Abstract
Objective
To assess bone thickness augmentation and implant survival in ridges with horizontal atrophy managed through split crest technique with concomitant installation of dental implants.
Materials and Methods
Thirteen patients with maxillary bone atrophy underwent surgery and had their bone thickness assessed through cone beam computed tomography 6 months pre- and postoperatively. Comparative measurements of initial and final bone height and thickness were taken using Dolphin Imaging® 11.5 software. The distance between the nasal fossa floor or the maxillary sinus and the alveolar crest determined the bone height, while the measurement of bone thickness took into account the distance between the vestibular cortical bone and the palatal cortical bone at the crest level, and at 5 mm and 10 mm from it.
Results
The bone height loss of 0.68 mm was statistically significant (p = 0.01). The average horizontal bone gain was 3.45 mm at ridge level, 3.03 mm at 5 mm from it and 2.42 mm at 10 mm from it. The mean horizontal gain for the three regions was 2.97 mm, and the values were statistically significant for all three regions assessed (p < 0.01). No complications were associated with the surgical procedures, and 23 implants were installed following the surgical expansion. No implants were lost (100% survival).
Conclusion
The split crest technique proved to be viable and predictable, enabling a significant increase in ridge thickness and a high percentage of implant survival.
Keywords: Dental implants, Rehabilitation, Alveolar ridge augmentation
Introduction
The function of the alveolar process is to support teeth, and loss of that function leads to a gradual, chronic and cumulative resorption in the region. That physiological process of bone resorption whether spontaneous or, more commonly, associated with traumas, pathologies and traumatic dental extractions constantly results in bone defects that represent a real difficulty for the installation of dental implants [1].
The horizontal defects of the alveolar ridge hinder implant-supported rehabilitation due to the lack of sufficient bone volume to support the dimensions of the implants, thus affecting the final prosthetic result, from both a functional and an esthetic point of view [2].
The gold standard for the treatment of atrophic horizontal ridges is still the use of autologous bone grafts harvested from intra- or extraoral donor areas of the subject and used in the form of blocks or particulates. Although those treatment modalities have high success rates and low rates of complications described in the literature, the complaint of morbidity related to the removal of the graft of a second surgical area of the patient has motivated the search for alternative techniques.
In that regard, the technique of surgical expansion of the alveolar ridge, also known as the split crest technique, consists of horizontal and vertical osteotomies intended to separate vestibular and lingual/palatal bone cortices, creating a space for the simultaneous installation of implants and introduction of biomaterials [3]. The main advantages of such technique are the fact that it allows the installation of implants in the same surgery, decreasing the number of surgical procedures and the time of treatment for the patients; and especially the fact that it does not need a donor area to remove grafts, which reduces the morbidity and the complication rate for the patients [4].
The split crest technique, in addition to the fact that it does not require a donor area to remove the graft, makes it possible to install dental implants in the same operative procedure, decreasing morbidity, treatment time, number of surgical procedures and even the risk of complications to the patients, and it is therefore more easily accepted by them [5].
Given the above, the purpose of this study was to assess the increase in bone thickness and survival of implants in the ridges of patients who had horizontal atrophy and were treated using the split crest technique with simultaneous installation of dental implants.
Materials and Methods
Patient Population
A total of 13 patients (10 women and 3 men), with an average age of 44.2 years (ranging from 28 to 56), seeking treatment for the installation of dental implants were included in the sample, and after clinical and tomographic assessment (CBCT) (Picasso Trio CBCT unit—Vatech, Hwaseong, Republic of Korea—80 kvp, 3.7 mA, scanning time of 24 s and voxel size of 0.2 mm—FOV 80 × 80 mm), they were diagnosed with horizontal atrophy in the anterior maxillary region (region of incisors, canines and/or premolars), with linear remaining ridge, no large concavities and requiring bone grafting for adequacy (Table 1). Cases with bone thicknesses of 2.5–3.5 mm and heights of 12 mm or more were included in the sample. All the patients had their bone atrophies treated through the split crest technique with simultaneous installation of dental implants. In all cases, the gaps between osteotomized segments were filled with bovine biomaterial.
