Abstract
Background
COVID-19 continues to affect the dental community worldwide. The authors conducted a cross-sectional electronic study using a multisite survey to examine dentists’ knowledge, attitudes, and professional behavior toward COVID-19 and the affect on their livelihood.
Methods
A questionnaire was circulated via e-mail and social media platforms to dentists in North America, Europe, Eastern Mediterranean, and Western Pacific regions. It covered demographic characteristics and questions about the COVID-19 outbreak related to dentists’ levels of comfort for preventive and safety measures, provision of treatment, affect on work, and financial implications. Responses were tabulated and analyzed by means of χ2 or Fisher exact test. Mann-Whitney and Kruskal-Wallis tests were used to compare means. P < .05 was considered significant.
Results
A total of 1,251 dentists responded. General dentists represented 63.9% of the respondents and 62.5% worked in private practice. The global score for level of comfort with the preventive measures and provisions of treatment during the COVID-19 pandemic was low (14 of 30), and differences between regions were significant (P < .01); dentists working in private practice and general dental practitioners were less comfortable (P < .01).
Conclusions and Practical Implications
The respondents reported a lack of preparedness to confront a highly infectious respiratory disease. A new level of protective armamentarium in the dental operatory and updated operational guidance and policies are required, necessitating educators and regulators to ensure the delivery of knowledge and skills to oral health care providers. Dentists need to address the sustainability of their practices and have a robust business plan.
Key Words: Dentist awareness, dentist level of comfort, COVID-19, personal protective equipment, N95 respirator, affect on practice, financial impact
Abbreviation Key: ADA, American Dental Association; PPE, Personal protective equipment; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2

On January 30, 2020, the World Health Organization declared that COVID-19 was a Public Health Emergency of International Concern, and on March 11, 2020, after the rapid spread of the disease beyond China, the World Health Organization declared COVID-19 a pandemic. The affect of the outbreak has been felt across the globe.1 On March 16, 2020, the American Dental Association (ADA), the largest professional organization that advocates for dentists and public health in the United States, called on dentists to postpone elective dental procedures for 3 weeks to mitigate the spread of COVID-19 and to reserve treatment for emergencies only (the ADA addressed what constitutes “emergency” and “nonemergency”2); this suspension was extended subsequently. The National Health Service in the United Kingdom took a similar action on March 25, 2020.3 The Centers for Disease Control and Prevention, ADA, and World Health Organization published guidance for oral health care providers on how to control the spread of the disease.4, 5, 6 The science and understanding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 are evolving, and recommendations and guidance are modified continuously as a result of this scientific evidence.
The highly infectious nature of COVID-19, a disease transmitted through aerosols, droplets, and contact routes even in patients who are asymptomatic, requires robust personal protection for staff members and screening protocols for patients, undermining the standard personal protective equipment (PPE) used in dentistry.7
The frequency with which guidance is issued, the need to adopt more advanced measures for infection control in the dental practice, and the restrictions imposed on the scope of practice created an unprecedented challenge to oral health care. We believe that dentists are not well prepared to confront the pandemic or similar future outbreaks. The aims of our multisite cross-sectional study were to capture dentists’ perceptions of preventive measures and level of comfort with providing treatment to patients with COVID-19, as well as assess the affect that the outbreak has had on their practice and finances.
