Abstract
Introduction:
Although behavioral therapies can effectively treat skin picking disorder (SPD), there is no standardized treatment for improving SPD and its comorbidities and there is no group intervention option. This trial aimed to adapt the Rothbaum trichotillomania protocol to SPD (Study 1) and test its efficacy for treating SPD and comorbidities in individual and group formats (Study 2).
Methods:
The adapted protocol was applied to 16 SPD patients, who were allocated to group or individual treatment (Study 1). Afterwards, 54 patients were randomly allocated to treatment in an individual (n=27) or group format (n=27) (Study 2). In both studies, assessments of SPD severity, anxiety, depression, clinical status and skin lesion severity were performed at baseline and the endpoint.
Results:
The adapted protocol was feasible in both treatment modalities (Study 1) and led to high SPD remission rates (individual 63%; group 52%), with no significant difference between intervention types (p = 0.4) (Study 2). SPD, anxiety, and depression symptoms and objective patient lesion measures improved after treatment. There was large effect size for SPD symptom improvement in both treatment types (Cohen’s d: group = 0.88; individual = 1.15) (Study 2).
Conclusion:
The adapted Rothbaum protocol was effective for SPD remission, comorbidities, and skin lesions, both in individual and group formats.
Clinical trial registration:
Keywords: Skin picking disorder, cognitive behavioral therapy, psychotherapy, group psychotherapy
Introduction
Skin picking disorder (SPD), also known as excoriation disorder, affects 1.4 to 5.4% of the general population and 7 to 30% of psychiatric patients.1,2 Its course tends to be chronic, causing negative socioeconomic impact.3 Among individuals with SPD, 23% have comorbid anxiety disorder and 48% have comorbid depression, sometimes with suicidal ideation.1,4
Despite the importance of this pathology, less than a half of patients with SPD seek treatment, only 53% receive a correct diagnosis, and 57% do not improve after treatment. Moreover, the majority of patients (85%) believe that professionals are not trained to treat SPD.1 Regarding treatment options, neither antidepressants nor lamotrigine are more effective than placebo, and only behavioral techniques were superior to placebo in clinical trials.5-7 Four studies have evaluated behavioral techniques in SPD treatment, applying 3 to 4 sessions of therapy based on Azrin and Nunn’s habit reversal method, including: self-monitoring, competing response practice, and searching for better social support through family and friends about how to cope with the problem.8 There was improvement in all of these studies after the intervention,6,8 and one study added a session on cognitive techniques.9 However, they involved different protocols and had small samples, which makes it difficult to generalize the results.6 In addition, their protocols did not address anxious and depressive symptoms associated with SPD.6,10 One study (n=12) evaluated a cognitive psychophysiological model for body-focused repetitive behaviors (including SPD) that treated the habit-triggering emotional construct rather than the habit itself, finding improvement in depressive and anxious symptoms after the intervention.11
One important limitation of behavioral techniques is the low availability of trained therapists.12 Recent studies have found that unified cognitive behavioral therapy (CBT) protocols can effectively treat different pathologies in the same spectrum, facilitating therapist training and improving treatment dissemination.12-14 Moreover, group CBT interventions have also been found effective and can treat more patients at the same time.15 Thus, besides treating more patients, effective group CBT interventions could also train therapists in loco, improving cost effectiveness. To our knowledge, no SPD interventions have been tested in a group format.6,10
The Rothbaum CBT protocol effectively treats trichotillomania with habit reversal techniques and also manages anxiety and depressive symptoms.16,17 Recent studies have found that the rate of co-occurrence of SPD and trichotillomania is higher than expected, and it has been hypothesized that these disorders are part of a single spectrum of pathology.1,18,19
The aim of the present study was to adapt the Rothbaum CBT protocol to SPD treatment (Study 1) and test its efficacy in individual and group formats (Study 2). This study’s hypothesis was that the Rothbaum protocol would effectively treat SPD, improving skin-picking symptoms, as well as comorbid anxious and depressive symptoms, in both individual and group formats.
Study 1
Methods
Study design and participants
This study was conducted as an open pilot trial with 16 patients allocated to treatment with the adapted Rothbaum protocol in individual or group format, according to the patient’s availability. The sample consisted of individuals who sought treatment at a public hospital’s Psychiatry Service between July 2014 and July 2015 after a public advertising campaign. Inclusion criteria were a diagnosis of SPD according to the DSM-52 and motivation to engage in CBT. Exclusion criteria were a psychotic disorder, intellectual disability or suicide risk according to the Mini International Neuropsychiatric Interview.20 The sample’s demographic characteristics are presented in Table 1.
