Abstract
The effects of psychoactive substance abuse are not limited to the user, but extend to the entire family system, with children of substance abusers being particularly at risk. This meta-analysis attempted to quantify the longitudinal relationship between parental alcohol, tobacco, and drug use and child well-being, investigating variation across a range of substance and well-being indices and other potential moderators. We performed a literature search of peer-reviewed, English language, longitudinal observational studies that reported outcomes for children aged 0 to 18 years. In total, 56 studies, yielding 220 dependent effect sizes, met inclusion criteria. A multilevel random-effects model revealed a statistically significant, small detriment to child well-being for parental substance abuse over time (r = .15). Moderator analyses demonstrated that the effect was more pronounced for parental drug use (r = .25), compared with alcohol use (r = .13), tobacco use (r = .13), and alcohol use disorder (r = .14). Results highlight a need for future studies that better capture the effect of parental psychoactive substance abuse on the full breadth of childhood well-being outcomes and to integrate substance abuse into models that specify the precise conditions under which parental behavior determines child well-being.
Registration: PROSPERO CRD42017076088
Keywords: alcohol, children, meta-analysis, parent, substance abuse, tobacco, well-being
The effects of psychoactive substance abuse are not limited to the user but extend to the entire family system and society at large. In line with the growing body of research on the detrimental influence of adverse childhood experiences, children of users are particularly at risk, with effects on their health, well-being, and their own use of tobacco, alcohol, or drugs (e.g., National Center on Addiction and Substance Abuse, 2005). Millions of children are likely to be affected by parental psychoactive substance abuse, as estimates suggest that 12.3% of US children aged 17 years or younger reside in a home with at least one parent with a substance abuse disorder (Lipari & Van Horn, 2017). In Europe, the estimates for children under the age of 20 years living with alcohol abusing parents varies greatly and ranges from 5.7% in Finland, 10.5% in Denmark, 15.4% in Germany, and 17% to 23% in Poland (European Monitoring Centre for Drugs and Drug Addiction, 2008).
A large body of evidence spanning several decades has documented that the children of parents who abuse alcohol, tobacco, and drugs (henceforth collectively referred to as parental substance abuse) are more likely to develop a variety of emotional, behavioral, physical, cognitive, academic, and social problems in the short and long run (e.g., Barnard & McKeganey, 2004; Straussner & Fewell, 2011). For example, passive tobacco exposure has been linked to somatic health problems in children and adolescents, together with an increased risk of children's own tobacco use initiation and dependence (Hussong et al., 2008). In addition, parental substance abuse has been linked to family breakdown, which is a key risk factor for children's poor mental health (Mallett, Rosenthal, & Keys, 2005; Størksen, Røysamb, Moum, & Tambs, 2005). It has also been linked to a reduction in the quality of the parent-child relationship and maladaptive relationship models that can be detrimental to the development of later peer relationships (Fearon, Bakermans, Kranenburg, Van Ijzendoorn, Lapsley, & Roisman, 2010; Hoeve et al., 2012).
Parental substance abuse has also been associated with a reduction in the extent that parents monitor their children, which may undermine parents’ ability to provide a safe and nurturing home environment (Barnard & McKeganey, 2004). Instability with respect to employment, family structure, housing, childcare, and household finances has also been shown to co-occur with parental substance abuse, with consequences that extend beyond the family environment to influence children's social functioning (Berger, Paxson, & Waldfogel, 2009; De Goede, Branje, Delsing, & Meeus, 2009; Giesbrecht, Cukier, & Steeves, 2010; Lander, Howsare, & Byrne, 2013; Martin, Razza, & Brooks-Gunn, 2012; Öberg, Jaakkola, Woodward, Peruga, & Prüss-Ustün, 2011; Parsons, Adler, & Kaczala, 1982).
There appears to be a general consensus amongst researchers, clinicians, and policy makers that parental substance abuse negatively affects child well-being (Bountress & Chassin, 2015; Hussong, Huang, Curran, Chassin, & Zucker, 2010; McGrath, Watson, & Chassin, 1999; Peterson et al., 2006; Puttler, Zucker, Fitzgerald, & Bingham, 1998; Rossow, Keating, Felix, & McCambridge, 2016). However, the extent and nature of this relationship is currently unknown, because findings in the literature vary considerably in magnitude and studies have typically focused on a subset of child well-being outcomes or a specific parental substance abuse type. Furthermore, there is considerable variation in the way that parental substance abuse and child well-being outcomes have each been operationalized. A systematic synthesis of the available evidence using an overarching framework is needed to quantify the extent to which parental substance abuse predicts detrimental child well-being outcomes over time in order to draw more general conclusions and to determine the degree of heterogeneity in this relationship while also identifying factors that could explain any inconsistencies. In doing so, it would also be possible to identify gaps in the research literature and key directions for future research.
