Graphical abstract
Keywords: Alcohol use disorder, Neighborhood environment, Social control, Racial/ethnic differences, Family history, Gender differences
Highlights
-
•
Family history effects on drinking were stronger with more alcohol availability.
-
•
For some subgroups, this moderation effect appeared for alcohol dependence as well.
-
•
For Whites, family history effects were weaker with more religious social control.
Abstract
Background
Effects of a family history of alcoholism may be moderated by area-level social control factors. We examine whether increased neighborhood alcohol availability (low social control environment) or increased presence of religious adherents in the county (high social control environment) interact with family history in relation to alcohol outcomes.
Methods
Weighted data from 12,686 adult drinkers (51% male; mean age 44; 80% White, 9% Black, 11% Hispanic) in three US National Alcohol Surveys were linked with data on area-level off-premise alcohol availability and adherence to religions with strong prohibitions against drinking. Family history density had four levels (family history negative, extended family only, first-degree relative(s) only, high family density). Dichotomous outcomes were past-year high-risk drinking and alcohol dependence. Logistic regression models with interaction terms assessed whether associations of family history with alcohol outcomes differed significantly by area-level social control. Stratified models assessed differences by sex and by race/ethnicity.
Results
In the full sample, effects of first-degree relatives and high family density on high-risk drinking strengthened as alcohol availability increased. This was replicated in the subsample of women and suggested in relation to dependence among men and Black drinkers. For White drinkers, higher religious social control reduced effects of first-degree relatives on high-risk drinking.
Conclusions
Low social control—in particular, greater density of off-premise alcohol outlets—appears to exacerbate effects of a family history of alcoholism on high-risk drinking. Policy makers should consider differential benefits of decreasing alcohol availability for people from high-risk families to reduce high-risk drinking and alcohol problems.
1. Introduction
1.1. Family history
Having biological relatives with alcohol problems increases an individual’s risk for alcohol problems (Dawson et al., 1992, Chartier et al., 2010). The intergenerational transmission of alcohol use is attributed to multiple mechanisms, including genetic vulnerability (Verhulst, Neale, & Kendler, 2015) and learned attitudes about alcohol and drinking behaviors (Bailey et al., 2011, Peterson et al., 1994). Many people report a family history (FH) of alcohol problems: A recent national survey documented 21.0% of adults had a biological parent with a history of alcohol problems, and 37.6% had another biological relative with a history of alcohol problems (Karriker-Jaffe, Greenfield, & Kaplan, 2017). Adults with familial alcohol problems are more likely to transition from at-risk drinking to alcohol use disorder (AUD) (Beseler et al., 2008, Milne et al., 2009). Secondhand effects of family members’ alcohol problems also are significant, particularly for women (Nayak, Patterson, Wilsnack, Karriker-Jaffe, & Greenfield, 2019) and children (Kaplan, Nayak, Greenfield, & Karriker-Jaffe, 2017).
FH captures potentially heritable genetic and early family environment effects (Light et al., 1996, Zucker et al., 1994) and is commonly measured by retrospective indicators of alcohol problems in parents or in first-degree relatives (Elliott, Carey, & Bonafide, 2012). Some studies use a degree measure of FH density in both first- and second-degree relatives (Dawson et al., 1992, Harford et al., 1992), while other studies consider both the proportion of affected relatives and level of relatedness (Turner et al., 1993, Stoltenberg et al., 1998, Milne et al., 2008), or presence of affected relatives across multiple generations (Dawson et al., 1992, Hill et al., 1994, Kendler et al., 2018). Studies using these composite FH measures consistently find individuals from more densely-affected families are at greater risk for hazardous alcohol use and AUD. In a US population sample, Dawson et al. (Dawson, Harford, & Grant, 1992) showed odds of AUD among drinkers were highest in individuals from high-density families with alcohol problems in both first- and second- or third-degree relatives (OR = 2.79). Odds of dependence also were higher in those with alcohol problems only in first-degree relatives (OR = 1.91) compared to negative FH (Dawson et al., 1992).
Studies on sex differences in the effect of FH in adult samples are relatively limited. There is prior evidence that the effects of FH are stronger in males than females, particularly when the effects of childhood exposure to family drinking are controlled (Light, Irvine, & Kjerulf, 1996). We know less about the influence of FH on adult drinking behaviors in non-White populations, as demonstrated by a 2012 meta-analysis in college students which found only four of 53 study samples were fully non-White, as were fewer than one in four participants across studies (Elliott et al., 2012). There also is a gap in current scientific knowledge about FH effects later in life, as most analyses of age-related genetic effects to date focus on adolescence and young adulthood (Kendler et al., 2015, Thomas et al., 2018, Khoddam et al., 2015, Irons et al., 2012), with few examples of studies that include adults at midlife or older ages (Russell, Cooper, & Frone, 1990).
1.2. Social control
In addition to liabilities transmitted within families, social environments contribute to alcohol use and AUD. Differential environmental exposures lead to sex and racial/ethnic differences in alcohol outcomes (Karriker-Jaffe et al., 2012, Zapolski et al., 2014, Zemore et al., 2011). Prior models of joint genetic and environmental factors (Dick and Kendler, 2012, Shanahan and Hofer, 2005) further suggest genetic effects on alcohol use are more pronounced in adverse environments (with low social control) and become muted in protective environments (with high social control). Because there are few FH studies in adults that examine intersections with environmental context, we review evidence supporting social control mechanisms from twin and measured gene studies. Most of these studies have focused on proximal environmental exposures (Chartier, Karriker-Jaffe, Cummings, & Kendler, 2017). Alternatively, the current study focuses on two area-level indicators of social control: neighborhood alcohol availability and county-level adherence to religions with strong prohibitions against drinking.
Environmental social control processes decrease excessive alcohol use by regulating access to alcohol and helping to maintain social order through more restrictive social norms and involvement with prosocial institutions (including places of worship) that discourage alcohol use. (Dick and Kendler, 2012, Shanahan and Hofer, 2005) In areas with greater alcohol availability, alcohol consumption is higher (Popova et al., 2009, Scribner et al., 2000), and restricting the number of alcohol outlets in an area reduces alcohol problems (Livingston, Chikritzhs, & Room, 2007). Kendler, Gardner, and Dick (2011) found more pronounced genetic effects on alcohol consumption when access to alcohol was high, and this finding replicates at the area level. Specifically, one study of young adults found heritability of frequent drinking was stronger in areas with higher levels of alcohol availability than in areas without alcohol outlets (Slutske, Deutsch, & Piasecki, 2019), suggesting a lack of social control strengthens expression of genetic predispositions to heavy alcohol use.
Other studies have shown religious participation and affiliated practices act as social controls on alcohol use. Twin studies show genetic effects on alcohol use are attenuated at increasing levels of religiosity (Button et al., 2010, Koopmans et al., 1999). Chartier, Dick, and Almasy (2016) found genetic markers associated with alcohol metabolism had weaker effects on high-risk drinking as a function of increasing religious participation. This is the first study, to our knowledge, to examine the moderating effect of area-level religiosity. Because religious denominations play a role in both promoting abstinence and reducing heavy drinking among those who choose to drink (Michalak, Trocki, & Bond, 2007), we extend prior studies by examining area-level religious adherence and FH in relation to both high-risk drinking and dependence among current drinkers, while controlling for individual-level religious affiliation.
Some studies have shown area-level effects on alcohol outcomes vary by sex (Orozco et al., 2017, Karriker-Jaffe et al., 2018, Karriker-Jaffe et al., 2012, Brown et al., 2016). Other work suggests neighborhood areas may have stronger effects for Blacks/African Americans1 and Hispanics/Latinos/Latinas2 than Whites (Karriker-Jaffe et al., 2012, Jones-Webb et al., 1997, Glass et al., 2017, Zemore et al., 2016). Further, religious social controls on drinking may be stronger for women than for men (Michalak et al., 2007), and they may be stronger for Blacks, who are more likely to belong to religions that strongly discourage drinking alcohol, and for Hispanics, who show high levels of religiosity (Michalak et al., 2007). Thus, we examine interactions between FH and area-level social control factors separately by sex and by race/ethnicity. As individuals age into early and mid-adulthood, alcohol-specific genetic factors increase in influence (Kendler et al., 2011, van Beek et al., 2012), with effects moderated by interpersonal social controls (Barr, Salvatore, & Maes, 2017). As such, it is important to examine joint effects of FH and area-level social control in adult respondents across the lifespan.
1.3. Current study
The current study, like Dawson et al. (1992), examines FH across levels of relatedness in a sample of US adults. We examine associations of FH density with two alcohol outcomes, expecting drinkers with alcohol problems in close relatives3 or from more densely-affected families4 will be more likely to be high-risk drinkers and to have alcohol dependence. We also expect individuals residing in areas with greater alcohol availability to be more likely to be high-risk drinkers and to have alcohol dependence, while those residing in areas with greater adherence to religions that discourage or prohibit drinking will be less likely to be high-risk drinkers or alcohol dependent. To extend prior work, we examine whether relationships of FH with high-risk drinking and dependence vary by environmental context. We assess interactions of FH with our two social control measures. We expect environments characterized by low social control (greater alcohol availability) will be associated with a stronger relationship of FH with alcohol outcomes and environments associated with high social control (more religious adherents) will conversely be associated with weaker relationships. We explore differences in these effects by sex and by race/ethnicity as well.
