed] [Google Scholar]
- 21.Alegbeleye O.O., Opeolu B.O., Jackson V.A. Polycyclic aromatic hydrocarbons: a critical review of environmental occurrence and bioremediation. Environ Manage. 2017;60:758–783. doi: 10.1007/s00267-017-0896-2. [DOI] [PubMed] [Google Scholar]
- 22.Iwegbue C.M.A., Odogbor D., Egobueze F.E., Emoyan O.O., Tesi G.O., Odali E.W. Polycyclic aromatic hydrocarbons in smoked ethmalosa fimbriata and gymnarchus niloticus from selected fish markets in the Niger delta, Nigeria. Polycycl Aromat Compd. 2018;0:1–14. doi: 10.1080/10406638.2018.1550794. [DOI] [Google Scholar]
- 23.Yu H. Environmental carcinogenic polycyclic aromatic hydrocarbons: photochemistry and phototoxicity. J Environ Sci Heal C Environ Carcinog Ecotoxicol Rev. 2002;20:149–183. doi: 10.1081/GNC-120016203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balcıoğlu E.B. Potential effects of polycyclic aromatic hydrocarbons (PAHs) in marine foods on human health: a critical review. Toxin Rev. 2016;35:98–105. [Google Scholar]
- 25.WHO . World Health Organization; 2006. Evaluations of the joint FAO/WHO expert committee on food additives (JECFA) [Cited 2020 Jul 22. Available from: https://apps.who.int/food-additives-contaminants-jecfa-database/chemical.aspx?chemID=4306] [Google Scholar]
- 26.Fismes J., Perrin-Ganier C., Empereur-Bissonnet P., Morel J.L. Soil-to-root transfer and translocation of polycyclic aromatic hydrocarbons by vegetables grown on industrial contaminated soils. J Environ Qual. 2002;31:1649–1656. doi: 10.2134/jeq2002.1649. [DOI] [PubMed] [Google Scholar]
- 27.Gomes A., Santos C., Almeida J., Elias M., Roseiro L.C. Effect of fat content, casing type and smoking procedures on PAHs contents of Portuguese traditional dry fermented sausages. Food Chem Toxicol. 2013;58:369–374. doi: 10.1016/j.fct.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Iwamoto M., Ayers T., Mahon B.E., Swerdlow D.L. Epidemiology of seafood-associated infections in the United States. Clin Microbiol Rev. 2010;23:399–411. doi: 10.1128/CMR.00059-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menichini E., Bocca B. Encyclopedia of food sciences and nutrition. In: B C., LC T., PM F., editors. 2nd ed. 2nd ed. Academic Press; Amsterdam, Netherlands: 2003. p. 4616. [Google Scholar]
- 30.MacKay D., Fraser A. Bioaccumulation of persistent organic chemicals: mechanisms and models. Environ Pollut. 2000;110:375–391. doi: 10.1016/s0269-7491(00)00162-7. [DOI] [PubMed] [Google Scholar]
- 31.Šimko P. Factors affecting elimination of polycyclic aromatic hydrocarbons from smoked meat foods and liquid smoke flavorings. Mol Nutr Food Res. 2005;49:637–647. doi: 10.1002/mnfr.200400091. [DOI] [PubMed] [Google Scholar]
- 32.Martorell I., Perelló G., Martí-Cid R., Castell V., Llobet J.M., Domingo J.L. Polycyclic aromatic hydrocarbons (PAH) in foods and estimated PAH intake by the population of Catalonia, Spain: temporal trend. Environ Int. 2010;36:424–432. doi: 10.1016/j.envint.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 33.García-Falcón M.S., Simal-Gándara J. Polycyclic aromatic hydrocarbons in smoke from different woods and their transfer during traditional smoking into chorizo sausages with collagen and tripe casings. Food Addit Contam. 2005;22:1–8. doi: 10.1080/02652030400023119. [DOI] [PubMed] [Google Scholar]
- 34.Djinovic J., Popovic A., Jira W. Polycyclic aromatic hydrocarbons (PAHs) in different types of smoked meat products from Serbia. Meat Sci. 2008;80:449–456. doi: 10.1016/j.meatsci.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 35.EFSA Scientific opinion of the panel on contaminants in the food chain on a request from the European Commission on Polycyclic Aromatic Hydrocarbons in Food. EFSA J. 2008;724:1–114. [Google Scholar]
