Abstract
To observe the ocular axis, visual acuity and intraocular pressure (IOP) of aphakic eye in infants with congenital cataract and complex microphthalmos after first-stage cataract surgery.
This retrospective study included infants with congenital cataract and operated at the Qingdao Eye Hospital between January 2010 and December 2014. The infants were divided into 2 groups: preoperative axial length <18 mm (microphthalmos) or ≥18 mm (controls). Follow-up lasted 24 months; visual acuity, axial length, and IOP were evaluated.
There were 28 infants (55 eyes) in the microphthalmos group and 35 (61 eyes) in the control group. The preoperative visual acuity was negative for optokinetic nystagmus, while the postoperative visual acuity was positive for optokinetic nystagmus in both groups. The growth rate was higher in the microphthalmos group (1.4 ± 0.8 vs 0.8 ± 0.4 mm/yr, P < .001 vs controls). The axial length was smaller in the microphthalmos group at all time points compared with the control group (all P < .001). There was no changes in IOP in the microphthalmos group from baseline to 24 months (P = .147), but the IOP was slightly decreased in the control group (P = .015).
Cataract surgery may contribute to ocular axis growth in infants with complex microphthalmos.
Keywords: cataract, congenital, microphthalmos, ocular axis
1. Introduction
Cataract is a relatively common disease leading to poor vision and blindness in infants. There are about 1.5 million infants around the world suffering from blinding eye diseases, and 7.4% to 15.3% of them suffer from congenital cataract,[1] which can be accompanied by ocular dysplasia such as microphthalmos. Microphthalmos is a congenital abnormality that is often combined with congenital cataract due to its characteristic structures including thickened sclera, normal or slightly larger lens with relatively small eye volume, higher volume ratio of lens to eye, shallow anterior chamber, narrow chamber angle, and short ocular axis.[2] Microphthalmos is likely to cause glaucoma and other complications involving the retina and choroid.[2] Congenital cataract with complex microphthalmos is often combined with ocular or systemic abnormalities, and patients after surgery are prone to secondary glaucoma, corneal opacity, and other serious complications.[3] The impact of preoperative axial length on eyeball growth of postoperative aphakic eye was unclear. Indeed, despite having a shorter axis length, the eyes with congenital cataract show a similar growth rate to that of normal eyes,[4] but other studies showed that shorter ocular axis before lens extraction is associated with faster ocular axis growth after surgery.[5,6] Due to the low incidence of congenital cataract with complex microphthalmos, the characteristics of ocular axis growth of aphakic eye in these patients after cataract surgery are unknown. Nevertheless, thanks to careful intervention and implantation of intraocular lens (IOL), the vision of these patients can now be improved to varying degrees.[7–11]
Microphthalmos is defined as an eye with an axial length more than 2 standard deviations below the mean for the age adjusted population.[12,13] The axial length is 16.8 mm at birth and 20 mm at 1 year of age, but with individual differences.[14] In this study, we selected infants under 1 year of age with congenital cataract whose axial length was <18 mm, observed their ocular axis growth between first-stage cataract surgery and second-stage IOL implantation, and compared with eyes with preoperative axial length of ≥18 mm.
2. Methods
2.1. Study design and subjects
This retrospective study included infants who had congenital cataract, and who underwent surgical treatment at the Qingdao Eye Hospital between January 2010 and December 2014. This study was approved by the ethics committee of the Qingdao Eye Hospital. The inclusion criteria were:
-
(1)
diagnosed with congenital cataract;
-
(2)
<1 year old at first-stage cataract surgery;
-
(3)
the vision was affected due to dense opacity of the lens cortex or nucleus; and
-
(4)
ophthalmoscopy failed to examine the situation of the ocular fundus.
The exclusion criteria were:
-
(1)
combined with other ocular diseases such as retinopathy of prematurity, persistent hyperplasia of primary vitreous, retinoblastoma, congenital glaucoma, retinal detachment, etc; or
-
(2)
systemic diseases such as congenital heart disease.
The infants with congenital cataract were divided into 2 groups according to whether their preoperative axial length was <18 mm (microphthalmos) or not (normal eyeballs).