Methods
We developed an electronic questionnaire that received approval from the Research Ethics Committee, Deanship of Research, Jordan University (electronic approval dated April 1, 2020). A statement at the beginning of the questionnaire introduced the purpose of our study, and acceptance to participate was considered as consent; no incentives were provided to the respondents. Dental practitioners from Eastern Mediterranean, Europe, North America, and Western Pacific regions were invited to participate via e-mail, WhatsApp, or postings on social media platforms that included a link to the survey. The survey included closed-ended questions and partially closed-ended questions. It was available from March 28 through April 10, 2020, and was composed of 2 parts. The first part gathered demographic data, such as sex, age, country of practice, scope of practice (general dental practitioner versus specialist), place of practice (private versus public), employment status (full time versus part time), and experience (experienced, with ≥ 10 years or junior, with < 10 years). The second part consisted of 5 main sections with a total of 18 questions. Section 1 examined level of comfort with preventive measures and provision of treatment in the dental practice setting during the COVID-19 pandemic (6 questions); a 5-point Likert scale was used (1 equals extremely uncomfortable and 5 equals extremely comfortable). Section 2 assessed the understanding of benefits and use of N95 respirators (4 questions). Section 3 assessed attitudes toward treating patients with or suspected of having COVID-19 (1 question). Section 4 investigated the affect that COVID-19 outbreak had on the workplace (4 questions). Section 5 examined the financial impact of COVID-19 (3 questions). Statistical analyses were performed using SPSS Statistics for Windows, Version 25.0 (IBM). Categorical variables were described as frequencies and percentages and continuous variables as means (standard deviations). The score for level of comfort and safety per respondent was calculated by means of summing the answers to the 6 questions. Cross-tabulation was used to examine the independence among related categorical variables and statistics were performed by means of χ2 or Fisher exact test, as appropriate. Mann-Whitney test was used to compare means between 2 continuous variables. Kruskal-Wallis test was used to compare means among more than 2 groups. P < .05 was considered significant in all statistical analyses.
Results
Table 1 provides the demographic data for our study sample. The number of survey respondents was 1,251 from 49 countries; the number of dentists answering different questions varied. Most participants (65.7%) were aged 31 through 50 years. Most participants practiced in Europe (37.8%) and Eastern Mediterranean (29.2%) regions; 19.7% practiced in North America and 13.3% practiced in the Western Pacific region. General dentists represented 63.9% of participants and 36.1% were specialists. Approximately two-thirds of participants (62.5%) worked in private practice and the remaining one-third (37.5) worked in public sectors. Most participants were employed full time (77.4%) and had more than 10 years of experience (63.5%).
Table 1.
Demographic characteristics of respondents.
| CHARACTERISTIC | NO. (%) |
|---|---|
| Age, y (n = 1,220) | |
| 23-30 | 224 (18.4) |
| 31-40 | 436 (35.7) |
| 41-50 | 366 (30.0) |
| 51-60 | 139 (11.4) |
| ≥ 60 | 55 (4.5) |
| Sex (n = 1,214) | |
| Male | 480 (39.5) |
| Female | 734 (60.5) |
| Region (n = 1,188) | |
| Eastern Mediterranean | 347 (29.2) |
| Europe | 449 (37.8) |
| North America | 234 (19.7) |
| Western Pacific | 158 (13.3) |
| Place of Practice (n = 1,216) | |
| Private practice | 760 (62.5) |
| Public services∗ | 456 (37.5) |
| Scope of Practice (n = 1,213) | |
| General dentist | 775 (63.9) |
| Specialist | 438 (36.1) |
| Employment Status (n = 1,206) | |
| Full time | 933 (77.4) |
| Part time | 273 (22.6) |
| Experience (n = 1,213) | |
| ≤ 1 year | 44 (3.6) |
| 2-5 years | 175 (14.4) |
| 6-10 years | 224 (18.5) |
| > 10 years | 770 (63.5) |
Public services refer to a practice in governmental health authorities, military, universities, organization affiliated, and not for profit.
