Abstract
Purpose
Bladder neck contracture is an annoying problem for patients as well as urologists. Recurrence still remains a common problem associated with significant morbidity. This study evaluated the efficacy and side effects of mitomycin C (MMC) which has anti-fibroblast as well as anti-collagen properties in the deterrence of bladder neck contracture (BNC) recurrence after transurethral bladder neck resection (TUBNR).
Materials and Methods
Ten patients between March 2017 and April 2018 with extremely persistent BNCs who underwent multiple failed endoscopic procedures (≥3 times) were evaluated by using International Prostate Symptom Score (IPPS), uroflowmetry, quality of life (QOL) and post void residual urine (PVR) preoperatively. All patients underwent transurethral bladder neck resection (TUBNR) followed by ten-point intraoperative MMC injection, not exceeding a total dose of 2 mg (0.2 mg/mL), which was given circumferentially at the resected site, using Williams cystoscopic needle. Patients were reviewed at 3 months, 6 months, 1 year and 2 years postoperatively.
Results
The procedure was done on a day care basis. The recurrence period prior to our treatment was 3.2 ± 1.3 months. The follow-up was for 24 months. Overall 80% (8 of 10) of patients demonstrated resolution of BNCs as well as sufficient flow rate which was evaluated by uroflowmetry, PVR, IPPS and QoL postoperatively. One patient had detrusor underactivity. Relapse was seen in two patients. None of the patients experienced any significant adverse effects related to MMC.
Conclusion
Intraoperative ten-site injection of MMC after TUBNR can be regarded as a safe and efficient technique with no serious adverse event.
Keywords: bladder neck contracture, mitomycin c, scar modulators, transurethral resection of prostate, Williams cystoscopic needle
Introduction
Benign prostatic hyperplasia (BPH) is a frequent condition encountered in genitourinary medicine. Transurethral resection of the prostate (TURP) is a recognized common urological procedure done for BPH. However, bladder neck contracture (BNC) is a well documented problem following TURP, varying from 1 to 9.7%.1 Even though the majority of patients can be treated productively with endoscopic technique, development of refractory BNC accounts for 27% of patients requiring multiple and complex management, and eventually, may end up in open reconstruction.2 However, the scar hypertrophy was deemed to be the exact reason for recurrent BNC. Recently, intraoperative treatment with Mitomycin C (MMC), that decreases collagen deposition has been studied.
MMC, a DNA cross-linker that has anti fibroblast properties, potentially leads to apoptosis and helps to prevent recurrent BNC.3 Therefore, in the present study, we carried out transurethral resection of bladder neck scar tissues along with administration of cystoscopy guided intraoperative MMC injections at the resection sites. We evaluated the wellbeing as well as effectiveness of this procedure in the management of BNCs in post TURP patients.
Materials and Methods
This study complied with the Declaration of Helsinki and was approved by the Institutional ethics committee as a clinical study at the Apollo Hospital, Chennai. It was conducted between March 2017 and April 2018. Written consent was obtained from all patients with recurrent BNCs (≥3 times) prior to the procedure. Ten patients with post TURP refractory BNCs underwent the procedure. It was performed by the same surgeon. The patient’s IPPSs, QOL, uroflowmetry (Q max, Q ave), PVR and cystourethroscopy findings were used for diagnosis of BNC.4,5 For comparison with preoperative results, IPSSs, QOL, PVR, Q ave and uroflowmetry (Q max) were repeated 3 months, 6 months, one year and two years following surgery.
