Summary
On Aug 25 2020, the Africa Regional Commission for the Certification of Poliomyelitis Eradication declared that the WHO African region had interrupted transmission of all indigenous wild polioviruses. This declaration marks the African region as the fifth of the six WHO regions to celebrate this extraordinary achievement. Following the Yaoundé Declaration on Polio Eradication in Africa by heads of state and governments in 1996, Nelson Mandela launched the Kick Polio out of Africa campaign. In this Health Policy paper, we describe the long and turbulent journey to the certification of the interruption of wild poliovirus transmission, focusing on 2016–20, lessons learned, and the strategies and analyses that convinced the Regional Commission that the African region is free of wild polioviruses. This certification of the WHO African region shows the feasibility of polio eradication in countries with chronic insecurity, inaccessible and hard-to-reach populations, and weak health systems. Challenges have been daunting and the sacrifices enormous—dozens of health workers and volunteers have lost their lives in the pursuit of a polio-free Africa.
Introduction
Poliomyelitis, a viral disease that can lead to a lifetime of paralysis or even death, is caused by three serotypes of poliovirus. Since the launch of the Global Polio Eradication Initiative in 1988 with the aim of eradicating wild polioviruses, the incidence of polio has decreased by 99·99%, from approximately 350 000 cases annually in 125 countries in 1988, to 102 cases in two countries in 2020 as of Aug 19, 2020.1 Since the eradication effort began in 1988, an estimated 18 million cases of paralytic polio have been prevented.2 Globally, of the three serotypes of wild poliovirus, the last case of poliomyelitis due to indigenous wild poliovirus type 2 (WPV2) was reported in 1999, and wild poliovirus type 3 (WPV3) has not been detected since November, 2012.3 WPV2 was certified by the WHO Global Certification Commission for Poliomyelitis Eradication as eradicated in September, 2015,4 and WPV3 was so certified in October, 2019.3 Since that time, the circulation of wild poliovirus type 1 (WPV1) has been limited to parts of Afghanistan and Pakistan.
On Aug 25, 2020, the Africa Regional Commission for the Certification of Poliomyelitis Eradication declared that the WHO African region had interrupted the transmission of all indigenous wild poliovirus. The last person infected with WPV1 with acute flaccid paralysis in the African region was reported in the Monguno local government area, Borno State, Nigeria, and the date of onset of paralysis was Aug 21, 2016. The last time WPV1 was detected in Africa was in a stool sample from a healthy child in the same local government area on Sept 27, 2016.5 This declaration marks the African region as the fifth of the six WHO regions to celebrate this crucial milestone.
Certification mechanism
The Regional Commission comprises 16 members with expertise in public health, epidemiology, virology, microbiology, paediatrics, and neurology, and its membership has continued to be renewed since its inception in 1998. The Commission is the only body with the authority to certify the interruption of wild poliovirus transmission in the African region. Members can not have direct responsibility for polio programme activities in the African region or in their own countries. To facilitate sharing of information and best practices, members from the Regional Commissions of the WHO region of the Americas (PAHO), Eastern Mediterranean region, European region, and South-East Asia region are on the Africa Regional Commission.
Principles
Certification of the African Region was based on an assessment of documented evidence, with a focus on high-quality surveillance and improved routine immunisation coverage. Evidence was solicited from border areas and areas of conflict and high risk to ensure that no blind spots remained in any country or area, such as might occur due to war, among migratory or internally displaced populations, or for remote or hard-to-access areas. Complete country documentation of polio-free status was not submitted to the Africa Regional Commission until 3 years after the last detected occurrence of wild poliovirus in the presence of high-quality surveillance.
Criteria for certification
The main criterion established for certification was the absence of wild poliovirus isolated from patients with acute flaccid paralysis (ie, suspected poliovirus infection) for a period of at least 3 years in the presence of high-quality certification-standard surveillance.6 The Africa Regional Commission determined that the absence of wild poliovirus in stool samples from healthy children and from environmental (waste water) samples would provide valuable additional information to confirm the absence of circulating wild poliovirus. Evidence of improved routine immunisation coverage also was sought given the focus on improving immunisation coverage in all countries in the region.7 Finally, evidence of the destruction or containment of all wild poliovirus stocks in laboratories and other facilities was required.