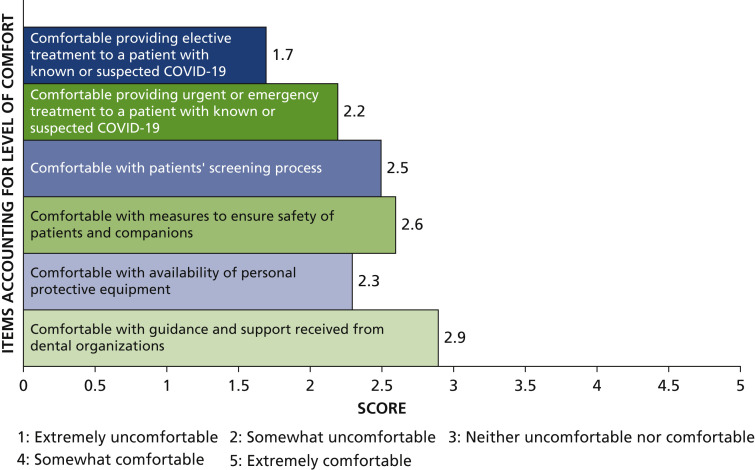
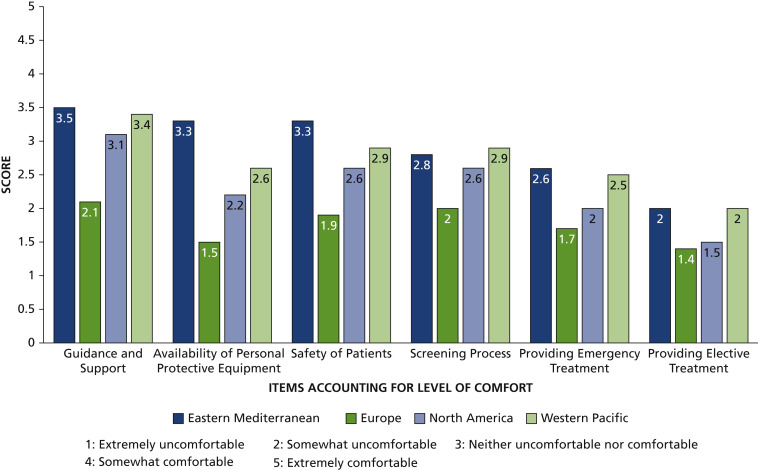
Figure 1 shows the level of comfort with preventive measures and provision of treatment among all respondents; the overall score was 14, which lies at the midpoint between “somewhat uncomfortable” and “neither comfortable nor uncomfortable.” Participants were least comfortable with providing elective treatment to a patient with known or suspected COVID-19 (mean score 1.7), and participants were “somewhat uncomfortable” with providing urgent treatment to such a patient (mean score 2.2). The mean score for guidance and support received from dental organizations was 2.9, which was closest to “neither uncomfortable nor comfortable,” and the score for availability of PPE was 2.3, which is near “somewhat uncomfortable.” On average, participants were between “somewhat uncomfortable” and “neither uncomfortable nor comfortable” when assessing available measures to ensure safety of patients and companions, and the screening process to detect potential COVID-19 cases at the workplace (2.6 and 2.5, respectively). Figure 2 illustrates the level of comfort with preventive measures and provision of treatment in the dental practice according to the geographic regions.
Figure 1.
Level of comfort with preventive measures and provision of treatment in the dental practice during the COVID-19 pandemic from a global perspective.
Figure 2.
Level of comfort with preventive measures and provision of treatment in the dental practice during the COVID-2019 pandemic based on geographic regions.
Approximately one-half of respondents were familiar with use of N95 or other high-level respirators (46.6%) and 92.3% of participants indicated that an N95 mask was necessary when attending to a patient with known or suspected COVID-19. However, only 20.5% used an N95 mask in practice, and 56.7% of the sample were aware of recommendations of extended versus limited use of the mask. When asked about attitudes toward delivery of care, 51.7% of respondents “strongly agreed” with the statement “prefer not to treat and would refer a known or suspected COVID-19 patient,” 22% “agreed,” 13% were “neutral,” and only 13.3% “disagreed” or “strongly disagreed.”
Most respondents (80.9%) indicated that their workplaces were closed as a result of the COVID-19 outbreak. Most of those who continued to work during the outbreak deferred elective treatment (76%) and were still able to function on an emergency basis (73.3%). Approximately three-quarters of dentists surveyed (73.6%) “strongly agreed” that there was a substantial financial impact on their income, and 15.4% “agreed” with this statement; 47.9% expected compensation, and 77% of those expected a public authority to provide compensation.