Table 1. Baseline sociodemographic and clinical characteristics of Study 1’s sample, including a comparison of patients who concluded or dropped out of treatment.
| Total sample (n=12) | Patients that concluded the treatment (n=10) | Patients that dropped out (n=2) | Test coefficient; p-value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 43.6 (17.72) | 48.25 (16.61) | 24 (1.41) | 1.87; 0.09* |
| Female gender | 11 (91.7) | 9 (90) | 2 (100) | 1.00† |
| Comorbidities | ||||
| Major depressive disorder | 2 (16.7) | 1 (10) | 1 (50) | 0.31† |
| Dysthymia | 1 (8.3) | 1 (10) | 0 (0) | 1.00† |
| Bipolar affective disorder | 1 (8.3) | 1 (10) | 0 (0) | 1.00† |
| Generalized anxiety disorder | 3 (25) | 1 (10) | 2 (100) | 0.04† ‡ |
| Psychotropic treatment | ||||
| SSRIs | 5 (41.7) | 4 (40) | 1 (50) | 1.00† |
| Tricyclics | 1 (8.3) | 1 (10) | 0 | 1.00† |
| Lamotrigine | 1 (8.3) | 1 (10) | 0 | 1.00† |
| Clinical scales, mean (SD) | ||||
| URICA | 9.57 (1.71) | 10.4 (1.14) | 7.5 (0.7) | 3.24; 0.02* ‡ |
| SPIS | 20.86 (13.39) | 18.56 (10.79) | 28 (5.65) | -1.16; 0.27* |
| CGI | 4.57 (1.27) | 4.5 (1.22) | 5 (1.41) | -0.48; 0.64* |
| BDI | 21.14 (9.72) | 20.17 (11) | 20.5 (2.12) | -0.04; 0.96* |
| HAM-A | 26.14 (9.1) | 23.71 (11.91) | 24 (1.41) | −0.03; 0.97* |
Data presented as n (%), unless otherwise specified.
BDI = Beck Depression Inventory; CGI = Clinical Global Impression; HAM-A = Hamilton Anxiety Scale; SPIS = Skin Picking Impact Scale; SSRI = Selective Serotonin Reuptake Inhibitor; URICA = University of Rhode Island Change Assessment.
Student’s t-test;
Fisher’s exact test.
Statistically significant.
Procedure and measures
Under the supervision of a senior researcher, a diagnostic interview was conducted by a psychiatry resident that consisted of the MINI20 (Brazilian Portuguese version)21 and a checklist of SPD symptoms according to DSM-5.2 Patients who met the inclusion criteria completed a baseline evaluation conducted by two trained evaluators that consisted of the Beck Depression Inventory (BDI),22 the Hamilton Anxiety Scale (HAM-A),23 the Clinical Global Impression (CGI) scale,24 the Skin Picking Impact Scale (SPIS),25 and the University of Rhode Island Change Assessment (URICA) instrument.26
The BDI is a self-report questionnaire that evaluates depressive symptoms; in the validated Brazilian Portuguese version, scores range from 0 to 63, with higher scores indicating more severe symptoms.22,27 The HAM-A is a questionnaire for evaluating anxiety symptoms; in the validated Brazilian Portuguese version, scores range from 0 to 56, with higher scores indicating more severe symptoms.23,28 The CGI scale is a questionnaire for assessing the impact that a disease/disorder has on a patient’s life; in the Brazilian Portuguese version, scores range from 1 (asymptomatic) to 7 (very severe impact).24,29 The SPIS is a self-applied questionnaire30 for assessing the severity and life impact of skin picking; the validated Brazilian Portuguese version consists of 10 items on skin-picking habits and their influence on the patient’s daily life during the last week. Each item is rated from 0 to 5 on a Likert scale, and total scores range between 0 and 50, with higher scores indicating more severe impact.25 The URICA is a self-applied scale that assesses the respondent’s current motivation to change a specific condition. In the validated Brazilian Portuguese version, its 32 randomly ordered questions cover pre-contemplative, contemplative, action or maintenance stages, with higher scores indicating more advanced motivational status.26,31 The 9-week Rothbaum CBT protocol17 was adapted into an 8-week format for SPD patients. Sessions 3 and 4 were condensed into a single session due to the content’s similarity and to enhance treatment compliance through a shorter protocol. The adapted Rothbaum protocol maintained the same techniques while changing the target habit from trichotillomania to skin picking. The adapted protocol was applied in weekly sessions of 45 and 90 minutes in individual and group formats, respectively. After the intervention, the baseline questionnaires were reapplied. Under the supervision of a senior CBT therapist, both treatment modalities were conducted by four professionals with theoretical and practical training in CBT (Table 2).
Table 2. Rothbaum protocol sessions framework and adaptations for use with skin picking disorder.
