Abstract
Aim
To evaluate the efficacy of postsurgical oral prophylactic antibiotic versus antimicrobial suture placement in preventing infection after removal of an impacted mandibular third molar.
Materials and methods
This was a prospective, single-blind study including 150 individuals of 18–40 years divided into two groups with 75 patients each. The patients in Group 1 were administered oral amoxicillin tablets 500 mg for 5 days postsurgery with 3–0 polyglactin sutures for closure and in group 2 with (3–0) antimicrobial chlorhexidine diacetate-impregnated polyglactin sutures only. Evaluation was done on 3rd, 7th, 15th days and 1 month.
Results
There was no significant difference in rates of infection between the groups. Abnormal erythema, pain and trismus showed statistically better results in group 2 on 3rd and 7th days. An antibiotic side effect assessment showed 17.65% patients with minor side effects.
Conclusion
Chlorhexidine diacetate-impregnated polyglactin sutures showed reduced erythema, pain and trismus in healthy patients undergoing surgical removal of third molar.
Keywords: Chlorhexidine diacetate-impregnated polyglactin suture, Postsurgical antibiotic prophylaxis, Infection, Erythema, Trismus, Antibiotic side effect assessment
Introduction
The surgical removal of impacted third molars represents the keystone of oral and maxillofacial ambulatory procedures that are considered as clean-contaminated operations [1]. Numerous studies indicate that the incidence of postoperative infections following the surgical removal of third molar ranges from 1 to 5.8% and the routine use of antibiotics is not advised for the prevention of such a low incidence of serious infection [2].
The debate about the use of antibiotic prophylaxis began in the early 1950s following which Peterson, in his article, has precisely described these principles: (1) the surgical procedure should have a significant risk of infection; (2) the correct antibiotic should be selected for the surgical procedure; (3) the antibiotic level must be high; (4) the antibiotic should be administered in a correct time; (5) the shortest effective antibiotic exposure should be used [3]. The first principle sets the criterion for antibiotic usage, whereas principles 2–5 outline the protocol for administration of the antibiotic. If the routine use of antibiotics for third molar surgery is to be prescribed, principle 1 must be proved right.
Antibiotic resistance is currently a serious issue, which was not the case 50 years ago. It is estimated that 6–7% of patients who are given antibiotics have some kind of adverse reaction [2]. But, the lack of detailed data leads to the use of antibiotics in the absence of a precise indication. Clinicians are forced to give antibiotics in most cases, as patients may lack confidence on their surgeon who do not prescribe antibiotics [4].
Sutures are of paramount importance, whose major purpose is to hold tissues together and facilitate primary healing process [5]. But, in contact with the wound surface, suture materials are immediately coated with protein-rich fluids, such as fibrinogen and fibronectin, which is an ideal environment for microorganisms to harbour and rapidly multiply in large numbers infecting the surgical site [6]. Among antimicrobials, chlorhexidine has a broad antibacterial spectrum as well as high biocompatibility indices and is routinely used in oral surgery.
So, a suture impregnated with chlorhexidine will show antibacterial efficacy, safety and high tissue integration. It is effective against the most gram-negative and gram-positive bacteria including the most clinically relevant pathogen genus staphylococci, causing wound and nosocomial infections [7]. Therefore, chlorhexidine diacetate-impregnated polyglactin sutures are a good choice that can replace the conventional method of administering antibiotic in routine third molar surgeries, thus maximising antimicrobial benefits locally and reducing antibiotic load systemically and the complications that follow.
Methodology
In our prospective, blinded study, we included 150 consented individuals of age group 18–40 years who were indicated to undergo surgical removal of impacted mandibular third molar under local anaesthesia at our unit.
The patients were divided into two groups for the study, each consisting of 75 patients.
Group 1: Individuals who were given postsurgical oral prophylactic antibiotic amoxicillin 500 mg thrice a day with plain 3–0 polyglactin sutures in simple interrupted sutures for 5 days.
Group 2: Individuals who were given antimicrobial chlorhexidine diacetate-impregnated 3–0 polyglactin sutures in a simple interrupted fashion without any antibiotics for closure of the surgical site.