Analyses of data according to demographic characteristics
Table 2 provides the differences in respondents’ level of comfort with measures taken to prevent COVID-19 transmission and provision of care in the dental practice; there were statistically significant (P< .01) differences among dentists from different regions. There was no statistically significant difference between regions on necessity of N95 respirators, but there were statistically significant differences in regard to familiarity of use, actual use, and awareness of extended use versus limited use of N95 respirators (P < .01). There was no statistically significant difference in regard to the workplace’s perceived ability to function on an emergency basis. However, there were statistically significant differences on workplace closure and deferring elective dental treatment (P < .01). There were statistically significant differences in reporting substantial financial impact, expecting financial compensation, and preference for not treating and referring patients with known or suspected COVID-19 (P < .01).
Table 2.
Response based on geographic regions.
| GEOGRAPHIC REGION |
|||||
|---|---|---|---|---|---|
| VARIABLE | Eastern Mediterranean | Europe | North America | Western Pacific | P Value |
| Level of Comfort With Preventive Measures and Provision of Treatment in the Dental Practice, Mean Score on the Likert Scale (Standard Deviation) | |||||
| Guidance and support | 3.5 (1.4) | 2.1 (1.2) | 3.1 (1.3) | 3.4 (1.1) | < .01 |
| Availability of personal protective equipment | 3.3 (1.4) | 1.5 (0.9) | 2.2 (1.3) | 2.6 (1.2) | < .01 |
| Safety of patients | 3.3 (1.4) | 1.9 (1.1) | 2.6 (1.4) | 2.9 (1.2) | < .01 |
| Screening process | 2.8 (1.4) | 2.0 (1.2) | 2.6 (1.3) | 2.9 (1.3) | < .01 |
| Providing emergency treatment | 2.6 (1.4) | 1.7 (1.0) | 2.0 (1.2) | 2.5 (1.3) | < .01 |
| Providing elective treatment | 2.0 (1.3) | 1.4 (0.9) | 1.5 (1.0) | 2.0 (1.3) | < .01 |
| Total | 17.7 | 10.6 | 13.9 | 16.3 | < .01 |
| Understanding of Benefits and Use of N95 Respirators, Yes (No. [%]) | |||||
| Familiar with use of N95 | 218 (63.2) | 187 (41.6) | 158 (67.8) | 64 (40.5) | < .01 |
| Use of N95 in practice | 119 (34.4) | 37 (8.3) | 38 (16.4) | 40 (25.3) | < .01 |
| If N95 use is necessary for a patient with COVID-19 | 315 (91.3) | 408 (91.8) | 215 (93.1) | 149 (94.3) | .644 |
| Affect on Workplace, Yes (No. [%]) | |||||
| Workplace closed | 258 (74.8) | 398 (88.6) | 204 (87.6) | 97 (61.4) | < .01 |
| Workplace deferred elective treatment | 57 (65.5) | 47 (92.2) | 25 (86.2) | 45 (73.8) | < .01 |
| Workplace providing emergency treatment | 63 (72.4) | 36 (70.6) | 26(89.7) | 43 (70.5) | .216 |
| Financial Impact | |||||
| Substantial financial impact on respondent, mean score on the Likert Scale (standard deviation) | 4.3 (1.00) | 4.7 (0.7) | 4.8 (0.6) | 4.4 (0.9) | < .01 |
| Expecting financial compensation, yes (no. [%]) | 373 (49.8) | 193 (44.8) | 120 (36.9) | 229 (51.6) | < .01 |
Dentists working in privately owned practices were less comfortable with preventive measures and provision of treatment than dentists working in public sectors (P < .01) (Table 3 ). Place of practice did not influence the need to use N95 respirators for a patient with known or suspected COVID-19; however, dentists in private practice were less familiar with N95 respirators, used them less often, and were less aware of their extended versus limited use (P < .01). Place of practice did not influence the provision of emergency treatment. However, there were statistically significant differences in regard to workplace closure and defering elective dental treatment (P < .01). There were statistically significant differences in reporting substantial financial impact (P < .01), expecting financial compensation (P < .01), and preference for not treating and referring patients with known or suspected COVID-19 (P < .01).
Table 3.