2. Materials and methods
2.1. Sample description
Data were drawn from the pooled 2000, 2005 and 2010 U.S. National Alcohol Surveys (NAS). These surveys provide comprehensive data on alcohol consumption for residents of all 50 U.S. states and the District of Columbia. Data were collected using random digit dialing (RDD) strategies to sample from the non-institutionalized population ages 18 and older. Computer-assisted telephone interviews were conducted using landline telephones in 2000 and 2005, and both landline and cellular telephones in 2010. The surveys included targeted oversamples of Black and Hispanic respondents, and interviews were conducted in either English or Spanish. An introductory consent script was used, with the requirement for written proof of consent waived by the relevant Institutional Review Boards. Data were weighted to be population-representative at the time of data collection. More details on NAS methodology can be found elsewhere (Kerr, Mulia, & Zemore, 2014).
To ensure respondents had recent exposure to alcohol, the current sample was limited to 13,793 past-year drinkers (64.7% of weighted total sample), of whom 12,833 (91.8%) had data on their neighborhood of residence at the time of the survey. To allow subgroup analyses by race/ethnicity, we excluded 147 people who identified with any group other than White, Black, or Hispanic, as the other groups were too small for sub-analysis and too heterogeneous for combined analysis. The final, weighted analysis sample was 51.3% male and 80% White, 9% Black and 11% Hispanic (Table 1 ). A majority (61.6%) of Hispanics were born in the US. Approximately 33% of the sample came from each survey, with no differences in distribution across surveys by sex or race/ethnicity.
Table 1.
Characteristics of weighted sample of past-year drinkers, 2000–2010 US National Alcohol Surveys.
| Women | Men | Whites | Blacks | Hispanics | Total | |
|---|---|---|---|---|---|---|
| n = 6,603 | n = 6,083 | n = 8,880 | n = 1,850 | n = 1,956 | N = 12,686 | |
| High-risk drinking exceeding NIAAA recommended guidelines1, % | 46 | 48.7 | 48.3 | 35.3 | 51.7 | 47.4 a, bbb |
| Alcohol dependence symptoms, M(SD) | 0.27 (0.83) | 0.47 (1.06) | 0.33 (0.86) | 0.51 (1.44) | 0.57 (1.37) | 0.37 (0.97) aaa, bbb |
| Alcohol dependence2 , % | 2.6 | 5.7 | 3.5 | 6.2 | 7.3 | 4.2 aaa, bbb |
| Family history of alcohol problems, % | aaa, bbb | |||||
| Negative family history | 46.3 | 52.1 | 50.0 | 46.6 | 45.4 | 49.2 |
| Problems in extended family only | 19.9 | 20.2 | 19.4 | 24.2 | 21.3 | 20 |
| Problems in 1st degree relative(s) | 20.5 | 17.1 | 19.1 | 16.3 | 18.0 | 18.8 |
| Problems in 1st degree relative(s) & extended family | 13.3 | 10.7 | 11.5 | 13.0 | 15.3 | 12 |
| Liquor/convenience stores per square mile, M(SD) | 1.13 (2.56) | 1.15 (2.47) | 0.92 (2.06) | 2.09 (4.67) | 1.97 (3.60) | 1.14 (2.52) bbb |
| Religious adherents in county per 1,000 residents, M(SD) | 118.9 (113.4) | 120.8 (108.4) | 119.8 (107.3) | 140.7 (129.7) | 101.6 (96.6) | 119.9(111.0) bbb |
| Percent disadvantaged residents in neighborhood, M(SD) | 28.7 (9.8) | 28.9 (9.5) | 27.5 (8.0) | 34.5 (14.5) | 33.6 (14.5) | 28.8(9.7) bbb |
| Age, M(SD) | 44.3 (16.4) | 43.0 (15.1) | 45.1 (14.9) | 39.5 (17.3) | 36.6 (16.5) | 43.7 (15.8) aaa, bbb |
| Respondent age, % | bbb | |||||
| 18–29 | 21.8 | 23.4 | 19.9 | 29.1 | 37.2 | 22.6 |
| 30–39 | 20.3 | 21.7 | 19.8 | 25.8 | 26 | 21 |
| 40–49 | 21.8 | 21.2 | 22.1 | 20.7 | 17.4 | 21.5 |
| 50–59 | 17.9 | 17.3 | 18.7 | 14.2 | 12.3 | 17.6 |
| 60+ years | 18.3 | 16.4 | 19.5 | 10.1 | 7.2 | 17.3 |
| Education, % | aaa, bbb | |||||
| Less than high school | 6.5 | 9.8 | 5.7 | 12.1 | 23 | 8.2 |
| High school graduate | 27.1 | 28 | 26.7 | 34.8 | 27.2 | 27.5 |
| Some college | 31.8 | 26.8 | 29.3 | 29.6 | 28.4 | 29.2 |
| College graduate | 34.7 | 35.5 | 38.3 | 23.5 | 21.4 | 35.1 |
| Marital status, % | aaa, bbb | |||||
| Married/live with partner | 63 | 68.6 | 68.8 | 45.1 | 62.1 | 65.9 |
| Separated/divorced/widowed | 19 | 9.1 | 14.1 | 17.2 | 10 | 13.9 |
| Never married | 18.1 | 22.2 | 17.2 | 37.7 | 27.9 | 20.2 |
| Employment status, % | aaa, bbb | |||||
| Employed full- or part-time | 63.2 | 74.4 | 68.7 | 68.2 | 71.6 | 68.9 |
| Unemployed | 5.6 | 5.4 | 4.5 | 9.7 | 9 | 5.5 |
| Not in workforce | 31.1 | 20.3 | 26.8 | 22.1 | 19.4 | 25.6 |
| Income in 2005 US dollars, % | aaa, bbb | |||||
| Income less than $20,000 | 18.7 | 16.3 | 14.2 | 31.7 | 29.6 | 17.5 |
| Income $20,001–40,000 | 21.5 | 20.8 | 20.4 | 24.1 | 24 | 21.2 |
| Income $40,001–70,000 | 24.9 | 25.6 | 26.4 | 21.8 | 19.7 | 25.3 |
| Income $70,001+ | 22.4 | 28.2 | 27.8 | 13.8 | 17.4 | 25.3 |
| Missing | 12.5 | 9.1 | 11.2 | 8.6 | 9.3 | 10.7 |
| Own religion discourages drinking, % | 27.7 | 25.1 | 24 | 40.9 | 31.6 | 26.4 aa, bbb |
n, number of observations. a Sex differences, b Racial/ethnic differences. a,b p < 0.05, aa,bb p < 0.01, aaa,bbb p < 0.001 for each test.
1Past-year drinking more than 3 or 4 drinks/day or more than 7 or 14 drinks/week (for women and men, respectively);
2Past-year alcohol dependence symptoms in 3 or more of 7 domains; M, mean; SD, standard deviation.
2.2. Measures
2.2.1. High-risk drinking5
High-risk drinking was defined based on daily and weekly drinking guidelines (National Institute, 2009, U.S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010). Drinkers who exceeded daily and/or weekly guidelines in the past year were classified as at-risk drinkers, with low-risk drinkers as the referent.
2.2.2. Alcohol dependence
Alcohol dependence was measured by 17 items based on DSM-IV criteria (American Psychiatric Association, 1994) validated in prior NAS data (Caetano & Tam, 1995). A dichotomous variable indicated whether respondents reported at least one symptom in three or more of the seven criteria domains in the past year.6
2.2.3. Family history of alcohol problems
Family history of alcohol problems was assessed by asking respondents whether any of their blood relatives have ever been a “problem drinker or alcoholic”, with affirmative responses followed by a checklist of relatives. For this study, FH was implemented as a four-level variable: negative history (referent); extended family only (grandparents, aunts/uncles, cousins); first-degree relatives only (parents, siblings); and both first-degree and extended family (high FH density) (Dawson et al., 1992, Hill et al., 1994, Kendler et al., 2018). Measures of degree of FH provide more information than dichotomous parental or first-degree relative measures, as increases in an outcome measure with greater cumulative levels of FH imply genetic effects (Hill, Blow, Young, & Singer, 1994).
2.2.4. Neighborhood alcohol availability
Neighborhood alcohol availability was assessed based on ZIP code density per square mile of liquor stores and convenience stores that sell alcohol (range: 0–76, with the highest values representative of highly urban areas included in the national sample) (Ahern et al., 2015, Ahern et al., 2016, Ahern et al., 2013). Businesses were identified from the US Census Bureau’s national ZIP Code Business Patterns data for 2000, 2005 and 2010. Store classification was based on state laws, using published information on the types of stores allowed to sell beer, wine or spirits at the time of data collection (The Beverage Information Group, 2011a, The Beverage Information Group, 2011b, The Beverage Information Group, 2010, National Alcohol Beverage Control Association, 2010). These national data correspond well with official state licensure records (Matthews, McCarthy, & Rafail, 2011). Access to alcohol through off-premise outlets is associated with binge drinking (Ahern et al., 2016, Ahern et al., 2013) and AUD (Ahern, Balzer, & Galea, 2015).