Surgical Technique
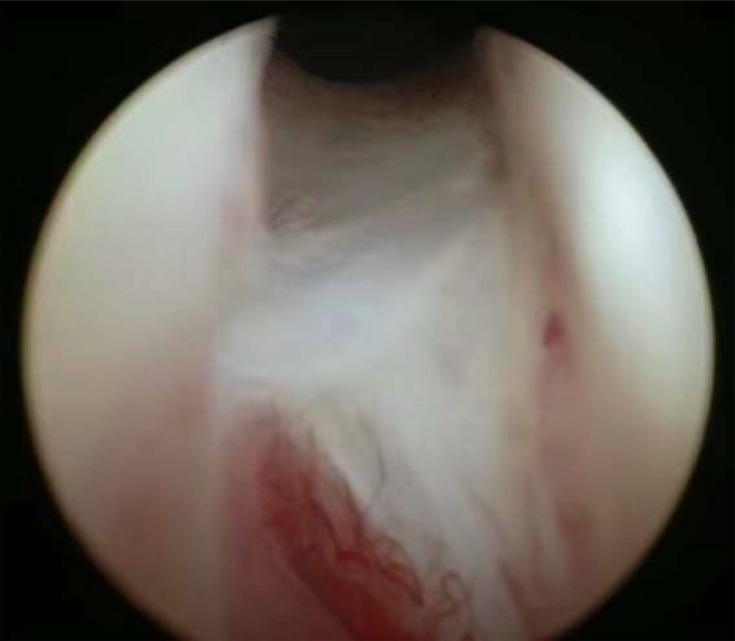
Under general anesthesia, surgery was carried out in all ten patients in the lithotomy position. Using 22Fr sheath 30 degree cystoscopy was done. The sequential visualization of anterior urethra, posterior urethra, Verumontanum and post TURP status of prostatic fossa were assessed. Bladder neck tight contracture was present in all patients as well as not allowing the scope to advance beyond it (Figure 1). Anterior urethrotomy was done using Otis uretherotome for all cases up to 30 Fr to accommodate the resectoscope. By using 24Fr intermittent resectoscope and 1.5% glycine as irrigant, bladder neck scar was initially incised at 5 and 7 o'clock positions to gain entry across the contracture into the bladder using a Collin’s Knife and monopolar current.
Figure 1.
Bladder neck contracture.
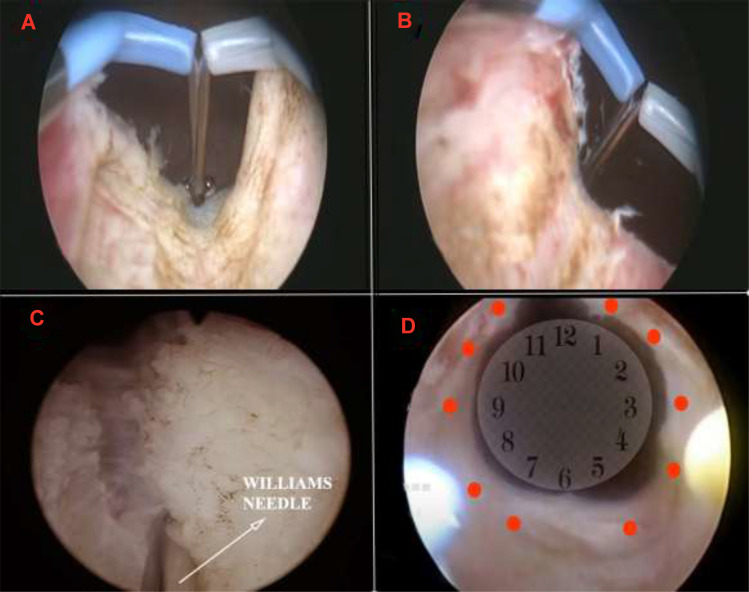
The intervening bladder neck was resected with a loop electrocautery (from 3 o’clock to 9 o’clock position) up-to perivesical fat. Complete hemostasis was secured. Bladder neck chips were evacuated using Ellick’s evacuator. Resectoscope was removed after securing hemostasis and a 22Fr cystoscope sheath was deployed into the bladder, through which the Williams needle was introduced up to the bladder neck. Injection Mitomycin C (2 mg) was diluted in 10 mL of distilled water and thus constituting 0.2 mg per mL.
One mL of reconstituted MMC was injected circumferentially into the resected bladder neck at 10 sites, using Williams cystoscope needle (Figure 2). Intraoperative image depicting the ten sites of injection (1, 2, 3, 4, 5, 7, 8, 9, 10, and11 o’clock positions) are shown in (Figure 3). A 22Fr - three way foley was deployed and irrigation was started. Irrigations were stopped after 6 hours.
Figure 2.