The present meta-analysis
To address these important knowledge gaps, we conducted a systematic review and meta-analysis of the longitudinal relationship between parental psychoactive substance abuse and child well-being that included multiple substance abuse types and well-being domains. We focused on longitudinal studies, as this provides insight into the directionality of any effect and the long-term characteristics of any association. We used a state-of-the-art multilevel meta-analytic approach that allowed us to model the dependency among effect sizes, which is common in primary studies, in part because they include multiple outcome measures and multiple informants, or they report on multiple family members. Given the broad and comprehensive nature of this meta-analysis, heterogeneity within the results was expected. Therefore, the following study and sample characteristics that could potentially moderate the strength of the relationship between substance abuse and well-being were examined.
Parental substance abuse refers to the consumption of psychoactive substances, including licit and illicit substances, of which alcohol (Rossow et al., 2016) and tobacco (Saulyte, Regueira, Montes-Martínez, Khudyakov, & Takkouche, 2014) are the most frequently used. Given differences in the legal and social status, addictive potential, and cognitive effects, the effect on family members has been proposed to vary according to the particular substance consumed (Straussner, 1994; Straussner & Fewell, 2011). Apart from the different types, the use of such substances have commonly been considered to range on a continuum from recreational use to chronic dependence (Straussner, 2004). Substance dependence may vary in severity from mild to severe and refers to compulsive and continued use irrespective of any adverse consequences. We hypothesised that the association with child well-being would be less pronounced for the use of licit substances of a recreational nature.
Well-being is a nebulous term that is informed by personal, cultural, and other factors (Diener, Oishi, & Lucas, 2003), and there is no clear distinction between well-being and quality of life or mental health problems (Siddaway, Taylor, & Wood, 2018; Siddaway, Wood, & Taylor, 2017). Well-being is typically considered a multidimensional construct (Gallagher, Lopez, & Preacher, 2009; Keyes, 2009; Ryff & Keyes, 1995) that includes both subjective and objective features (Newman, Tay, & Diener, 2014) and, for young people, can refer to domains as disparate as relationships, health, activities, finance, education, and skills (Bradshaw, 2016). Because existing research has largely focused on a specific well-being domain, a comprehensive examination of whether and how well-being subtype moderates the substance abuse–well-being relationship is currently lacking. We sought to address this gap by conceptualizing child well-being as a broad, multidimensional construct that involves physical, psychological, cognitive, social, and economic subdomains. This broad conceptualization is similar to the World Health Organization's (WHO, 2004, p. 10) definition of mental and physical health (“a state of complete physical, mental and social well-being”).
Although parental substance abuse can be detrimental at any point in a child's life, it is feasible that its effects could vary according to the age of the child. For example, parental tobacco use in a child's first year of life has been associated with a greater risk of physical health symptoms (Mitchell et al., 2012). For substance abuse, it has been argued that, compared with younger children, adolescents are at greater risk due to more prolonged exposure to parental substance abuse (Straussner & Fewell, 2011). We therefore examined whether effects differed according to the age of the child.
Although substance abuse by the mother and the father are both important, previous research has often found more pronounced associations with multiple adverse child outcomes for maternal substance abuse (Mitchell et al., 2012; Straussner & Fewell, 2011). These gender differences may be due to children spending more time in the presence of their mothers than their fathers, as mothers traditionally take a more active role in child rearing. It is also possible that parental substance abuse effects may manifest differently in boys and girls. For example, associations between parental smoke exposure and child mental health outcomes have been found to be more apparent for boys (Bandiera, Richardson, Lee, He, & Merikangas, 2011). Given previous findings on gender differences, we examined whether the gender of parent and child moderates the substance abuse–well-being relationship.