2.2.5. County-level religious adherents
County-level religious adherents was the rate of residents per 1,000 who adhere to religions with strong prohibitions against drinking.7 Religion data came from the 2000 Religious Congregations and Membership Study (Jones, Doty, & Grammich, 2002) (for the 2000 and 2005 surveys) and the 2010 US Religion Census/Religious Congregations and Membership Study (Grammich, Hadaway, & Houseal, 2012) (for the 2010 survey).
2.2.6. Neighborhood disadvantage
Neighborhood disadvantage, a confounder, was based on proportions of adults without a high school diploma, males unemployed or not in labor force, people with incomes below the poverty limit or<50% of US median, and households without access to a car (Karriker-Jaffe et al., 2012). Neighborhood demographic data came from the 2000 US Decennial Census (for the 2000 and 2005 surveys) and the 2005–2009 American Community Survey (for the 2010 survey). An average neighborhood disadvantage score was calculated (M = 19.9%, SD = 10.8; Cronbach’s alpha = 0.89).
2.2.7. Demographic correlates
Demographic correlates were included in all models. Sex was coded with female as referent. Race/ethnicity was categorized using mutually-exclusive indicators for Black and Hispanic, with White as referent. Age was divided into 10-year intervals through 60+ years, with ages 18–29 as referent. Marital status was coded using indicators for never married, and separated/divorced/widowed, with currently married/living with partner as referent. Educational attainment was coded using three indicators for high school diploma/equivalent, some college, and four-year college/university degree, with less than high school as referent. Income was calculated in 2005 US dollars and coded using indicators for $20,001-$40,000; $40,001-$70,000; and $70,001 and up, with an extra indicator for missing income (approximately 13%), using income less than $20,000 per year as referent. Employment was coded with two indicators for unemployment and being out of the workforce (such as retired or homemaker), with full- or part-time employment as referent. Models also adjusted for whether the respondent reported their own religion discourages drinking; this was a dichotomous indicator, where all non-religious respondents were classified with those reporting that their own religion did not strongly discourage drinking (referent) (Michalak et al., 2007).
2.3. Analysis
Analyses were conducted using Stata (Stata Statistical Software, 2017) to accommodate sampling and non-response weights adjusting for survey design. Preliminary analyses found FH was not significantly associated with the area-level social control variables.8 Associations of alcohol outcomes with FH and area-level social control were assessed using adjusted logistic regression models that included all demographic controls and indicators for survey year (using 2000 as referent). Because the national samples were selected through RDD methods, multilevel modeling was not necessary. The multiplicative interactions were tested simultaneously, as correlations between the two area-level social control variables were modest.9 Interactive effects were assessed using multiple-degrees-of-freedom contrasts of the joint effects of the interaction (adjusted Wald tests), as well as tests of marginal effects of FH across different levels of the area-level variables. Due to generally limited power for tests of interactions (Frazier, Tix, & Barron, 2004), those interactions that did not reach p < 0.10 were removed to improve interpretability of the main effects (Aiken, West, & G., 1991). Preliminary analyses (see Supplemental Tables S1-S2) showed interactions of neighborhood alcohol availability with sex in relation to high-risk drinking, as well as an interaction of FH with race/ethnicity in relation to dependence, so we used stratified models for subgroup analyses, even though three-way interactions (such as sex X FH X outlet density) were not statistically significant. All demographic covariates and an indicator for survey year were included in the stratified models, although only selected coefficients are reported (full models available upon request).
3. Results
3.1. Models in the full sample
3.1.1. High-risk drinking
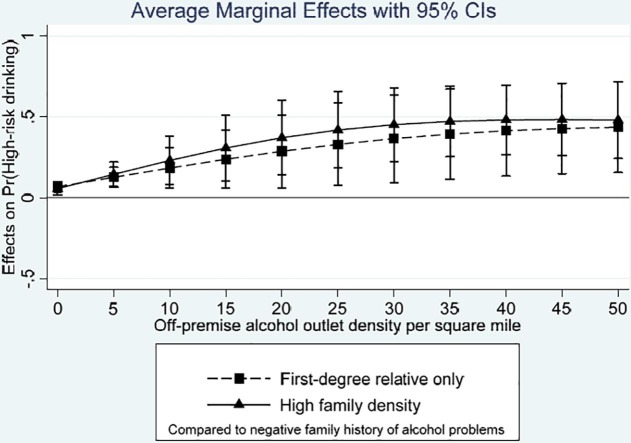
In the full sample (Table 2 ), there was an interaction of FH with alcohol availability in relation to high-risk drinking. Contrasts showed the interaction was present for the combined group of respondents with either an affected first-degree relative or with both affected first-degree and affected extended family members (F(2, 18951) = 3.06, p = .047). This group had a significant increase in high-risk drinking compared to negative FH, and these FH effects
Table 2.
Regression models in full sample of past-year drinkers.
| High-risk Drinking (wtd N = 9,999) |
Dependence (wtd N = 10,540) |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.297*** | (1.112–1.512) | 1.719** | (1.185–2.492) |
| AUD in 1st degree | 1.400*** | (1.194–1.641) | 2.383*** | (1.642–3.458) |
| AUD in 1st degree and extended | 1.323** | (1.093–1.601) | 4.451*** | (3.130–6.330) |
| Liquor/convenience stores per mi2 | 1.012 | (0.990–1.035) | 1.012 | (0.981–1.044) |
| Extended family X Liquor stores | 1.009 | (0.959–1.062) | –a | |
| 1st degree X Liquor stores | 1.056 | (0.989–1.128) | – | |
| 1st degree & extended X Liquor stores | 1.088* | (1.002–1.180) | – | |
| Religious adherents in countyb | 1.000+ | (0.999–1.000) | 1.001 | (1.000–1.002) |
| Neighborhood disadvantage | 0.717 | (0.386–1.334) | 0.470 | (0.103–2.137) |
| Male | 1.098+ | (0.984–1.226) | 2.641*** | (1.963–3.554) |
| Black | 0.414*** | (0.345–0.497) | 1.288 | (0.889–1.866) |
| Hispanic | 0.754** | (0.631–0.901) | 1.289 | (0.906–1.833) |
| Age 30–39 | 0.536*** | (0.445–0.644) | 0.748 | (0.528–1.060) |
| Age 40–49 | 0.312*** | (0.259–0.377) | 0.426*** | (0.278–0.652) |
| Age 50–59 | 0.204*** | (0.167–0.249) | 0.265*** | (0.163–0.430) |
| Age 60+ | 0.123*** | (0.098–0.154) | 0.076*** | (0.0325–0.177) |
| High school graduate | 0.772* | (0.615–0.970) | 0.618* | (0.410–0.932) |
| Some college | 0.898 | (0.714–1.129) | 0.683+ | (0.457–1.020) |
| College graduate | 0.704** | (0.558–0.889) | 0.414*** | (0.259–0.662) |
| Separated/divorced/widowed | 1.289*** | (1.116–1.489) | 1.724* | (1.128–2.633) |
| Never married | 1.353*** | (1.152–1.590) | 2.075*** | (1.483–2.904) |
| Unemployed | 1.068 | (0.809–1.410) | 1.619* | (1.026–2.556) |
| Not in workforce | 0.809** | (0.699–0.937) | 1.409+ | (0.945–2.099) |
| Income $20,001–40,000 | 1.049 | (0.881–1.250) | 0.624* | (0.434–0.897) |
| Income $40,001–70,000 | 1.193+ | (0.992–1.436) | 0.722 | (0.483–1.080) |
| Income $70,001+ | 1.375** | (1.125–1.680) | 0.797 | (0.492–1.292) |
| Missing income | 0.889 | (0.708–1.117) | 0.926 | (0.552–1.553) |
| Own religion discourages drinking | 0.599*** | (0.529–0.678) | 1.227 | (0.920–1.638) |
| 2005 NAS | 1.443*** | (1.278–1.629) | 1.041 | (0.773–1.401) |
| 2010 NAS | 1.299*** | (1.115–1.512) | 1.206 | (0.836–1.741) |
| Constant | 2.377*** | (1.651–3.423) | 0.0315*** | (0.0134–0.0737) |
Adjusted Wald test was not statistically significant for the interaction of FH with liquor store density for dependence (F(3,19522) = 0.44, p = .727), so interaction terms were removed to improve interpretability of the model.
The interaction of FH with religious density also was not statistically significant for high-risk drinking (F(3,18950) = 1.16, p = .323) or dependence (F(3,19522) = 0.33, p = .801).
p < 0.001,
p < 0.01,
p < 0.05,
p < 0.10.
