Abstract
The reconstruction of central forehead defect is challenging because of the paucity of the adjacent extensible tissue and aesthetic importance of the area. Reconstruction of this region should be done keeping in mind brow symmetry and natural hairline. Camouflaging the final scar lines in wrinkles or hairline should be the final goal. Even small resections in this region can be surprisingly difficult owing to resistance offered by galea to advancement despite significant undermining due to its inelastic composition and position over the skull’s natural convexity. Following, we present a case report wherein we describe a technique for the reconstruction of central forehead defects using simple Burrow’s triangles.
Keywords: O to T flap, Forehead defect, Periglabellar flap, Burrow’s triangle
Introduction
The reconstruction of central forehead defect is challenging because of the paucity of the adjacent extensible tissue and aesthetic importance of the area [1]. Reconstruction of this region should be done keeping in mind brow symmetry and natural hairline [1]. Camouflaging the final scar lines in wrinkles or hairline should be the final goal. Even small resections in this region can be surprisingly difficult owing to resistance offered by galea to advancement despite significant undermining due to its inelastic composition and position over the skull’s natural convexity [1]. Following, we present a case report wherein we describe a technique for the reconstruction of central forehead defects using simple Burrow’s triangles.
Case Report
A 77-year-old gentleman presented to the head and neck surgical oncology department with complains of progressively increasing non-healing ulcer, measuring 2 × 2 cm2, over the central forehead since last 1 year. The patient was a farmer, ECOG 2 with cardiac comorbidities and uncontrolled hypertension precluding the use of general anaesthesia. Biopsy revealed the lesion to be squamous cell carcinoma, and a CT scan did not show any bone erosion or cervical lymphadenopathy. He underwent wide excision of the lesion with 1.5 cm margin all around with base being the periosteum. The final defect size was 5 × 5 cm2.
Surgical Technique for Closure of the Defect
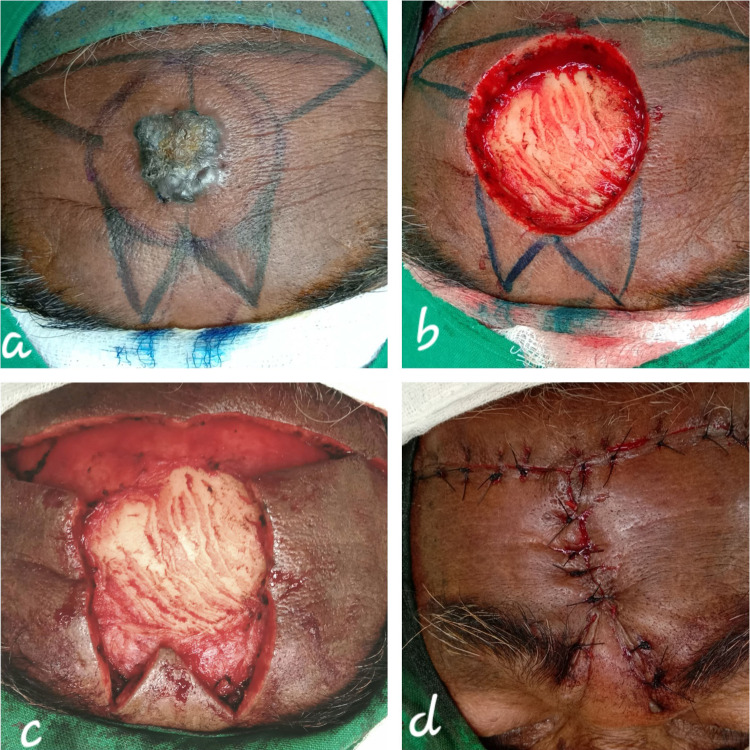
Superiorly, a horizontal tangent was drawn, designed to lie within the natural transverse forehead crease formed by the frontalis muscle, with the length approximately equal to twice the diameter of the lesion, with the midpoint aligning with that of the lesion. Two inferior vertical limbs with widths equal to the radius of the lesion were marked in a fashion so that the final scar lies within creases formed by the corrugator muscles in a ‘W-plasty’ fashion. With the limbs thus marked, the Burrow’s triangles were designed. The inferior triangles were designed such that the apex points towards the medial canthus (Fig. 1).
Fig. 1.