The choice of informants in behavioral research has been a subject of a long-lasting debate. For many measures of child functioning and parenting behavior, inter-informant agreement is low-to-moderate because parent and child reports are often discrepant (De Los Reyes et al., 2015; Kuppens, Grietens, Onghena, & Michiels, 2009b). Similarly, for licit and illicit substances, there is variation in prevalence by data collection mode (Beck, Guignard, & Legleye, 2014). Such inconsistent research findings may reflect method bias related to the specific informant or data collection mode (e.g., socially desirable responding, shared method variance; Kuppens, Grietens, Onghena, & Michiels, 2009a; Podsakoff, MacKenzie, Lee, & Podsakoff, 2003; |Tourangeau & Yan, 2007). As the potential method effect remains unexplored for the parental substance abuse–child well-being relationship, we examined the moderating role of informant and data collection mode.
Finally, the interval adopted in longitudinal studies can vary considerably, which in turn may influence the strength of the relationship between substance abuse and well-being over time for several reasons (Collins & Horn, 1991). The strength of the relationship could potentially decrease over time, as there is increasing opportunity for other cognitive, biological, and environmental variables to exert an effect. In addition, respondents may more easily remember their answers to a previous assessment when the time interval is shorter. We hypothesized that longitudinal relationships would be less pronounced as the time interval between parental substance abuse exposure and assessment of child well-being outcomes increased.
Method
This meta-analysis was conducted in accordance with guidelines for conducting a systematic review (Siddaway, Wood, & Hedges, 2019), the Preferred Reporting Items for Systematic Reviews and Meta-analyses (Moher, Liberati, Tetzlaff, Altman, & The PRISMA Group, 2009) and Meta-Analysis of Observational Studies in Epidemiology (Stroup et al., 2000) standards.
Literature search
Four electronic databases (PubMed, Medline, Embase, PsychInfo) were searched from inception to June 26, 2017. In addition, reference lists from eligible publications and relevant reviews were hand-searched. Comprehensive search strategies were developed by combining key and index terms covering the concepts of parental substance abuse AND child well-being (or related terms, see Supplement).
Inclusion and exclusion criteria
Peer-reviewed, English language, longitudinal observational studies (Morrison et al., 2012) were eligible for inclusion. Studies were required to include at least one association over time between a measure of parental substance abuse (measured at Time 1) and well-being (measured at Time 2) for children aged 18 years or younger. As previous research revealed polysubstance abuse in parental substance abuse (Hussong et al., 2008; Straussner & Fewell, 2011), we included recreational and disordered (including clinically defined dependence) alcohol, tobacco, and drug use. We included studies reporting comorbid substance use, as this is frequently observed in dependent users and excluding such groups might bias results towards being more conservative and less generalizable to the general population.
We operationalized child well-being broadly according to five distinct domains, in-keeping with a narrative literature review of how well-being can be conceptualized (Pollard & Lee, 2003), and in order to achieve a comprehensive overview of subjective and objective well-being of children, namely, (a) physical (including overall health and risks to health); (b) psychological (including emotional and mental states of mind); (c) cognitive (including capacity for learning and recall, academic achievement, and learning disability); (d) social (including social relationships and behaviors and anti-social behavior); and (e) economic (whether outside financial support is required) well-being. As we attempted to provide estimates of the association in the general population, studies were excluded if they were sampled from specific groups experiencing conditions that were likely to significantly affect associations between parental substance abuse and child well-being (e.g., detained adolescents, parents diagnosed with HIV). One author (V.G.) screened titles and abstracts, and S.M. rechecked extraction methods. Two authors (V.G. and S.M.) screened full text articles for inclusion, N = 381, kappa = .93, 95% CI [.92, .99]. References were exported and managed with Endnote X7.
Coding
To capture as much variation in substance abuse type, effect sizes were categorized into “Alcohol,” “Alcohol Use Disorder,” “Drugs,” “Drug Use Disorder,” “Tobacco,” and a non-descript category, “Any substance.” We used “Use Disorder” to identify parents whose use of substances was clinically significant and recorded using a clinically validated instrument. Child well-being was coded according to the aforementioned five domains, namely physical, psychological, social, cognitive, or economic well-being.
Several other study and outcome characteristics were extracted from each study: year; country from which the sample was drawn; sample size; retention rate; sample type (general population or specific subpopulation such as school children); parent and child gender, child age (0–5, 6–11, or 12–18 years); data collection mode for child and parent variables (interview, questionnaire); measurement instrument (standardized diagnostic, validated but nondiagnostic, or unstandardized); informant (parent, child, or teacher report); and follow-up duration (number of data collection points and the time in months between first and last assessment).
