ABSTRACT
Objectives:
The aim of this study was to evaluate toothbrushing effectiveness in children with mild and moderate levels of severity of autism spectrum disorder (ASD) after using visual pedagogy.
Materials and Methods:
This quasi-experimental study was carried out with 30 children with ASD aged 5–17 years; 21 had mild ASD and 9 had moderate ASD. Informed consent and the subject’s demographic information were obtained from caregivers. All subjects were then asked to show their toothbrushing practices, which were recorded by video. The toothbrushing ability, toothbrushing cooperation, and plaque index were evaluated before the study and at 2 weeks, 4 weeks, 3 months, and 6 months after visual pedagogy had been used. Results were analyzed by the Friedman test, Pearson’s chi-square test, Fisher’s exact test, and Mann‒Whitney U test.
Results:
Toothbrushing ability was significantly improved at all periods of follow-up. Toothbrushing cooperation and the dental plaque index were significantly better than before the study at 4 weeks, 3 months, and 6 months of follow-up. The toothbrushing ability of subjects with mild ASD was significantly better than that of subjects with moderate ASD at 4 weeks and 6 months of follow-up. The toothbrushing cooperation of the mild group was significantly better than that of the moderate group at 2 weeks, 4 weeks, and 3 months. There was no statistically significant reduction in the plaque index between the two groups.
Conclusion:
Visual pedagogy is useful for improving toothbrushing effectiveness in children with mild or moderate severity ASD. However, children with moderate severity ASD take longer to improve.
KEYWORDS: Autism, autistic spectrum disorder, toothbrushing, visual pedagogy
INTRODUCTION
The autism spectrum disorder (ASD) encompasses a group of neurodevelopmental disabilities that diminish social interactions and communication and involve restrictive or repetitive patterns of behavior. The symptoms present in early childhood and impair daily functioning. Patients with different levels of severity of ASD show dissimilar characteristics. The diagnostic classification systems are used to screen and assess the symptoms. The severity classification can lead a psychiatrist to develop an individual teaching program for each patient. Children with severe ASD usually have severe deficits in verbal and nonverbal social communication and extreme difficulty in coping with change. They require more support than children with low levels of severity.[1,2]
Although patients with ASD have social and communication problems, they are able to learn from visual cues. Their visual processing is usually more effective than their audio or verbal processing.[3,4] Their understanding is heightened when visual formats such as pictures or short written words are used.[5] Visual pedagogy is a nontraditional approach to learning which composes of a set of coloring pictures accompanied with statements that guide patient with ASD to be familiar with the treatment tools and processes. It is part of the treatment and education of autistic and related communication-handicapped children (TEACCH) concept.[6] Visual pedagogy can help patients with ASD improve their learning ability both at home and at school. Rayner[7] and Marshall et al.[8] reported that a communicative technique or visual pedagogy was the most acceptable technique used by the parents of healthy or disabled children. There are several types of visual pedagogy, such as books with color photographs, social stories, and video modelling.[9,10,11]
Previous studies reported a higher prevalence of periodontitis in patients with ASD than in the general population. This is possibly due to a low compliance with dental care, limited motor skills, and the side effects of medications.[12,13,14,15,16] Moreover, the prevalence of dental caries in these children was lower than or similar to that of the typical population; however, it can be considered as high.[12,17,18,19] Therefore, preventive dental care is essential to prevent oral diseases in patients with ASD.
Regarding the routine oral care of patients with ASD, parents or caretakers usually complain about behavioral problems during brushing. The study of Pilebro and Backman[20] showed the use of visual pedagogy in subjects with ASD, and the results stated that it was a useful approach for oral hygiene instruction in these subjects. The studies did not mention the severity of ASD in the subjects who participated, and the researchers measured only the upper incisors and canine teeth, a fact that may have prevented reporting of the overall oral hygiene status. When we undertook this study, there had been no other study on the effectiveness of visual pedagogy in teaching oral hygiene for patients at different levels of severity of ASD. Therefore, this study aimed to evaluate toothbrushing effectiveness by assessing the toothbrushing ability, toothbrushing cooperation, and dental plaque reduction in children with ASD after using visual pedagogy and to compare the outcomes between children with mild and moderately severe levels of ASD.