Response according to place of practice and scope of practice.
| PLACE OF PRACTICE |
SCOPE OF PRACTICE |
|||||
|---|---|---|---|---|---|---|
| VARIABLE | Private | Public∗ | P Value | General Dental Practitioner | Specialist | P Value |
| Level of Comfort With Preventive Measures and Provision of Treatment in the Dental Practice, Mean Score on the Likert Scale (Standard Deviation) | ||||||
| Guidance and support | 2.1 (1.2) | 3.3 (1.3) | < .01 | 2.6 (1.4) | 3.3 (1.4) | < .01 |
| Availability of personal protective equipment | 1.5 (0.9) | 2.8 (1.4) | < .01 | 2.0 (1.3) | 2.8 (1.4) | < .01 |
| Safety of patients | 1.9 (1.1) | 3.0 (1.4) | < .01 | 2.3 (1.3) | 3.0 (1.4) | < .01 |
| Screening process | 2.0 (1.2) | 2.8 (1.4) | < .01 | 2.3 (1.3) | 2.8 (1.3) | < .01 |
| Providing emergency treatment | 1.7 (1.0) | 2.4 (1.3) | < .01 | 1.9 (1.2) | 2.6 (1.3) | < .01 |
| Providing elective treatment | 1.4 (0.9) | 1.8 (1.2) | < .01 | 1.6 (1.1) | 1.9 (1.6) | < .01 |
| Total | 10.6 | 16.1 | < .01 | 12.7 | 16.4 | < .01 |
| Understanding of Benefits and Use of N95 Respirators, Yes (No. [%]) | ||||||
| Familiar with the use of N95 | 187 (41.6) | 440 (59.8) | < .01 | 363 (47) | 281 (64.4) | < .01 |
| Use of N95 in practice | 37 (8.3) | 197 (26.8) | < .01 | 110 (14.2) | 136 (31.2) | < .01 |
| If N95 use is necessary for a patient with COVID-19 | 408 (91.9) | 679 (92.5) | .391 | 701 (91.5) | 409 (93.8) | .391 |
| Affect on Workplace, Yes (No. [%]) | ||||||
| Workplace closed | 398 (88.6) | 559 (76) | < .01 | 643 (83.3) | 335 (76.7) | < .01 |
| Workplace defered elective treatment | 47 (92.2) | 127 (71.8) | < .01 | 101 (78.3) | 76 (73.8) | .258 |
| Workplace providing emergency treatment | 36 (70.6) | 132 (74.6) | .344 | 88 (68.2) | 83 (80.6) | < .05 |
| Financial Impact | ||||||
| Substantial financial impact on respondent, mean score on the Likert Scale (standard deviation) | 4.7 (0.7) | 4.5 (0.9) | < .01 | 4.7 (0.7) | 4.4 (1.0) | < .01 |
| Expecting financial compensation, yes (no. [%]) | 229 (51.6) | 324 (45.4) | < .05 | 389 (51.4) | 176 (41.7) | < .01 |
Public refer to a practice in governmental health authorities, military, universities, organization affiliated, and not for profit.
General dentists were less comfortable with preventive measures and provision of treatment than specialist dentists (P < .01) (Table 3). There was no statistically significant difference between the responses of general dental practitioners and specialists on deferring elective dental treatment, and no statistically significant difference on the necessity for N95 respirators when attending to a patient with known or suspected COVID-19. However, specialists were more familiar with their use, used them more, and were more aware of their extended versus limited use (P < .01). More general dental practitioners reported workplace closure (P < .01), and more specialists reported providing emergency dental treatment (P < .05). There were statistically significant differences in reporting substantial financial impact (P < .01), expecting financial compensation (P < .01), and preference for not treating and referring patients with known or suspected COVID-19 (P < .01). When experience in practice was examined, experienced dentists were more familiar with the use of N95 respirators (P < .05), more reported workplace closure than junior dental practitioners (P < .05). They continued to work during the outbreak and were able to function on an emergency basis compared with junior dentists (P < .05).