Documentation
Complete country documentation requirements were presented on a template with instructions to ensure the standardised provision of the essential data required for certification. These data included country background information, history of confirmed poliovirus cases, performance of surveillance for acute flaccid paralysis, laboratory surveillance activities, immunisation activities, laboratory containment of wild polioviruses and potentially infectious materials, and a polio risk assessment. Supplementary documentation included a polio outbreak preparedness and response plan. In Nigeria, state-level data were requested for Borno State and other chronic security-compromised areas in the northeastern part of the country.
Process
The Africa Regional Commission met annually and, since 2013, two to three times a year to review the required annual country progress reports for those not yet certified as polio-free, national documentation of polio-free status for those claiming polio-free status for the first time, and annual country updates for those whose national documentation of polio-free status had previously been accepted.
The national documentation of polio-free status was reviewed in detail by at least two designated Commission members, and additional feedback was solicited from all other members after a formal presentation and closed session with the country team. The decision to accept the documentation was based on the opinion of the National Certification Committees, the quality of the complete country documentation, and field visits to countries to ensure that the country was well prepared to present their complete documentation and to verify the data for completeness and accuracy. Acceptance of the documentation meant that the Regional Commission agreed with the National Committee that sufficient information was provided to support the claim that the country had interrupted transmission of all indigenous wild polioviruses. The National Certification Committees were responsible for reviewing and assessing the documentation prepared by national staff and, where necessary, for doing field visits. They had no authority to certify polio elimination in the country but submitted their opinion and justification on whether the country should be declared free of wild poliovirus to the Regional Commission.
Advocacy visits by Regional Commission members to ministers of health or heads of governments were done as required to ensure political commitment to elimination and to discuss any perceived barriers to meeting the certification requirements established by the Commission. During the field verification visits, the Commission provided further recommendations to the country at national and subnational levels to improve its documentation and polio programme performance.
The road to certification
Absence of wild polioviruses
The WHO African region comprises 47 countries and includes most of the African continent (figure 1). It has a current estimated population of 1019·9 million, 13·7% of the global population;8 approximately 15% of the population are younger than 5 years and 41% are younger than 15 years.9 Cases of wild poliovirus infection have been imported and exported between countries in the Eastern Mediterranean and African regions over the years, necessitating collaborative programmatic efforts between WHO regions to respond to outbreaks and plan immunisation activities, with a particular focus on mobile populations.
Figure 1.
Map of the WHO African region
Although the Africa Regional Commission was appointed in 1998, countries needed several years to establish the certification-standard surveillance required for submission of complete country documentation. Also, WHO had required that countries should continue use of clinical case confirmation criteria (ie, confirmation on the basis of signs and symptoms of polio), until surveillance, including collection of adequate stool specimens (ie, two samples collected at least 24 h apart, within 14 days after onset of paralysis),10 was good enough to switch to virological case confirmation (ie, only patients with acute flaccid paralysis and isolation of poliovirus being confirmed as having polio). The Commission initially used its yearly meetings to advocate for rapid improvements in surveillance quality, particularly the collection of adequate stool specimens from patients with acute flaccid paralysis and improvements to laboratory-based surveillance. Additionally, once a country was selected to submit its complete country documentation, up to a year could be spent generating the documentation.
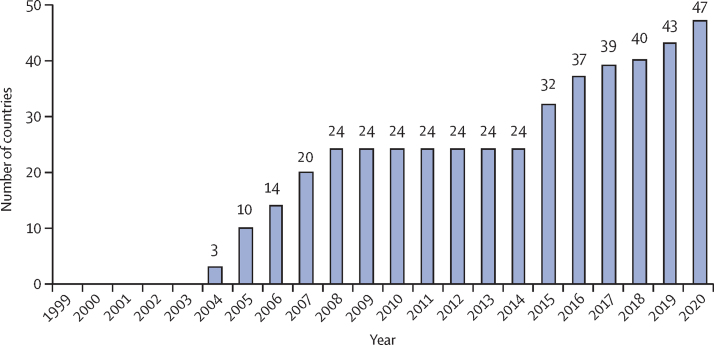
When countries began submitting their complete country documentation to the Regional Commission, 12 had not detected polio since 1998, Comoros had not detected polio since 1969, and Mauritius and Seychelles had not detected polio since 1967. In 2004, the Regional Commission accepted the national documentation of polio-free status of only three countries: The Gambia, Senegal, and Rwanda. By 2008, 24 countries had been declared free of wild poliovirus (figure 2).