Procedure
All patients chosen for the study underwent basic hemogram investigations and were prepared in a standard manner under aseptic conditions. The cases were operated utilising standard incisions and procedural steps through buccal bone guttering technique and tooth splitting as per the type, depth and position of the impacted mandibular third molar. Following the third molar removal adequate curettage, debridement, thorough irrigation and the flaps were closed with plain (3–0) polyglactin or chlorhexidine diacetate-impregnated (3–0) polyglactin. They were given saline mouthwashes postoperatively for 7 days to be used thrice daily after the procedure and infiltration of long-acting local anaesthetic 0.5% bupivacaine with no steroidal injections postoperatively. Patients were prescribed analgesics for 3 days postoperatively. The patients were evaluated on 3rd, 7th and 15th days and 1 month after the day of surgery.
Inclusion Criteria
Patients of age 18 years or older with the impacted mandibular third molar with no prior signs of clinical infection or pain with adequate mouth opening and normal TMJ function. Partial or complete bony impactions of mandibular third molars.
Exclusion Criteria
Patients on drugs that might alter the course of study and affect the healing of the surgical site, e.g. aspirin, NSAIDs, steroids and cytotoxic drugs.
Patients who have taken antibiotics prior, in a span of 2–3 weeks for any head and neck infections or upper respiratory tract (penicillin/cephalosporin).
Patients with known allergic reactions to chlorhexidine, beta-lactams and cephalosporins.
Patients lost to follow-up.
Pregnancy and lactating mothers or oral contraceptives.
Patients with poor oral hygiene.
Patients under radiotherapy or chemotherapy.
Chronic smokers.
Evaluation Criteria
Primary efficiency variable was the development of infection throughout the study period. The secondary variables were taken as abnormal erythema, swelling, trismus and pain.
Infection defined as
Presence of purulent discharge in the extraction socket with or without swelling or pain.
Presence of local abscess.
Onset of any facial or cervical cellulitis or any space infections.
Abnormal erythema scored as
0 = absence of any signs of erythema.
1 = presence of redness and hyperaemia around the surgical site.
2 = bleeding from the surgical site.
3 = ulceration of the surgical site.
Swelling (the distance between the lower insertion of auricular lobe to the chin medial point and distance between the medial canthus of the eye to the gonial angle were evaluated) scored as
0 = absence of swelling.
1 = increase, less than 5 mm compared to pre-surgery.
2 = increase, more than 10 mm compared to pre-surgery.
Trismus (measurement taken before and after surgery using a ruler assessed on days 0, 3, 7 and 15) scored as
0 = absence of any difference.
1 = decrease, less than 10 mm compared to pre-surgery.
2 = decrease, more than 10 mm pre-surgery.
Pain scored as
0 = absence of pain.
1 = pain assessment less than 5.
2 = pain assessment greater than 5.
Patients were given a subjective pain scale ranging from 0 to 10 (visual analogue scale—Wong–Baker scale).
Assessment of side effects Questionnaire given to the patients in all three groups during the first and second visits. Side effects such as headache, weakness, insomnia, nausea, diarrhoea, tremors, constipation, taste disturbances, acidity and dizziness.
Results
The study was comprised of 150 patients with 75 allotted to each of the treatment groups in a randomised manner. Seven and six patients were excluded in group 1 and group 2, respectively, as these patients were lost to follow-up. Among 68 patients in group 1, 27 were females and 41 were males with a mean age of 25.205, whereas in group 2, 69 patients were evaluated of whom 24 were females and 45 were males with a mean age of 24.463.
The incidence of infection in group 1 was numerically 2 out of 68 cases and in group 2 was 3 in 69 cases during which all patients returned to us with severe pain, purulent discharge and severe trismus by the 3rd to 5th postoperative days. These cases were thoroughly evaluated, necessary intervention was done and appropriate medications were prescribed as required. They were evaluated in the subsequent visits as well. The statistical analyses comparing both the groups were performed on the first, second and third visits respectively which were insignificant. The fourth visit seemed to be irrelevant for comparison.
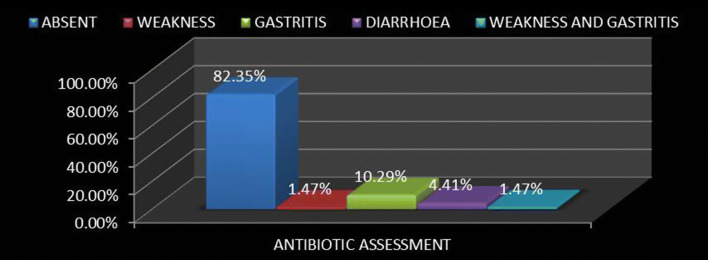
There was a clear difference in the values of abnormal erythema between the groups in the first visit with a frequency distribution of abnormal erythema of 76.5% (Fig. 1) and 43.5% (Fig. 2) in group 1 and group 2, respectively, with a P value of 0.000 which was highly significant, whereas the second visit showed no significant difference in either groups.