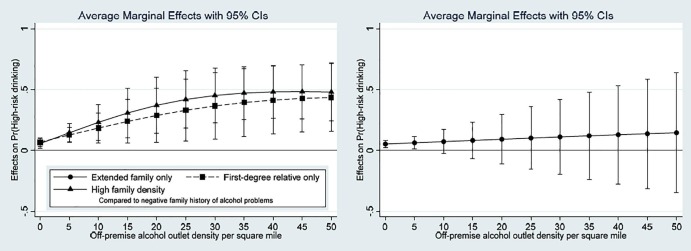
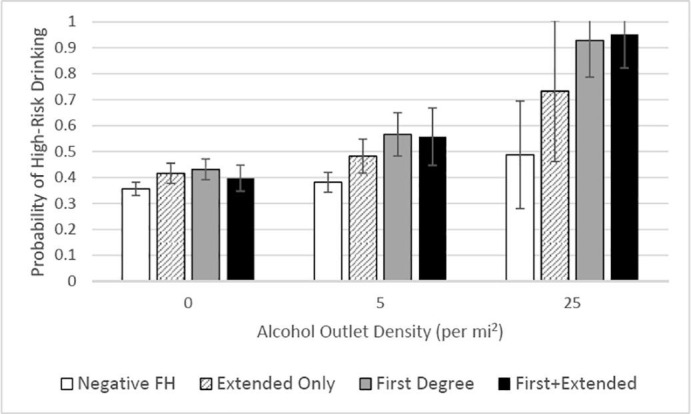
became stronger as alcohol availability increased (Fig. 1 , left panel). The average marginal effect of FH in only extended family members (compared to negative FH) was associated with increases in high-risk drinking at low levels of alcohol availability (Fig. 1, right panel), but this FH effect became non-significant as alcohol availability increased to 10+ outlets per square mile. However, the interaction of alcohol availability with only extended family was not significant (F(1,18952) = 0.12, p = .73). Predicted probabilities of high-risk drinking are shown in Fig. 2 for selected levels of alcohol availability, with higher values representing more urban settings. Testing the simple slope for alcohol availability across the four levels of FH revealed that alcohol availability was only significantly associated with high-risk drinking for people with either an affected first-degree relative (average marginal effect = 0.013, p = .034) or both a first-degree relative and extended family with alcohol problems (average marginal effect = 0.019, p = .016).
Fig. 1.
Effects of family history of alcoholism on high-risk drinking across levels of alcohol availability in full sample of drinkers. Note: Left panel depicts average marginal effects of first-degree relatives only (dashed line) and first-degree relatives plus extended family members (solid line) on high-risk drinking; right panel depicts average marginal effect of only extended family members on high-risk drinking. All are compared to negative family history of alcohol problems.
Fig. 2.
Predicted probability of high-risk drinking across levels of alcohol availability and family history of alcoholism in full sample of drinkers. Note: FH = family history. Extended Only = history of alcohol problems in extended family only (grandparents, aunts or uncles, cousins). First Degree = history of alcohol problems in first-degree relatives only (parents, siblings). First + Extended = history of alcohol problems in both first-degree relatives and extended family.
3.1.2. Dependence
The interaction of FH of alcohol problems with alcohol availability was not present for alcohol dependence. In the reduced main effect model (Table 2), FH density was increasingly associated with higher odds of dependence, as expected, but none of the area-level variables were associated with alcohol dependence.
3.2. Models stratified by sex
For female drinkers (see Table 3 ), there was an interaction of FH with alcohol availability in relation to high-risk drinking. Contrasts showed the interaction was significant for the group of women with either an affected first-degree relative or a high-density FH (adjusted Wald test: F(2,20479) = 3.49, p = .031). This followed a similar pattern as seen in the full sample (Fig. 3 ), with these women showing differentially elevated probability of high-risk drinking if they lived in areas with high alcohol availability.
Table 3.
Select coefficients from reduced models stratified by sex.
| Female Drinkers | ||||
|---|---|---|---|---|
| High-risk Drinking (wtd N = 4,797) |
Dependence (wtd N = 5,300) |
|||
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.354** | (1.077–1.703) | 1.999+ | (0.940–4.253) |
| AUD in 1st degree | 1.457*** | (1.158–1.832) | 2.677** | (1.302–5.501) |
| AUD in 1st degree and extended | 1.234 | (0.934–1.630) | 3.127** | (1.524–6.414) |
| Liquor/convenience stores per mi2 | 1.026 | (0.984–1.070) | 1.029 | (0.928–1.140) |
| Extended family X Liquor stores | 1.039 | (0.961–1.124) | 0.588* | (0.353–0.979) |
| 1st degree X Liquor stores | 1.110* | (1.003–1.228) | 0.860 | (0.663–1.116) |
| 1st degree & extended X Liquor stores | 1.138+ | (0.999–1.296) | 1.009 | (0.866–1.177) |
| Religious adherents in county | 1.000 | (0.999–1.000) | 1.001 | (0.999–1.003) |
| Neighborhood disadvantage | 0.548 | (0.224–1.342) | 3.598 | (0.281–46.105) |
| Own religion discourages drinking | 0.537*** | (0.449–0.642) | 1.282 | (0.823–1.998) |
| Male Drinkers | ||||
| High-risk Drinking (wtd N = 5,322) |
Dependence (wtd N = 5,360) |
|||
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.227* | (1.013–1.486) | 1.614+ | (0.988–2.636) |
| AUD in 1st degree | 1.367** | (1.114–1.677) | 2.050** | (1.227–3.425) |
| AUD in 1st degree and extended | 1.523*** | (1.195–1.941) | 4.628*** | (2.887–7.419) |
| Liquor/convenience stores per mi2 | 1.004 | (0.980–1.028) | 0.959 | (0.875–1.052) |
| Extended family X Liquor stores | – a | 1.081 | (0.969–1.207) | |
| 1st degree X Liquor stores | – | 1.125+ | (0.981–1.289) | |
| 1st degree & extended X Liquor stores | – | 1.108 | (0.964–1.273) | |
| Religious adherents in county | 0.999+ | (0.999–1.000) | 1.000 | (0.999–1.002) |
| Neighborhood disadvantage | 0.938 | (0.399–2.205) | 0.223 | (0.034–1.479) |
| Own religion discourages drinking | 0.653*** | (0.548–0.779) | 1.264 | (0.866–1.844) |
Note. Models also adjusted for age, race/ethnicity, level of education, marital status, employment status, income and survey year.
***p < 0.001, ** p < 0.01, * p < 0.05, + p < 0.10.
Adjusted Wald test for the interaction of FH with liquor store density for high-risk drinking by male drinkers was not statistically significant (F(3,20949) = 0.44, p = .725), so interaction terms were removed to improve interpretability of the model. None of the interactions of FH with religious density were statistically significant (all p > .10; detailed results available upon request), and they also were removed from the models.
Fig. 3.
Predicted probability of high-risk drinking across levels of alcohol availability and family history of alcoholism in female drinkers. Note: FH = family history. Extended Only = history of alcohol problems in extended family only (grandparents, aunts or uncles, cousins). First Degree = history of alcohol problems in first-degree relatives only (parents, siblings). First + Extended = history of alcohol problems in both first-degree relatives and extended family.
For women there also was an interaction of FH with alcohol availability in relation to dependence. Contrasts showed this was significant for women with only extended FH of alcohol problems, but the pattern of effects suggested lower probability of dependence for these women if they lived in areas with high alcohol availability (Fig. 4 , left panel).
Fig. 4.
Predicted probability of alcohol dependence across levels of alcohol availability and family history of alcoholism in female (left) and male (right) drinkers. Note: FH = family history. Extended Only = history of alcohol problems in extended family only (grandparents, aunts or uncles, cousins). First Degree = history of alcohol problems in first-degree relatives only (parents, siblings). First + Extended = history of alcohol problems in both first-degree relatives and extended family.
For male drinkers, there were no interactions for high-risk drinking. In reduced main effects models (Table 3), FH density was increasingly associated with higher odds of high-risk drinking, but none of the area-level variables were significant. For dependence, there was a marginal interaction of FH with alcohol availability. Contrasts showed this was just for men with only first-degree relatives with alcohol problems (Fig. 4, right panel).
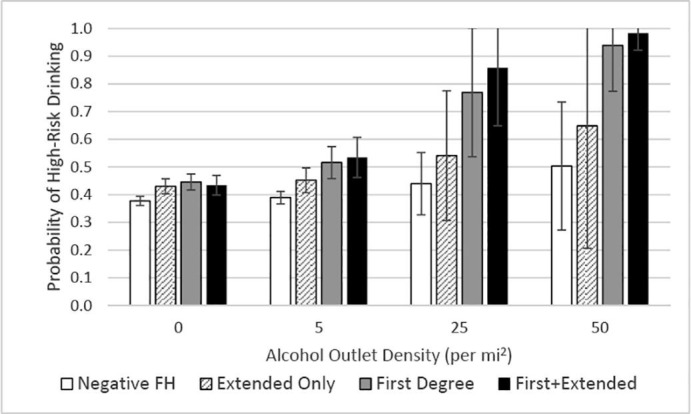
3.3. Models stratified by race/ethnicity
For White drinkers (see Table 4 ), there was an interaction of FH with area-level religious adherence in relation to high-risk drinking. Contrasts showed the interaction was present for those with an affected first-degree relative (adjusted Wald test: F(1,20449) = 5.30, p = .021). The average marginal effect of first-degree FH (compared to negative FH) on high-risk drinking was stronger at low levels of religious adherence in the county, and this effect became weaker as county-level religious adherence increased (Fig. 5 ). Stated another way, the risk of having one (or more) first-degree relatives with alcohol problems was exacerbated in areas with low religiosity and buffered in areas with high religiosity (Fig. 6 ). Average marginal effects for respondents with only extended family or with high FH density (compared to negative FH), were not as strongly attenuated as county-level religious adherence increased.
Table 4.