Figure 2.
Cumulative number of countries with national documentation of polio-free status accepted by the Africa Regional Commission for the Certification of Poliovirus Elimination, annually, 1999–2020
Extensive and repeated outbreaks of wild poliovirus in 2009 resulted in the discontinuation of certification activities in 2010–12, and no submissions or acceptance of complete country documentation until 2015. These outbreaks started in Nigeria, catalysed by false rumours about the safety of oral poliovirus vaccine and vaccine refusals, and had spread to many countries in the region and beyond.11 In 11 of these countries, complete country documentation had been previously accepted by the Africa Regional Commission, and the annual country updates from those countries were reviewed with the aim of determining whether the acceptance of the documentation should be rescinded.
Then, another major setback occurred. In August–September, 2016, 2 years after the most recent wild poliovirus case was reported in Nigeria in July, 2014, four cases of infection with WPV1 were detected in a remote and security-challenged area of Borno State in northeastern Nigeria.5 In 2015, WHO had announced that Nigeria had been removed from the list of polio-endemic countries.12 The serious security issues in that part of the country resulting from the killing of health workers, destruction of health facilities, and widespread displacement of large populations, had a strong negative impact on polio programme activities.5
In response to the WPV1 outbreak in Nigeria, the WHO African Regional Office rapidly consulted with the ministers of health of Nigeria and its neighbours in the Lake Chad Basin—Cameroon, Central African Republic, Chad, and Niger. In August, 2016, ministers declared a subregional public health emergency, within the context of the broader humanitarian emergency response ongoing in parts of the region. In collaboration with the Global Polio Eradication Initiative partners, and under the leadership of each government in the five countries in the Lake Chad Basin, staff members from the Nigeria Polio Emergency Operations Centre planned and implemented a large-scale regional response. The response was linked to the Lake Chad Basin polio task team, comprising governments and Global Polio Eradication Initiative partners, which was established to strengthen collaboration in response to the outbreak.13
Political, military, traditional, and community leaders were engaged to ensure the success of the polio immunisation campaign in Africa. The response included supplementary immunisation activities in the five countries in the Lake Chad Basin, intensified surveillance for cases of acute flaccid paralysis, and enhanced environmental surveillance. To avoid further spread of WPV1, the geographical scope of the immunisation response was also expanded. Over 190 000 health-care workers and volunteers immunised more than 116 million children younger than 5 years in 13 countries over a 1 week period in March, 2017, in a coordinated effort in west and central Africa.14 Where security permitted, preventive supplementary immunisation activities were synchronised. In Nigeria, a National Emergency Routine Immunization Coordination Centre was established to strengthen routine immunisation coverage.15
As part of this effort, there was also expanded use of technologies for planning and monitoring supplementary immunisation activities and conducting surveillance, and an increase in surge capacity at subnational levels. To improve the timeliness, completeness, and quality of surveillance for acute flaccid paralysis, GPS-based tools with mobile phone technology were used in the highly security-compromised areas of Nigeria, Cameroon, Central African Republic, and South Sudan, and in the high-risk areas of the Mali, Burkino Faso, and Niger border triangle subregion; the other Lake Chad Basin countries of Chad and Niger; and eastern Ethiopia. Although started in 2012 on a small geographical scale in Kano, Nigeria, these measures were then expanded to most northern states in Nigeria by 2014, and then to other countries from 2014 onwards. The technology supported the monitoring and tracking of the movement of immunisation teams and the estimation of immunisation coverage, and included electronic surveillance; integrated supportive supervision, which facilitated active surveillance in health facilities in real time; and AVADAR (auto-visual acute flaccid paralysis detection and reporting)—an SMS-based smartphone application used by community informants in areas with weak health systems.16 Polio surveillance reviews and retrospective searches for missed cases of acute flaccid paralysis were done and enhanced environmental surveillance for polioviruses was implemented.5 Regular and rigorous supervision, evaluations, and reviews focusing on surveillance performance at subnational levels were also implemented.5
The planned decrease in the number of staff funded by the Polio Eradication Program in the five countries of the Lake Chad Basin was suspended by the Global Polio Eradication Initiative to ensure enough capacity in the group. The regional directors of the African region and UNICEF co-chaired quarterly meetings to monitor progress beginning in the first quarter of 2017. In September, 2016, Nigeria was reclassified as a country with endemic transmission of WPV1, indicating that this strain had been circulating undetected since 2011, and not previously eliminated.17
With respect to certification, in light of these events, an adjustment was made to the Regional Certification plan to receive the complete country documentation from Cameroon, Central African Republic, and Nigeria, placing them among the last of the remaining countries in the region to submit their documentation. As the complete country documentation had been accepted from Niger and Chad earlier in 2016, 4 years after the detection of the last case of wild poliovirus infection in these countries, annual country updates continued to be submitted and closely monitored.