MATERIAL AND METHODS
STUDY POPULATION
The sample size of this study was based on a study by Pilebro and Backman,[20] which evaluated visual pedagogy as a method of teaching oral hygiene to children with ASD. The results showed that the difference proportion was 0.8 and the estimate error in the calculation was 0.15. The calculated formula was the infinite population proportion. The total sample size of the formula was 28. After compensating for 10% dropout, the sample size in this study was 31 in total.
Children with ASD aged 5–17 years who were diagnosed with mild or moderate ASD by psychiatrists of the Child and Adolescent Mental Health Rajanagarindra Institute were invited into this study. The Childhood Autism Rating Scale standard version (CASRS2‒ST)[21] was used to classify the severity of the ASD. The severity level information was blinded to investigators by using ID code numbers instead of patients’ names. Exclusion criteria included children with ASD who had physical disabilities, severe psychiatric comorbidities, or severe behavior problems. Parents/caretakers of the patients were asked to give their consent for their children to participate in the study.
SELF-ASSESSMENT QUESTIONNAIRE
The self-assessment questionnaire was composed of questions regarding demographic information, medical treatment, previous dental experiences, and experience in using toothbrushing visual pedagogy. The reliability of the questionnaire was evaluated by the Cronbach method as 0.8. The questionnaire included binary yes/no answers and open-ended questions.
THE VISUAL PEDAGOGY FOR ORAL HYGIENE PRACTICE
The set of drawing pictures in the visual pedagogy was approved by a psychiatrist and the ethical committee. All of the pictures were sent to five specialists to test the Index of Item-Objective Congruence (IOC) before it was used in this study. All of the validity results had an IOC equal to 1.
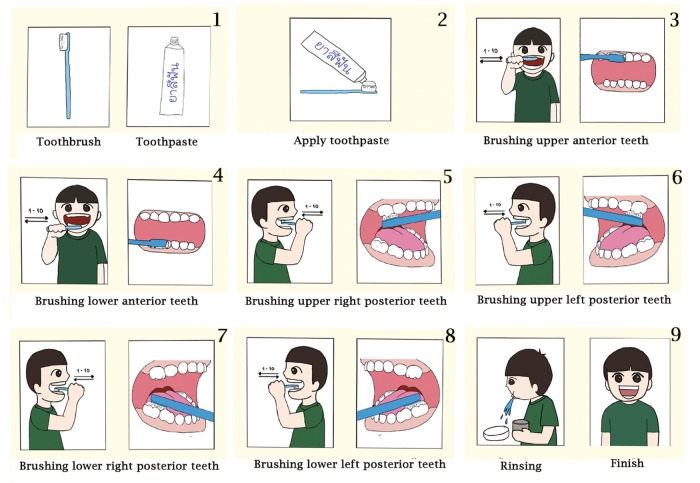
The visual pedagogy in this study had two formats: the visual pedagogy table calendar and visual pedagogy checklist board. The visual pedagogy table calendar consisted of nine pages of color pictures of toothbrushing steps in a table calendar format that could be set up in the bathroom or wherever children brushed their teeth, as shown in Figure 1. Each page contained one picture of 7cm × 9cm with a brief instruction at the bottom. The visual pedagogy table calendar was given to each subject for use at home. The visual pedagogy checklist board was used to guide subjects when brushing their teeth in the dental office. It had seven color pictures showing the six quadrants of the mouth that need brushing and minimal rinsing or splitting of remaining toothpaste. This was similar to the pictures in the table calendar except that the checklist did not show the toothbrush, toothpaste, or how to put the toothpaste on the toothbrush. Each 5cm × 4cm picture showed one step in the brushing of teeth. It was attached by a magnet to the vertical board [Figure 2]. As a child finished each step, the picture of that step was removed and placed in an attached box.
Figure 1.
Visual pedagogy table calendar
Figure 2.