Table 1.
Sample characteristics
| Patient | Age | Gender | Missing teeth |
|---|---|---|---|
| 1 | 34 | M | 12, 11, 21, 22 |
| 2 | 29 | F | 22 |
| 3 | 44 | F | 11, 12 |
| 4 | 52 | F | 12, 11, 21, 22 |
| 5 | 28 | F | 22 |
| 6 | 38 | M | 14, 15 |
| 7 | 28 | F | 22 |
| 7 | 46 | F | 13, 14 |
| 9 | 56 | F | 11,12,21,23 |
| 10 | 51 | F | 11,12,21,22 |
| 11 | 55 | F | 13, 14, 15 |
| 12 | 48 | F | 11,12,21,22 |
| 13 | 56 | M | 11,12,21,22 |
| Mean | 44.2 |
All surgical procedures were performed by two surgeons according to a standardized surgical technique. The study protocol was explained to each subject, and each one of them signed an informed consent form.
Patients with health conditions that contraindicated the surgical procedures; patients with bone defects other than the horizontal ones; patients with a horizontal defect in a region other than the anterior region of the maxilla; patients with a horizontal defect in the anterior region of the maxilla, but without enough bone thickness to perform the split crest technique; patients in whom it was not possible to install the implant simultaneously with the split crest technique; and those who did not return for control assessments/examinations and/or who abandoned treatment were excluded from the sample.
Surgical Procedure
All patients were given oral, steroidal anti-inflammatory (dexamethasone 4 mg—Hypofarma, Ribeirão da Neves—Brazil) and antibiotic (amoxicillin 1 g—Ranbaxy, Arsenal—Brazil) drugs one hour before the procedure.
The surgical procedure was initiated with an anesthetic infiltration with 2% lidocaine solution with vasoconstrictor 1:100.000 (DFL, Rio de Janeiro—Brazil), followed by an incision with scalpel blade number 15 (Solidor, Osasco—Brazil) in the alveolar ridge of the anterior region of the maxilla, associated with two relaxing incisions. A careful mucoperiosteal detachment of the incised area was performed, and horizontal and vertical osteotomies were made in order to allow the separation of the bone cortices (Figs. 1 and 2).
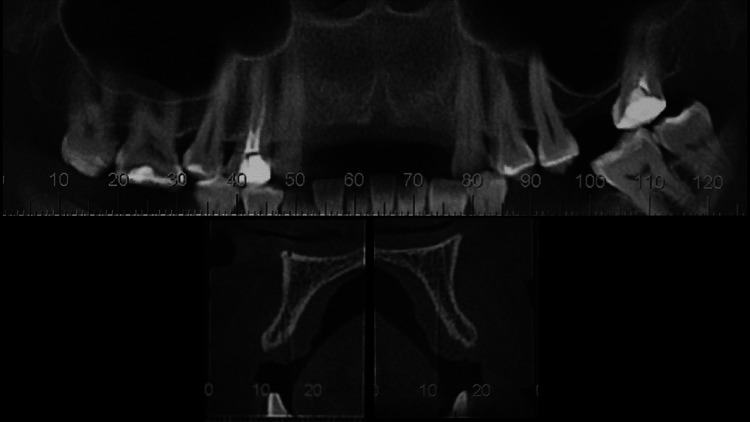
Fig. 1.
CBCT showing dental absences in the anterior region of the maxilla. Notice the presence of a bone thickness around 3 mm in the tomographic sections, as well as the presence of bone marrow structure between the vestibular and palatal cortices
Fig. 2.
