Figure 3.
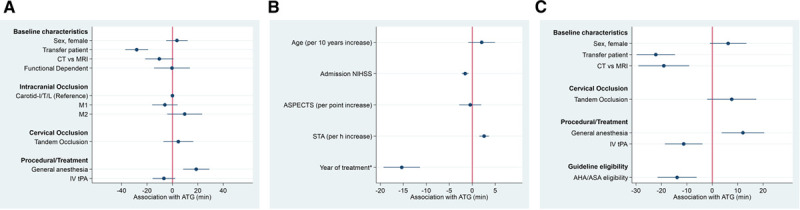
Adjusted differences in admission-to-groin-puncture (ATG) intervals according to baseline and procedural variables. A, Categorical variables (effect scale, −60 to 60 min), patients receiving magnetic resonance imaging (MRI) or general anesthesia had increased ATG. B, Continuous variables (effect scale, −10 to 10 min), patients presenting late, patients with lower National Institutes of Health Stroke Scale (NIHSS), and patients treated in earlier years had increased ATG. C, Same model but functional dependence, age, Alberta Stroke Program Early CT Score (ASPECTS), admission NIHSS, and symptom-to-admission (STA) replaced by a compound variable of meeting American Heart Association (AHA)/American Stroke Association (ASA) guideline indication criteria. Patients meeting AHA/ASA guideline indication criteria on average had 14 min shorter ATG. CT indicates computed tomography; IV tPA, intravenous tissue-type plasminogen activator; M1, first segment of the middle cerebral artery; and M2, second segment of the middle cerebral artery. *Year of treatment implemented as continuous variable as per year increase since 2015.