Data analysis
Effect size calculations
Pearson correlations (r) were computed to represent associations such that a positive correlation denoted that higher levels of parental substance abuse were associated with lower child well-being over time. Results reported in another metric were transformed to r whenever possible (Wilson, 2017). Study authors were contacted for additional information when an effect size or data to construct an effect size were not reported. Before pooling effect sizes, the correlations were transformed using Fisher's Zr transformation (Rosenthal, 1991). Pooled Zr expressions were transformed back to r expressions for reporting.
Meta-analytic integration
As most studies (71%) reported more than one relevant effect size, the independence assumption that underlies traditional meta-analysis was violated. Common approaches to addressing such dependency include choosing only one effect size from many or averaging across effect sizes within studies. Although such approaches allow one to adopt traditional meta-analytic techniques, they also result in a loss of information, rule out critical analyses of within-study moderators (e.g., well-being outcome differences), and may distort meta-analytic results (e.g., Cheung & Chan, 2004). We therefore employed a multilevel random-effects meta-analysis that permitted incorporating all of the relevant effect sizes from each study, while accounting for dependency among these effect sizes with SAS PROC HPMIXED (Littell, Milliken, Stroup, Wolfinger, & Schabenberger, 2006; Van den Noortgate, Lopez-Lopez, Marin-Martinez, & Sanchez-Meca, 2013).
The meta-analysis was implemented as a three-level model that models sampling variation for each effect size (Level 1), within-study variation (Level 2), and between-study variation (Level 3) (Van den Noortgate et al., 2013). We first computed an overall estimate of the longitudinal association between parental substance abuse and child well-being in a random-effects model. Between-study heterogeneity was reflected by the between-study variance (Level 3, representing differences between studies), but the three-level model also yielded an estimate of the within-study variance (Level 2, representing differences between effect sizes within studies). A likelihood ratio test was used to test the variation in effect sizes between and within studies, while the ratio of the variance at each level and the total variance was computed to reflect the amount of variance situated between and within studies. Subsequently, six substantive (study region, child age, child gender, parent gender, parental consumption type, child well-being type) and six methodological moderators were examined with grand-mean centering applied to continuous moderators. Separate mixed-effects models were fitted for each moderator variable to avoid inflating Type II error (Raudenbush & Bryk, 2002), and subgroup analyses were only conducted when data from at least four studies were available (Fu et al., 2011).
Risk of bias
In the absence of a standard risk of bias tool for longitudinal observational studies (see Siddaway et al., 2019), six criteria were adopted to reflect the methodological rigor of each study (Faragher, Cass, & Cooper, 2005; Higgins & Green, 2011; Wong, Cheung, & Hart, 2008): whether the study sample size provided adequate statistical power (calculated as at least N = 193 to provide a power of .80 in order to detect r = .20 with α = .05), retention rate, representativeness of the sample, standardized assessment tool for parental substance abuse, standardized assessment tool for child well-being, and whether associations were adjusted for confounding. We tested whether effect sizes differed according to the separate criteria.
Three strategies were used to assess publication bias. First, a funnel plot was created to visually search for evidence of bias, which would be apparent in an asymmetrical plot. Next, asymmetry was assessed using Egger's weighted regression test (Egger, Smith, Schneider, & Minder, 1997; Torgerson, 2006). Third, a sensitivity analysis was performed, which applies different a priori weight functions to correct the population effect size estimate for different types and severities of potential publication bias (Vevea & Woods, 2005). A mean study effect size was used in the publication bias analyses because independence is assumed in these methods and it is not yet possible to account for effect size dependency in these tests.