In September, 2018, a framework for certification of interruption of wild poliovirus transmission in the African region was endorsed by the Regional Committee for Africa, comprising health ministers from the 47 countries in the region.13 The goal of the framework was to achieve polio-free certification of the region by the end of 2019 by strengthening surveillance for acute flaccid paralysis in all countries and functional environmental surveillance in selected countries, and by strengthening the national polio certification committees and documentation processes in all countries. The framework also provided a list of priority interventions and actions to sustain a polio-free region after certification of the interruption of wild poliovirus transmission. At that time, no wild poliovirus cases had been confirmed for 24 months, and 40 of 47 countries had their complete country documentation accepted by the Regional Commission (figure 2).
By late 2019, only four countries remained for which review of their complete country documentation was required—Cameroon, Central African Republic, Nigeria, and South Sudan. These countries constitute a continuous geographical area with surveillance and immunisation challenges resulting from insecurity and related lockdowns, inaccessibility, and hard-to-reach populations (nomadic populations, those living on islands and between water bodies, and those living in areas prone to flooding). From the last quarter of 2019 to the end of the first quarter of 2020, field verification visits were done by members of the Commission to each of these countries, usually in the presence of security or military personnel.
In Cameroon, the last case of WPV1 infection was detected in 2014 and, since 2016, the national rate of non-polio-related acute flaccid paralysis and proportion of acute flaccid paralysis cases with adequate stool samples remained above the required certification levels. In Central African Republic, the last case of WPV1 infection was detected in 2011, and core surveillance indicators had been satisfactory at both national and subnational levels with rates of non-polio-related acute flaccid paralysis exceeding the required level for certification since 2017. In South Sudan, the last case of WPV1 infection was detected in 2009, and the country has achieved and maintained core surveillance indicators above certification level since 2010. Environmental surveillance is operating in all three countries and no wild poliovirus has been detected.
In Nigeria, as of late 2019, over 3 years since WPV1 was last detected, surveillance indicators had consistently surpassed required certification standards at national and state levels since 2016. Additionally, 82% of local government areas met both core surveillance indicators annually. Throughout northern Nigeria, government officials and partners engaged traditional leaders and associations such as the Federation of Muslim Women's Associations in Nigeria,18 youth groups against polio,19 The Journalists Initiatives on Immunisation Against Polio,20 and groups of polio survivors, community health workers, and traditional birth attendants, who used their networks to advocate, engage, and sensitise communities to advance polio immunisation efforts. In Borno State, Nigeria, special surveillance and immunisation initiatives were introduced, including recruiting community informants residing in inaccessible areas who regularly report cases of acute flaccid paralysis and have ongoing contact with adjacent secured areas in which surveillance activities have been intensified; taking stool samples from contacts and healthy children residing in or escaping from inaccessible areas; and the creation of the Reaching Inaccessible Communities initiative, a partnership between the polio programme and the Nigerian military to improve the reach of immunisation and surveillance activities in areas truly inaccessible to the polio programme.21 Through the ongoing Reaching Inaccessible Communities initiative, and as of February, 2020, 57% of targeted settlements had been reached at least once, and 46% of those that are inhabited had been reached at least five times.22 Additionally, the Reaching Every Settlement initiative, which employs civilian teams accompanied by armed security to access partially accessible settlements monthly, had reached 99·6% of all target settlements at least once as of February, 2020.22
From September, 2016, to January, 2020, estimates of the number of children younger than 5 years living in settlements unreached by GPS-tracked immunisation activities in Borno State had decreased by 89% from approximately 434 000 being immunised to approximately 48 000.23 And in Borno State, largely due to the community informants residing in inaccessible areas, the number of children reached by surveillance activities exceeded those reached by immunisation.23
A pre-certification analysis was also done in 2020, with a focus on areas remaining to be certified, especially where security had hampered programmatic activities, to provide the Commission with more evidence that transmission of wild poliovirus had been interrupted in areas of greatest insecurity.23 The analyses included an expansion of previous work using satellite imagery to do a habitation analysis in Borno State;24 modelling to estimate the likelihood of undetected WPV1 transmission in Borno and Yobe States;25 and compilation and assessment of other data sources generated from non-traditional surveillance methods.23
Routine immunisation coverage
With respect to immunisation coverage, according to 2019 WHO–UNICEF estimates,26 17 countries had achieved three-dose bivalent oral poliovirus vaccine type 1 and type 3 coverage of at least 90% and 29 countries had achieved coverage of at least 80%. 13 countries had achieved inactivated poliovirus vaccine coverage of at least 90%, and 26 countries had achieved coverage of at least 80%.