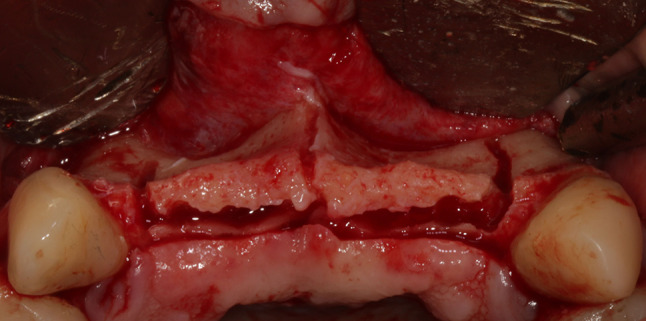
After mucoperiosteal incision and detachment, horizontal and vertical osteotomies were performed in order to facilitate the bone expansion process. All osteotomies were performed with a 701 tronco-conical drill (Jet, Rio de Janeiro—Brazil) coupled to a straight hand piece (KaVo, Ribeirão Preto—Brazil) at a velocity of 15.000 rpm under intense irrigation with physiological serum
Following the surgical procedure, the rotary expander kit (Supremo, São Paulo—Brazil) was used sequentially (from the smallest to the largest caliber), according to manufacturer’s recommendations, until sufficient bone expansion was achieved for the installation of the planned dental implants (Figs. 3, 4, 5 and 6).
Fig. 3.

Rotary expander kit. Notice that the kit starts with a spear cutter and has expanders of different calibers. Expanders should be used in sequence up to a caliber close to the diameter of the implant to be installed
Fig. 4.

Separation of bone cortices through the use of expanders. Note that, as they are used, a gap is created between the bone plates
Fig. 5.
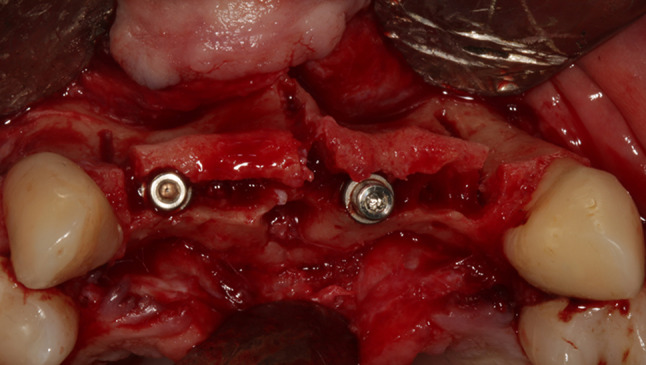
Dental implants installed (Due cone 3.5 × 9, Implacil de Bortoli, São Paulo—Brazil) after expansion of bone cortices. In this case, implants were installed in the region of dental elements 12 and 21. Note the gap between the bone cortices
Fig. 6.
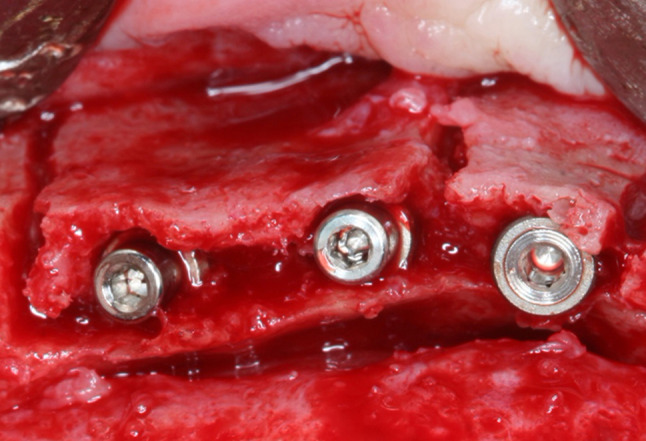
Implants (Due cone 3.5 × 9, Implacil de Bortoli, São Paulo—Brazil) installed in the premolar region in the positions of teeth 13, 14 and 15
All the gaps and areas of implant thread exposure were then filled with biomaterial of bovine origin (Lumina-Porous, Critéria, São Carlos—Brazil) and covered with a collagen membrane (Lumina–Coat Double Time, Critéria, São Carlos—Brazil) in order to homogenize all the reconstruction (Fig. 7). Suture with a Vicryl 4-0-type absorbable wire (Ethicon, Rio de Janeiro—Brazil) was carried out in the intraoral incisions to obtain closure by first intent.
Fig. 7.