Results
Study characteristics
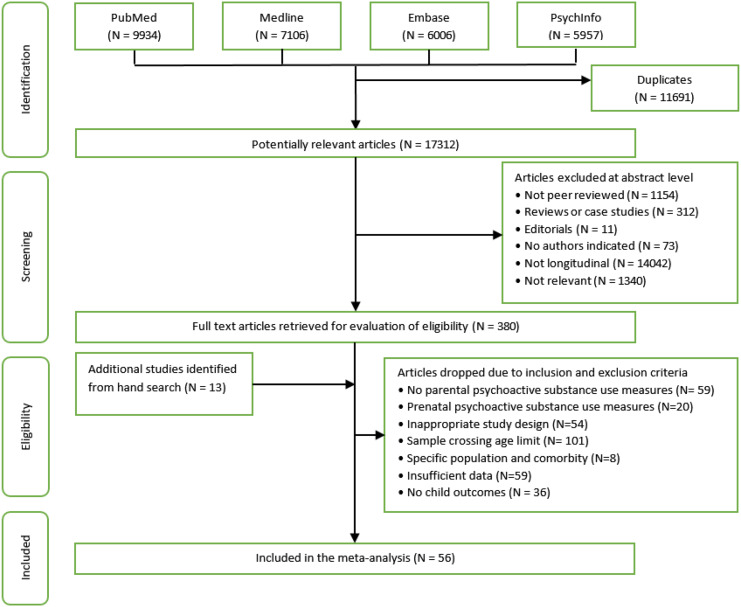
The meta-analysis included 56 studies and 220 effect sizes. A flow diagram of study identification and selection is presented in Figure 1. All 56 studies explicitly stated or used terminology implying that children and parents cohabited. Sample sizes varied from 83 to 49,5. Most studies drew samples from a general (34%) or school (27%) population; the remaining studies sampled from clinically dependent parents (22%) or used a specific sampling frame (e.g., 16% of families living in rural areas). Most studies (n =35) were conducted in North America, followed by Europe (n = 9), Australasia (n = 9), Asia (n = 2), and South America (n = 1).
Figure 1.
Flow diagram of study identification and selection, including reasons for exclusion.
Drug use was variously defined and predominantly included cannabis use. Most of the effect sizes (78%) examined outcomes in young people aged 12 to 18 years and on average included 45% female children. For parental consumption, 37% and 27% of reported effect sizes referred to maternal and paternal behavior, respectively, and 36% reported on the consumption for both parents combined. Effect sizes were evenly split across alcohol (38%) and tobacco (32%) use; drug use and alcohol use disorder were assessed in 6% and 19% of the effect sizes, respectively. The remaining effect sizes (5%) considered “any substance abuse.” No studies considered prescription medication. Information on parental substance abuse was mainly retrieved directly from parents (72%) or their children (25%). Most child well-being effect sizes concerned physical (74%) or psychological (19%) well-being, while social, cognitive, and economic well-being were assessed less frequently (7%). Well-being was mainly child (76%) or parent reported (15%). Time between parental substance abuse measurement and child well-being outcome averaged 60.26 months across all effect sizes (SD = 47.90, range = 3–190 months). Table 1 presents descriptive and mean effects sizes for the 56 included studies.
Table 1.
Descriptives and mean effect size for studies included in the meta-analysis (N = 56).
| Study | Country | Child age (years) | Gender child (% female) | Gender parents | Parental consumption | Child Well-being |
Informant (parental consumption) | Informant (child well-being) | Method of assessment | Time lag (months) | Mean N | Mean r |
Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adalbjarnardottir & Rafnsson, 2002 | Iceland | 12–18 | 54% | B | T, A | Tobacco, Alcohol | Child | Self-report | Q | 36 | 928 | .10 | .03 | .17 |
| Barman, et al., 2004 | Finland | 12–18 | 50% | MF | T | Tobacco | Self-report | Self-report | Q | 36 | 4739 | .20 | .13 | .27 |
| Barnow, et al., 2007 | USA | 12–18 | 48% | B | A | Behavioral problems | Self-report | Parent | I | 60 | 83 | .06 | −.15 | .26 |
| Bor, McGee, & Fagan, 2004 | Australia | 12–18 | 48% | M | T | Antisocial behavior | Self-report | Mother | Q | 168 | 5278 | .09 | −.10 | .28 |
| Brook, et al., 2001 | Colombia | 12–18 | 49% | MF | T, D | Drug use | Self-report | Self-report | I | 24 | 1374 | .12 | .02 | .21 |
| Bufferd et al., 2014 | USA | 6–11 | 46% | B | DD | Depression | Self-report | Self-report | I | 36 | 456 | .15 | .00 | .29 |
| Burke, et al., 2001 | Australia | 12–18 | 53% | MF | A | Alcohol | Self-report | Self-report | Q | 798 | .26 | .15 | .37 | |