A Williams cystoscope needle.
Figure 3.
Intraoperative images. (A) and (B) BNC incisions. (C) Injection of MMC using a Williams needle. (D) Red dots denoting ten sites of injection.
Patients were discharged as day-care with indwelling foley, which was removed on POD-10. The patients were assessed postoperatively at 3 months, 6 months, 1 year and 2 year with IPSS, QoL, Q ave, Q max, and PVR. Complications like infections, incontinence of urine as well as hematuria were assessed.
SPSS version 20.0 was used for statistical analysis. Continuous variables are represented as mean ± standard deviations. Repeated ANOVA test was used to find out if variables changed drastically over time. The differences were done to compare parameters between the follow-up period and the baseline. Differences were considered to be statistically significant if the p-value < 0.05.
Results
All ten patients successfully completed the study. The median patient age was 63.2 years. The intraoperative BNC pictures are illustrated in Figure 3. Patients recurrence period before our surgical technique was a mean of 3.2± 1.3 months. Bladder neck was having near total blockage with scar tissue in all the patients. The mean operative time was 20 ± 5.5 minutes.
Foley was removed on 10th POD as per institutional protocol. Outcomes with regard of Q ave, Q max, PVR, IPSS and QoL are mentioned in Table 1. On subsequent visits, the Q max as well as Q ave augmented following surgery, while PVR, QoL and IPSS declined at 3 months, 6 months, 1 year and 2 years after surgery. On follow up of the ten patients with BNCs, seven patients (70%) showed no recurrence after the procedure at 3 months. The histopathology report in all the patients showed chronic inflammation and adenomatous hyperplasia with cystitis in three patients.
Table 1.
Preoperative and Postoper+ative Variables
| Parameters | Baseline (n=10) | 3 months (n=10) | 6 months (n=10) | 12 months (n=10) | 24 months (n==10) |
|---|---|---|---|---|---|
| Q max | 6.36±1.7 | 19.6±3.5* | 17.7±4.6* | 18.6±3.4* | 15.9±3.2* |
| Q ave | 0.9±0.8 | 10.6±2.4* | 11.9±2.7* | 12.2±3.6* | 10.±2.4* |
| IPPS | 24.4±4.2 | 6.3±1.4* | 7.2±2.8* | 7.7±4.0* | 8.1±4.2* |
| QOL | 4.3±1.0 | 1.3±0.6* | 1.9±1.3* | 2.1±1.3* | 2.8±1.4* |
| PVR | 128.7±13.2 | 24.7±4.1* | 29.3±3.4* | 32.4±2.7* | 34.8±3.6* |
Notes: Results are reported as mean ± standard deviation. *Significant difference compared with baseline, p < 0.05.
Abbreviations: Q max, maximum urinary flow rate; Q ave, average urinary flow rate; QoL, quality of life; PVR, postvoid residual urine; ANOVA, analysis of variance; BNC, bladder neck contracture; CIC, clean intermittent catheterization; IPPS, International Prostate Symptom Score; MMC, mitomycin C; PVR, post void residual urine; POD, post operative day; Q ave, average urinary flow rate; Q max, maximum urinary flow rate; QoL, quality of life; TUBNI, transurethral bladder neck incision; TUBNR, transurethral bladder neck resection; TURP, transurethral resection of prostate.
Nevertheless, three patients reported painful micturition, diminished Q max as well as Q ave at 3 months and continued to worsen at 6 months after surgery. On further flexi-cystoscopic examination, there was recurrence of BNC in two patients and one patient showed no obstruction. On further urodynamic evaluation, detrusor underactiviy was discovered in one patient. However, the severity was lesser than primary BNC in two of the other patients. One patient underwent repeat transurethral Bbladder neck resection (TUBNR) with MMC injection at 6 months, and is currently on follow up with no recurrence at 18 months post second procedure. Other patients refused further surgery, therefore, we advised to be on CIC.
Complications were documented during follow-up which include, dysuria 4 (40%), transient hematuria 2 (20%) and urge incontinence 1 (10%). After symptomatic management, complications were resolved. In the present study, we observed no significant harmful events linked to MMC. The overall success rate was 80% at 24 months follow-up.