| Summary content of Rothbaum protocol | Adaptations | Rothbaum protocol adapted to Skin Picking | |
|---|---|---|---|
| 1. Information gathering | - Psychoeducation about trichotillomania. - Describing the hair pulling habit. - Identifying trigger situations.- Self-monitoring of hair pulling. - Homework: self-monitoring and collecting pulled hairs. |
- Substituting skin picking for trichotillomania as the targeted habit; no technique changes. | - Psychoeducation about Skin Picking Disorder. - Describing the skin touching habit. - Identifying of trigger situations. - Self-monitoring the skin touching habit. - Homework: self-monitoring and collecting scabs. |
| 2. Habit change strategies | - Azrin and Nunn’s habit reversal techniques. - Channels for manifesting anxiety. - Trichotillomania self-monitoring inspection. - Competing response practice. - Listing the drawbacks of trichotillomania. - Homework: self-monitoring using habit-reversal techniques. Collecting pulled hair to show the therapist in the next session. |
- Substituting skin picking for trichotillomania as the targeted habit, e.g. applying some product to the skin rather than the hair; simulating the impulse by keeping the hands above the wound rather than the hair. - Wearing rings to avoid skin picking. - Substituting collected scabs for collected hair. |
- Azrin and Nunn’s habit reversal techniques targeting skin picking. - Wearing rings to avoid skin picking. - Channels for manifesting anxiety. - Skin picking self-monitoring inspection. - Competing response practice. - Listing the drawbacks of skin picking. - Homework: self-monitoring using habit reversal techniques and checking their efficacy. Collecting scabs to show the therapist in the next session. |
| 3. Coping skills | - Diaphragmatic breathing (session 3). - Progressive muscle relaxation (session 4). - Homework: self-monitoring, reading the list of drawbacks, and coping skills practice. |
- Merging sessions 3 and 4 of the Rothbaum protocol. | - Diaphragmatic breathing. - Progressive muscle relaxation. - Homework: self-monitoring, reading the list of drawbacks and coping skills practice. |
| 4. Thought stopping | - Explaining the A-B-C cognitive model. - Thought stopping and distraction technique. - Homework: self-monitoring and thought stopping practice. |
- No changes. | - Explaining the A-B-C cognitive model. - Thought stopping and distraction technique. - Homework: self-monitoring and thought stopping practice. |
| 5. Cognitive restructuring | - Technique for analyzing evidence within the A-B-C cognitive model. - Homework: self-monitoring and cognitive restructuring practice. |
- Adding the decatastrophization technique, using a Likert scale of severity and the reassignment technique (pie chart).* | - Technique for analyzing evidence within the A-B-C cognitive model. - Decatastrophization technique, using a Likert scale of severity.* - Reassignment technique (pie chart).Homework: self-monitoring and practice with these 3 cognitive restructuring techniques. |
| 6. Targeted internal dialogue | - Internal dialogue guidance in preparation for a stressor, based on the work of Veronen and Kilpatrick. - Positive reinforcement practice. - Homework: self-monitoring and targeted internal dialogue practice. |
- No changes. | - Internal dialogue guidance in preparation for a stressor, based on the work of Veronen and Kilpatrick. - Positive reinforcement practice. - Homework: self-monitoring and targeted internal dialogue practice. |
| 7. Role-changing and role-playing | - Exchanging therapist/patient roles and CBT role-playing for trichotillomania. - Reviewing the studied techniques and points for improvement. - Homework: self-monitoring. |
- Changing the targeted habit from trichotillomania to skin picking. | - Exchanging therapist/patient roles and CBT role-playing for skin picking. - Reviewing the studied techniques and points for improvement. - Homework: self-monitoring and reviewing the studied techniques and points for improvement. |
| 8. Relapse prevention | - Assembling the Trichotillomania Relapse Prevention Guide. | - Changing the targeted habit from trichotillomania to skin picking. | - Assembling the Skin Picking Relapse Prevention Guide. |
Adapted from Wright et al.32
The study’s primary endpoint was the adaptability of the Rothbaum protocol, assessed through dropout rates. Secondary outcomes included improvement in CGI, SPIS, BDI and HAM-A results.
Statistical analysis
Statistical analyses were performed in SPSS version 20.0. Subjects who attended less than 50% of the treatment sessions were included in the statistical analysis through the last observation carried forward model. Variable distribution was analyzed with the Shapiro-Wilk test and a parametric or non-parametric test, according to distribution. The chi-square test was used to compare categorical variables. The significance level was set at p < 0.05.
Ethics statement
All participants gave written informed consent to participate in the research. This study was conducted in accordance with Brazilian National Health Council guidelines and norms regulating research involving human beings and followed the ethical principles of the Declaration of Helsinki. It was approved by the local ethics and research commission (protocol 1,197,672).
Results
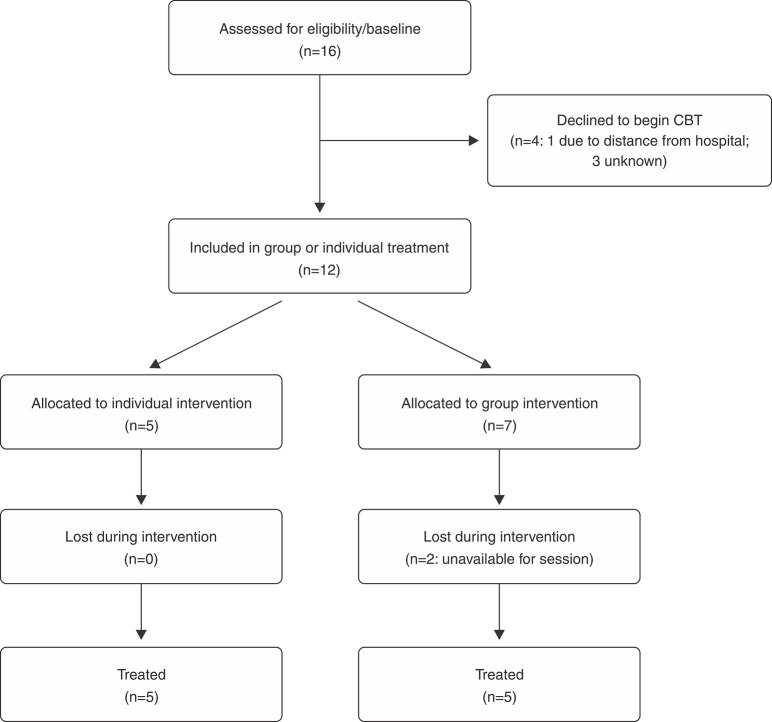
The study flow chart is depicted in Figure 1. There was no significant difference in dropout rates between individual and group treatment (0 vs. 28.5%, p = 0.47); both rates are in accordance with the literature.33 Patients who completed the treatment were more motivated according to URICA scores and had less incidence of generalized anxiety disorder (Table 1). The protocol was feasible in both the group and individual modalities, leading to clinical improvement, although no significant change was found in the assessment scales.