| Chaffin, et al., 1996 | USA | missing | 43% | B | A | Physical abuse, Neglect | Self-report | Parents | I | 12 | 7103 | .30 | .17 | .41 |
| Colder, et al., 1997 | USA | 12–18 | 43% | MF | AD | Heavy alcohol use | Self-report | Self-report | Q | 36 | 428 | .17 | .02 | .31 |
| Connolly, et al., 1992 | USA | 12–18 | missing | M | A | Behavior problems | Self-report | Self-report, Teacher | I | 48 | 652 | .05 | −.09 | .19 |
| Crandall, et al., 2006 | USA | 0–5 | 0% | M | A | Head injury | Self-report | Mother | I | 12 | 3808 | .21 | .02 | .38 |
| Cranford, et al., 2010) | USA | 12–18 | 31% | MF | AD | Alcohol | Self-report | Self-report | I | 72 | 148 | .21 | .12 | .29 |
| Dwyer, et al., 1999 | Tasmania | 0–5 | 49% | MF | T | Sudden Infant Death Syndrome | Self-report | Parent | I | 3 | 9788 | .26 | .19 | .32 |
| Eiden, et al., 2007 | USA | 0–5 | 48% | B | A | Externalizing behavior | Self-report | Mother, Father, Teacher | I | 48 | 227 | .03 | −.06 | .13 |
| Ellickson, et al., 2001 | USA | 12–18 | missing | B | A | Problem Alcohol | Self-report | Self-report | Q | 60 | 4283 | .04 | −.16 | .22 |
| Fergusson, et al., 1993 | New Zealand | 12–18 | missing | M | T | Conduct disorder, Attention deficit, Total disruptive behavior | Self-report | Mother, Teacher | Q | 84 | 960 | .16 | .07 | .23 |
| Fergusson, et al., 1994 | New Zealand | 12–18 | missing | B | D | Multiple problem behaviors | Self-report | Self-report | Q | 48 | 942 | .07 | −.13 | .26 |
| Fergusson, et al., 1996 | New Zealand | 12–18 | missing | B | T | Depression, Nicotine dependence | Self-report | Self-report | Q | 48 | 942 | .10 | −.04 | .24 |
| Frank et al., 2014 | USA | 12–18 | 0% | B | D | Drug use | Other | Self-report | I | 180 | 157 | .34 | .11 | .54 |
| Fuller et al., 2003 | USA | 6–11 | 53% | B | AD | Aggression | Self-report | Parent | Q | 36 | 186 | .15 | −.09 | .37 |
| Griesler, et al., 2011 | USA | 12–18 | 63% | B | T | Nicotine dependence | Self-report | Self-report | I | 24 | 814 | .15 | −.05 | .34 |
| Gritz et al., 2003 | USA | 12–18 | missing | B | T | Tobacco | Self-report | Self-report | Q | 12 | 659 | .11 | −.10 | .30 |
| Hanewinkel et al., 2014 | Germany | 12–18 | 57% | B | A | Alcohol | Self-report | Q | 12 | 13642 | .11 | −.03 | .24 | |
| Heron et al., 2013 | UK | 12–18 | 51% | M | A, T, D | Problematic drug use, Non-problematic drug use | Self-report | Self-report | Q | 190 | 4159 | .25 | .18 | .32 |
| Hoffmann & Cerbone, 2002 | USA | 12–18 | Mixed/ boys only/ girls only | B | DD | Drug abuse, Alcohol abuse | Self-report | Self-report | I | 96 | 804 | .25 | .11 | .38 |
| Hussong & Chassin, 1997 | USA | 12–18 | 51% | B | AD | Heavy alcohol use | Self-report | Self-report | I | 36 | 293 | .08 | −.05 | .20 |
| Johnson & Leff, 1999 | USA | 0–5 | 51% | B | T | IQ | Self-report | Self-report | I | 48 | 122 | .03 | −.23 | .28 |
| Kaplow, et al., 2002 | USA | 12–18 | 51% | B | D | Drug use | Self-report | Self-report | I | 84 | 295 | .24 | .02 | .43 |
| Knudsen, et al., 2015 | Norway | 0–5 | 52% | M | A | Externalising & Internalising behavior problems | Self-report | Mother | Q | 18 | 49553 | .38 | .26 | .49 |
| Korhonen et al., 2008 | Finland | 12–18 | 61% | MF | A, T | Drug use | Self-report | Self-report | Q | 72 | 4138 | .14 | .08 | .21 |