Discussion
COVID-19 is a global pandemic affecting more than 195 countries and territories.8 It is unknown whether this outbreak will be contained without recurring or will be a recurring epidemic.9 Health care professionals, including dentists, should be better prepared to deal with the challenges that the pandemic and similar future occurrences pose. In our cross-sectional study, we provide insight into the dentists’ knowledge about preventing the spread of COVID-19 in the dental practice, their attitudes and professional behavior toward treating patients with confirmed or suspected cases, and the affect the outbreak has on their practices and livelihoods.
The respondents’ levels of comfort with relevant knowledge of COVID-19 and available measures to prevent the spread of disease in dental practice was low and similar to that for providing elective or emergency treatment to a patient with confirmed or suspected COVID-19, understandably more so with the former. These findings could be attributed to the novelty of the disease, with published reports on human-to-human transmission in the community and evidence that SARS-CoV-2 transmission through respiratory aspirates, aerosols, and saliva mucous contact is highly likely.10 , 11 In addition, dentists are facing a new reality, with more new guidance for patient screening, new sets of PPE, modifying diagnostic and treatment protocols, restricting practice to urgent oral health care, and doing teleconsultations.2 , 3 , 5 , 12 Reports of dentists dying of COVID-19 might have introduced stress and anxiety among the professional community.13 , 14 These findings are in concordance with those from a study on Jordanian dentists in which researchers reported limited comprehension of the extra precautionary measures to protect patients and staff during the pandemic.15
On PPE, the survey investigated N95 and high-level respirators because of the concerns raised about aerosol-generating procedures in dentistry and the higher risk of spreading the disease. Although there was overwhelming agreement about the necessity of N95 masks among respondents, familiarity with their use varied considerably, with dentists in North America most accustomed to them. However, their availability to dentists in North America and Europe was lower than to dentists in the other regions we investigated. In a systematic review in which Verbeek and colleagues16 evaluated the types of PPE most effective for reducing contamination and infection, none of the included studies referred to measures in a dental operatory. Before the COVID-19 pandemic, N95 masks and similar respirators were uncommon in dentistry17; their use requires fit-testing to ensure proper seal around the nose and mouth and a full face shield, and they are not readily available to dentists when needed because of their high demand for frontline health care providers. Therefore, the findings from our study about dentists’ understanding of the benefits of such masks and how they are used, and their preferences to refer rather than treat patients with known or suspected COVID-19 were not surprising. Oral health care providers are unprepared when faced with a highly infectious disease that is transmissible through respiratory droplets and contact routes.18
The differences between regions reflect the timeline in regional outbreaks and the speed with which countries responded to COVID-19. Some countries were better prepared because they had experienced virus outbreaks in the past, such as severe acute respiratory syndrome in South East Asia and the Western Pacific region in 200319 , 20 and Middle East respiratory syndrome in the Eastern Mediterranean region in 2012.21 , 22 The outbreak of the disease in Italy alerted health authorities in the West to the seriousness of the disease, leading to immediate suspension of elective dental treatment and confining treatment to emergency care,2 , 3 , 12 , 23 with a subsequent financial impact on dentists.24 This is in agreement with a study from the Irish Dental Association in which investigators reported an estimated financial loss of more than 70% amid the COVID-19 outbreak.25 Similarly, the British Dental Association indicated that dental practices in the United Kingdom were facing substantial losses due to the suspension of routine oral health care.26 In the United States, some of the measures that practice owners were taking to ensure the sustainability of their practices were revealed through the American Dental Association’s Health Policy Institute’s polling from the second week of the shutdown.27 There is uncertainty about when the full scope of oral health care will be resumed and governments of developed and wealthy countries are offering stimulus packages to small and medium-sized business, including dental practices. The situation remains unclear for practices elsewhere.24
The limitations to our study influence interpretation. The survey was randomly distributed as an online link through e-mail, WhatsApp, and social media. Therefore, country representations in the samples varied, although the number of respondents was sufficiently high to provide statistical power. The exponential increase in COVID-19 cases in different countries throughout the period of the survey and the frequency with which guidance and recommendations were published might have contributed to different responses from the same country and region. Practitioners might not be comfortable replying to questions that would put them in an unfavorable position, in spite of assurances of anonymity, which probably introduced bias. Some questions were ambiguous and created overlapping categories. A piloted, limited sample survey before distribution was not conducted to identify these questions.