Visual pedagogy check list board
DATA COLLECTION
After caretakers had completed a consent form and self-assessment questionnaire, all subjects were invited to enter the dental office at the Pediatric Dentistry Clinic, Faculty of Dentistry, Mahidol University. They were given toothbrushes to show how they usually practiced at home in front of a sink with running water. Their dental status and plaque index were recorded, according to the suggestions by LÖe and Silness.[22] The behavior and toothbrushing ability of each subject were recorded by a video recorder during all toothbrushing procedures. Then the visual pedagogy table calendars were given to subjects and their parents. Parents were advised on how to use visual pedagogy during toothbrushing and were encouraged to do so daily during brushing times.
Toothbrushing effectiveness was reevaluated for all subjects at 2 weeks, 4 weeks, 3 months, and 6 months after the first study visit. The children were invited into the dental office and asked to show their toothbrushing by using the pedagogy checklist that was coordinated with the brushing steps. After each step was performed, the picture of that step attached to the checklist board by a magnet was removed so that the subject would know that the step had been completed. Video recording was used during all procedures for analyzing the toothbrushing ability and subject’s cooperation.
OUTCOME
Primary outcome
The primary outcome was the score of toothbrushing ability after using the toothbrushing visual pedagogy from the time of the first study visit until the visit at 6 months of follow-up. There were seven main steps of evaluation of the toothbrushing ability: brushing the upper anterior teeth, upper left posterior teeth, upper right posterior teeth, lower anterior teeth, lower left posterior teeth, lower right posterior teeth, and minimal rinsing or splitting the remaining toothpaste. Each step had four scoring options, which were based on the study of Shin and Saeed:[23] score 0 = inability to complete the step, score 1 = dentist/parent completed the step for the individual, score 2 = a prompt was needed for the individual to complete the step, and score 3 = individual completed the step independently. Each complete step required that 10 strokes of brushing be recorded in each quadrant. The summary of the mean score of the toothbrushing practice was used as the toothbrushing ability score.
Secondary outcome
The secondary outcome was the score for toothbrushing cooperation and the plaque index after using the toothbrushing visual pedagogy from the time of the first study visit until the 6-month follow-up visit. Toothbrushing cooperation was recorded based on the Frankl behavior rating scale[24]: scale 1 = definitely negative to or refusal of toothbrushing, scale 2 = negative to or reluctance to accept toothbrushing, scale 3 = positive to or acceptance of toothbrushing, and scale 4 = definitely positive to or good rapport with caregiver. Moreover, the dental plaque index was evaluated with the mean plaque index, according to the Green and Vermilion’s[25] criteria as follows: score 0 = no debris or staining, score 1 = soft debris or extrinsic staining covering less than one third of the tooth surface, score 2 = soft debris or extrinsic staining covering more than one third but not less than two thirds of the tooth surface, and score 3 = soft debris or extrinsic staining covering more than two thirds of the tooth surface. The areas measured for the plaque index were the labial surfaces of teeth 16 or 55, 11 or 51, 26 or 65, and 31 or 71 and the lingual surfaces of teeth 36 or 75 and 46 or 85.
Outcome assessment
Each toothbrushing video recording was replayed for three evaluators, two postgraduate dentists and a pediatric dentist, for rating the toothbrushing ability and the cooperation during toothbrushing. The score was recorded based on agreement among two of the three evaluators.
STATISTICAL ANALYSIS
The Statistical Package for the Social Sciences (SPSS) software program, version 18.0 (SPSS, Chicago, Illinois) was used to analyze all data. The difference in oral hygiene practices from before the study to the end of the study was compared using the Friedman test over a 6-month interval. The differences in demographic characteristics in the two groups (i.e., gender, educational program, and medical treatment) were compared by using the Pearson chi-square test. If more than 20% of a cell had an expected count of less than 5, that group was compared by using the Fisher’s exact test. The differences in mean age, toothbrushing ability, plaque index, and toothbrushing cooperation in the dental office between the mild and moderate severity groups were analyzed by the Mann‒Whitney U test. A value of p < 0.05 was considered statistically significant.
RESULTS
For the three evaluators, the average intraclass correlation coefficient of toothbrushing ability was 0.98 and of toothbrushing behavior was 0.97. The average intraclass correlation coefficient of intraexaminer agreement on toothbrushing cooperation and toothbrushing ability of all three examiners was 1.00. The average intraclass correlation coefficient of the plaque index between two examiners was 0.81, and the intraexaminer coefficients were 0.96 and 0.94. The interexaminer and intraexaminer agreements on toothbrushing ability, toothbrushing cooperation, and plaque index examination were excellent.