Figure 1. Flow diagram of Study 1. CBT = cognitive behavioral therapy.
Study 2
Methods
Study design and participants
This evaluator-blinded clinical trial included 54 patients, who were randomly allocated to treatment with the adapted Rothbaum CBT protocol in an individual (n=27) or group (n=27) format. The sample consisted of individuals who sought treatment at the Psychiatry Service of the Universidade Federal de Ciências da Saúde de Porto Alegre between July 2016 and January 2018 after a public advertising campaign. The inclusion and exclusion criteria were the same as in Study 1. Individuals who were not included in this study were referred to the appropriate community resources. The sample’s demographic characteristics of are presented in Table 3.
Table 3. Sociodemographic and clinical characteristics of the Study 2 sample at baseline, including comparison between patients randomized to group and individual treatment.
| Total sample (n=54) | Individual modality (n=27) | Group modality (n=27) | Test coefficient; p-value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 36.26 (13.55) | 32.67 (14.12) | 40.32 (12.07) | -2.00; 0.51* |
| Female | 48 (88.9) | 24 (88.9) | 24 (88.9) | 1.00† |
| Caucasian | 48 (88.9) | 23 (85.2) | 25 (92.6) | 6.03; 0.10‡ |
| Status | 6.71; 0.15‡ | |||
| Married | 14 (31.5) | 5 (18.5) | 12 (44.4) | |
| Single | 30 (55.6) | 19 (70.4) | 11 (40.7) | |
| Religion | 4.98; 0.41‡ | |||
| Catholic | 21 (38.9) | 9 (33.3) | 12 (44.4) | |
| Agnostic | 13 (24.1) | 9 (33.3) | 4 (14.8) | |
| Occupation | 0.11§ | |||
| Working | 22 (40.7) | 8 (29.6) | 14 (51.9) | |
| Student | 14 (31.5) | 11 (40.7) | 6 (22.2) | |
| Education (years), mean (SD) | 14.23 (3.48) | 14.0 (3.31) | 14.5 (3.73) | 0.62* |
| Income (US$), median (minimum-maximum) | 600 (0-8,500) | 598.8 (0-8,383.23) | 898.2 (0-2,994.01) | 0.15|| |
| Trigger situation | 21 (38.9) | 10 (37) | 11 (40.7) | 0.00; 1.00† |
| Age of SPD onset, median (minimum-maximum) | 15 (4-64) | 18.5 (8-64) | 14 (4-51) | 0.07|| |
| Previous treatment | 4.39; 0.49‡ | |||
| None | 37 (68.5) | 14 (63) | 20 (74.1) | |
| Medication | 11 (20.4) | 7 (25.9) | 4 (14.8) | |
| Family history of SPD | 16 (29.6) | 6 (22.2) | 10 (37) | 0.79; 0.37† |
| Family history of psychiatric disease | 21 (39.6) | 7 (25.9) | 14 (55.6) | 6.56; 0.16† |
| Clinical scales | ||||
| Current depressive episode | 16 (29.6) | 9 (33.3) | 7 (25.9) | 0.15; 0.69† |
| Past depressive episode | 13 (24.1) | 4 (14.8) | 9 (33.3) | 1.43; 0.23† |
| Dysthymia | 3 (5.6) | 1 (3.7) | 2 (7.4) | 1.00§ |
| Bipolar disorder | 4 (7.4) | 2 (7.4) | 2 (7.4) | 1.00§ |
| Panic disorder | 17 (31.5) | 8(29.6) | 9 (33.3) | 0.00; 1.00† |
| Agoraphobia | 9 (16.7) | 4 (14.8) | 5 (18.5) | 1.00§ |
| Social anxiety | 5 (9.3) | 5 (18.5) | 0 (0) | 0.02§¶ |
| Obsessive Compulsive Disorder | 2 (3.7) | 2 (7.4) | 0 (0) | 0.23§ |
| Post-traumatic stress disorder | 3 (5.6) | 1 (3.7) | 2 (7.4) | 1.00§ |
| Nervous bulimia | 2 (3.7) | 2 (7.4) | 0 (0) | 0.23§ |
| Generalized anxiety disorder | 21 (39.6) | 9 (33.3) | 14 (44.4) | 0.20; 0.65† |
| URICA, median (minimum-maximum) | 10.8 (6.4-14) | 11.6 (6.4-12.8) | 9.7 (6.8-14) | 0.07|| |
| SPIS, median (minimum-maximum) | 28.5 (3-48) | 33.0 (7-44) | 23.0 (3-48) | 0.14|| |
| CGI, median (minimum-maximum) | 5 (2-7) | 5 (3-7) | 5 (2-7) | 0.27|| |
| BDI, mean (SD) | 17.3 (11.28) | 19.08 (13.12) | 15.59 (9.1) | 0.98; 0.33* |
| HAM-A, mean (SD) | 29.1 (14.09) | 24.38 (15.13) | 30.63 (13.13) | -0.8; 0.43* |
Data presented as n (%), unless otherwise specified.