Conclusions
Researchers believe that dental professionals can play an important role in preventing the transmission of COVID-19. Infection control guidance adopted in dentistry was last provided during the HIV and AIDS pandemic, and the same guidance might have obviated the spread of the last serious respiratory epidemic (severe acute respiratory syndrome in 2003) in dental settings. In addition, the latter had a low degree of viral shedding in the prodromal phase.20 Our findings revealed a concerning lack of preparedness in the dental community to confront a highly infectious respiratory disease that is spread through aerosols, droplets, and contact routes, despite previous warning.20 , 28 As SARS-CoV-2 shedding occurs in various stages of the disease, including the presymptomatic phase and in patients who are asymptomatic,29 the ADA’s Interim Mask and Face Shield Guidance require the use of the highest-level respirators when treating all patients with the assumption that they all can transmit the disease.30 , 31 This is a wakeup call to educators and professional regulators who are on the frontlines, including the newest ADA specialty, dental anesthesiologists, who provide care directly in the airway and respiratory system, to better prepare dentists on a new level of protective measures in the dental setup to face this outbreak and similar diseases in the future and to enhance the role of teledentistry. We would argue about redefining the role of dental public health specialists to promote public health in this crisis. In addition, dentists need to address the ability of their practices to survive crises that impose restrictions on services for a considerable period.
Biographies
Dr. Bakaeen is a prosthodontist in private practice, Amman, Jordan.
Dr. Masri is a professor, the division director, and the prosthodontics director, School of Dentistry, University of Maryland, Baltimore, MD.
Dr. AlTarawneh is an associate professor of prosthodontics, University of Jordan, Amman, Jordan; and a visiting clinical associate professor, College of Dentistry, University of Illinois at Chicago, Chicago, IL.
Dr. Garcia is a dean and professor of prosthodontics, School of Dental Medicine, University of Nevada, Las Vegas, Nevada.
Dr. AlHadidi is an assistant professor of oral and maxillofacial radiology, School of Dentistry, University of Jordan, Amman, Jordan.
Dr. Khamis is a professor of biostatistics, Hamdan Bin Mohammed College of Dental Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates.
Dr. Hamdan is the dean and a professor of orthodontics, School of Dentistry, University of Jordan, Amman, Jordan.
Dr. Baqain is the dean and a professor of oral and maxillofacial surgery, Hamdan Bin Mohammed College of Dental Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates; and a professor of oral and maxillofacial surgery, School of Dentistry, University of Jordan, Amman, Jordan.
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
Footnotes
Disclosure. None of the authors reported any disclosures.
The authors would like to acknowledge the assistance of Professor Bruce Dunoff, former dean of Harvard School of Dental Medicine; their respected colleagues for insightful suggestions; and leaders of professional societies for recruiting participants for our study.
Supplemental data related to this article can be found at https://doi.org/10.1016/j.adaj.2020.09.022.
Supplemental Data
References
- 1.World Health Organization https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen Rolling updates on coronavirus disease (COVID-19), Available at:
- 2.American Dental Association What consititutes a dental emergency? https://success.ada.org/∼/media/CPS/Files/Open%20Files/ADA_COVID19_Dental_Emergency_DDS.pdf?utm_source=adaorg&utm_medium=covid-resources-lp&utm_content=cv-pm-emerg-def&utm_campaign=covid-19&_ga=2.32369854.1290463808.1584935488-268976772.1584935488 Available at:
- 3.NHS Issue 3. Preparedness letter for primary dental care. Available at: https://www.england.nhs.uk/coronavirus/publication/preparedness-letters-for-dental-care. Accessed April 8, 2020.