SUBJECTS’ CHARACTERISTICS
Thirty-one children with ASD aged 5–17 years participated in this study with the consent of their parents or caregivers. One subject in the moderate severity group was excluded due to an extreme behavioral problem after a drug adjustment during follow-up visits. Therefore, a total of 30 children with ASD participated in this study from the first visit until the visit at 6 months of follow-up. They were 25 males (83.3%) and 5 females (16.7%). The mean age was 9.3 ± 3.5 years (age range, 5 to 16.25 years). Fifty percent of subjects had experienced using visual pedagogy in their behavior modification training, as is shown in Table 1.
Table 1.
Descriptive characteristics of study population
| Descriptive characteristic* | Total (N = 30) | ASD level of severity | ||
|---|---|---|---|---|
| Mild (N = 21) | Moderate (N = 9) | P Value | ||
| †Age (mean ± SD) | 9.3 ± 3.5 | 8.9 ± 3.5 | 10.4 ± 3.5 | 0.209 |
| Gender (N [%]) | 0.622 | |||
| Male | 25 (83.3%) | 18 (85.7%) | 7 (77.8%) | |
| Female | 5 (16.7%) | 3 (14.3%) | 2 (22.2%) | |
| Educational program (N [%]) | 0.065 | |||
| School for special needs children | 19 (63.3%) | 11 (52.4%) | 8 (88.9%) | |
| School for normal and special needs children | 11 (36.7%) | 10 (47.6%) | 1 (11.1%) | |
| Medical treatment (N [%]) | ||||
| Drug taken | 23 (76.7%) | 16 (53.3%) | 7 (23.3%) | 0.547 |
| Speech therapy | 27 (90.0%) | 18 (85.7%) | 9 (100.0%) | 0.328 |
| Behavior modification | 26 (86.7%) | 18 (85.7%) | 8 (80.0%) | 0.655 |
| Occupational therapy | 11 (36.7%) | 8 (38.1%) | 3 (33.3%) | 0.571 |
| Dental care experience | 0.514 | |||
| Yes | 23 (76.7%) | 17 (81.0%) | 6 (66.7%) | |
| No | 7 (23.3%) | 4 (19.0%) | 3 (33.3%) | |
| Experience using visual pedagogy | 1.000 | |||
| No | 15 (50%) | 10 (47.6%) | 5 (55.6%) | |
| Yes | 15 (50%) | 11 (52.4%) | 4 (44.4%) | |
ASD = autism spectrum disorder, SD = standard deviation
*The percentage of descriptive characteristics was calculated for the total subjects and each severity group
†The differences in mean age were analyzed by the Mann–Whitney U test, whereas other demographic characteristics were analyzed by the Fisher’s exact test at P < .05
According to the Childhood Autism Rating Scale standard version (CASRS2‒ST) used by the psychiatrists for the study, there were 21 subjects with mild ASD and 9 subjects with moderately severe ASD. The mean age, gender distribution, educational program, medical treatment, dental care experience, and experience of using visual pedagogy of each severity group are shown in Table 1. There was no statistical significance between the groups with mild or moderate levels of severity.
EFFECTIVENESS OF VISUAL PEDAGOGY FOR TOOTHBRUSHING IN ALL SUBJECTS
When compared with the toothbrushing practice at the first study visit, there was a statistically significant improvement in toothbrushing ability after 2 weeks, 4 weeks, 3 months, and 6 months of using visual pedagogy. However, there was no statistically significant difference during follow-up periods after using visual pedagogy as shown in Table 2. The overall toothbrushing cooperation and plaque index showed statistically significant improvement after 4 weeks, 3 months, and 6 months of using the visual pedagogy when compared with the baseline. Similarly, there was no statistically significant difference in the toothbrushing cooperation or plaque index during follow-up periods, except between 2 weeks and 6 months of follow-up [Table 2].
Table 2.