Fig. 1.
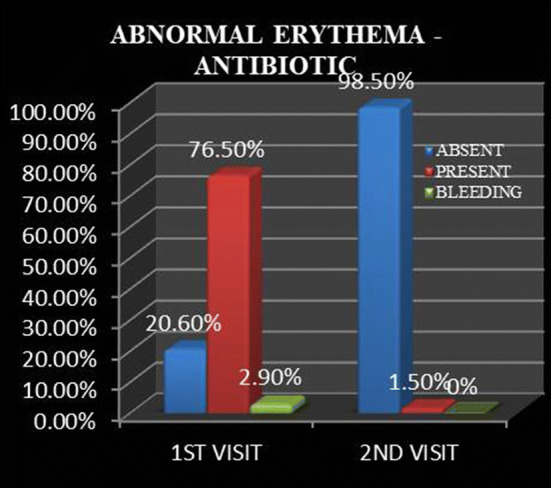
Abnormal erythema in antibiotic group in the first and second visits
Fig. 2.
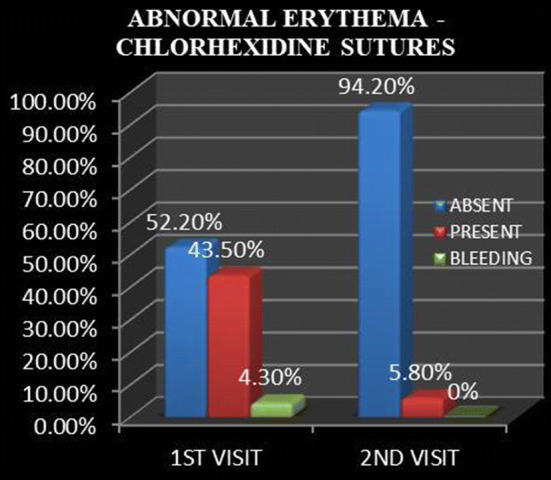
Abnormal erythema in chlorhexidine group in the first and second visits
There was no significant difference between the values in swelling in either groups during the first or the second visits. But, numerically the antibiotic group showed candidates with lesser amount of swelling when compared with the chlorhexidine-impregnated suture group. Swelling was completely eliminated in the third and fourth visits in all the patients.
There was a clear difference between the values in case of trismus of the first visit in either groups with a frequency of 49.27% of no trismus in the chlorhexidine-impregnated suture group (group 2) as compared to 17.64% in postsurgical antibiotic group (group 1), < 10 mm difference in maximum mouth opening from preoperative values as 44.11% in group 1 and 27.53% in group 2 and > 10 mm difference in maximum mouth opening from preoperative values as 38.23% in group 1 and 23.18% in group 2 with a P value of 0.000 which was inferred as highly significant, showing that trismus was much less in the chlorhexidine-impregnated suture group as compared to postsurgical antibiotic group. The second visit values showed that almost 45 in group 1 and 50 in group 2 had completely regained preoperative values of mouth opening and the remaining candidates had < 10 mm of trismus in either groups; hence, it was statistically insignificant. The third and fourth visits showed no relevant values for comparison as all the candidates were completely relieved of trismus and achieved complete preoperative values of maximum mouth opening (Figs. 3, 4).
Fig. 3.
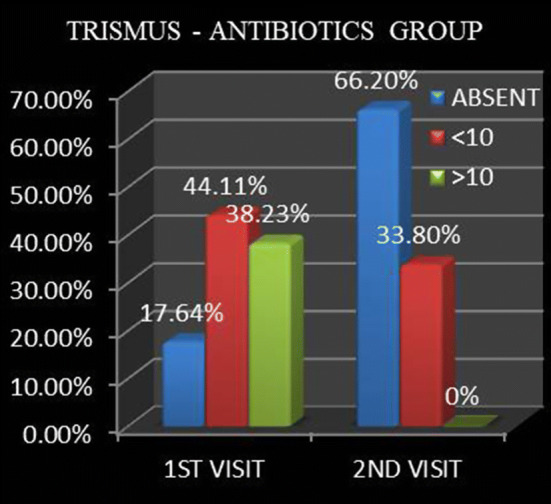
Trismus parameter in antibiotic group in the first and second visits
Fig. 4.