- 4.World Health Organization Clinical Management of Severe Acute Respiratory Infection (SARI). When COVID-19 Disease Is Suspected: Interim Guidance. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected Available at:
- 5.Centers for Disease Control and Prevention CDC Guidance for Providing Dental Care During COVID-19. https://www.cdc.gov/oralhealth/infectioncontrol/statement-COVID.html Available at:
- 6.ADA Center for Professional Success COVID-19 frequently asked questions. American Dental Association. https://success.ada.org/en/practice-management/patients/coronavirus-frequently-asked-questions Available at:
- 7.Molinari J.A. Dental infection control at the year 2000: accomplishment recognized. JADA. 1999;130(9):1291–1298. doi: 10.14219/jada.archive.1999.0399. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19), World Map. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/world-map.html Available at:
- 9.Weston S., Frieman M.B. COVID-19: knowns, unknowns, and questions. mSphere. 2020;5(2) doi: 10.1128/mSphere.00203-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92(6):568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan J.F.-W., Yuan S., Kok K.-H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Dental Association Summary of ADA Guidance During the COVID-19 Crisis. https://www.ada.org/en/member-center/coronavirus-resource-toolkit-for-ada-members?utm_source=adaorg&utm_medium=vanityurl&utm_content=covid19resources&utm_campaign=covid-19 Available at:
- 13.Izzetti R., Nisi M., Gabriele M., Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J Dent Res. 2020;99(9):1030–1038. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 14.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khader Y., Al Nsour M., Al-Batayneh O.B. Dentists' awareness, perception, and attitude regarding COVID-19 and infection control: cross-sectional study among Jordanian dentists. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verbeek J.H., Rajamaki B., Ijaz S. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020 Apr 15;4(4):CD011621. doi: 10.1002/14651858.CD011621.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coulthard P. Dentistry and coronavirus (COVID-19): moral decision-making. Br Dent J. 2020;228(7):503–505. doi: 10.1038/s41415-020-1482-1. [DOI] [PubMed] [Google Scholar]
- 18.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Fact sheet: basic information about SARS. https://www.cdc.gov/sars/about/fs-SARS.pdf Available at: Published January 13, 2004. Accessed April 16, 2020.
- 20.Samaranayake L.P., Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. JADA. 2004;135(9):1292–1302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sukumaran A., Patil S. The MERS-CoV outbreak: challenges facing the dental profession. J Contemp Dent Pract. 2014;15(2):i–ii. [PubMed] [Google Scholar]
- 22.Aldohyan M., Al-Rawashdeh N., Sakr F.M., Rahman S., Alfarhan A.I., Salam M. The perceived effectiveness of MERS-CoV educational programs and knowledge transfer among primary healthcare workers: a cross-sectional survey. BMC Infect Dis. 2019;19(1):273. doi: 10.1186/s12879-019-3898-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): guidance for dental settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html Available at: Accessed October 5, 2020.
- 24.Farooq I., Ali S. COVID-19 outbreak and its monetary implications for dental practices, hospitals and healthcare workers [letter] Postgrad Med J. 2020 Apr 3 doi: 10.1136/postgradmedj-2020-137781. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irish Dental Association Irish Dental Association warns that dental profession on the brink of collapse. https://www.dentist.ie/latest-news/irish-dental-association-warns-that-dental-profession-on-the-brink-of-collapse.8336.html Available at: Published March 20, 2020. Accessed October 5, 2020.
- 26.British Dental Association Live updates: coronavirus and dentistry. https://bda.org/advice/Coronavirus/Pages/latest-updates.aspx Available at:
- 27.Carey M. Second week of HPI polling shows dentists’ response to COVID-19. ADA News. https://bda.org/advice/Coronavirus/Pages/financial-impact.aspx Available at:
- 28.Harrel S.K., Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. JADA. 2004;135(4):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim E.S., Chin B.S., Kang C.K. Korea National Committee for Clinical Management of COVID-19. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean Cohort Study on COVID-19. J Korean Med Sci. 2020;35(13):e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Dental Association Interim mask and face shield guidance. https://success.ada.org/∼/media/CPS/Files/COVID/ADA_Interim_Mask_and_Face_Shield_Guidelines.pdf Available at:
- 31.Centers for Disease Control and Prevention Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). CDC Stacks. https://stacks.cdc.gov/view/cdc/88624 Available at: Updated June 20, 2020. Accessed October 5, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.