Toothbrushing effectiveness from baseline to 6 months of follow-up
| Period | Toothbrushing ability | Toothbrushing | Plaque index |
|---|---|---|---|
| (mean ± SD) | (mean ± SD) | (mean ± SD) | |
| Baseline | 0.6 ± 0.5a | 2.4 ± 0.8a | 1.8 ± 0.7a |
| F/U 2 weeks | 1.9 ± 1.0b | 2.8 ± 0.9a,b | 1.5 ± 0.8a,b |
| F/U 4 weeks | 2.2 ± 0.9b | 3.0 ± 0.9b,c | 1.2 ± 0.7b,c |
| F/U 3 months | 2.4 ± 0.7b | 3.4 ± 0.8b,c | 1.1 ± 0.7b,c |
| F/U 6 months | 2.4 ± 0.8b | 3.5 ± 0.7c | 0.6 ± 0.3c |
SD = standard deviation
Different superscript symbols (a, b, c) in each column indicate the statistically significant difference between follow-up periods at P < .05
Differences between the groups with mild and moderate severity ASD in toothbrushing effectiveness
Toothbrushing ability
The toothbrushing ability of subjects in the mild group was statistically better than for those in the moderate group at baseline and after 4 weeks and 6 months of using the toothbrushing visual pedagogy [Table 3].
Table 3.
Differences in toothbrushing effectiveness between the groups with mild and moderate severity autism spectrum disorder
| Mild severity group (N = 21) | Moderate severity group (N = 9) | P Value | |
|---|---|---|---|
| Toothbrushing ability (mean ± SD) | |||
| • Baseline | 0.7 ± 0.5 | 0.3 ± 0.2 | .032* |
| • F/U 2 weeks | 2.1 ± 1.0 | 1.4 ± 0.9 | .094 |
| • F/U 4 weeks | 2.4 ± 0.8 | 1.6 ± 0.6 | .036* |
| • F/U 3 months | 2.5 ± 0.7 | 2.1 ± 0.7 | .077 |
| • F/U 6 months | 2.6 ± 0.6 | 1.9 ± 0.8 | .045* |
| Toothbrushing cooperation (mean ± SD) | |||
| • Baseline | 2.5 ± 0.9 | 2.1 ± 0.6 | .349 |
| • F/U 2 weeks | 3.0 ± 0.9 | 2.3 ± 0.7 | .045* |
| • F/U 4 weeks | 3.2 ± 1.0 | 2.6 ± 0.5 | .032* |
| • F/U 3 months | 3.6 ± 0.7 | 2.8 ± 0.7 | .005* |
| • F/U 6 months | 3.6 ± 0.5 | 3.1 ± 1.1 | .326 |
| Plaque index (mean ± SD) | |||
| • Baseline | 1.6 ± 0.6 | 2.1 ± 0.7 | .086 |
| • F/U 2 weeks | 1.4 ± 0.8 | 1.6 ± 0.8 | .397 |
| • F/U 4 weeks | 1.1 ± 0.7 | 1.3 ± 0.7 | .349 |
| • F/U 3 months | 1.1 ± 0.7 | 1.0 ± 0.4 | .859 |
| • F/U 6 months | 0.7 ± 0.3 | 0.6 ± 0.4 | .476 |
SD = standard deviation
*Significant differences between groups as found by the Mann‒Whitney U test at P < .05
Toothbrushing cooperation
At the first study visit, there was no significant difference in the Frankl behavior score between the mild and moderate groups. The results showed that most of the subjects refused to brush their teeth or were reluctant to do so. The Frankl behavior score of the mild group was significantly higher than that of the moderate group, however, at 2 weeks, 4 weeks, and 3 months after using the toothbrushing visual pedagogy. The Frankl behavior score for the mild group was similar to that of the moderate group after 6 months of using the toothbrushing visual pedagogy, as presented in Table 3.
Dental plaque index
Regarding the dental plaque index evaluation, the mean plaque index of subjects in the mild group was slightly lower than that of the moderate group. However, there was no statistically significant difference between the mild and moderate groups [Table 3].