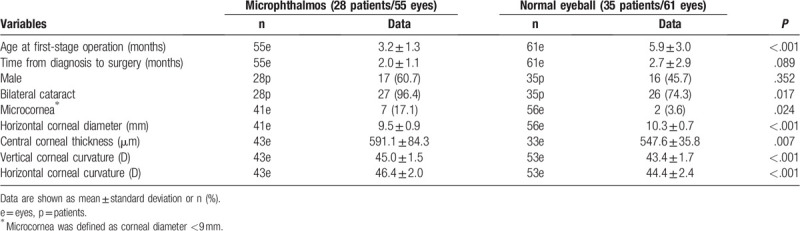
Table 1 presents the characteristics of the patients. There were 28 infants (55 eyes) in the microphthalmos group; they were 3.2 ± 1.3 months at first-stage operation; time from diagnosis to surgery was 2.0 ± 1.1 months; there were 17 males and 11 females. There were 35 infants (61 eyes) in the control group; they were 5.9 ± 3.0 months at first-stage operation; time from diagnosis to surgery was 2.7 ± 2.9 months; there were 16 males and 19 females.
Table 1.
Baseline characteristics.
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by Medical Ethics Committee of Qingdao Ophthalmological Hospital [2020(10)]. This article is a retrospective study. Therefore, the Institutional waived the requirement to obtain distinct written informed consent from the patients.
2.2. Treatment
Surgical treatment was performed as early as possible for infants with confirmed diagnosis. First-stage 3 combined surgeries were performed as phacoemulsification + circular posterior capsulotomy (about 4 mm in diameter, approached via the anterior segment using a 25G capsulotomy needle) + anterior vitrectomy. After first-stage surgery, the patients’ conditions were observed. When the infants were above 2 years, second-stage IOL implantation was performed with an AR40e lens placed in ciliary sulcus in case of suitable eye conditions (normal intraocular pressure [IOP] and ciliary groove width >12 mm). All surgeries were performed by the same chief physician. The complications were assessed, including capsulorhexis, posterior capsule rupture, crystals falling into the vitreous, and anterior chamber bleeding.
The instruments used included an ophthalmic ultrasonic diagnostic apparatus (MD-2300; Tianjin Maida, Tianjin, China), Icare tonometer (TA-03, Icare Finland Oy, Vantaa, Finland), hand-held slit lamp (KJ5S2; Kangjie Medical Co. Ltd, Suzhou, China), ophthalmoscope (Vantage Plus; Keeler, Windsor, United Kingdom), hand-held Auto REF/Keratometer (Handy REF-K; NIDEK, Tokyo, Japan), ultrasound biomicroscope (SW-3200L; Tianjin Suowei, Tianjin, China).
2.3. Follow-up
TY-G-A (Beijing Tongming Ophthalmic Instrument Development Co, Ltd, Beijing, China) was used to test the optokinetic nystagmus before and after the first-stage surgery. Infants were followed at 6, 12, 18, and 24 months after first-stage surgery and before second-stage IOL implantation. The follow-up visit included axial length, IOP, conditions of the anterior segment (including anterior chamber depth, aqueous flare, pupillary diameter, and pupillary adhesion), and conditions of the ocular fundus. If infants had abnormal intraocular hypertension, IOP-lowering eye drops were prescribed, and IOP was monitored and controlled within the normal range. If after-cataract was identified, YAG laser capsulotomy was performed immediately to keep the optical area transparent. All examinations were conducted and reviewed by 2 physicians (JW and LY). All retinoscopic examinations were performed and reviewed by 2 national first-class optometrists (YP and BY). The growth rate of the axial length was calculated as: (postoperative axial length - preoperative axial length)/(time from first-stage operation to postoperative follow-up [year]). The change rate in IOP was calculated as: (postoperative IOP - preoperative IOP)/ (time from first-stage operation to postoperative follow-up [year]).
2.4. Statistical analysis
Statistical analysis was performed using SPSS 16.0 (IBM, Armonk, NY). Continuous data are presented as means ± standard deviation and were analyzed using the Student t test or repeated measure ANOVA. Categorical data are presented as frequencies (percentage) and were analyzed using the chi-square test or Fisher exact test. Two-sided P-value <.05 was considered as statistically significant.
3. Results
3.1. Changes in visual acuity before/after the first-stage operation
The preoperative visual acuity was negative for optokinetic nystagmus, while the postoperative visual acuity was positive for optokinetic nystagmus in both groups.