BDI = Beck Depression Inventory; CGI = Clinical Global Impression; HAM-A = Hamilton Anxiety Scale; SPIS = Skin Picking Impact Scale; URICA = University of Rhode Island Change Assessment scale.
Student’s t-test;
Yates Chi-square (continuity correction);
Pearson chi-square;
Fisher exact test;
Mann-Whitney test.
Statistically significant.
Procedure and measures
The baseline evaluation was performed by two blinded evaluators (with high reliability: kappa = 0.9), following the same procedures and applying the same instruments as in Study 1 (URICA, SPIS, BDI, CGI and HAM-A). For Study 2, we also included a photographic instrument developed by two dermatologists to directly evaluate SPD lesions.30 All photos were analyzed by two blinded dermatologists with the photographic instrument, which has high internal consistency and moderate reliability. This measure is important since it specifically assesses lesion severity apart from the influence of patient habit awareness or associated depressive/anxious symptoms.30
The patients were randomized in blocks of 6 to receive individual or group treatment. The 8-week Rothbaum CBT protocol adapted for SPD, as described in Study 1, was applied in weekly sessions of 45 minutes for individual treatment and 90 minutes for group treatment, with the same therapists applying both formats.
The study’s primary endpoint was post-intervention symptom remission, characterized by CGI scores ≤ 2.29 The secondary outcome was change in CGI, SPIS, BDI, HAM-A and photographic instrument results.
Statistical analysis
Statistical analyses were performed in SPSS version 23.0. The sample size was based on a previous study by Schuck et al., which found CBT to be efficacious for SPD in a sample of 34 patients.9 Participants who attended less than 50% of the treatment sessions were included in the statistical analysis through the last observation carried forward method. The data were analyzed for normality using the Kolmogorov-Smirnov test, and categorical variables were compared with the Pearson chi-square test, the Yates chi-square test, or Fisher’s exact test. Generalized estimating equations with Bonferroni correction were used to assess improvement in clinical scales after treatment and to compare improvement between treatment modalities. The intervention effect size was calculated with Cohen’s d, using natural logarithm transformation for pre- and post-treatment CGI values.
Ethics statement
The ethical considerations were the same as in Study 1 (approval protocol 1,197,672). This trial was registered in the Clinical Trials database (NCT03182478).
Results
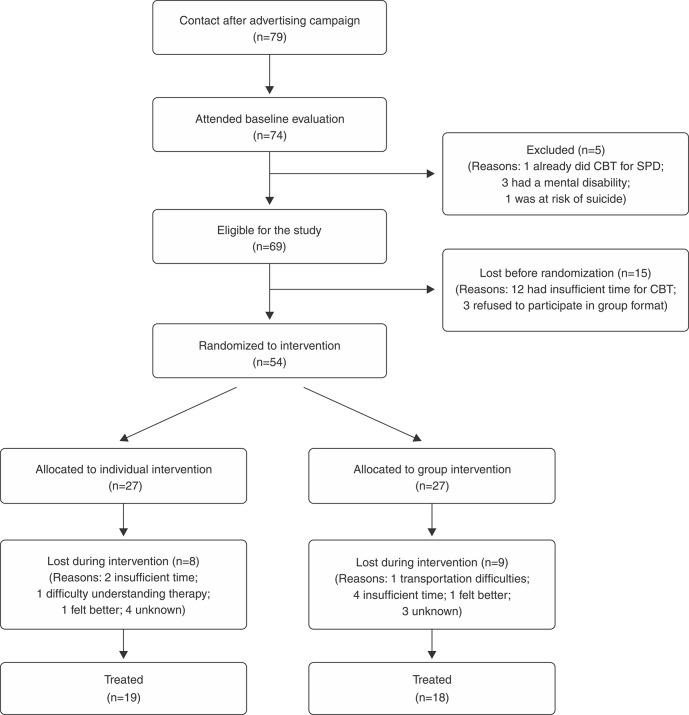
Figure 2 depicts the CONSORT study flow diagram.34 After treatment, 8 patients in individual treatment (29.6%) and 9 in group treatment (33.3%) dropped out before completing at least 50% of the sessions. There was no significant difference in dropout rate between treatment modalities (p = 0.99). There were no differences in patient clinical and sociodemographic characteristics between treatment modalities, except that patients in individual treatment had a higher rate of comorbid social anxiety (Table 3).
Figure 2. Flow diagram for Study 2. CBT= cognitive behavioral therapy; SPD = skin picking disorder.
After treatment with the adapted Rothbaum CBT protocol, both intervention modalities showed high remission rates (individual 63%; group 52%), with no significant difference between intervention types (p = 0.4). The treatment effect size, according to change in global clinical status, was large in both intervention types (Cohen’s d: Group format = 0.88; individual format = 1.15). Global status, skin picking symptoms, comorbid depressive symptoms and skin lesion severity significantly improved after treatment, with no significant differences between intervention types. Anxiety symptoms also improved significantly after treatment in both modalities, although there was more improvement among patients in individual treatment (p = 0.01) (Table 4).