DISCUSSION
At the first study visit, most of the subjects with ASD were incapable of controlling a toothbrush, and had inappropriate toothbrushing practices. Of the parents/caretakers, 22 (73.3%) were unable to help the child complete toothbrushing correctly. This finding is consistent with previous studies,[2,26,27,28,29,30] which mentioned that fine and gross motor impairments, mental disabilities, and sensory problems, as well as the need for parent/caregiver involvement, were barriers to the daily toothbrushing of patients with ASD. Furthermore, 63% of the subjects with ASD were classified as having uncooperative behavior because of crying, aggressive behavior, and gagging during toothbrushing. These behaviors were probably due to sensory problems, anxiety, and emotional impairment.[2,27,28,29] In addition, the mean plaque index at the beginning of the study was 1.8 ± 0.7, which showed poor oral hygiene status of subjects. This finding was similar to some other studies, which reported that patients with ASD usually suffered from gingivitis, periodontitis, and discomfort owing to poor oral hygiene practices.[14,15] After using the toothbrushing visual pedagogy, the results of this study showed that the overall toothbrushing ability, toothbrushing cooperation, and plaque index had significantly improved from baseline until 6 months of follow-up. These findings reinforced the results of previous studies[6,20] which stated that visual pedagogy was useful for instructing children with ASD in the practice of beneficial oral hygiene.
This study was the first one to compare the improvement in children with mild and moderately severe ASD. Although those in the moderate severity group had significantly less toothbrushing ability than those in the mild severity group at the beginning of the study, they showed a significant improvement after using the toothbrushing visual pedagogy; in fact, the improvement was similar to that of the mild severity group. The toothbrushing cooperation of the mild group was significantly better than that of the moderate group at 2 weeks of follow-up. Subjects in the moderate severity group required a longer time to improve their cooperation during toothbrushing; they showed positive behavior at 6 months after using visual pedagogy. All of the subjects showed plaque reduction in all areas without a statistically significant difference between the mild and moderate severity groups.
The reduction in the plaque index in the mild severity group was the result of improved toothbrushing ability because the mean score for toothbrushing ability at 6 months of follow-up was 2.6. The plaque reduction in the moderate severity group could have been the outcome of brushing by parents because the mean score for toothbrushing ability was 1.8. Therefore, the effectiveness of the toothbrushing of subjects in the moderate group did not truly represent their ability after 6 months of using visual pedagogy. Their parents reported that the toothbrushing ability and cooperation at home of some children with moderately severe ASD did improve, but they still required support from caretakers due to their limited cooperation.
There are several forms of visual pedagogy that can promote engagement in productive activities and reduce confusion and distress during toothbrushing.[6,20] The form of visual pedagogy used in this study was not similar to the forms used in previous studies.[20,31] It consisted of a set of drawing pictures, one for each page, showing a step-by-step process of toothbrushing, with clear short descriptions and set up in the style of a table calendar. Most parents mentioned that the toothbrushing pictures with a clear background attracted their child’s attention and helped the child to readily participate in toothbrushing at home. This result was similar to that of Mah and Tsang’s[31] study, which suggested that using a system of visual cues, along with weekly visits, helped patients with ASD to successfully complete more dental procedures in the dental office.
The limitation of this study was an unequal sample size between the two severity groups due to the limited number of subjects with ASD who were able to participate, especially subjects with moderate severity ASD. If more subjects in the moderate severity group had been able to participate, the results would have been more precise.
CONCLUSION
After using a toothbrushing visual pedagogy for 6 months, the results from this study showed that
The overall toothbrushing ability, toothbrushing cooperation, and dental plaque index were improved in children with either mild or moderate severity ASD.
-
Comparisons between the mild and moderate severity groups showed that
-
2.1
The toothbrushing ability of subjects in the mild group was significantly better than that in the moderate severity group at baseline, 4 weeks, and 6 months. The mild severity group tended to be able to brush independently, whereas the moderate severity group tended to require caretaker assistance during toothbrushing at 6 months of follow-up.
-
2.2
The toothbrushing cooperation of the mild group was significantly better than that of the moderate severity group at 2 weeks, 4 weeks, and 3 months.
-
2.3
There was no statistically significant difference in the plaque index reduction between the mild and moderately severe groups.
-
2.1
FINANCIAL SUPPORT AND SPONSORSHIP
This study was supported by Mahidol University Faculty of Dentistry Grant (2018).