Select coefficients from reduced models stratified by race/ethnicity.
| White Drinkers | ||||
|---|---|---|---|---|
| High-risk Drinking (wtd N = 8,109) |
Dependence (wtd N = 8,527) |
|||
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.370** | (1.082–1.736) | 2.138** | (1.310–3.490) |
| AUD in 1st degree | 1.814*** | (1.437–2.289) | 2.861*** | (1.722–4.756) |
| AUD in 1st degree and extended | 1.582** | (1.200–2.086) | 5.506*** | (3.416–8.877) |
| Liquor/convenience stores per mi2 | 1.027+ | (0.999–1.055) | 1.008 | (0.963–1.056) |
| Religious adherence in county | 1.000 | (0.999–1.001) | 1.001 | (0.999–1.002) |
| Extended family X Religious adherence | 0.999 | (0.998–1.001) | – a | |
| 1st degree X Religious adherence | 0.998* | (0.997–1.000) | – | |
| 1st degree & extended X Religious adherence | 0.999 | (0.998–1.001) | – | |
| Neighborhood disadvantage | 0.646 | (0.295–1.412) | 1.340 | (0.144–12.466) |
| Own religion discourages drinking | 0.559*** | (0.481–0.649) | 1.132 | (0.764–1.677) |
| Black Drinkers | ||||
| High-risk Drinking (wtd N = 864) |
Dependence (wtd N = 928) |
|||
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.670** | (1.133–2.463) | 0.843 | (0.316–2.247) |
| AUD in 1st degree | 1.613* | (1.045–2.491) | 1.517 | (0.568–4.051) |
| AUD in 1st degree and extended | 2.007** | (1.297–3.107) | 4.440** | (1.760–11.206) |
| Liquor/convenience stores per mi2 | 1.018 | (0.981–1.056) | 0.882 | (0.720–1.079) |
| Extended family X Liquor stores | – b | 1.067 | (0.778–1.463) | |
| 1st degree X Liquor stores | – | 1.203+ | (0.967–1.497) | |
| 1st degree & extended X Liquor stores | – | 1.213 | (0.868–1.695) | |
| Religious adherence in county | 0.998* | (0.997–1.000) | 0.999 | (0.996–1.002) |
| Neighborhood disadvantage | 1.702 | (0.401–7.228) | 0.136 | (0.007–2.657) |
| Own religion discourages drinking | 0.722* | (0.531–0.981) | 1.420 | (0.747–2.701) |
| Hispanic Drinkersc | ||||
| High-risk Drinking (wtd N = 1,026) |
Dependence (wtd N = 1,086) |
|||
| OR | 95% CI | OR | 95% CI | |
| AUD in extended family only | 1.231 | (0.861–1.759) | 1.642 | (0.806–3.347) |
| AUD in 1st degree | 1.285 | (0.869–1.901) | 1.846+ | (0.933–3.651) |
| AUD in 1st degree and extended | 1.279 | (0.823–1.987) | 1.937* | (1.008–3.721) |
| Liquor/convenience stores per mi2 | 1.013 | (0.976–1.051) | 1.050 | (0.988–1.116) |
| Religious adherence in county | 1.000 | (0.999–1.002) | 1.002+ | (1.000–1.004) |
| Neighborhood disadvantage | 0.613 | (0.171–2.200) | 0.322 | (0.029–3.510) |
| Own religion discourages drinking | 0.759+ | (0.564–1.021) | 1.540+ | (0.926–2.563) |
Note. Models also adjusted for age, sex, level of education, marital status, employment status, income and survey year. *** p < 0.001, ** p < 0.01, * p < 0.05, + p < 0.10. a Adjusted Wald tests were not statistically significant for the interaction of FH with religious density for dependence among White drinkers (F(3,20828) = 0.36, p = .779); neither of the interactions of FH with liquor store density were statistically significant for White drinkers (both p > .10; detailed results available upon request), and they also were removed from the models to improve interpretability. b The interaction of FH with liquor store density for high-risk drinking among Black drinkers was not statistically significant (F(3,22005) = 1.00, p = .391), and neither of the interactions of FH with religious density were statistically significant for Black drinkers (both p > .10; detailed results available upon request); these interaction terms were removed from the models. c None of the interactions of FH with liquor store density or FH with religious density among Hispanic drinkers were statistically significant (all p > .10; detailed results available upon request), so all interaction terms were removed.
Fig. 5.
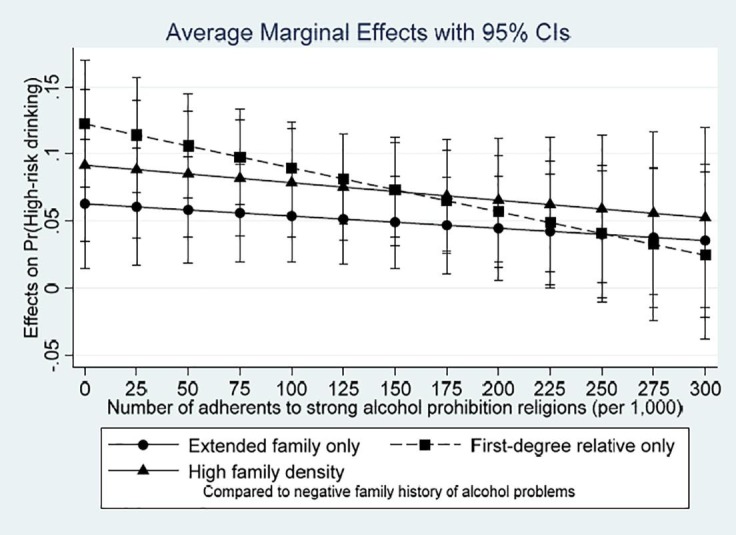
Effects of family history of alcoholism on high-risk drinking across levels of county-level religious adherence in White drinkers. Note: Average marginal effects of different family history densities, each compared to negative family history of alcohol problems.
Fig. 6.
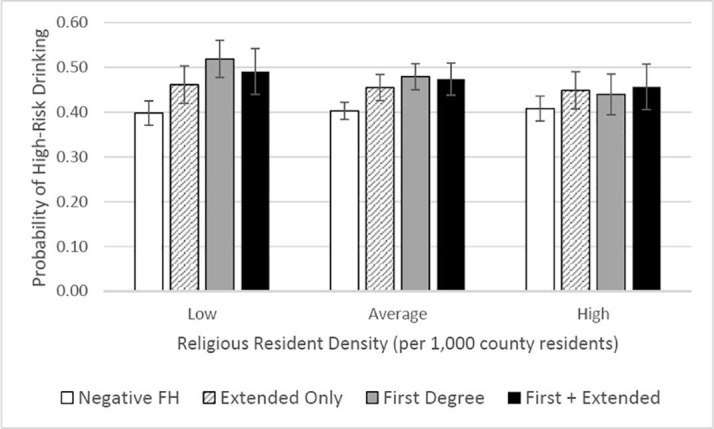
Predicted probability of high-risk drinking across levels of family history and county-level religious adherence in White drinkers. Note: FH = family history. Extended Only = history of alcohol problems in extended family only (grandparents, aunts or uncles, cousins). First Degree = history of alcohol problems in first-degree relatives only (parents, siblings). First + Extended = history of alcohol problems in both first-degree relatives and extended family.
The interaction of FH and county-level religious adherence was not present in relation to dependence among White drinkers. In the reduced main effect model (Table 4), FH was associated with higher odds of dependence, particularly for people with high FH density, but none of the area-level variables were associated with dependence.
For Black drinkers, there were no interactions of FH with the area-level variables in relation to high-risk drinking. In the reduced main effect models (Table 4), increasing FH density was associated with increased odds of high-risk drinking by Black drinkers. County-level religious adherence also was associated with higher odds of high-risk drinking.
In relation to dependence, contrasts showed a marginal interaction of first-degree FH with alcohol availability (adjusted Wald test: F(1,22114) = 2.74, p = .098). The pattern of effects suggested elevated probability of dependence for Black drinkers with affected first-degree relatives if they lived in areas with high alcohol availability (Fig. 7 ).
Fig. 7.
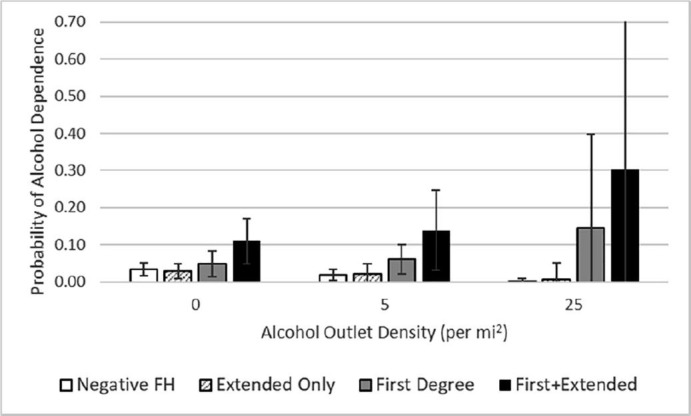
Predicted probability of alcohol dependence drinking across levels of alcohol availability and family history of alcoholism in Black drinkers. Note: FH = family history. Extended Only = history of alcohol problems in extended family only (grandparents, aunts or uncles, cousins). First Degree = history of alcohol problems in first-degree relatives only (parents, siblings). First + Extended = history of alcohol problems in both first-degree relatives and extended family.
For Hispanic drinkers, there were no interactions for either high-risk drinking or dependence. In reduced main effect models (Table 4), FH density was not significantly associated with high-risk drinking, and only the highest FH density level was associated with dependence. None of the area-level variables were significantly associated with high-risk drinking or dependence in Hispanic drinkers.