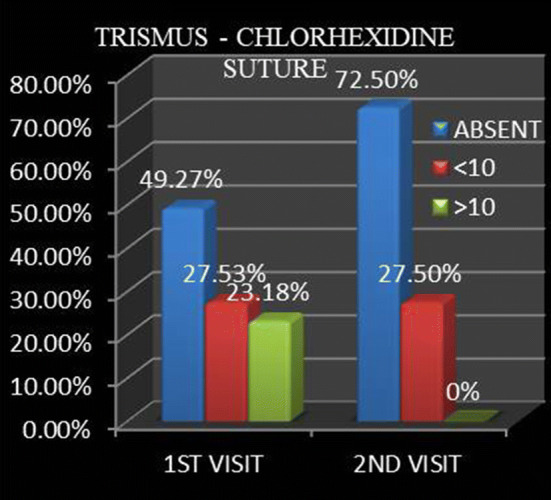
Trismus parameter in chlorhexidine group in the first and second visits
A statistically significant difference was seen in the case of pain either groups on the first visit with a frequency of no pain in 27.9% in group 1 and 47.8% in group 2, VAS < 5 in 69.1% in group 1 and 47.8% in group 2 and VAS > 5 in very few individuals and 2.9% in group 1 and 4.3% in group 2 with a P value of 0.041, whereas in the second visit there was amelioration of pain in either groups and only five candidates in group 1 and four candidates in group 2 showed VAS < 5. Patients were completely relieved of pain by the third visit. Hence, comparison was nil in the third and fourth visits (Table 1).
Table 1.
Pain parameter comparison between the groups
| Pain | No pain | VAS < 5 | VAS > 5 | Total | Chi square value | Sig. | |
|---|---|---|---|---|---|---|---|
| First visit | Antibiotic | 19 (27.9) | 47 (69.1) | 2 (2.9) | 68 (100) | 6.412 | 0.041 (S) |
| Chlorhexidine sutures | 33 (47.8) | 33 (47.8) | 3 (4.30 | 69 (100) | |||
| Total | 52 (38) | 80 (58.4) | 5 (3.6) | 137 (100) | |||
| Second visit | Antibiotic | 63 (92.6) | 5 (7.4) | 0 (0) | 68 (100) | 0.135 | 0.491 (N.S) |
| Chlorhexidine sutures | 65 (94.2) | 4 (5.8) | 0 (0) | 69 (100) | |||
| Total | 128 (93.4) | 9 (6.6) | 0 (0) | 137 (100) | |||
S significant, N.S non significant
Assessment of antibiotic side effects was done via a questionnaire in 68 random candidates; side effects were absent in 82.35%. Side effects were found in 17.65% of the patients who took antibiotics. It was distributed as gastritis in 10.29% being the highest, diarrhoea in 4.41% patients, weakness in 1.47% and weakness with gastritis in 1.47% (Fig. 5).
Fig. 5.
Frequency showing an antibiotic side effect assessment
Taking each parameter into consideration, abnormal erythema, pain and subsequently trismus were comparatively less in the chlorhexidine-impregnated suture group, whereas a mild difference in swelling was noted and antibiotic group had lesser swelling which was statistically insignificant. Infection among the individuals in either group was statistically insignificant in nature as owing to the very few cases reported in these healthy individuals. Antibiotic side effects were seen in 17.65% of patients which was a significant value, although the side effects were not severe in nature and subsided as soon as medications ceased.
Discussion
The history of antibiotics is dated back to 1928, when Sir Alexander Fleming discovered penicillin—the first antibiotic. Between 1940 and 1962, most of the antibiotic classes we use today were discovered and introduced into the market. Since then, antibiotics have changed the phase of medicine and their usage slowly gained pace leading to a common practice.
Poeschl et al. [8] in a prospective study of more than 30 months with a total of 528 impacted lower third molars concluded that postoperative oral prophylactic antibiotic treatment did not contribute to a better wound healing or prevent inflammatory complications after surgery; hence, it was not recommended for routine use. This result had compatible findings with the study conducted by Curran et al. [9] 30 years back, which also concluded that the use of prophylactic antibiotics in third molar surgery is unnecessary unless specific systemic factors are present.