3.2. Changes in axial length before/after the first-stage operation
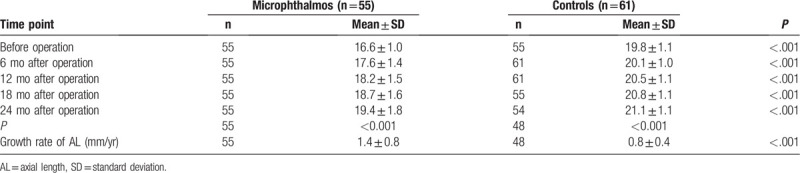
Table 2 presents the changes in axial length in the 2 groups. In the microphthalmos group, the axial length steadily increased from 16.6 ± 1.0 mm before the first-stage cataract surgery to 19.4 ± 1.8 mm at 24 months after operation (P < .001). In the control group, the axial length steadily increased from 19.8 ± 1.1 mm before the first-stage cataract surgery to 21.1 ± 1.1 mm at 24 months after operation (P < .001). The growth rate was significantly higher in the microphthalmos group than that in the control group (1.4 ± 0.8 vs 0.8 ± 0.4 mm/yr, P < .001). The axial length was significantly smaller in the microphthalmos group at all time points compared with the control group (P < .001).
Table 2.
Changes of AL (mm) in 2 groups.
3.3. Changes in intraocular pressure before/after the first-stage operation
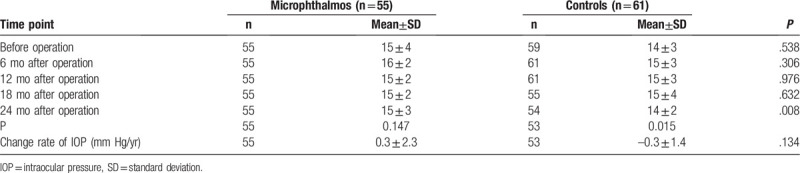
Table 3 presents the changes in IOP in the 2 groups. There was no changes in IOP in the microphthalmos group from baseline to 24 months (P = .147), but the IOP was slightly decreased in the control group (P = .015). There was no significant difference in the change rate of IOP between the 2 groups (P = .134). The IOP was lower in the control group at 24 months compared with the microphthalmos group (14 ± 2 vs 15 ± 3 mm Hg, P = .008).
Table 3.
Changes of IOP (mm Hg) in 2 groups.
3.4. Surgical complications
In the microphthalmos group, lens dislocation occurred in 2 infants during the first-stage operation. In the control group, anterior and posterior capsular rupture occurred in 1 patient during the first-stage operation. After the first-stage operation, in the microphthalmos group, 4 infants had increased IOP, one had corneal edema, one had hyphema, one had choroidal effusion, and one had posterior staphyloma. In the control group, 3 infants had increased IOP and four had posterior staphyloma.
4. Discussion
The axial length growth rate after the treatment of congenital cataract is controversial,[4–6] and no comparison was made between microphthalmos and normal-length eyeballs in infants with congenital cataract. Therefore, this study aimed to analyze the differences in ocular axis growth between complex microphthalmos and controls in infants under 1 year of age with congenital cataract after first-stage cataract surgery. The results suggest that the axial length growth rate is higher in complex microphthalmos compared with controls after first-stage operation for congenital cataract in infants <1 year of age.
The anatomical features of congenital cataract with complex microphthalmos include decreased eyeball volume, reduced axial length (<18 mm), mostly spherical lenses, increased volume ratio of lens to eyeball, possible microcornea, and shallow anterior chamber.[15,16] Patients with congenital microcornea often show a corneal diameter <9 mm, flattened cornea, and are often combined with cataract and coloboma of iris or choroid. Congenital cataract accompanied by complex microphthalmos or microcornea is often a nuclear cataract with difficulty in mydriasis, so that patients might have permanent amblyopia if not given early treatment. Due to the characteristic eyeball structures of congenital microphthalmos, the intervention for the cataract is of high difficulty and risk, and is likely to cause glaucoma, retinal detachment, and other serious complications.[17,18] Fortunately, novel approaches are available and result in good outcomes.[7–11]
Conventional intervention for congenital cataract include cataract extraction, posterior capsulotomy, and anterior vitrectomy in combination with IOL implantation,[19] but most authors believe that for safety reasons, the surgery should be performed in infants >2 years of age.[20] But patients under 2 years of age have a critical period of vision development, if persistent form deprivation occurs during this period, it can lead to severe visual impairment such as amblyopia and nystagmus. In the present study, the first stage of the intervention was carried out in infants <1 year of age and the second stage was performed when the infant was >2 years of age. Shallow anterior chamber and short ocular axis are the main reasons for the high incidence of postoperative complications.[7] Hence, axial length is important for making clinical decision in these patients, but also to ensure the success of the operation.[21] In normal eyeballs, operation for congenital cataract do not lead to eyeball growth retardation.[22] Shorter ocular axis before lens extraction is associated with faster ocular axis growth after surgery.[5,6] Accordingly, in the present study, the axial growth rate in the microphthalmos group was significantly higher than in normal eyeballs.