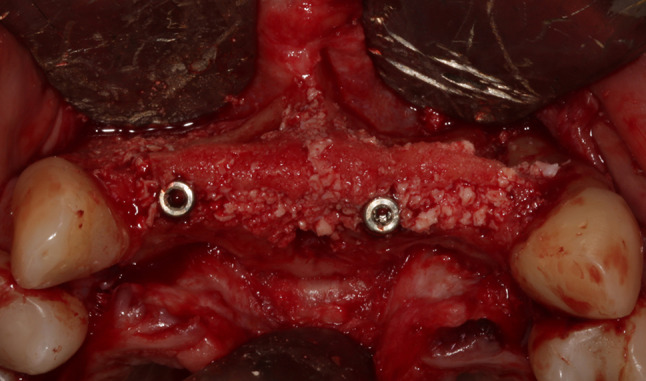
Clinical aspect after filling the gaps with biomaterials. Notice the reconstruction homogeneity
All patients were treated with nonsteroidal anti-inflammatory (nimesulide 100 mg Q12H for 3 days—Aché, Guarulhos—Brazil) and analgesic (dipyrone monohydrate 1 g Q6H for 3 days—Sanofi-Aventis, Suzano—Brazil) drugs in the postoperative period, and also received instructions to follow.
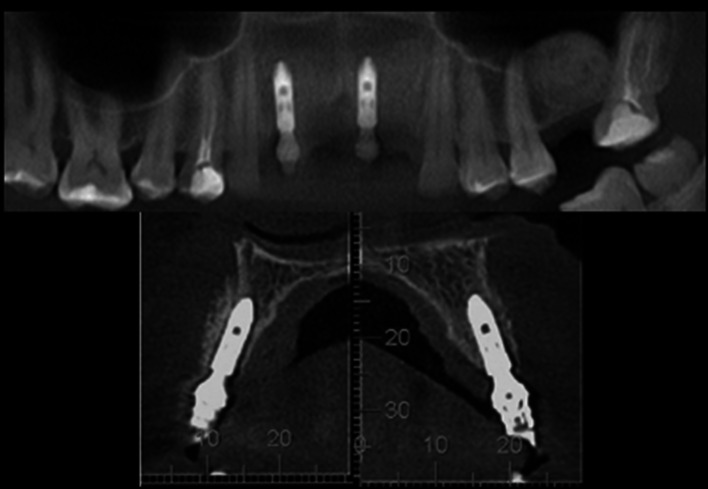
Six months after placing the implants, the patients were submitted to a new CBCT and a reopening surgery for the installation of healers (second surgical phase); then, they were referred to the prosthetist for prosthetic rehabilitation over the implants (Figs. 8, 9 and 10).
Fig. 8.

Abutments installed in the surgical second stage (Neodent, Curitiba—Brazil). Note the excellent scar tissue results in the soft tissues surrounding the implants
Fig. 9.
CBCT showing a considerable increase in alveolar thickness, as well as an adequate positioning of dental implants
Fig. 10.

Metal–ceramic fixed prosthesis involving upper incisors. Note the excellent results achieved
Evaluation Method
CBCT was used to assess the increase in bone thickness of patients who were treated using the split crest technique with simultaneous installation of dental implants. This imaging examination was conducted before the procedure and within 6 months postoperatively.
The measurements were taken by a single examiner, using Dolphin Imaging® 11.5 software (Dolphin Imaging and Management Solutions, Chatsworth—USA), according to the following parameters:
Bone height (Fig. 11A):
Fig. 11.
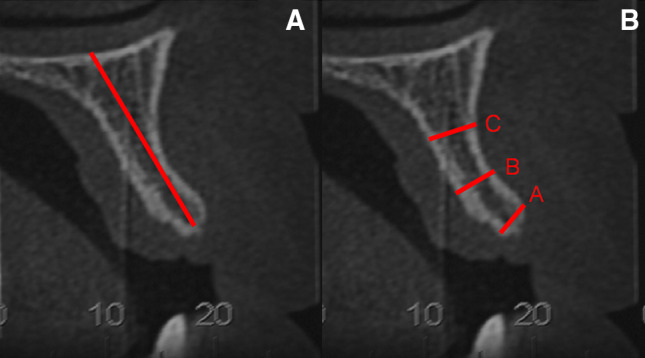
A Bone height measurement taken at the center of the alveolar bone crest. From a fixed point of the floor of the nasal fossa to the region of the ridge crest. B Bone thickness measurement taken at the level of the alveolar bone crest, and at 5 and 10 mm from it
Distance between the nasal fossa floor or maxillary sinus and the alveolar bone crest.