Table 4. Clinical scales before and after CBT according to treatment modality, including modality x time interaction.
| Global mean (SD) [95% confidence interval] | ||||||
|---|---|---|---|---|---|---|
| Scale/treatment modality | Before CBT | After CBT | p-value | Before CBT | After CBT | p-value between modalities |
| CGI | ||||||
| Individual | 4.92 (0.24) | 2.88 (0.39) | < 0.001 | 4.7 (0.17) [4.36-5.04] | 2.89 (0.24) [2.41-3.37] | 0.33 |
| Group | 4.48 (0.24) | 2.92 (0.29) | < 0.001 | |||
| SPIS | ||||||
| Individual | 28.4 (2.12) | 16.59 (2.42) | < 0.001 | 26.11 (1.55) [23.05-29.16] | 16.08 (1.79) [12.57-16.59] | 0.22 |
| Group | 23.81 (2.27) | 16.59 (2.63) | < 0.001 | |||
| BDI | ||||||
| Individual | 18.34 (2.41) | 11.76 (2.31) | < 0.001 | 16.87 (1.47) [10.69-19.41] | 12.31(1.49) [9.38-15.23] | 0.59 |
| Group | 15.4 (1.69) | 12.85 (1.81) | < 0.001 | |||
| HAM-A | ||||||
| Individual | 27.6 (2.91) | 17.88 (2.82) | < 0.001* | 27.6 (2.91) [21.89-33.31] | 17.88 (2.82) [12.35-23.40] | 0.01† |
| Group | 30.7 (2.47) | 27.33 (2.29) | 0.014 | 30.70 (2.47) [25.85-35.54] | 27.38(2.29) [22.88-31.87] | |
| PI | ||||||
| Individual | 1.71 (0.28) | 0.74 (0.18) | < 0.001 | 1.55 (0.16) [1.23-1.86] | 0.63 (0.11) [0.41-0.86] | 0.76 |
| Group | 1.38 (0.16) | 0.52 (0.13) | < 0.001 | |||
BDI = Beck Depression Inventory; CBT = cognitive behavioral therapy; CGI = Clinical Global Impression; HAM-A = Hamilton Anxiety Scale; PI = Photographic Instrument; SD = standard deviation; SPIS = Skin Picking Impact Scale.
Data expressed as mean (standard deviation).
Bonferroni correction.
Statistically significant.
Comparing patients who dropped out before completing at least 50% of the treatment with those who completed treatment, dropouts had a higher prevalence of agoraphobia (37.5% vs. 8.1%, p = 0.009) and were less motivated for treatment according to URICA scores (median 9.8 [6.86-13.71] vs. median 11 [6.4-14] p = 0.02).
Discussion
This study found that adapting the Rothbaum CBT protocol to SPD was feasible and efficacious. We were able to adapt the protocol while maintaining the same structure and techniques – only the target habit changed, which facilitated therapist training. Some new techniques were included specifically for skin picking, such as scab collection and wearing rings, which were well accepted and easily implemented by patients. Dropout rates during treatment were not higher than expected, reflecting the acceptability of the intervention.33
CBT-based interventions are not always equally effective in group and individual formats.35 Although the group modality has better cost-effectiveness, since it can treat more patients with fewer therapists, patients can sometimes feel inhibited in a group setting, they may not have the patience to wait for a group to be formed, or they may not comply over a several week program due to reduced scheduling flexibility.35 This study found no difference between dropout rates in the two treatment formats, suggesting that the group model can be as efficacious as the individual one. Although the group modality included no patients with social anxiety (and, thus, had no related dropouts), it is possible that some patients refused to participate due to social anxiety. However, since the baseline comorbidity evaluation was performed after inclusion in the study, we cannot confirm this. An important challenge in SPD treatment is the lack of trained therapists and the great demand.12 The group format is a viable way to fill this demand and, to our knowledge, this is the first study to evaluate such a format for SPD treatment.
Consistent with previous studies, we found a higher incidence of generalized anxiety disorder and depressive episodes, either past or current, than expected rates for the general population.1 Although some patients did not fulfill the criteria for anxiety or depressive disorders, many scored high on the BDI and HAM-A scales. These findings show the importance of treating SPD with interventions that include anxiety and depression components, such as the Rothbaum CBT protocol.
Grant et al. found that SPD is frequently associated with anxiety (8-23% of the cases), depression (12.5-48%), substance use (in 14-36% of patients) and major functional impairment.4,36 Despite these important findings, there is no current treatment for SPD that includes management of these symptoms. One study with 6 participants evaluated the use of acceptance-enhanced behavior therapy for trichotillomania and chronic SPD, but reported no benefits in managing depression.37 Another study applied a brief CBT protocol consisting of 4 sessions of psychoeducation, cognition assessment, habit reversal techniques and relapse prevention, but reported no benefits for anxiety or depression (i.e. treatment was no more effective than the waiting list condition).9 In this study, both treatment modalities of the adapted Rothbaum CBT protocol resulted in improvement in all assessed symptoms, not only for skin picking but for depression and anxiety as well, which was probably due to the protocol’s cognitive and anxiety coping techniques. Although the group and individual interventions resulted in significant reductions in anxiety, the individual format showed greater improvement, although probably at the cost of improving social anxiety. The effect size for the adapted Rothbaum protocol was considered large in both modalities, larger than CBT interventions for other anxiety disorders.33 Based on these results, as well as the fact that this protocol is short and easy to apply, it can be considered to have good cost-effectiveness.