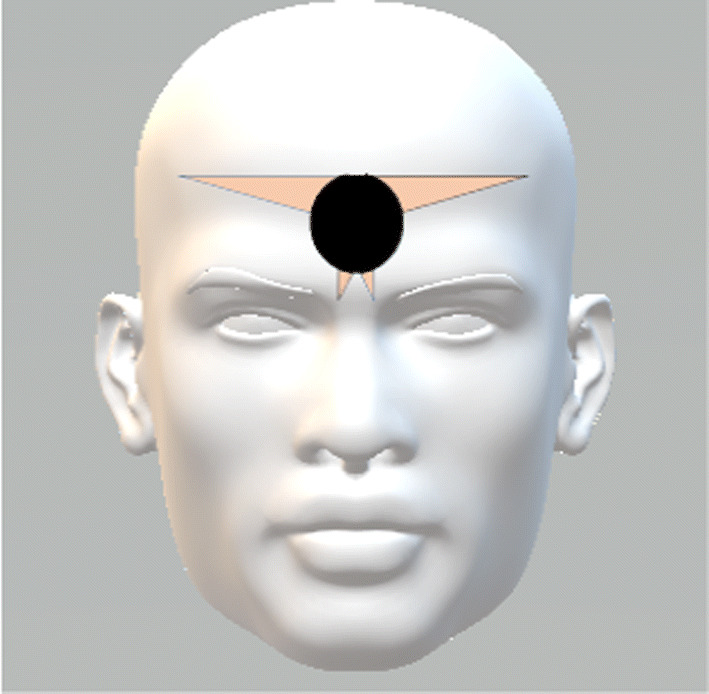
Dark circle represents the defect in the central forehead. The triangles represent the Burrow’s triangles designed for closure of the defect
The Burrow’s triangles were then excised, and the resultant flaps were then raised in a sub-galeal plane and advanced towards the defect. After completion of the sub-galeal dissection till full extent of the flaps, the galea was scored perpendicular to the long axis to improve tissue recruitment. After completely mobilizing the flaps, they were sutured in a ‘T-fashion’ with the tail end of the vertical arm ending in a ‘W-plasty’ (Fig. 2).
Fig. 2.
a Lesion in the central forehead, b defect after ablation, c after fashioning of the Burrow’s triangles and d final closure after mobilizing the flaps in sub-galeal plane
Discussion
While planning reconstruction, the following reconstructive ladder should be kept in mind.
| Technique | In relation to our case |
|---|---|
| Secondary intention | Poor cosmetic outcome |
| Primary closure | > 3 cm defects cannot be closed primarily |
| Split thickness skin graft | Periosteum was removed as part of ablation |
| Local skin flap (Advancement/Rotational) | O–T advancement flap was done. Ideal as like replaces like |
| Local pedicled flap [2] (frontalis musculocutaneous flap) | Could have been tried in our case |
| Distant pedicled flap | Donor sites are very remote. Not possible |
| Vascularized free flap | Patient’s age and comorbidities did not allow administration of general anaesthesia |
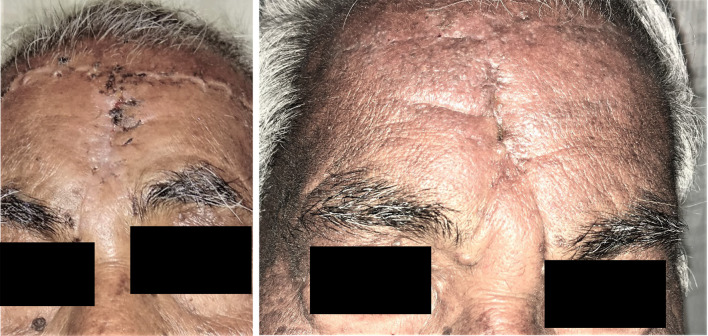
Gonzalez-Ulloa [3] is credited with conception of the idea of aesthetic facial units, wherein the entire forehead from eyebrow to hairline was considered a single aesthetic unit. Subsequently, it was subdivided into para-median, lateral and lateral temporal regions [4]. The goal is to hide the final scar lines in the resting skin tension lines (RSTLs) or in the borders between the subunits (Fig. 3).
Fig. 3.
First picture is post-op 2 weeks, and the second picture is post-op 6 weeks
Advancement of local tissue from the forehead and glabellar regions by using Burrow’s triangles is a simple and effective method for closure of central forehead defects [5]. The superior triangles create a scar that lies within the frontalis crease, and the scar formed by the inferior triangles lies within corrugator crease and finally get camouflaged by the dynamic motion of the muscles overtime [5]. The eventual ‘W-plasty’ additionally helps by preventing the dog ear from extending down onto the nose [6]. The vertical scar in the midline or para-median is considered cosmetically superior as it avoids the risk of displacement in the position of the eyebrows or the hairline [7]. A dual-plane dissection in subcutaneous and sub-galeal planes has been described in the literature as a modification, which enables optimal en-bloc tissue advancement for closure of larger wounds with tension-free and everted skin edges [8].