Bone thickness (Fig. 11B):
A—Distance between the vestibular cortical and palatal cortical bones in the alveolar bone crest.
B—Distance between the vestibular cortical and palatal cortical bones at 5 mm from the alveolar bone crest.
C—Distance between the vestibular cortical and palatal cortical bones at 10 mm from the alveolar bone crest.
Those measurements were repeated for each patient according to each sampling period.
Statistical Analysis
A descriptive and comparative analysis was performed using the computer software Statistical Package for Social Sciences, version 18.0 (SPSS Inc., Chicago, IL, USA). The sample presented a normal distribution (Shapiro–Wilk test) and homogeneity of variances (Levene’s test), so parametric tests were used. The paired t test was used to compare bone width values. As bone height, initial and final height measures did not show homogeneity of variances, nonparametric tests were used. Wilcoxon’s test was used to assess height loss.
Results
Measurement showed that patients had an average bone height of 18.27 mm in the preoperative period, whereas in the postoperative period, that average height decreased to 17.59 mm, thus showing a vertical loss of 0.68 mm, which was statistically significant (p = 0.01) (Table 2).
Table 2.
Results of the statistical analysis to assess bone height loss through Wilcoxon’s test
| Hight | N | Mean | Standard deviation | p = |
|---|---|---|---|---|
| Initial | 13 | 18.27 | 3.15569 | 0.01 |
| Final | 13 | 17.59 | 3.00803 |
In regard to bone thickness, it was 2.92 mm in the crest, 4.35 mm at 5 mm from the crest and 5.74 mm at 10 mm from the crest, preoperatively. For the 6-month postoperative period, those values increased to 6.37 mm in the crest, 7.38 mm at 5 mm from the crest and 8.61 mm at 10 mm from the crest, and those results are statistically significant in the three regions assessed—p < 0.01 (Table 3). The thickness gain was 2.97 mm when the average of the three regions assessed in the pre- and postoperative periods was considered.
Table 3.
Comparative assessment of bone thickness measurements before and after conduction of the split crest technique according to each region assessed—paired t test
| Mean | N | Standard deviation | p | |
|---|---|---|---|---|
| Crest—initial thickness | 2.9223 | 13 | 0.34162 | < 0.01 |
| Crest—final thickness | 6.3700 | 13 | 0.66371 | |
| 5 mm from the crest—initial thickness | 4.3592 | 13 | 0.61002 | < 0.01 |
| 5 mm from the crest—final thickness | 7.3846 | 13 | 0.61256 | |
| 10 mm from the crest—initial thickness | 5.7485 | 13 | 0.85767 | < 0.01 |
| 10 mm from the crest—final thickness | 8.6192 | 13 | 0.69313 |
No complications with split crest surgeries were observed. A total of 23 implants were installed in 13 patients of the sample, amounting to an average of 1.7 implants per subject. Morse Cone connection was used in all cases. Most implants used were 3.5 × 9 mm in diameter and height (12 of 23 sample implants), followed by 3.5 × 11 mm implants (6 implants). The average follow-up time of patients after conduction of the split crest technique was 18.3 months, with the shortest follow-up time of 7 months and the longest follow-up time of 36 months. No implants were lost during the assessment period, corresponding to 100% survival (Table 4).
Table 4.