4. Discussion
Familial and area-level factors were associated with high-risk drinking and alcohol dependence in this national sample of adults, with findings similar to prior research on social control of heavy alcohol use and associated risk behaviors (Dick and Kendler, 2012, Kendler et al., 2011). We saw some key differences between predictors of high-risk drinking and alcohol dependence, however; full-sample models suggested context-dependent FH effects (evidenced by the interaction of FH and alcohol availability) for high-risk drinking and stronger FH main effects for dependence. The FH and alcohol dependence relationship may be less susceptible to changes in access to alcohol, once consumption becomes compulsive and motivated by negative reinforcement (Koob & Volkow, 2016), although this explanation does not fit with findings from our stratified analyses. A fuller examination of the different mechanisms through which FH and increased alcohol availability may affect high-risk drinking and alcohol dependence in different population subgroups is warranted. Considering the large proportion of the population with affected relatives, studies describing how FH of alcohol problems interacts with social control mechanisms has potential clinical and policy implications. However, few previous studies have examined sex- and racial/ethnic-specific influences of FH and area-level social controls on high-risk drinking and alcohol dependence.
Similar to prior studies with younger adults (Slutske et al., 2019a, Slutske et al., 2019b), in the full national sample, the effect of first-degree relatives and high FH density on high-risk drinking strengthened as alcohol availability increased. Post hoc analyses (described below) showed this did not vary systematically by age, although our results suggest there may be different combinations of risk factors that are salient for certain population subgroups. Specifically, the interaction of FH and alcohol availability in relation to high-risk drinking was replicated in the subsample of women, and a similar pattern emerged for alcohol dependence among men and among Black drinkers. The finding for Black drinkers aligns with earlier studies showing neighborhoods have stronger effects for Blacks than Whites on alcohol outcomes, but our results do not align with similar prior findings for Hispanics (Karriker-Jaffe et al., 2012, Jones-Webb et al., 1997, Glass et al., 2017, Zemore et al., 2016). More proximal social factors may have a greater relative importance for dependence among Hispanic individuals than area-level factors. In fact, other studies have suggested that FH and US generational status are important factors in understanding alcohol dependence among Hispanic drinkers (Chartier, Thomas, & Kendler, 2017), however, whether generational status and area-level factors are interdependent remains to be explored in more detail.
Interestingly, the interaction results seen in relation to high-risk drinking by women did not hold for men. Further, alcohol availability was not associated with high-risk drinking by men. Instead, for male drinkers the FH main effect was associated with high-risk drinking, with a pattern of increasing risk for greater FH density. Compared with the negative FH group, odds of high-risk drinking risk increased 50% for men with high-density FH, and this was independent of their social environment. By contrast, men’s odds of dependence increased as a function of both FH and alcohol availability. While an effect of FH on alcohol dependence is congruent with other studies (Dawson et al., 1992, Hill et al., 1994, Kendler et al., 2018), and previous work in other countries suggests alcohol availability may be more strongly associated with alcohol dependence among men than among women (Karriker-Jaffe, Ohlsson, Kendler, Cook, & Sundquist, 2018), the interactions suggest the local alcohol environment may play an especially important role in increasing risk for dependence for men and Black drinkers from high-risk families.
For White drinkers, higher religious social control reduced associations of first-degree FH with high-risk drinking, similar to other work using individual-level religious practices to measure social control (Button et al., 2010, Koopmans et al., 1999, Chartier et al., 2016). It was unexpected that these interactive effects did not emerge for women or for Blacks and Hispanics, given prior studies suggesting that religious social controls on drinking may be stronger for these demographic groups (Michalak et al., 2007). However, area-level religious effects were assessed when accounting for religious rules against drinking at the individual level, which was consistently associated with a lower likelihood of high-risk drinking across all sex and race/ethnicity subgroups. In post-hoc analyses, we tested whether individual-level religious prohibition on drinking moderated the associations of FH with the drinking outcomes, but there were no significant interactions in any of the three racial/ethnic subgroups for either outcome (all p > .10; detailed results available upon request). Further work to assess how individual- and area-level religion interact with each other, and with FH, in relation to adult drinkers’ alcohol consumption patterns and problems would be informative.
As noted above, this study was conducted in a national sample of adults. Research has shown that, while genetic factors account for 28% of the variance in alcohol dependence in adolescence, in young adulthood (age 30 to 32) effects of genetic factors nearly double (58%) and remain above 50% into adulthood (van Beek, Kendler, & de Moor, 2012). As such, in post-hoc analyses we checked for 3-way interactions (such as age X FH X outlet density) but these were not statistically significant when assessed several ways, including using the categorical age variable included in the adjusted models, using a continuous age variable, and using a dichotomous indicator separating respondents under age 40 from older respondents. It would be valuable for future studies to fully examine differences in FH effects and area-level social control on alcohol outcomes across the lifespan, including data from adolescents to older adults.
4.1. Study strengths and limitations
Our study used data from a large, nationally-representative sample of adult drinkers to examine associations of FH of alcohol problems with two different alcohol outcomes along the risk continuum. The large sample also permitted us to examine differences by sex and by race/ethnicity. These strengths are somewhat offset by a few limitations. First, despite the large sample, we may have had limited power to test some interactions in the stratified models. Further, based on available survey measures, we used DSM-IV criteria for alcohol dependence, so our findings bear replication using DSM-5 criteria. With a large enough sample, this would allow distinction of risk factors for mild, moderate and severe AUD. Additionally, our measure of FH considered the presence of affected relatives across multiple generations (Dawson et al., 1992, Hill et al., 1994, Kendler et al., 2018); however, we were unable to assess the proportion of affected relatives (Turner et al., 1993, Stoltenberg et al., 1998, Milne et al., 2008) or to parse out genetic influences from family environment effects (Light et al., 1996, Zucker et al., 1994). Most family method studies for AUD (Roy et al., 1994, Roy et al., 1996, Rice et al., 1995) show high specificity (correct indication of negative diagnosis) and moderate sensitivity (correct indication of positive diagnosis), but also acknowledge the potential for reporting bias based on the sex and age of both the informant and the subject, as well as the closeness of the relationship between the subject and informant. Future studies with more detailed FH measures would be informative in this regard. Finally, although we tested whether FH was associated with the social control indicators and did not find evidence for gene-environment correlation,8 twin and adoption studies and longitudinal studies are better-suited to testing neighborhood selection effects.
5. Conclusions
Low social control—in particular, greater density of off-premise alcohol outlets—appears to exacerbate associations between family history of alcohol problems and high-risk drinking by adults. Sex- and racial/ethnic-specific differences did appear, suggesting that risk factors for AUD do not increase liability for alcohol use for all groups equally. Clinicians should consider not only family history but also area-level factors as they gather information and prepare treatment plans for their clients. Policymakers should consider benefits of decreasing alcohol availability, especially for people from high-risk families, to reduce high-risk drinking and associated problems. Retirement of outlet licenses for businesses lost during the recession due to the coronavirus 2019 (COVID-19) pandemic may provide a legislative opportunity to decrease alcohol availability.
6. Role of funding sources
This work was supported by the National Institutes of Health’s National Institute on Alcohol Abuse and Alcoholism (P50AA005595 & K01AA021145) and National Institute on Drug Abuse (K01DA036681). The supporting organizations had no role in study design, data collection, data analysis, interpretation of results or decision to submit the manuscript for publication. The content of this paper is the sole responsibility of the authors and does not reflect official positions of NIH, NIAAA or NIDA.
7. Contributors
Karriker-Jaffe contributed to data curation, conceptualization, formal analysis, data interpretation, and writing the original draft. Chartier contributed to conceptualization, data interpretation, and writing the original draft. Bares contributed to data interpretation and writing the original draft. Kendler contributed to conceptualization and writing (review and editing). Greenfield contributed to funding acquisition, conceptualization, and writing (review and editing). All authors materially participated in the work and have approved the final manuscript.
8. Author agreement
The work described has not been published previously (except in the form of an early abstract) and is not under consideration for publication elsewhere. Its submission is approved by all authors and tacitly by the responsible authorities where the work was carried out. If accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
CRediT authorship contribution statement
Katherine J. Karriker-Jaffe: Conceptualization, Data curation, Formal analysis, Writing - original draft. Karen G. Chartier: Conceptualization, Writing - original draft. Cristina B. Bares: Writing - original draft. Kenneth S. Kendler: Conceptualization, Writing - review & editing. Thomas K. Greenfield: Funding acquisition, Conceptualization, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Hereafter, Blacks.
Hereafter, Hispanics.
First-degree relatives.
Affected family of first degree, plus second- or third-degree relatives with alcohol problems.
These guidelines recommend no more than 4 drinks in any single day and no more than 14 drinks per week on average for men and no more than 3 drinks in a day and no more than 7 drinks per week on average for women.
The DSM-IV domains assessed were withdrawal; tolerance; drinking despite consequences; unsuccessful efforts to reduce drinking; drinking more than intended; time spent drinking/recovering; and giving up activities because of drinking.
These religions included Baptist, Assembly of God, Mormon, Pentecostal, Seventh-Day Adventist and Muslim denominations (Michalak et al., 2007).
Adjusted Wald tests from regression models testing associations of FH with logged values for alcohol outlet density and religious adherent density were not statistically significant (F(3,19522)=1.27, p=.283 and F(3,19522)=1.06, p=.366, respectively).