Another mode of reconstruction with defect diameter < 30 mm in the central forehead region is ‘H-flap’. The concept is based on double opposing rectangular advancement flap with length–breadth ratio of up to 2:1. The resultant transverse scars are camouflaged in the forehead creases, and the length of the vertical scar is minimal [9].
Besley et al. have proposed a staging classification of the scalp and forehead defects, where in they have classified forehead and scalp defects < 50 and 200 cm2, respectively, as stage IA and that can be closed with primary closure or with local flaps. Stage IB represents similar defects, however, with associated heavy trauma/osteomyelitis/osteoradionecrosis/previously irradiated tissue/post-op radical radiation/local flap failure. Stage II represents > 50 cm2 forehead defect or 200–600 cm2 scalp defect. For stage IB and II, authors recommend free vascular tissue transfer reconstruction [10].
Conclusion
Central forehead defects where primary closure is not feasible can be reconstructed with good aesthetic outcome by local tissue advancement using Burrow’s triangles especially in the elderly with relatively good tissue pliability. Defects in the central forehead region with diameter up to 5.3 cm and total; area of < 50 cm2 can be closed by this technique [5, 11]. This technique may not be suitable for the younger generation owing to their better skin tone and lack of camouflaging rhytides [5].
Funding
No funding was received for this project from any source.
Compliance with Ethical Standards
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abhishek Ghosh, Email: 13abhishekghosh@gmail.com.
Swagnik Chakrabarti, Email: dr.swagnik@gmail.com.
Atul Kumar Rai, Email: atulrai.dentist@gmail.com.
Tanvi Choubey, Email: choubeytanvi@gmail.com.
Achyuth Panuganti, Email: achyuth.panuganti@gmail.com.
Sandeep Bhukar, Email: cool.sandz@gmail.com.
References
- 1.Temple CLF, Ross DC. Scalp and forehead reconstruction. Clin Plast Surg. 2005;32:377–390. doi: 10.1016/j.cps.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Guerrerosantos J. Frontalis musculocutaneous island flap for coverage of forehead defect. Plast Reconstr Surg. 2000;105:18–22. doi: 10.1097/00006534-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Ulloa M. Restoration of the face covering by means of selected skin in regional aesthetic units. Br J Plast Surg. 1957;9(3):212–215. doi: 10.1016/s0007-1226(56)80036-2. [DOI] [PubMed] [Google Scholar]
- 4.Siegle RJ. Reconstruction of the forehead. In: Baker SR, Swanson NA, editors. Local flaps in facial reconstruction. St. Louis: Mosby-Year Book; 1995. pp. 421–442. [Google Scholar]
- 5.Birgfeld C, Chang B. The periglabellar flap for closure of central forehead defects. J Plast Reconstr Surg. 2007;120:130–133. doi: 10.1097/01.prs.0000263534.37515.51. [DOI] [PubMed] [Google Scholar]
- 6.Grigg R. Forehead and temple reconstruction. Otolaryngol Clin North Am. 2001;34(3):583–600. doi: 10.1016/S0030-6665(05)70007-4. [DOI] [PubMed] [Google Scholar]
- 7.Burget G. The paramedian forehead flap. In: Burget GC, Menick F, editors. Aesthetic reconstruction of the nose. St. Louis: Mosby; 1994. pp. 57–91. [Google Scholar]
- 8.Boustany A, Ghareeb P, McClellan WT. Forehead reconstruction using a modified dual-plane A to T flap. Can J Plast Surg. 2012;20(4):251–254. doi: 10.1177/229255031202000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose V, Overstall S, Moloney DM, Powell BWEM. The H-flap: a useful flap for forehead reconstruction. Br J Plast Surg. 2001;54:705–707. doi: 10.1054/bjps.2001.3689. [DOI] [PubMed] [Google Scholar]
- 10.Beasley NJP, Gilbert RW, Gullane PJ, et al. Scalp and forehead reconstruction using free revascularized tissue transfer. Arch Facial Plast Surg. 2004;6(1):16–20. doi: 10.1001/archfaci.6.1.16. [DOI] [PubMed] [Google Scholar]
- 11.Kruse-Losler B, Presser D, Meyer U, Schul C, Luger T, Joos U. Reconstruction of large defects on the scalp and forehead as an interdisciplinary challenge: Experience in the management of 39 cases. Eur J Surg Oncol. 2006;32:1006–1014. doi: 10.1016/j.ejso.2006.05.001. [DOI] [PubMed] [Google Scholar]