Complications of split crest technique, characteristics of the implants installed and follow-up of patients
| Patient | Split crest complications | No. of implants | Lost implants | Connection | Implant diameters and lengths | Follow-up (months) |
|---|---|---|---|---|---|---|
| 1 | No | 2 | 0 | CM |
1—3.5 × 11 mm 2—3.5 × 11 mm |
36 |
| 2 | No | 1 | 0 | CM | 3.5 × 11 mm | 18 |
| 3 | No | 2 | 0 | CM |
1—3.5 × 11 mm 2—3.5 × 11 mm |
30 |
| 4 | No | 2 | 0 | CM |
1—3.5 × 11 mm 2—4.0 × 9 mm |
24 |
| 5 | No | 1 | 0 | CM | 4.0 × 11 mm | 12 |
| 6 | No | 2 | 0 | CM |
1—4.0 × 11 mm 2—4.0 × 11 mm |
35 |
| 7 | No | 1 | 0 | CM | 3.5 × 9.5 mm | 30 |
| 8 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
12 |
| 9 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
12 |
| 10 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
7 |
| 11 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
7 |
| 12 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
7 |
| 13 | No | 2 | 0 | CM |
1—3.5 × 9 mm 2—3.5 × 9 mm |
7 |
| Total: 23 | Total: 0 | Average: 18.3 |
Discussion
Several surgical materials and techniques have been developed and are widely used in implantology for the reconstruction of areas with bone atrophy. In that regard, the readjustment of the alveolar ridge for the installation of dental implants can be performed through the use of autogenous, heterogenous, allogenic or synthetic grafts or growth factors, and they may be used either in particulate form or in blocks [6].
The use of autogenous grafts is still considered the gold standard in the literature due to its considerable osteogenic, osteoinductive and osteoconductive potential. However, the need for a second surgical site as donor area, the longer operative time and even the need for a hospital environment in cases of use of the extraoral donor regions make such modality of treatment result in greater morbidity and risks of complications to the patients, thereby making it more difficult for them to accept.
The split crest technique is recommended for the treatment of horizontal bone defects that present a remnant thickness of around 3.0 mm, as the bone marrow is more flexible and vascularized, much easier to expand, with less tendency to fracture and easier revascularization in the postoperative period [7]. Cases with remnants smaller than 3.0 mm tend to be highly corticalized and have little or no bone marrow structure, making it difficult to expand and facilitating fracture, so it is preferable to using autogenous block grafts or autogenous particulate grafts graft associated with titanium mesh techniques and the like.
According to the literature, the survival rate of implants installed in sites where the split crest technique was conducted varies from 93 to 100% [8, 9], which supports the results of this study, where a total of 23 implants were installed and a survival rate of 100% was found in the follow-up (average of 18.3 months postoperatively).
The average bone height loss in the alveolar ridge was 0.68 mm at the six-month postoperative assessment, which was not significant from the clinical point of view, but statistically significant according to the statistical analysis. The authors found no other work in the literature in which the measurement of height loss has been taken, which makes this work quite unusual.
Such bone loss might be mainly attributed to the surgical technique employed by using drills and not to peri-implant bone remodeling, since the implants were still not loaded at the time of measurement. Loss of height may also have occurred due to the small quantity of bone in the ridge or a very thin bone which would be more prone to necrosis. One way to minimize such bone loss caused by the surgical technique may be to use oscillatory instruments (ultrasound). Waechter et al. (2017), however, in a systematic review and meta-analysis study, showed that the results obtained with the use of drills or the use of ultrasound for making the osteotomies hardly vary [10, 11].
The average bone thickness gain was 2.97 mm, and it is statistically significant in all regions assessed (crest, and 5 and 10 mm from the crest). According to Waechter et al. (2017), any increase in bone thickness can be considered as success of the technique. According to those authors, the average thickness increase is 3.80 mm when the measurement is taken at the crest of the ridge [11]. That result was higher than the one obtained in this study. However, in our study it was standardized to assess not only the thickness of the ridge crest but also the thickness at 5 and 10 mm from it, which, in our opinion, makes these results more complete and reliable.
Complication rates associated with the procedure are low. The main complication found in the literature is the fracture of the vestibular bone plate. According to Shibuya et al. (2014), the undesirable fracture of the vestibular segment most commonly occurs in the mandible and does not prevent the procedure, since fastening by means of screws may be performed and the implants may be installed as initially planned [12]. No complication has been observed in this study, which supports the results of low complication rate associated with this technique when appropriately indicated.
Conclusion
The split crest technique proved to be feasible and predictable, providing a significant increase in the thickness of the ridge, absence of complications, high percentage of implant survival and reduction in time and morbidity caused by the treatment.