- 36.Visha A., Gandhi N., Bhavsar S.P., Arhonditsis G.B. A Bayesian assessment of polychlorinated biphenyl contamination of fish communities in the Laurentian Great Lakes. Chemosphere. 2018;210:1193–1206. doi: 10.1016/j.chemosphere.2018.07.070. [DOI] [PubMed] [Google Scholar]
- 37.Tesi G.O., Iniaghe P.O. Polychlorinated biphenyls in canned sardines in Nigeria and health risk assessment. Food Addit Contam Part B Surveill. 2020;00:1–7. doi: 10.1080/19393210.2020.1762758. [DOI] [PubMed] [Google Scholar]
- 38.Helou K., Harmouche-Karaki M., Karake S., Narbonne J.F. A review of organochlorine pesticides and polychlorinated biphenyls in Lebanon: environmental and human contaminants. Chemosphere. 2019;231:357–368. doi: 10.1016/j.chemosphere.2019.05.109. [DOI] [PubMed] [Google Scholar]
- 39.Ti Q., Gu C., Liu C., Cai J., Bian Y., Yang X. Comparative evaluation of influence of aging, soil properties and structural characteristics on bioaccessibility of polychlorinated biphenyls in soil. Chemosphere. 2018;210:941–948. doi: 10.1016/j.chemosphere.2018.07.111. [DOI] [PubMed] [Google Scholar]
- 40.Tomasallo C., Anderson H., Haughwout M.L., Imm P., Knobeloch L. Mortality among frequent consumers of Great Lakes sport fish. Environ Res. 2010;110:62–69. doi: 10.1016/j.envres.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Turyk M.E., Anderson H.A., Persky V.W. Relationships of thyroid hormones with polychlorinated biphenyls, dioxins, furans, and DDE in adults. Environ Health Perspect. 2007;115:1197–1203. doi: 10.1289/ehp.10179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu D., Hornbuckle K.C. Inadvertent polychlorinated biphenyls in commercial paint pigments. Environ Sci Technol. 2010;44:2822–2827. doi: 10.1021/es902413k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olatunji O.S., Fatoki O.S., Ximba B.J., Opeolu B.O. Polycyclic aromatic hydrocarbons (PAHs) in edible oil: temperature effect on recovery from base hydrolysis product and health risk factor. Food Public Heal. 2014;4:23–30. [Google Scholar]
- 44.Thompson L.A., Darwish W.S. Environmental chemical contaminants in food: review of a global problem. J Toxicol. 2019;2019:2345283. doi: 10.1155/2019/2345283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abdel-Shafy H.I., Mansour M.S.M. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet. 2016;25:107–123. doi: 10.1016/j.ejpe.2015.03.011. [DOI] [Google Scholar]
- 46.Rengarajan T., Rajendran P., Nandakumar N., Lokeshkumar B., Rajendran P., Nishigaki I. Exposure to polycyclic aromatic hydrocarbons with special focus on cancer. Asian Pac J Trop Biomed. 2015;5:182–189. doi: 10.1016/S2221-1691(15)30003-4. [DOI] [Google Scholar]
- 47.ATSDR . Agency for Toxic Substances and Disease Registry; 2011. Polycyclic aromatic hydrocarbons (PAHs) [Cited 2020 May 12. Available from: https://www.atsdr.cdc.gov/substances/toxsubstance.asp?toxid=25] [PubMed] [Google Scholar]
- 48.Bamforth S.M., Singleton I. Bioremediation of polycyclic aromatic hydrocarbons: current knowledge and future directions. J Chem Technol Biotechnol. 2005;80:723–736. [Google Scholar]
- 49.Sen S., Field J.M. 1st ed. Vol. 7. Elsevier B.V; 2013. Genotoxicity of polycyclic aromatic hydrocarbon metabolites: radical cations and ketones; pp. 83–127. (Advances in Molecular Toxicology). [DOI] [Google Scholar]
- 50.Idowu O., Semple K.T., Ramadass K., O’Connor W., Hansbro P., Thavamani P. Beyond the obvious: environmental health implications of polar polycyclic aromatic hydrocarbons. Environ Int. 2019;123:543–557. doi: 10.1016/j.envint.2018.12.051. [DOI] [PubMed] [Google Scholar]