The removal of impacted third molar invariably causes some degree of infection, erythema around the surgical site, pain, swelling, trismus and wound dehiscence. In the current prospective randomised control study, we included 150 patients with 75 in each group out of whom few were lost to follow-up and the above-mentioned parameters were taken into consideration.
The choice of prophylactic antibiotic for transoral procedures is penicillin, as it is effective against a large bacterial spectrum, non-toxic and bactericidal [2]. Among penicillin, amoxicillin is a widely used antibiotic in transalveolar exodontia cases and hence chosen as the antibiotic for postsurgical oral prophylactic antibiotics in our study.
Chlorhexidine is a widely used antimicrobial in various forms. Chlorhexidine diacetate is a bisbiguanide compound with a rapid bactericidal activity against both gram-positive and gram-negative organism. The antibacterial effect of chlorhexidine is related to its action on the bacterial cell membrane and precipitation of intracellular contents [10]. They are both bacteriostatic and bactericidal in nature.
An infection rate in group 1 was 3% and group 2 was 4.3%, which majorly challenges the benefit of antibiotic prophylaxis in third molar surgery in patients who are healthy. On the other hand, the chlorhexidine diacetate-impregnated polyglactin sutures showed almost equal results to group 1 which further questions the need for postsurgical prophylactic antibiotics and considering antimicrobial sutures as an acceptable alternative.
Abnormal erythema showed a clear difference between the groups. The significant absence can be attributed to the prevention of biofilm formation over the suture material. The main issue is the proliferation of attached bacteria and formation of persistent biofilms over the suture material. Once a biofilm has developed, it protects bacteria against the host’s immune system as well as systemically and locally applied antibiotics. The use of antimicrobial coated sutures can be used to inhibit viable adhered microbes and thus prevent biofilm formation. In detail, testing with Staphylococcus aureus by Obermeier et al. [7], the chlorhexidine laurate coating (CL11) molecularly similar to chlorhexidine diacetate which is chlorhexidine palmitate, best meets the medical requirements for a fast bacterial eradication and a high drug release during the first clinically most relevant 48 h, as well as biocompatibility.
Swelling can be caused by the response of the tissues to manipulation and trauma caused during surgery. Its onset is gradual and maximum swelling would be present during 48 h after surgery. Regression of the swelling is expected by the 4th day and complete resolution occurs in 7 days [11]. Zeitler [2] in his review article stated that the use of antibiotics to decrease adverse outcomes such as trismus, pain and swelling tends to show little improvement with antibiotics. Follow-up visits showed no difference between the groups.
The postsurgical pain begins when the effect of the local anaesthesia subsides and reaches peak levels in 6–12 h postoperatively [11]. In our study, we had locally infiltrated the surgical site with 0.5% bupivacaine, and the pain control lasted for approximately 8 h postoperatively. Non-steroidal anti-inflammatory drugs were prescribed to the patient for appropriate pain control for the next 3 days. On the first visit (3rd day postoperatively), a subjective evaluation of pain was done with the Wong–Baker facial grimace scale and visual analogue scale (VAS).
Antibiotic side effects in our study were evaluated via a questionnaire provided to the subjects on their first visit. 17.65% of patients who took antibiotics complained of side effects. Medical misuse is one of the most important factors to contribute to the development of antibiotic resistance in bacteria [12]. According to Zeitler’s opinion about antibiotic usage in third molar removal, he proposed that the potential for adverse reaction to antibiotic therapy must exceed any possible decrease in infection rate [2]. In accordance with Petersons with his classification of the procedures, surgical removal of a third molar is considered as Class II or clean-contaminated surgery. Other surgical factors taken into consideration by Peterson were the duration of the procedure more than 3 h and the insertion of a foreign body [3], either of which did not take place in this procedure. Hence, the routine usage of antibiotics in a normal healthy individual without the risk of infection cannot be justified.
To conclude, we have found that chlorhexidine diacetate-impregnated polyglactin sutures showed superior results when compared with postsurgical antibiotic prophylaxis with plain polyglactin sutures taking into account the inflammatory outcomes of localised erythema, pain and trismus following the procedure. The local action of chlorhexidine sutures on the surgical site must have resulted in this difference as compared to plain polyglactin sutures.