Funding
No funding received.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the research ethics committee of the Piracicaba School of Dentistry—Unicamp (Protocol Number is 93082218.1.0000.5418).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Carolina Santos Ventura de Souza, Email: carolina.ventura@outlook.com.br.
Bruno Costa Martins de Sá, Email: brunosa01@gmail.com.
Douglas Goulart, Email: douglasrgoulart@gmail.com.
Gabriel Albuquerque Guillen, Email: guillen.spee@gmail.com.
Felipe Germóglio C. Macêdo, Email: felipegermogliobmf@gmail.com
Claudio Ferreira Nóia, Email: claudion@unicamp.br.
References
- 1.Nóia CF, Ortega-Lopes R, Kluppel LE, De Sá BCM. Sandwich osteotomies to treat vertical defects of the alveolar ridge. Implant Dent. 2017;26:101–105. doi: 10.1097/ID.0000000000000522. [DOI] [PubMed] [Google Scholar]
- 2.Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17:136–159. doi: 10.1111/j.1600-0501.2006.01357.x. [DOI] [PubMed] [Google Scholar]
- 3.Filho JG, Araújo MG. Modificação da técnica de expansão do rebordo alveolar atrófico seguida da instalação imediata de implantes Straumann®: acompanhamento de 10 casos clínicos observados durante 1 ano. Rev Dent Press Periodontia Implant. 2007;1:84–97. [Google Scholar]
- 4.Figliuzzi MM, Giudice A, Pileggi S, Pacifico D, Marrelli M, Tatullo M, et al. Implant-Prosthetic rehabilitation in bilateral agenesis of maxillary lateral incisors with a mini split crest. Case Rep Dent. 2016;2016:1–6. doi: 10.1155/2016/3591321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bassetti MA, Bassetti RG, Bosshardt DD. The alveolar ridge splitting/expansion technique: a systematic review. Clin Oral Implants Res. 2016;27:310–324. doi: 10.1111/clr.12537. [DOI] [PubMed] [Google Scholar]
- 6.Triplett RG, Schow S. Autologous bone grafts and endosseous implants: complementary technique. J Oral Maxillofac Surg. 1996;54:486–494. doi: 10.1016/S0278-2391(96)90126-3. [DOI] [PubMed] [Google Scholar]
- 7.Agabiti I, Botticelli D. Two-stage ridge split at narrow alveolar mandibular bone ridges. J Oral Maxillofac Surg. 2017;75:2115.e1–2115.e12. doi: 10.1016/j.joms.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 8.Garcez-Filho J, Tolentino L, Sukekava F, Seabra M, Cesar-Neto JB, Araújo MG. Long-term outcomes from implants installed by using split-crest technique in posterior maxillae: 10 years of follow-up. Clin Oral Implants Res. 2015;26:326–331. doi: 10.1111/clr.12330. [DOI] [PubMed] [Google Scholar]
- 9.Bruschi G, Capparé P, Bravi F, Grande N, Gherlone E, Gastaldi G, et al. Radiographic evaluation of crestal bone level in split-crest and immediate implant placement: minimum 5-year follow-up. Int J Oral Maxillofac Implants. 2017;32:114–120. doi: 10.11607/jomi.4203. [DOI] [PubMed] [Google Scholar]
- 10.Blus C, Szmukler-Moncler S. Split-crest and immediate implant placement with ultra-sonic bone surgery: a 3-year life-table analysis with 230 treated sites. Clin Oral Implants Res. 2006;17:700–707. doi: 10.1111/j.1600-0501.2006.01206.x. [DOI] [PubMed] [Google Scholar]
- 11.Waechter J, Leite FR, Nascimento GG, Carmo Filho LC, Faot F. The split crest technique and dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46:116–128. doi: 10.1016/j.ijom.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Shibuya Y, Yabase A, Ishida S, Kobayashi M, Komori T. Outcomes and treatments of mal fractures caused by the split-crest technique in the mandible. Kobe J Med Sci. 2014;60:E37–E42. [PubMed] [Google Scholar]