Destruction or containment of wild poliovirus stocks
With respect to poliovirus containment, no country in the region, other than South Africa, plans to retain poliovirus infectious materials. Surveys of laboratories and other facilities have been done in all 47 countries as per Global Polio Eradication Initiative Global Action Plan III.27 Surveys and destruction of potentially infectious materials have been done in all countries except the Democratic Republic of the Congo, where there have been multiple competing emergencies. In South Africa, an initial Certificate of Participation was awarded in 2018 as per the global Containment Certification Scheme.28
Polio-free certification
On June 15–18, 2020, due to the COVID-19 pandemic, the 25th meeting of the Africa Regional Commission was held by video conference. The complete country documentation from the four remaining countries was presented to all participants by the chairs of the National Certification Committees and discussed during closed sessions. On June 18, 2020, the Africa Regional Commission agreed that sufficient information was provided to support the claims that Cameroon, Central African Republic, Nigeria, and South Sudan had interrupted transmission of all indigenous wild polioviruses, and the complete country documentation was accepted.
Discussion
Certification of the interruption of wild poliovirus transmission in the WHO African region has been a long and turbulent journey, hampered until 2016 by the spread of WPV1, largely due to chronic insecurity in northeastern Nigeria, the Lake Chad Basin, and localised areas of Africa. The importance of countries meeting the requirement of achieving certification-standard surveillance for a period of at least 3 years was illustrated by the need to reinstate Nigeria as a polio-endemic country 2 years after the last detected case of WPV1 infection and only 1 year after it was removed from the list of polio-endemic countries.
The assessment of country documentation was also supported by valuable field verification visits that enabled Africa Regional Commission members to determine political and programmatic commitment to polio elimination, country capacity to do required certification activities, and to make recommendations to the highest political levels on how they could be addressed. However, the assessment of whether high-quality surveillance and improvements in routine immunisation coverage were achieved posed an ongoing challenge, because the assessment of acute flaccid paralysis rates and immunisation coverage are dependent on adequate denominator data. The lack of recent censuses and substantial population mobility in many parts of sub-Saharan Africa made assessment extremely difficult.
In 1994, the WHO Region of the Americas was the first WHO region to certify the interruption of transmission of indigenous wild polioviruses,29 showing that eradication could be achieved with regional leadership, strong international partnerships, clear criteria and strategies, and country-level commitment to execution. This achievement paved the way for accelerating elimination efforts in the other WHO regions, and was followed by wild poliovirus-free certification of the WHO Western Pacific region (2000),30 European region (2002),31 and South-East Asia region (2014).32 Certification of the South-East Asia region reaffirmed the feasibility of elimination in areas where the risks of wild poliovirus transmission are highest—ie, locations with high population densities, large birth cohorts, high population mobility, and poor sanitation.33
Certification of the African region shows the feasibility of elimination in areas that are inaccessible because of chronic insecurity, with resultant movement of refugees and internally displaced populations, nomadic populations, and difficult terrain. It also shows that elimination is possible even in the presence of fragile health systems, in which large proportions of the population are unimmunised or children are under-immunised; vaccine refusal is high; management and resource risks are present; and multiple, competing, urgent priorities are present, including large communicable disease outbreaks, some of which have resulted in additional declarations of Public Health Emergencies of International Concern.34
These challenges were dealt with via sustained political leadership at regional, national, and subnational levels of government; country-level ownership of the Polio Eradication Program; strong and committed national and international partnerships; effective community engagement; focused attention to improve surveillance and routine immunisation; fearless and determined health-care workers; and innovation and ingenuity.