Discussion
BNC is not an uncommon complication following transurethral prostate surgeries.6,7 Approximately 27% BNC patients progress to refractory stenosis extremely resistant to conventional treatment, with successful 0–20% proportion following subsequent urethrotomy or dilation.8,9
Recurrent BNC becomes a major indelible problem for patients. It frequently makes patients undergo multiple repeated surgeries with a decreased possibility of permanent solution with each successive treatment. As a result, significant morbidity and poor quality of life will occur.10 To treat the refractory BNC, minimally invasive procedures such as TUBNI, offers a quicker recovery. However, the success rate is less than open reconstruction.
Nonetheless, several centers have promoted the usage of adjuvant immune modulators such as triamcinolone and scar modulators like MMC along with TUBNI in an effort to decrease scar formation at the bladder neck. In this study, we carried out simultaneous TUBNR and intraoperative injection of MMC in the neck of bladder.
In 1950, MMC was discovered by Japanese scientists in the culture of Streptomyces caespitosus microorganism. It inhibits collagen deposition and fibroblast proliferation, thereby decreasing scar formation.3 It is also utilized as a chemotherapeutic drug by virtue of its antitumor activity. It is administered intravenously to manage upper gastro-intestinal cancers, anal, breast cancer, as well as by bladder instillment for superficial bladder malignancy.
In spite of having these benefits, MMC has few potential complications coupled with administration of a single dosage such as urinary retention, pain, urinary tract infections, transient irritative bladder symptoms, asymptomatic perivesical inflammation, incontinence, cystitis, and rarely urethral necrosis. The most regular complication following even a single dosage of MMC is aseptic cystitis, present as urinary urgency, frequency and dysuria.11
Vanni et al,14 with their study showed 72% success in 18 patients managed with deep cold-knife incision subsequently with MMC injection. Triamcinolone acetonide as well as MMC lowers scar proliferation. Eltahawy et al13 reported an 83% success rate in 24 patients who were managed with Ho laser BNC incision at 3 o’clock as well as 9 o’clock, and subsequently with steroid injection of 80 mg triamcinolone.
However, MMC injection may result in serious adverse events and showed limited value with intralesional MMC injection at the transurethral incision of BNC as reported by Redshaw et al,12 In addition, Ramirez et al15, and Brede et al performed deep incision for BNC using two different techniques such as electrocautery and cold knife. They reported overall success of 86% and 70% respectively.
In our present study, we included a total of ten patients who had TUBNR+MMC injection procedures with 80% comprehensive success rate. The technique was simple and results were promising. It showed a firm bladder neck in 80% patients following TUBNR+ MMC at a follow up of 2 years which was almost in concordance with Eltahawy et al,13 and Vanni et al.14 There were no major significant MMC-related adverse reactions reported in our study which is in contrast to Redshaw et al.12 In our study, we used monopolar electrocautery. However, Ramirez et al15 and Brede et al performed deep incision for BNC using two different techniques (electrocautery vs cold knife). They reported a primary success rate of 72% and 70% respectively.
Limitatons of the Study
Limitations of our study were the small number of cases and lack of a control group. Unfortunately, no standardized management has yet been proposed, which clarifies the absence of a control group.
Conclusion
To conclude, TUBNR combined with intra-operative MMC injections for refractory BNCs in post TURP patients showed an 80% successful rate in this present study group. Our method is safe, trouble-free, effective, simple to perform and complications are insignificant. Moreover, further robust randomized control studies with statistically significant sample sizes and with lengthier follow-up period are essential to verify the effectiveness of this procedure.
Funding Statement
There is no funding to report.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Ethical Committee Approval
Ethics approval for the study was given by the “Institutional Ethics Committee - Clinical Studies.” The procedures and the ethical clearance were in accordance with the Helsinki declaration.