The photographic instrument results also improved after treatment with the adapted Rothbaum protocol. These results reflect the severity of SPD skin lesions and are a reliable way of determining skin picking habit reduction. Since previous studies have found that change in photographic instrument results is not correlated with change in depression or anxiety symptoms,30 it can be hypothesized that the treatment applied in this study directly reduced the skin picking habit, independently of other variables.
It is well known that compliance with CBT is directly associated with better outcomes. In this study we found that the URICA scale was an appropriate way to assess the patients’ readiness to change, thus reflecting motivation for therapy. When a treatment is offered, it is important to consider its cost-effectiveness for patients. Our study shows preliminary data regarding motivation and dropout rates in SPD treatment. If this data is confirmed in other clinical trials, we could hypothesize that patients unmotivated for CBT according to the URICA instrument should not be included in this treatment modality, since the chance of dropout or non-response is high. This is of special concern in group interventions, which can be more cost-effective in public health settings, but cannot replace patients who drop out during therapy.
Our results should be interpreted in light of some limitations. After randomization, the intervention group included no patients with social anxiety, a pathology that is a barrier to group treatment,35 so it is prudent not to generalize our group intervention findings to patients with comorbid social anxiety. Since our study had no follow-up evaluation, generalizations about the long-term efficacy of our results cannot be made. Although the risk of relapse is an important issue in CBT, only one CBT study on SPD has included follow-up (which was only 3 months).9 Another study limitation was the lack of a placebo or waitlist control condition. Since the protocol was found efficacious, future studies with control conditions are expected. The main strength of this trial was its two-study format, including adequate design and conservative statistical analysis. This is the first study to have used an SPD treatment that manages important comorbid symptoms in both individual and group formats.
In conclusion, despite being a prevalent disorder, there is currently no treatment for SPD that addresses the management of comorbid symptoms, and no group treatment options exist to overcome low therapist availability. This study found that the Rothbaum CBT protocol for trichotillomania can be adapted to SPD and it effectively led to symptom remission, including improvement in clinical status and in skin picking, anxiety, and depression symptoms, as well as skin lesion severity, both in individual and group formats. These findings are innovative and can fill the current gap in SPD treatment. Follow-up studies evaluating the risk of relapse are expected.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
The authors would like to thank Dr. Barbara O. Rothbaum, who graciously allowed us to adapt her protocol in our study.
Footnotes
How to cite this article: Xavier ACM, de Souza CMB, Flores LHF, Bermudez MB, Silva RMF, de Oliveira AC, et al. Skin picking treatment with the Rothbaum cognitive behavioral therapy protocol: a randomized clinical trial. Braz J Psychiatry. 2020;42:510-518. http://dx.doi.org/10.1590/1516-4446-2019-0636
References
- 1.Tucker BT, Woods DW, Flessner CA, Franklin SA, Franklin ME. The skin picking impact project: phenomenology, interference, and treatment utilization of pathological skin picking in a population-based sample. J Anxiety Disord. 2011;25:88–95. doi: 10.1016/j.janxdis.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.Machado MO, Köhler CA, Stubbs B, Nunes-Neto PR, Koyanagi A, Quevedo J, et al. Skin picking disorder: prevalence, correlates, and associations with quality of life in a large sample. CNS Spectr. 2018;23:311–20. doi: 10.1017/S1092852918000871. [DOI] [PubMed] [Google Scholar]
- 4.Grant JE, Odlaug bL, Chamberlain SR, Keuthen NJ, Lochner C, Stein DJ. Skin picking disorder. Am J Psychiatry. 2012;169:1143–9. doi: 10.1176/appi.ajp.2012.12040508. [DOI] [PubMed] [Google Scholar]
- 5.Schumer MC, Bartley CA, Bloch MH. Systematic review of pharmacological and behavioral treatments for skin picking disorder. J Clin Psychopharmacol. 2016;36:147–52. doi: 10.1097/JCP.0000000000000462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selles RR, McGuire JF, Small BJ, Storch EA. A systematic review and meta-analysis of psychiatric treatments for excoriation (skin-picking) disorder. Gen Hosp Psychiatry. 2016;41:29–37. doi: 10.1016/j.genhosppsych.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Gelinas BL, Gagnon MM. Pharmacological and psychological treatments of pathological skin-picking: a preliminary meta-analysis. J Obsessive Compuls Relat Disord. 2013;2:167–75. [Google Scholar]
- 8.Azrin NH, Nunn RG. Habit-reversal: a method of eliminating nervous habits and tics. Behav Res Ther. 1973;11:619–28. doi: 10.1016/0005-7967(73)90119-8. [DOI] [PubMed] [Google Scholar]