CONFLICTS OF INTEREST
There are no conflicts of interest.
AUTHORS CONTRIBUTIONS
AS and TK contributed to the development of study design. AS, TK, ST, and WW collected data. AS, TK, PR, and NS participated in data analysis. AS and TK are responsible for manuscript preparation.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
This quasi-experimental study was approved by the Institutional Review Board (IRB), Faculty of Dentistry and Faculty of Pharmacy, Mahidol University, Bangkok, Thailand (COA.N0.MU-DT/PY-IRB 2018/010.0202), and the Thai Clinical Trial Registry (TCTR20181115009).
PATIENT DECLARATION OF CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
DATA AVAILABILITY STATEMENT
The additional data of this study are available on request from Apiwan Smutkeeree at apiwan.dan@mahidol.ac.th.
ACKNOWLEDGEMENT
The authors acknowledge Dr. Matana Kettratad for her useful discussion. The authors would like to thank all the staffs of Child and Adolescent Mental Health Rajanagarindra Institute and Pediatric Dental Clinic, Faculty of Dentistry, Mahidol University for their valuable support throughout the study.
REFERENCES
- 1.Grant R, Nozyce M. Proposed changes to the American Psychiatric Association diagnostic criteria for autism spectrum disorder: Implications for young children and their families. Matern Child Health J. 2013;17:586–92. doi: 10.1007/s10995-013-1250-9. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM–5) Washington, DC: American Psychiatric Publishing; 2013. p. 947. [Google Scholar]
- 3.Mesibov GB, Shea V. The TEACCH program in the era of evidence‒based practice. J Autism Dev Disord. 2010;40:570–9. doi: 10.1007/s10803-009-0901-6. [DOI] [PubMed] [Google Scholar]
- 4.Santangelo SL, Tsatsanis K. What is known about autism: Genes, brain, and behavior. Am J Pharmacogenomics. 2005;5:71–92. doi: 10.2165/00129785-200505020-00001. [DOI] [PubMed] [Google Scholar]
- 5.Friedlander AH, Yagiela JA, Paterno VI, Mahler ME. The pathophysiology, medical management, and dental implications of autism. J Calif Dent Assoc. 2003;3:681–91. [PubMed] [Google Scholar]
- 6.Backman B, Pilebro C. Visual pedagogy in dentistry for children with autism. ASDC J Dent Child. 1999;66:325–31. [PubMed] [Google Scholar]
- 7.Rayner CS. Video‒modelling to improve task completion in a child with autism. Dev Neurorehabil. 2010;13:225–30. doi: 10.3109/17518421003801489. [DOI] [PubMed] [Google Scholar]
- 8.Marshall J, Sheller B, Mancl L, Williams BJ. Parental attitudes regarding behavior guidance of dental patients with autism. Pediatr Dent. 2008;30:400–7. [PubMed] [Google Scholar]
- 9.Nelson TM, Sheller B, Friedman CS, Bernier R. Educational and therapeutic behavioral approaches to providing dental care for patients with Autism Spectrum Disorder. Spec Care Dentist. 2015;35:105–13. doi: 10.1111/scd.12101. [DOI] [PubMed] [Google Scholar]
- 10.Meadan H, Ostrosky MM, Triplett B, Michna B, Fettig A. Using visual supports with young children with autism spectrum disorder. Teach Except Child. 2011;43:28–35. [Google Scholar]
- 11.Green D, Flanagan D. Understanding the autistic dental patient. Gen Dent. 2008;56:167–71. [PubMed] [Google Scholar]
- 12.Silva SN, Gimenez T, Souza RC, Mello-Moura ACV, Raggio DP, Morimoto S, et al. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int J Paediatr Dent. 2017;27:388–98. doi: 10.1111/ipd.12274. [DOI] [PubMed] [Google Scholar]
- 13.Lowe O, Lindemann R. Assessment of the autistic patient’s dental needs and ability to undergo dental examination. ASDC J Dent Child. 1985;52:29–35. [PubMed] [Google Scholar]