Consent for Publication
Written consent was obtained from the participants in the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Zhang L, Liu S, Wu K, Mu X, Yang L. Management of highly recurrent bladder neck contractures via transurethral resection combined with intra-and post-operative triamcinolone acetonide injections. World J Urol. 2020;4:1–6. [DOI] [PubMed] [Google Scholar]
- 2.Lyon TD, Ayyash OM, Ferroni MC, Rycyna KJ, Chen ML. Bipolar transurethral incision of bladder neck stenoses with mitomycin C injection. Adv Urol. 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferguson B, Gray SD, Thibeault S. Time and dose effects of mitomycin C on extracellular matrix fibroblasts and proteins. Laryngoscope. 2005;115(1):110–115. doi: 10.1097/01.mlg.0000150694.08259.80 [DOI] [PubMed] [Google Scholar]
- 4.Kovell RC, Terlecki RP. Management strategies for post-prostatectomy bladder neck contractures. Curr Urol Rep. 2015;16(9):65. doi: 10.1007/s11934-015-0536-4 [DOI] [PubMed] [Google Scholar]
- 5.Reiss CP, Rosenbaum CM, Becker A, et al. The T- plasty: a modified YV-plasty for highly recurrent bladder neck contracture after transurethral surgery for benign hyperplasia of the prostate: clinical outcome and patient satisfaction. World J Urol. 2016;34(10):1437–1442. doi: 10.1007/s00345-016-1779-5 [DOI] [PubMed] [Google Scholar]
- 6.Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)—incidence, management, and prevention. Eur Urol. 2006;50(5):969–980. doi: 10.1016/j.eururo.2005.12.042 [DOI] [PubMed] [Google Scholar]
- 7.Puppo P, Bertolotto F, Introini C, et al. Bipolar transurethral resection in saline (TURis): outcome and complication rates after the first 1000 cases. J Endourol. 2009;23:1145–1149. doi: 10.1089/end.2009.0011 [DOI] [PubMed] [Google Scholar]
- 8.Borboroglu PG, Sands JP, Roberts JL, Amling CL. Risk factors for vesicourethral anastomotic stricture after radical prostatectomy,”. Urology. 2000;56(1):96–100. doi: 10.1016/S0090-4295(00)00556-2 [DOI] [PubMed] [Google Scholar]
- 9.Giannarini G, Manassero F, Mogorovich A, et al. Cold- knife incision of anastomotic strictures after radical retropubic prostatectomy with bladder neck preservation: efficacy and impact on urinary continence status. Eur Urol. 2008;54(3):647–656. [DOI] [PubMed] [Google Scholar]
- 10.Wang R, Wood DP, Hollenbeck BK, et al. Risk factors and quality of life for post-prostatectomy vesicourethral anastomotic stenoses. Urology. 2012;79:449. doi: 10.1016/j.urology.2011.07.1383 [DOI] [PubMed] [Google Scholar]
- 11.Filson CP, Montgomery JS, Dailey SM, et al. Complications associated with single-dose, perioperative mitomycin-C for patients undergoing bladder tumor resection. Urol Oncol. 2014;32(1):40e1–8. doi: 10.1016/j.urolonc.2013.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Redshaw JD, Broghammer JA, Smith TG 3rd et al. Intralesional injection of mitomycin C at transurethral incision of bladder neck contracture may offer limited benefit: TURNS study group. J Urol. 2015;193:587–592. doi: 10.1016/j.juro.2014.08.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eltahawy E, Gur U, Virasoro R, Schlossberg SM, Jordan GH. Management of recurrent anastomotic stenosis following radical prostatectomy using holmium laser and steroid injection. BJU Int. 2008;102:796–798. doi: 10.1111/j.1464-410X.2008.07919.x [DOI] [PubMed] [Google Scholar]
- 14.Vanni AJ, Zinman LN, Buckley JC. Radial urethrotomy and intralesional mitomycin C for the management of recurrent bladder neck contractures. J Urol. 2011;186:156–160. doi: 10.1016/j.juro.2011.03.019 [DOI] [PubMed] [Google Scholar]
- 15.Ramirez D, Zhao LC, Bagrodia A, Scott JF, Hudak SJ, Morey AF. Deep lateral transurethral incisions for recurrent bladder neck contracture: promising 5-year experience using a standardized approach. Urology 2013;82(6):1430–1435. [DOI] [PubMed] [Google Scholar]