The correlation between neighborhood alcohol outlet density and county-level density of adherents to religions with strong prohibitions on drinking was −0.13.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.addbeh.2020.106668.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahern J., Balzer L., Galea S. The roles of outlet density and norms in alcohol use disorder. Drug and Alcohol Dependence. 2015;151:144–150. doi: 10.1016/j.drugalcdep.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahern J., Colson K.E., Margerson-Zilko C., Hubbard A., Galea S. Predicting the population health impacts of community interventions: The case of alcohol outlets and binge drinking. American Journal of Public Health. 2016;106(11):1938–1943. doi: 10.2105/AJPH.2016.303425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahern J., Margerison-Zilko C., Hubbard A., Galea S. Alcohol outlets and binge drinking in urban neighborhoods: The implications of nonlinearity for intervention and policy. American Journal of Public Health. 2013;103(4):e81–e87. doi: 10.2105/AJPH.2012.301203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.S., West S.G. Sage Publications; Newbury Park, CA: 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- American Psychiatric Association . 4th ed. American Psychiatric Association; Washington, DC: 1994. DSM-IV: Diagnostic & statistical manual of mental disorders. [Google Scholar]
- Bailey J.A., Hill K.G., Meacham M.C., Young S.E., Hawkins J.D. Strategies for characterizing complex phenotypes and environments: General and specific family environmental predictors of young adult tobacco dependence, alcohol use disorder, and co-occurring problems. Drug and Alcohol Dependence. 2011;118(2–3):444–451. doi: 10.1016/j.drugalcdep.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr P.B., Salvatore J.E., Maes H.H. Social Relationships Moderate Genetic Influences on Heavy Drinking in Young Adulthood. Journal of Studies on Alcohol and Drugs. 2017;78(6):817–826. doi: 10.15288/jsad.2017.78.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beseler C.L., Aharonovich E., Keyes K.M., Hasin D.S. Adult transition from at-risk drinking to alcohol dependence: The relationship of family history and drinking motives. Alcoholism, Clinical and Experimental Research. 2008;32(4):607–616. doi: 10.1111/j.1530-0277.2008.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Q., Milam A.J., Bowie J.V., Ialongo N.S., Gaskin D.J., Furr-Holden D. The moderating role of gender in the relationship between tobacco outlet exposure and tobacco use among African American Young Adults. Prevention Science. 2016;17(3):338–346. doi: 10.1007/s11121-015-0622-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button T.M., Hewitt J.K., Rhee S.H., Corley R.P., Stallings M.C. The moderating effect of religiosity on the genetic variance of problem alcohol use. Alcoholism, Clinical and Experimental Research. 2010;34(9):1619–1624. doi: 10.1111/j.1530-0277.2010.01247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R., Tam T.W. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence: 1990 U.S. National Alcohol Survey. Alcohol and Alcoholism. 1995;30(2):177–186. [PubMed] [Google Scholar]
- Chartier K.G., Dick D.M., Almasy L. Interactions between alcohol metabolism genes and religious involvement in association with maximum drinks and alcohol dependence symptoms. Journal of Studies on Alcohol and Drugs. 2016;77(3):393–404. doi: 10.15288/jsad.2016.77.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier K.G., Hesselbrock M.N., Hesselbrock V.M. Development and vulnerability factors in adolescent alcohol use. Child and Adolescent Psychiatric Clinics of North America. 2010;19(3):493–504. doi: 10.1016/j.chc.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier K.G., Karriker-Jaffe K.J., Cummings C.R., Kendler K.S. Environmental influences on alcohol use: Informing research on the joint effects of genes and the environment in diverse U.S. populations. American Journal on Addictions. 2017 doi: 10.1111/ajad.12478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier K.G., Thomas N.S., Kendler K.S. Interrelationship between family history of alcoholism and generational status in the prediction of alcohol dependence in US Hispanics. Psychological Medicine. 2017;47(1):137–147. doi: 10.1017/S0033291716002105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.A., Harford T.C., Grant B.F. Family history as a predictor of alcohol dependence. Alcoholism, Clinical and Experimental Research. 1992;16(3):572–575. doi: 10.1111/j.1530-0277.1992.tb01419.x. [DOI] [PubMed] [Google Scholar]
- Dick D.M., Kendler K.S. The impact of gene-environment interaction on alcohol use disorders. Alcohol Research. 2012;34(3):318–324. [PMC free article] [PubMed] [Google Scholar]
- Elliott J.C., Carey K.B., Bonafide K.E. Does family history of alcohol problems influence college and university drinking or substance use? A meta-analytical review. Addiction. 2012;107(10):1774–1785. doi: 10.1111/j.1360-0443.2012.03903.x. [DOI] [PubMed] [Google Scholar]
- Frazier P.A., Tix A.P., Barron K.E. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol. 2004;51(1):115–134. [Google Scholar]
- Glass J.E., Rathouz P.J., Gattis M., Joo Y.S., Nelson J.C., Williams E.C. Intersections of poverty, race/ethnicity, and sex: Alcohol consumption and adverse outcomes in the United States. Social Psychiatry and Psychiatric Epidemiology. 2017;52(5):515–524. doi: 10.1007/s00127-017-1362-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grammich C., Hadaway C., Houseal R. Association of Statisticians of American Religious Bodies; Kansas City, MO: 2012. 2010 U.S. Religious Census: Religious Congregations & Membership Study. [Google Scholar]
- Harford T.C., Parker D.A., Grant B.F. Family history, alcohol use and dependence symptoms among young adults in the United States. Alcoholism, Clinical and Experimental Research. 1992;16(6):1042–1046. doi: 10.1111/j.1530-0277.1992.tb00696.x. [DOI] [PubMed] [Google Scholar]
- Hill E.M., Blow F.C., Young J.P., Singer K.M. Family history of alcoholism and childhood adversity: Joint effects on alcohol consumption and dependence. Alcoholism, Clinical and Experimental Research. 1994;18(5):1083–1090. doi: 10.1111/j.1530-0277.1994.tb00085.x. [DOI] [PubMed] [Google Scholar]
- Irons D.E., Iacono W.G., Oetting W.S., McGue M. Developmental trajectory and environmental moderation of the effect of ALDH2 polymorphism on alcohol use. Alcoholism, Clinical and Experimental Research. 2012;36(11):1882–1891. doi: 10.1111/j.1530-0277.2012.01809.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D.E., Doty S., Grammich C. Glenmary Research Center; Nashville, TN: 2002. Religious congregations and membership in the United States. [Google Scholar]
- Jones-Webb R., Snowden L., Herd D., Short B., Hannan P. Alcohol-related problems among black, Hispanic and white men: The contribution of neighborhood poverty. Journal of Studies on Alcohol. 1997;58(5):539–545. doi: 10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- Kaplan L.M., Nayak M.B., Greenfield T.K., Karriker-Jaffe K. Alcohol’s harm to children: Findings from the 2015 United States National Alcohol’s Harm to Others Survey. The Journal of Pediatrics. 2017;184:186–192. doi: 10.1016/j.jpeds.2017.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Greenfield T.K., Kaplan L.M. Distress and alcohol-related harms from intimates, friends, and strangers. Journal of Substance Misuse. 2017;22(4):434–441. doi: 10.1080/14659891.2016.1232761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Lonn S.L., Cook W.K., Kendler K.S., Sundquist K. Chains of risk for alcohol use disorder: Mediators of exposure to neighborhood deprivation in early and middle childhood. Health Place. 2018;50:16–26. doi: 10.1016/j.healthplace.2017.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Ohlsson H., Kendler K.S., Cook W.K., Sundquist K. Alcohol availability and onset and recurrence of alcohol use disorder: Examination in a longitudinal cohort with cosibling analysis. Alcoholism, Clinical and Experimental Research. 2018;42(6):1105–1112. doi: 10.1111/acer.13752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Zemore S.E., Mulia N., Jones-Webb R., Bond J., Greenfield T.K. Neighborhood disadvantage and adult alcohol outcomes: Differential risk by race and gender. Journal of Studies on Alcohol and Drugs. 2012;73(6):865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K., Zenmore S.E., Mulia N., Jones-Webb R., Bond J., Greenfield T.K. Neighborhood disadvantage and adult alcohol outcomes: Differential risk by race and gender. Journal of Studies on Alcohol and Drugs. 2012;73(6):865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Edwards A., Myers J., Cho S.B., Adkins A., Dick D. The predictive power of family history measures of alcohol and drug problems and internalizing disorders in a college population. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2015;168B(5):337–346. doi: 10.1002/ajmg.b.32320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Gardner C., Dick D.M. Predicting alcohol consumption in adolescence from alcohol-specific and general externalizing genetic risk factors, key environmental exposures and their interaction. Psychological Medicine. 2011;41(7):1507–1516. doi: 10.1017/S003329171000190X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Ohlsson H., Sundquist J., Sundquist K. Transmission of alcohol use disorder across three generations: A Swedish National Study. Psychological Medicine. 2018;48(1):33–42. doi: 10.1017/S0033291717000794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr W.C., Mulia N., Zemore S.E.U.S. trends in light, moderate, and heavy drinking episodes from 2000 to 2010. Alcoholism, Clinical and Experimental Research. 2014;38(9):2496–2501. doi: 10.1111/acer.12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoddam R., Worley M., Browne K.C., Doran N., Brown S.A. Family history density predicts long term substance use outcomes in an adolescent treatment sample. Drug and Alcohol Dependence. 2015;147:235–242. doi: 10.1016/j.drugalcdep.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob G.F., Volkow N.D. Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry. 2016;3(8):760–773. doi: 10.1016/S2215-0366(16)00104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmans J.R., Slutske W.S., van Baal G.C., Boomsma D.I. The influence of religion on alcohol use initiation: Evidence for genotype X environment interaction. Behavior Genetics. 1999;29(6):445–453. doi: 10.1023/a:1021679005623. [DOI] [PubMed] [Google Scholar]