- 9.Schuck K, Keijsers GP, Rinck M. The effects of brief cognitive-behaviour therapy for pathological skin picking: a randomized comparison to wait-list control. Behav Res Ther. 2011;49:11–7. doi: 10.1016/j.brat.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Teng EJ, Woods DW, Twohig MP. Habit reversal as a treatment for chronic skin picking: a pilot investigation. Behav Modif. 2006;30:411–22. doi: 10.1177/0145445504265707. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor K, Lavoie M, Desaulniers B, Audet JS. Cognitive psychophysiological treatment of bodily-focused repetitive behaviors in adults: an open trial. J Clin Psychol. 2017;74:273–85. doi: 10.1002/jclp.22501. [DOI] [PubMed] [Google Scholar]
- 12.Keuthen NJ, Tung ES, Reese HE, Raikes J, Lee L, Mansueto CS. Getting the word out: cognitive-behavioral therapy for trichotillomania (hair-pulling disorder) and excoriation (skin-picking) disorder. Ann Clin Psychiatry. 2015;27:10–5. [PubMed] [Google Scholar]
- 13.Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, et al. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav Ther. 2012;43:666–78. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gallagher MW, Sauer-Zavala SE, Boswell JF, Carl JR, Bullis J, Farchione TJ, et al. The impact of the unified protocol for emotional disorders on quality of life. Int J Cogn Ther. 2013;6(1) doi: 10.1521/ijct.2013.6.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Quality Ontario. Psychotherapy for major depressive disorder and generalized anxiety disorder: a health technology assessment. Ont Health Technol Assess Ser. 2017;17:1–167. [PMC free article] [PubMed] [Google Scholar]
- 16.Flessner CA. Cognitive behavior therapy for childhood repetitive behavior disorders: tic disorders and trichotillomania. Child Adolesc Psychiatr Clin N Am. 2011;20:319–28. doi: 10.1016/j.chc.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothbaum BO. The behavioral treatment of trichotillomania. Behav Cogn Psychother. 1992;20:85–90. [Google Scholar]
- 18.Van Ameringen M, Patterson B, Simpson W. DSM-5 obsessive-compulsive and related disorders: clinical implications of new criterea. Depress Anxiety. 2014;31:487–93. doi: 10.1002/da.22259. [DOI] [PubMed] [Google Scholar]
- 19.Snorrason I, Belleau EL, Woods DW. How related are hair pulling disorder (trichotillomania) and skin picking disorder? A review of evidence for comorbidity, similarities and shared etiology. Clin Psychol Rev. 2012;32:618–29. doi: 10.1016/j.cpr.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- 21.Amorim P. Mini International Neuropsychiatric Interview (MINI): validação de entrevista breve para diagnóstico de transtornos mentais. Braz J Psychiatry. 2000;22:106–15. [Google Scholar]
- 22.Gorenstein C, Andrade L. Validation of a Portugues version of the beck depression inventory and the state-trait anxiety inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–7. [PubMed] [Google Scholar]
- 23.Kummer A, Cardoso F, Teixeira AL. Generalized anxiety disorder and the Hamilton anxiety rating scale in parkinson's disease. Arq Neuropsiquiatr. 2010;68:495–501. doi: 10.1590/s0004-282x2010000400005. [DOI] [PubMed] [Google Scholar]
- 24.de Lima MS, Soares BG, Paoliello G, Vieira RM, Martins CM, da Mota JI, Neto, et al. The Portuguese version of the clinical global impression - schizophrenia scale: validation study. Braz J Psychiatry. 2007;29:246–9. doi: 10.1590/s1516-44462007000300010. [DOI] [PubMed] [Google Scholar]
- 25.Keuthen NJ, Deckersbach T, Wilhelm S, Engelhard I, Forker A, O´Sullivan RL, et al. The Skin Picking Impact Scale (SPIS): scale development and psychometric analyses. Psychosomatics. 2001;42:397–403. doi: 10.1176/appi.psy.42.5.397. [DOI] [PubMed] [Google Scholar]
- 26.Hasler G, Klaghofer R, Buddeberg C. [The University of Rhode Island Change Assessment Scale (URICA)] Psychother Psychosom Med Psychol. 2003;53:406–11. doi: 10.1055/s-2003-42172. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 29.Busner J, Targum SD. The clinical global impression scale – applying a research tool in clinical practice. Psychiatry (Edgmont) 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 30.Xavier AC, de Souza CM, Flores LH, Prati C, Cassal C, Dreher CB. Improving skin picking diagnosis: validation of the skin picking impact scale and development of a photographic instrument. An Bras Dermatol. 2019;94:553–60. doi: 10.1016/j.abd.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szupszynski KP, Oliveira MS. Brasilian version of the University of Rhode Island Change Assessment (URICA) for illicit substance users. Psico-USF. 2008;13:31–9. [Google Scholar]
- 32.Wright JH, Basco MR, Thase ME. Aprendendo a terapia cognitivo-comportamental. Porto Alegre: Artmed; 2008. [Google Scholar]
- 33.Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JA, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35:502–14. doi: 10.1002/da.22728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–32. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 35.Stangier U, Heidenreich T, Peitz M, Lauterbach W, Clark DM. Cognitive therapy for social phobia: individual versus group treatment. Behav Res Ther. 2003;41:991–1007. doi: 10.1016/s0005-7967(02)00176-6. [DOI] [PubMed] [Google Scholar]
- 36.Grant JE, Chamberlain SR. Clinical correlates of symptom severity in skin picking disorder. Compr Psychiatry. 2017;78:25–30. doi: 10.1016/j.comppsych.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keuthen NJ, Rothbaum BO, Falkenstein MJ, Meunier S, Timpano KR, Jenike MA, et al. DBT-enhanced habit reversal treatment for trichotillimania: 3- and 6-month follow-up results. Depress Anxiety. 2011;28:310–3. doi: 10.1002/da.20778. [DOI] [PubMed] [Google Scholar]