Success in the face of these enormous challenges is truly a monumental achievement. The sacrifices have been enormous; indeed, dozens of health-care workers and volunteers have lost their lives in the pursuit of a polio-free Africa.35 Success is also tempered by ongoing outbreaks caused by circulating vaccine-derived poliovirus type 2, a genetic variant of the oral poliovirus vaccine that can cause paralysis indistinguishable from that caused by wild polioviruses. The Global Certification Commission and Africa Regional Commission have expressed their concern about these outbreaks and have recommended activities and procedures that will be needed to verify elimination of these outbreaks. However, the interruption of wild poliovirus transmission in the African region will be recorded as one of the greatest achievements of the continent and a clear demonstration of what is possible through commitment and collaboration.
Acknowledgments
Acknowledgments
We thank the national polio committees in the 47 countries in the WHO African region; Koffi Kouadio, Mbaye Salla, and Sam Okiror, as current and past regional certification officers; and Eddy Sokolua, Daudi Manyanga, and Aïcha Diaketé, as certification focal points for central, east and southern, and west Africa, respectively, and their teams for their support of the certification process. We also thank Alex Gasasira, former regional surveillance and polio coordinator; Norbert Ngendabanyikwa, Fussum Daniel, and Ado Bwaka, as polio and immunisation focal points for central, east and southern, and west Africa, respectively; Ticha Johnson, as regional medical officer for polio surveillance, Keith Shaba, as regional polio data manager, Modjirom Ndoutabe, as Africa polio rapid response team coordinator; Nicksy Gumede and Francis Kasolo, as current and previous regional virologists; and Deo Nshimirimana, as former immunisation and polio eradication coordinator for the WHO African region, for their many contributions and support of the certification process. We also thank Francis K Nkrumah, Redda Tekle Haimanot, and Kusum J Nathoo, former member of the Africa Regional Commission. Finally, we thank the WHO Representatives in the countries of the African region for supporting the Africa Regional Commission advocacy and field verification visits. This Health Policy paper is dedicated to the many polio workers who lost their lives while carrying out their work. The contents of this Health Policy paper are solely the responsibility of the authors and do not necessarily represent the official views of the US Centers for Disease Control and Prevention (CDC) or the Department of Health and Human Services.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contributors
RGFL and AK conceived of the manuscript. AK led the writing, revision, and production of the manscript. RGFL, MAP, and RHT contributed to the writing and revision of the manuscript. RGFL and OT reviewed and contributed to the cited literature. All Commission members reviewed and endorsed the final manuscript. PM contributed to the writing and revision of the manuscript. All members of the Commission and PM contributed equally to the creation of the manuscript.
The Africa Regional Commission for the Certification of Poliomyelitis Eradication
Cameroon Rose Gana Fomban Leke (Chair); Burkino Faso B Jean Kaboré; Canada Arlene King; USA Mark A Pallansch; Nigeria Oyewale Tomori; The Gambia Abdoulie D Jack; Iran Bijan Sadrizadeh; Mauritania Ibrahima Kane; Uganda Naddumba Edward Kironde; Angola Raul Jorge Lopes-Feio; Thailand Supamit Chunsuttiwat; Mali Zakaria Maiga; Côte d'Ivoire Beugré Kouassi; South Africa Ngokoana Esther Khomo; Germany Rudolf H Tangermann; Tanzania William Bahati Pungu Matuja; Malawi Pascal Mkanda*.
*Coordinator of the Polio Eradication program for the WHO African region; not a member of the Commission but contributed to writing.
Declaration of interests
RGFL is the chair of the Africa Regional Commission for the Certification of Poliomyelitis Eradication. PM is the coordinator of the Polio Eradication Program in the African region. All other members of the Africa Regional Commission declare no competing interests.