Complex microphthalmos combined cataract is often a nuclear cataract, and might develop into total cataract. Some cases may also have posterior capsule defects under dense nuclear opacity of the lens.[23] Thus, careful operation is required when performing hydrodissection and aspirating lens substance, thus preventing decrease of intraocular flow, sudden increase of IOP, and expansion of posterior capsule defect.[24] Secondary glaucoma is a common complication among infants undergoing cataract surgery; the onset of glaucoma should range from 10 days to 16.8 years after surgery, and the incidence is as high as 50%.[3,25,26] The main reasons for secondary glaucoma include pupil block, chronic angle closure caused by peripheral anterior synechia of the iris, and the deposition of diffusive pigment granules and crystallins at the trabecular meshwork that affects aqueous humor circulation. In a study by Prasad et al,[27] 5/37 microphthalmos developed glaucoma after surgery. Praveen et al,[28] showed a rate of glaucoma of 11/37. In the present study, some patients developed intraocular hypertension after surgery, and most of them were improved after conservative drug treatment. Globally, the IOP did not decrease over 24 months in the microphthalmos group, but did decrease slightly in the control group. Hence, the anatomy of the eye itself and the associated difficulty in operation due to the smaller structures could be involved in this difference, but additional studies are necessary.
This study suffers from some limitations. First, this was a retrospective study, with inherent shortcomings, for example, the lack of good controls for the microphthalmos group. In addition, the sample size was relatively small. Furthermore, an axial length of less than 18 mm in some patients may not necessarily reflect microphthalmos. In addition, the microphthalmos group had first operations significantly sooner than control individuals by several months. Moreover, though the axial length of patients with complex microphthalmos did increase during the 24-month follow-up, it also increases during the normal growing process of infants. Thus, the evaluation of surgery outcome lacked an effective control in this study.
In conclusion, the axial length growth rate is higher in complex microphthalmos compared with normal eyeballs after first-stage operation for congenital cataract in infants <1 year of age. This suggests that cataract surgery may contribute to the ocular axis growth in infants with complex microphthalmos.
Acknowledgments
The authors acknowledge the invaluable participation of the subjects.
Author contributions
J. Sun and L. Xie conceptualized the study. J. Sun performed data analysis and visualization, and wrote the manuscript. J. Zhang and L. Xie revised the manuscript. X. Wan, Y.Dai provided technical assistance. All authors read and approved the final manuscript.
Footnotes
Abbreviations: IOL = intraocular lens, IOP = intraocular pressure.
How to cite this article: Sun J, Zhang J, Dai Y, Wan X, Xie L. Cataract surgery contributes to ocular axis growth of aphakic eyes in infants with complex microphthalmos. Medicine. 2020;99:39(e22140).
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Apple DJ, Ram J, Foster A, et al. Elimination of cataract blindness: a global perspective entering the new millenium. Surv Ophthalmol 2000;45: Suppl 1: S1–96. [PubMed] [Google Scholar]
- [2].Khokhar SK, Dave V. Cataract surgery in infant eyes with microphthalmos. J Cataract Refract Surg 2009;35:1844–5. doi:10.1016/j.jcrs.2009.05.040. [DOI] [PubMed] [Google Scholar]
- [3].Sahin A, Caca I, Cingu AK, et al. Secondary glaucoma after pediatric cataract surgery. Int J Ophthalmol 2013;6:216–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wilson ME, Trivedi RH. Axial length measurement techniques in pediatric eyes with cataract. Saudi J Ophthalmol 2012;26:13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wilson ME, Trivedi RH, Weakley DR, et al. Globe axial length growth at age 5 years in the infant aphakia treatment study. Ophthalmology 2017;124:730–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Negalur M, Sachdeva V, Neriyanuri S, et al. Long-term outcomes following primary intraocular lens implantation in infants younger than 6 months. Indian J Ophthalmol 2018;66:1088–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Day AC, MacLaren RE, Bunce C, et al. Outcomes of phacoemulsification and intraocular lens implantation in microphthalmos and nanophthalmos. J Cataract Refract Surg 2013;39:87–96. [DOI] [PubMed] [Google Scholar]