- 14.Power TJ, Radcliffe J. The relationship of play behavior to cognitive ability in developmentally disabled preschoolers. J Autism Dev Disord. 1989;19:97–107. doi: 10.1007/BF02212721. [DOI] [PubMed] [Google Scholar]
- 15.Kopycka‒Kedzierawski DT, Auinger P. Dental needs and status of autistic children: Results from the National Survey of Children’s Health. Pediatr Dent. 2008;30:54–8. [PubMed] [Google Scholar]
- 16.Klein U, Nowak AJ. Autistic disorder: A review for the pediatric dentist. Pediatr Dent. 1998;20:312–17. [PubMed] [Google Scholar]
- 17.Loo CY, Graham RM, Hughes CV. The caries experience and behavior of dental patients with autism spectrum disorder. J Am Dent Assoc. 2008;139:1518–24. doi: 10.14219/jada.archive.2008.0078. [DOI] [PubMed] [Google Scholar]
- 18.Kamen S, Skier J. Dental management of the autistic child. Spec Care Dentist. 1985;5:20–3. doi: 10.1111/j.1754-4505.1985.tb00928.x. [DOI] [PubMed] [Google Scholar]
- 19.Jaber MA, Sayyab M, Abu Fanas SH. Oral health status and dental needs of autistic children and young adults. J Investig Clin Dent. 2011;2:57–62. doi: 10.1111/j.2041-1626.2010.00030.x. [DOI] [PubMed] [Google Scholar]
- 20.Pilebro C, Backman B. Teaching oral hygiene to children with autism. Int J Paediatr Dent. 2005;15:1–9. doi: 10.1111/j.1365-263X.2005.00589.x. [DOI] [PubMed] [Google Scholar]
- 21.Schopler E, Van Bourgondien ME, Wellman GJ, Love SR. The Childhood Autism Rating Scale. Los Angeles, CA: Western Psychological Services; 2010. p. 109. [Google Scholar]
- 22.LÖe H, Silnes J. The gingival index, the plaque index and retention index system. J Periodontol. 1967;38:610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 23.Shin CJ, Saeed S. Tooth brushing barriers for people with developmental disabilities: A pilot study. Spec Care Dentist. 2013;33:269–74. doi: 10.1111/scd.12024. [DOI] [PubMed] [Google Scholar]
- 24.Wright GZ, Stigers JI. Nonpharmacologic management of children’s behaviors. In: Dean JA, Avery DR, McDonald RE, editors. McDonald and Avery’s Dentistry for the Child and Adolescent. 9th ed. Maryland, MO: Mosby–Elsevier; 2011. pp. 27–40. [Google Scholar]
- 25.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 26.Dawson G, Watling R. Interventions to facilitate auditory, visual, and motor integration in autism: A review of the evidence. J Autism Dev Disord. 2000;30:415–21. doi: 10.1023/a:1005547422749. [DOI] [PubMed] [Google Scholar]
- 27.Stein LI, Polido JC, Mailloux Z, Coleman GG, Cermak SA. Oral care and sensory sensitivities in children with autism spectrum disorders. Spec Care Dentist. 2011;31:102–10. doi: 10.1111/j.1754-4505.2011.00187.x. [DOI] [PubMed] [Google Scholar]
- 28.Stein LI, Polido JC, Cermak SA. Oral care and sensory concerns in autism. Am J Occup Ther. 2012;66:73–6. doi: 10.5014/ajot.2012.004085. [DOI] [PubMed] [Google Scholar]
- 29.Stein LI, Polido JC, Cermak SA. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent. 2013;35:230–5. [PubMed] [Google Scholar]
- 30.Kuhaneck HM, Chisholm EC. Improving dental visits for individuals with autism spectrum disorders through an understanding of sensory processing. Spec Care Dentist. 2012;32:229–33. doi: 10.1111/j.1754-4505.2012.00283.x. [DOI] [PubMed] [Google Scholar]
- 31.Mah JW, Tsang P. Visual schedule system in dental care for patients with autism: A pilot study. J Clin Pediatr Dent. 2016;40:393–9. doi: 10.17796/1053-4628-40.5.393. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The additional data of this study are available on request from Apiwan Smutkeeree at apiwan.dan@mahidol.ac.th.