Contributor Information
The Africa Regional Commission for the Certification of Poliomyelitis Eradication:
Rose Gana Fomban Leke, Arlene King, Mark A Pallansch, Rudolf H Tangermann, Pascal Mkanda, Supamit Chunsuttiwat, Abdoulie Jack, B Jean Kaboré, Ibrahima Kane, Ngokoana Esther Khomo, Raul Jorge Lopes-Feio, Zakaria Mahamadine Maiga, William Bahati Pungu Matuja, Naddumba Edward Kironde, Beugré Kouassi, Bijan Sadrizadeh, and Oyewale Tomori
References
- 1.Global Polio Eradication Initiative . World Health Organization; Geneva: August, 2020. This week: polio this week as of 19 August 2020.http://polioeradication.org/polio-today/polio-now/this-week [Google Scholar]
- 2.WHO . World Health Organization; Geneva: 2019. Global Polio Eradication Initiative investment case 2019–2023.http://polioeradication.org/wp-content/uploads/2019/08/Polio-InvestmentCase-Report-20190819.pdf [Google Scholar]
- 3.WHO . World Health Organization; Geneva: May 5, 2020. Poliomyelitis: polio eradication: report by the Director-General.https://apps.who.int/gb/ebwha/pdf_files/WHA73/A73_12-en.pdf [Google Scholar]
- 4.Adams A, Salisbury DM. Eradicating polio. Science. 2015;350:609. doi: 10.1126/science.aad7294. [DOI] [PubMed] [Google Scholar]
- 5.Nnadi C, Damisa E, Esapa L. Continued endemic wild poliovirus transmission in security-compromised areas—Nigeria, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:190. doi: 10.15585/mmwr.mm6607a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Expanded Programme on Immunization. Global Programme for Vaccines and Immunization . World Health Organization; Geneva: Feb 16–17, 1995. Report of the 1st meeting of the global commission for the certification of the eradication of poliomyelitis.http://polioeradication.org/wp-content/uploads/2016/07/10Report.pdf [Google Scholar]
- 7.Addis Declaration on Immunization Brazzaville: World Health Organization Regional Office for Africa. https://www.afro.who.int/health-topics/immunization/the-addis-declaration-immunization
- 8.WHO . World Health Organization; Geneva: 2018. Global Health Observatory data repository. Population data by WHO region.https://apps.who.int/gho/data/view.main.POP2020 [Google Scholar]
- 9.UN Economic Commission for Africa . Addis Ababa, Economic Commission for Africa; 2016. The demographic profile of African countries.https://www.uneca.org/sites/default/files/PublicationFiles/demographic_profile_rev_april_25.pdf [Google Scholar]
- 10.WHO WHO-recommended surveillance standards for poliomyelitis. Geneva: World Health Organization. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/poliomyelitis_standards/en/
- 11.Centers for Disease Control and Prevention Progress toward poliomyelitis eradication—Nigeria, January 2004-July 2005. MMWR Morb Mortal Wkly Rep. 2005;54:873–877. [PubMed] [Google Scholar]
- 12.WHO . World Health Organization; Geneva, New York, NY: Sept 25, 2015. WHO removes Nigeria from polio-endemic list.https://www.who.int/mediacentre/news/releases/2015/nigeria-polio/en/ [Google Scholar]
- 13.WHO Regional Office for Africa . World Health Organization Regional Office for Africa; Brazzaville: 2018. Sixty-eighth session of the WHO Regional Committee for Africa, Dakar, Republic of Senegal, 27–31 August 2018: final report.https://www.afro.who.int/sites/default/files/sessions/final-reports/AFR-RC68-17%20Report%20of%20the%20Regional%20%20Committee%20-%20Final-Web.pdf [Google Scholar]
- 14.WHO . World Health Organization; Geneva: March 23, 2017. From coast to coast: Africa unites to tackle threat of polio: joint new release UNICEF/WHO.https://www.who.int/news-room/detail/23-03-2017-from-coast-to-coast-africa-unites-to-tackle-threat-of-polio [Google Scholar]
- 15.Bristol N, Hussain I. Center for Strategic & International Studies; Washington, DC: July, 2018. Polio emergency operations centers.https://www.csis.org/features/polio-emergency-operations-centers [Google Scholar]
- 16.Shuaib FMB, Musa PF, Gashu ST. AVADAR (Auto-Visual AFP Detection and Reporting): demonstration of a novel SMS-based smartphone application to improve acute flaccid paralysis (AFP) surveillance in Nigeria. BMC Public Health. 2018;18(suppl 4) doi: 10.1186/s12889-018-6187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Polio Eradication Initiative . Global Polio Eradication Initiative; 2016. Polio this week as of 27 September 2016.https://reliefweb.int/sites/reliefweb.int/files/resources/Global%20Polio%20Eradication%20Initiative%20%3E%20Data%20and%20monitoring%20%3E%20Polio%20this%20week_8.pdf [Google Scholar]
- 18.Duru JI, Usman S, Adeosun O, Stamidis KV, Bologna L. Contributions of volunteer community mobilizers to polio eradication in Nigeria: the experiences of non-governmental and civil society organizations. Am J Trop Med Hyg. 2019;101(suppl 4):74–84. doi: 10.4269/ajtmh.19-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Musa A, Mkanda P, Manneh F. Youth group engagement in noncompliant communities during supplemental immunization activities in Kaduna, Nigeria, in 2014. J Infect Dis. 2016;213(suppl 3):S91–S95. doi: 10.1093/infdis/jiv510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warigon C, Mkanda P, Banda R. The Journalists Initiatives on Immunisation Against Polio and improved acceptance of the polio vaccine in northern Nigeria 2007–2015. J Infect Dis. 2016;213(suppl 3):s86–s90. doi: 10.1093/infdis/jiv545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bawa S, Shuaib F, Saidu M. Conduct of vaccination in hard-to-reach areas to address potential polio reservoir areas, 2014–2015. BMC Public Health. 2018;18(suppl 4) doi: 10.1186/s12889-018-6194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iliyasu Z. Nigeria's complete documentation for poliovirus-free status. 25th Meeting of the 2020 Africa Regional Commission for the Certification of Poliomyelitis Eradication (ARCC) Conference; virtual; June 15–18, 2020.