- [8].Sharan S, Grigg JR, Higgins RA. Nanophthalmos: ultrasound biomicroscopy and Pentacam assessment of angle structures before and after cataract surgery. J Cataract Refract Surg 2006;32:1052–5. [DOI] [PubMed] [Google Scholar]
- [9].Bluwol E, Nordmann JP. Syndrome d’effusion uvéale après trabéculectomie chez une patiente nanophtalme [Uveal effusion syndrome in nanophthalmic eye after trabeculectomy]. J Fr Ophtalmol 2007;30:e13.doi:10.1016/s0181-5512(07)89637-9. [DOI] [PubMed] [Google Scholar]
- [10].Yu YS, Kim SJ, Choung HK. Posterior chamber intraocular lens implantation in pediatric cataract with microcornea and/or microphthalmos. Korean J Ophthalmol 2006;20:151–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sinskey RM, Amin P, Stoppel J. Intraocular lens implantation in microphthalmic patients. J Cataract Refract Surg 1992;18:480–4. [DOI] [PubMed] [Google Scholar]
- [12].Verma AS, Fitzpatrick DR. Anophthalmia and microphthalmia. Orphanet J Rare Dis 2007;2:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Elder JM. Aetiology of severe visual impairment and blindness in microphthalmos. Br J Ophthalmol 1994;78:332–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hussain RN, Shahid F, Woodruff G. Axial length in apparently normal pediatric eyes. Eur J Ophthalmol 2004;24:120–3. [DOI] [PubMed] [Google Scholar]
- [15].Lemos JA, Rodrigues P, Resende RA, et al. Cataract surgery in patients with nanophthalmos: results and complications 2004;30:584–90. [DOI] [PubMed] [Google Scholar]
- [16].Wu W, Dawson DG, Sugar A, et al. Cataract surgery in patients with nanophthalmos: results and complications. J Cataract Refract Surg 2004;30:584–90. [DOI] [PubMed] [Google Scholar]
- [17].Kang KD, Yim HB, Biglan AW. Comparison of delayed-onset glaucoma and early-onset glaucoma after infantile cataract surgery. Korean J Ophthalmol 2006;20:41–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Khan AO, Al-Dahmash S. Age at the time of cataract surgery and relative risk for aphakic glaucoma in nontraumatic infantile cataract. J Aapos 2009;13:166–9. [DOI] [PubMed] [Google Scholar]
- [19].Solebo AL, Russell-Eggitt I, Nischal KK, et al. Cataract surgery and primary intraocular lens implantation in children < or = 2 years old in the UK and Ireland: finding of national surveys. Br J Ophthalmol 2009;93:1495–8. [DOI] [PubMed] [Google Scholar]
- [20].Vasavada VA, Dixit NV, Ravat FA, et al. Intraoperative performance and postoperative outcomes of cataract surgery in infant eyes with microphthalmos. J Cataract Refract Surg 2009;35:519–28. [DOI] [PubMed] [Google Scholar]
- [21].Capozzi P, Morini C, Piga S, et al. Corneal curvature and axial length values in children with congenital/infantile cataract in the first 42 months of life. Invest Ophthalmol Vis Sci 2008;49:4774–8. [DOI] [PubMed] [Google Scholar]
- [22].Hussin HM, Markham R. Changes in axial length growth after congenital cataract surgery and intraocular lens implantation in children younger than 5 years. J Cataract Refract Surg 2009;35:1223–8. [DOI] [PubMed] [Google Scholar]
- [23].Ventura MC, Sampaio VV, Ventura BV, et al. Congenital cataract surgery with intraocular lens implantation in microphthalmic eyes: visual outcomes and complications. Mayo Clin Proc 2013;53:260–1. [DOI] [PubMed] [Google Scholar]
- [24].Yu YS, Jin HL, Chang BL. Surgical management of congenital cataract associated with severe microphthalmos. J Cataract Refract Surg 2000;26:1219–24. [DOI] [PubMed] [Google Scholar]
- [25].Nishina S, Noda E, Azuma N. Outcome of early surgery for bilateral congenital cataracts in eyes with microcornea. Am J Ophthalmol 2007;144:276–80. [DOI] [PubMed] [Google Scholar]
- [26].Chen D, Gong XH, Xie H, et al. The long-term anterior segment configuration after pediatric cataract surgery and the association with secondary glaucoma. Sci Rep 2017;7:43015.doi:10.1038/srep43015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Prasad S, Ram J, Sukhija J, et al. Cataract surgery in infants with microphthalmos. Graefes Arch Clin Exp Ophthalmol 2015;253:739–43. doi:10.1007/s00417-014-2908-8. [DOI] [PubMed] [Google Scholar]
- [28].Long-term postoperative outcomes after bilateral congenital cataract surgery in eyes with microphthalmos. J Cataract Refract Surg 2015;41:1910–8. [DOI] [PubMed] [Google Scholar]