- 51.FAO . Food and Agriculture Organization of the United States; 2020. Animal agriculture in Africa: opportunities for growth. [Cited 2020 Jul 3. Available from: http://www.fao.org/ag/againfo/home/en/news_archive/2011_Animal_Agriculture_in_Africa.html#%3A∼%3Atext=so%20that%20its%20growth-environment,goats%2C and 22 million pigs] [Google Scholar]
- 52.Kamuanga M.J.B., Somda J., Sanon Y., Kagoné H. SWAC-OECD/ECOWAS; 2008. Livestock and regional market in the Sahel and West Africa: potentials and challenges; pp. 1–170. [Available from: https://www.oecd.org/swac/publications/41848366.pdf] [Google Scholar]
- 53.Peltz J. Bloomberg; 2020. Tiger at NYC's bronx zoo tests positive for coronavirus. [Cited 2020 Apr 6. Available from: https://www.bloomberg.com/news/articles/2020-04-05/tiger-at-nyc-s-bronx-zoo-tests-positive-for-coronavirus] [Google Scholar]
- 54.Li H., Mendelsohn E., Zong C., Zhang W., Hagan E., Wang N. Human-animal interactions and bat coronavirus spillover potential among rural residents in Southern China. Biosaf Heal. 2019;1:84–90. doi: 10.1016/j.bsheal.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.EClinicalMedicine Editorial Emerging zoonoses: a one health challenge. EClinicalMedicine. 2020:19. doi: 10.1016/j.eclinm.2020.100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Broom F. Don’t panic, experts say after COVID-19 animal killings. Sci Dev Net. 2020 [Cited 2020 Apr 17. Available from: https://www.scidev.net/global/coronavirus/news/covid-19-animal-killings.html?__cf_chl_jschl_tk__=ef26a5983f6c351efbf64665121ec14c17ccb30b-1595497487-0-ARrx8NArJMzvBuiegPYYSljDMbToI9JPdeOZJ58dBNMz72koy1BEWSyGop1gg5CpU2O8_8V3fgWYiaUH3TVmW_Cpg3BuJ0csHo1CaXtC] [Google Scholar]
- 57.Fevre E. ILRI; 2020. Domestic livestock not a source of the COVID-19 disease. [Cited 2020 Apr 17. Available from: https://www.ilri.org/news/domestic-livestock-not-source-covid-19-disease—ilri-veterinary-epidemiologist-eric-fevre] [Google Scholar]
- 58.El-Sawalhy A. Effects on animal feed availability, veterinary and veterinary public health services, other production inputs and market access. African Union – Interafr Bur Anim Resour. 2020 [Google Scholar]
- 59.Cullen M.T. 2020. Coronavirus food supply chain under strain what to do? [Available from: http://www.fao.org/3/ca8308en/ca8308en.pdf] [Google Scholar]
- 60.Actionaid . 2020. Right to food, farmers’ rights & Covid-19: policy priorities and a call to action. [Available from: https://actionaid.nl/wp-content/uploads/2020/06/Right-to-food-and-farmers-rights-and-COVID-19-ActionAid-Policy-Brief.pdf] [Google Scholar]
- 61.Adesoji B.S. 2019. Nigerians spend N334.3 billion to import foodstuffs, tobacco, others in 6-months. [Available from: https://nairametrics.com/2019/10/03/nigerians-spent-n334-3-billion-to-import-foodstuffs-tobacco-others-in-6-months/] [Google Scholar]
- 62.ICRISAT . Reliefweb; 2020. What African farmers and processors say about the COVID-19 pandemic and lockdowns. [Cited 2020 Jul 14. Available from: https://reliefweb.int/report/world/what-african-farmers-and-processors-say-about-covid-19-pandemic-and-lockdowns] [Google Scholar]
- 63.Nabarro D., Wannous C. The potential contribution of Iivestock to food and nutrition security: the application of the One Health approach in livestock policy and practice. Rev Sci Tech. 2014;33:475–485. doi: 10.20506/rst.33.2.2292. [DOI] [PubMed] [Google Scholar]
- 64.FAO . Rome; 2020. Guidelines to mitigate the impact of the COVID-19 pandemic on livestock production and animal health. [Available from: http://www.fao.org/3/ca9177en/CA9177EN.pdf] [Google Scholar]