- Light J.M., Irvine K.M., Kjerulf L. Estimating genetic and environmental effects of alcohol use and dependence from a national survey: A “quasi-adoption” study. Journal of Studies on Alcohol. 1996;57(5):507–520. doi: 10.15288/jsa.1996.57.507. [DOI] [PubMed] [Google Scholar]
- Livingston M., Chikritzhs T., Room R. Changing the density of alcohol outlets to reduce alcohol-related problems. Drug and Alcohol Review. 2007;26(5):557–566. doi: 10.1080/09595230701499191. [DOI] [PubMed] [Google Scholar]
- Matthews S.A., McCarthy J.D., Rafail P.S. Using ZIP code business patterns data to measure alcohol outlet density. Addictive Behaviors. 2011;36(7):777–780. doi: 10.1016/j.addbeh.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak L., Trocki K., Bond J. Religion and alcohol in the U.S. National Alcohol Survey: How important is religion for abstention and drinking? Drug and Alcohol Dependence. 2007;87(2–3):268–280. doi: 10.1016/j.drugalcdep.2006.07.013. [DOI] [PubMed] [Google Scholar]
- Milne B.J., Caspi A., Harrington H., Poulton R., Rutter M., Moffitt T.E. Predictive value of family history on severity of illness: The case for depression, anxiety, alcohol dependence, and drug dependence. Archives of General Psychiatry. 2009;66(7):738–747. doi: 10.1001/archgenpsychiatry.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne B.J., Moffitt T.E., Crump R. How should we construct psychiatric family history scores? A comparison of alternative approaches from the Dunedin Family Health History Study. Psychological Medicine. 2008;38(12):1793–1802. doi: 10.1017/S0033291708003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alcohol Beverage Control Association . National Alcohol Beverage Control Association; Alexandria, VA: 2010. NABCA Survey Book: 2010. [Google Scholar]
- National Institute on Alcoholism and Alcohol Abuse (2009). Rethinking Drinking: Alcohol and your health [Accessed: 2011-03-02. Archived by WebCite® at http://www.webcitation.org/5wtRANlQ7]. Bethesda, MD: National Institute on Alcoholism and Alcohol Abuse; February 2009. NIH publication; 09-3770.
- Nayak M.B., Patterson D., Wilsnack S.C., Karriker-Jaffe K., Greenfield T.K. Alcohol’s Secondhand Harms in the United States: New data on prevalence and risk factors. Journal of Studies on Alcohol and Drugs. 2019;80(3):273–281. doi: 10.15288/jsad.2019.80.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orozco R., Benjet C., Ruiz Velasco-Acosta S. Area-level disadvantage and alcohol use disorder in northern Mexico. Drug and Alcohol Dependence. 2017;175:219–226. doi: 10.1016/j.drugalcdep.2017.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson P.L., Hawkins J.D., Abbott R.D., Catalano R.F. Disentangling the effects of parental drinking, family management, and parental alcohol norms on current drinking by Black and White adolescents. Journal of Research on Adolescence. 1994;4(2):203–227. [Google Scholar]
- Popova S., Giesbrecht N., Bekmuradov D., Patra J. Hours and days of sale and density of alcohol outlets: Impacts on alcohol consumption and damage: A systematic review. Alcohol and Alcoholism. 2009;44(5):500–516. doi: 10.1093/alcalc/agp054. [DOI] [PubMed] [Google Scholar]
- Rice J.P., Reich T., Bucholz K.K. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcoholism, Clinical and Experimental Research. 1995;19(4):1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- Roy M.A., Walsh D., Kendler K.S. Accuracies and inaccuracies of the family history method: A multivariate approach. Acta Psychiatrica Scandinavica. 1996;93(4):224–234. doi: 10.1111/j.1600-0447.1996.tb10639.x. [DOI] [PubMed] [Google Scholar]
- Roy M.A., Walsh D., Prescott C.A., Kendler K.S. Biases in the diagnosis of alcoholism by the family history method. Alcoholism, Clinical and Experimental Research. 1994;18(4):845–851. doi: 10.1111/j.1530-0277.1994.tb00049.x. [DOI] [PubMed] [Google Scholar]
- Russell M., Cooper M.L., Frone M.R. The influence of sociodemographic characteristics on familial alcohol problems: Data from a community sample. Alcoholism, Clinical and Experimental Research. 1990;14(2):221–226. doi: 10.1111/j.1530-0277.1990.tb00476.x. [DOI] [PubMed] [Google Scholar]
- Scribner R.A., Cohen D.A., Fisher W. Evidence of a structural effect for alcohol outlet density: A multilevel analysis. Alcoholism, Clinical and Experimental Research. 2000;24(2):188–195. [PubMed] [Google Scholar]
- Shanahan M.J., Hofer S.M. Social context in gene-environment interactions: retrospect and prospect. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60(Spec No 1):65–76. doi: 10.1093/geronb/60.special_issue_1.65. [DOI] [PubMed] [Google Scholar]
- Slutske W.S., Deutsch A.R., Piasecki T.M. Neighborhood density of alcohol outlets moderates genetic and environmental influences on alcohol problems. Addiction. 2019;114(5):815–822. doi: 10.1111/add.14534. [DOI] [PubMed] [Google Scholar]
- Slutske W.S., Deutsch A.R., Piasecki T.M. Neighborhood alcohol outlet density and genetic influences on alcohol use: Evidence for gene-environment interaction. Psychological Medicine. 2019;49(3):474–482. doi: 10.1017/S0033291718001095. [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software: Release 15 [computer program]. (2017). College Station, TX: StataCorp LLC.
- Stoltenberg S.F., Mudd S.A., Blow F.C., Hill E.M. Evaluating measures of family history of alcoholism: Density versus dichotomy. Addiction. 1998;93(10):1511–1520. doi: 10.1046/j.1360-0443.1998.931015117.x. [DOI] [PubMed] [Google Scholar]
- The Beverage Information Group . The Beverage Information Group Publications; Norwalk, CT: 2010. Beer Handbook. [Google Scholar]
- The Beverage Information Group . The Beverage Information Group Publications; Norwalk, CT: 2011. Liquor Handbook. [Google Scholar]
- The Beverage Information Group . The Beverage Information Group Publications; Norwalk, CT: 2011. Wine Handbook. [Google Scholar]
- Thomas N.S., Adkins A., Aliev F. Alcohol metabolizing polygenic risk for alcohol consumption in European American college students. Journal of Studies on Alcohol and Drugs. 2018;79(4):627–634. doi: 10.15288/jsad.2018.79.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner W.M., Cutter H.S., Worobec T.G., O'Farrell T.J., Bayog R.D., Tsuang M.T. Family history models of alcoholism: Age of onset, consequences and dependence. Journal of Studies on Alcohol. 1993;54(2):164–171. doi: 10.15288/jsa.1993.54.164. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, U.S. Department of Health and Human Services. (2010). Dietary Guidelines for Americans, 2010 [Accessed: 2011-02-08. Archived by WebCite® at http://www.webcitation.org/5wM9GjvZ3]. 7th ed. Washington, DC: US Government Printing Office.
- van Beek J.H., Kendler K.S., de Moor M.H. Stable genetic effects on symptoms of alcohol abuse and dependence from adolescence into early adulthood. Behavior Genetics. 2012;42(1):40–56. doi: 10.1007/s10519-011-9488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhulst B., Neale M.C., Kendler K.S. The heritability of alcohol use disorders: A meta-analysis of twin and adoption studies. Psychological Medicine. 2015;45(5):1061–1072. doi: 10.1017/S0033291714002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski T.C., Pedersen S.L., McCarthy D.M., Smith G.T. Less drinking, yet more problems: Understanding African American drinking and related problems. Psychological Bulletin. 2014;140(1):188–223. doi: 10.1037/a0032113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S.E., Karriker-Jaffe K.J., Keithly S., Mulia N. Racial prejudice and unfair treatment: Interactive effects with poverty and foreign nativity on problem drinking. Journal of Studies on Alcohol and Drugs. 2011;72(3):361–370. doi: 10.15288/jsad.2011.72.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S.E., Ye Y., Mulia N., Martinez P., Jones-Webb R., Karriker-Jaffe K. Poor, persecuted, young, and alone: Toward explaining the elevated risk of alcohol problems among Black and Latino men who drink. Drug and Alcohol Dependence. 2016;163:31–39. doi: 10.1016/j.drugalcdep.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker R.A., Ellis D.A., Fitzgerald H.E. Developmental evidence for at least two alcoholisms. I. Biopsychosocial variation among pathways into symptomatic difficulty. Annals of the New York Academy of Sciences. 1994;708:134–146. doi: 10.1111/j.1749-6632.1994.tb24706.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.