Chlorhexidine diacetate-impregnated polyglactin sutures have been introduced recently. No adverse effects were noted throughout our study. More extensive and advanced studies might be required in both microbiological and molecular levels to abstract additional information about the same.
Despite the limitations of the current study, we would recommend the use of this antimicrobial suture in various intraoral procedures for effective control of inflammatory and infectious parameters (with or without use of antibiotics as indicated in each procedure).
Acknowledgements
The author would like to express their sincere gratitude to Dr. Vinod Thangaswamy, Professor and Head of the Department of Coorg Institute of Dental Sciences.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ataoğlu H, Öz GY, Çandirli C, Kiziloğlu D. Routine antibiotic prophylaxis is not necessary during operations to remove third molars. Br J Oral Maxillofac Surg. 2008;46(2):133–135. doi: 10.1016/j.bjoms.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Zeitler DL. Prophylactic antibiotics for third molar surgery: a dissenting opinion. J Oral Maxillofac Surg. 1995;53(1):61–64. doi: 10.1016/0278-2391(95)90503-0. [DOI] [PubMed] [Google Scholar]
- 3.Peterson LJ. Antibiotic prophylaxis against wound infections in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1990;48(6):617–620. doi: 10.1016/s0278-2391(10)80477-x. [DOI] [PubMed] [Google Scholar]
- 4.Bezerra TP, Studart-Soares EC, Scaparo HC, Pita-Neto IC, Batista SH, Fonteles CS. Prophylaxis versus placebo treatment for infective and inflammatory complications of surgical third molar removal: a split-mouth, double-blind, controlled, clinical trial with amoxicillin (500 mg) J Oral Maxillofac Surg. 2011;69(11):e333–e339. doi: 10.1016/j.joms.2011.03.055. [DOI] [PubMed] [Google Scholar]
- 5.Dennis C, Sethu S, Nayak S, Mohan L, Morsi Y, Manivasagam G. Suture materials—current and emerging trends. J Biomed Mater Res Part A. 2016;104(6):1544–1559. doi: 10.1002/jbm.a.35683. [DOI] [PubMed] [Google Scholar]
- 6.Scaffaro R, Botta L, Sanfilippo M, Gallo G, Palazzolo G, Puglia AM. Combining in the melt physical and biological properties of poly (caprolactone) and chlorhexidine to obtain antimicrobial surgical monofilaments. Appl Microbiol Biotechnol. 2013;97(1):99–109. doi: 10.1007/s00253-012-4283-x. [DOI] [PubMed] [Google Scholar]
- 7.Obermeier A, Schneider J, Harrasser N, Tübel J, Mühlhofer H, Pförringer D, von Deimling C, Foehr P, Kiefel B, Krämer C, Stemberger A. Viable adhered Staphylococcus aureus highly reduced on novel antimicrobial sutures using chlorhexidine and octenidine to avoid surgical site infection (SSI) PloS one. 2018;13(1):e0190912. doi: 10.1371/journal.pone.0190912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poeschl PW, Eckel D, Poeschl E. Postoperative prophylactic antibiotic treatment in third molar surgery—a necessity? J Oral Maxillofac Surg. 2004;62(1):3–8. doi: 10.1016/j.joms.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Curran JB, Kennett S, Young AR. An assessment of the use of prophylactic antibiotics in third molar surgery. Int J Oral Maxillofac Surg. 1974;3(1):1–6. doi: 10.1016/s0300-9785(74)80030-x. [DOI] [PubMed] [Google Scholar]
- 10.Sanchez IR, Nusbaum KE, Swaim SF, Hale AS, Henderson RA, Mcguire JA. Chlorhexidine diacetate and povidone-iodine cytotoxicity to canine embryonic fibroblasts and Staphylococcus aureus. Vet Surg. 1988;17(4):182–185. doi: 10.1111/j.1532-950x.1988.tb00995.x. [DOI] [PubMed] [Google Scholar]
- 11.Deliverska EG. Petkova M (2016) Complications after extraction of impacted third molars-literature review. J IMAB Annu Proc Sci Pap. 2016;22(3):1202–1211. [Google Scholar]
- 12.Chitra N. Amoxicillin resistance in transient bacteremia after third molar surgeries. J Pharm Res. 2014;8(3):277–280. [Google Scholar]