- 23.Higgins J, Kovacs S, Peak C, et al. Findings from the AFRO Pre-Certification Analysis Project. 25th Meeting of the 2020 Africa Regional Commission for the Certification of Poliomyelitis Eradication (ARCC) Conference; virtual; June 15–18, 2020.
- 24.Higgins J, Adamu U, Adewara K. Finding inhabited settlements and tracking vaccination progress: the application of satellite imagery analysis to guide the immunization response to confirmation of previously-undetected, ongoing endemic wild poliovirus transmission in Borno State, Nigeria. Int J Health Geogr. 2019;18:11. doi: 10.1186/s12942-019-0175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalkowska DA, Thompson KM. Modeling undetected live poliovirus circulation after apparent interruption of transmission: Borno and Yobe in northeast Nigeria. Risk Anal. 2020 doi: 10.1111/risa.13486. https://doi.org/10.111/risa.13486 published online April 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization; Geneva: July 15, 2020. WHO-UNICEF estimates of DTP3 coverage.https://apps.who.int/immunization_monitoring/globalsummary/timeseries/tswucoveragedtp3.html [Google Scholar]
- 27.WHO . World Health Organization; Geneva: 2015. WHO Global Action Plan to minimize poliovirus facility-associated risk after type-specific eradication of wild polioviruses and sequential cessation of oral polio vaccine use.http://polioeradication.org/wp-content/uploads/2016/12/GAPIII_2014.pdf [Google Scholar]
- 28.WHO . World Health Organization; Geneva: 2015. Containment certification scheme to support the WHO Global Action Plan for poliovirus containment.http://polioeradication.org/wp-content/uploads/2017/03/CCS_19022017-EN.pdf [Google Scholar]
- 29.Robbins FC, de Quadros CA. Certification of the eradication of indigenous transmission of wild poliovirus in the Americas. J Infect Dis. 1997;175(suppl 1):S281–S285. doi: 10.1093/infdis/175.supplement_1.s281. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention Certification of poliomyelitis eradication—Western Pacific Region, October 2000. MMWR Morb Mortal Wkly Rep. 2001;50:1–3. [PubMed] [Google Scholar]
- 31.WHO Certification of poliomyelitis eradication: European region, June 2002. Wkly Epidemiol Rec. 2002;77:221–223. [PubMed] [Google Scholar]
- 32.WHO Polio-free certification of the WHO South-East Asia region, March 2014. Wkly Epidemiol Rec. 2014;89:500–504. [PubMed] [Google Scholar]
- 33.Bahl S, Kumar R, Menabde N. Polio-free certification and lessons learned--South-East Asia region, March 2014. MMWR Morb Mortal Wkly Rep. 2014;63:941–946. [PMC free article] [PubMed] [Google Scholar]
- 34.WHO . third edn. World Health Organization; Geneva: 2008. International health regulations (2005) [Google Scholar]
- 35.Centers for Disease Control and Prevention Progress toward poliomyelitis eradication – Nigeria, January 2012-September 2013. MMWR Morb Mortal Wkly Rep. 2013;62:1009–1013. [PMC free article] [PubMed] [Google Scholar]