| Kotch et al., 2014 | USA | 12–18 | 49% | B | T | Externalising behavior problems | Self-report | Self-report | I | 72 | 915 | .10 | −.10 | .29 |
| Lessard et al., 2014 | USA | 12–18 | 52% | MF | T, D, AD | E-cigarette use | Self-report | Self-report | Q | 48 | 136 | .10 | −.01 | .21 |
| Li, et al., 2002 | USA | 6–11 | missing | B | A, T, D, A | Alcohol, Tobacco, Drug use, Any substance use | Self-report | Self-report | Q | 1551 | .14 | .09 | .19 | |
| Lindsey et al., 2008 | USA | 6–11 | 0% | missing | A | Externalising & Internalising behavior problems | Self-report | Self-report | I | 48 | 514 | .15 | .01 | .29 |
| Loukas, et al., 2001 | USA | 6–11 | 52% | B | AD | Externalising behavior | Self-report | Parent | I | 36 | 208 | .27 | .04 | .47 |
| Malone, et al., 2002 | USA | 12–18 | missing | F | AD | Any substance disorder, Alcohol disorder, Drug diagnosis, Nicotine dependence, Conduct disorder, Oppositional defiant disorder, ADHD, Depression, Any disruptive disorder | Self-report | Self-report | I | 36 | 1020 | .19 | .13 | .25 |
| McGrath, et al., 1999 | USA | 12–18 | 49% | B | AD | Academic achievement | Self-report | Self-report, Teacher | I | 24 | 454 | .13 | .03 | .22 |
| Miller, 2001 | USA | 6–11 | 57% | M | T | Asthma | Self-report | Mother, Other | Q (parents), Other (children) | 36 | 3938 | .08 | −.05 | .21 |
| Morgenstern, et al., 2013 | Germany | 12–18 | missing | B | T | Tobacco, School performance | Self-report | Self-report | Q | 36 | 1320 | .12 | .03 | .21 |
| Naicker, et al., 2012 | Canada | 12–18 | 27% | B | A | Emotional disorder | Self-report | Self-report | Q | 937 | .10 | −.10 | .29 | |
| Nigg et al., 2006 | USA | 12–18 | missing | MF | AD | ADHD, Response inhibition, Set shifting and working memory, Conduct symptoms, IQ | Self-report | Self-report, Teacher | I | 180 | 498 | .06 | .00 | .13 |
| Pagani, et al., 2016 | Canada | 6–11 | 57% | M | T | Being overweight/obese | Self-report | Other | I (parents), Other (children) | 36 | 1323 | .14 | .00 | .27 |
| Power, et al., 2005 | USA | 12–18 | missing | F | A | Alcohol | Self-report | Self-report | Q | 6 | 743 | .00 | −.20 | .20 |
| Roosa, et al., 1990 | USA | 12–18 | missing | B | AD | Anxiety, Depression | Child | Self-report | Q | 3 | 145 | .30 | .13 | .45 |
| Selya, et al., 2012 | USA | 12–18 | 57% | MF | T | Tobacco | Self-report, Child | Self-report | Q | 42 | 1092 | .20 | .06 | .33 |
| Shortt, et al., 2007 | Australia | 12–18 | missing | B | A, T | Alcohol | Self-report | Self-report | Q | 12 | 1166 | .13 | −.01 | .26 |
| Thacher et al., 2016 | Sweden | 12–18 | Girls/ boys analysed separately | MFB | T | Allergies | Child, Spouse | Parents | Q | 144 | 3316 | .06 | −.02 | .13 |
| Thompson & Wilsnack, 1987 | USA | missing | 0% | MF | A | Alcohol | Child | Self-report | Q | 48 | 712 | .09 | .06 | .13 |
| Ting, et al., 2015 | Taiwan | 12–18 | 0% | B | A | Alcohol | Self-report | Self-report | Q | 48 | 496 | .13 | −.02 | .27 |
| Tjora, et al., 2011 | Norway | 12–18 | 54% | MF | T | Alcohol | Self-report | Self-report | Q | 60 | 1052 | .18 | .04 | .31 |
| Unger et al., 2006 | USA | 6–11 | 53% | B | T | Tobacco | Self-report | Q | 12 | 1940 | .10 | −.10 | .29 | |
| Van Der Vorst et al., 2013 | Canada | 12–18 | 48% | B | A | Alcohol | Child | Self-report | Q | 12 | 1142 | .14 | −.06 | .33 |
| Vella, et al., 2015 | Australian | 12–18 | 53% | M | T | Health-related Quality of Life | Self-report | Self-report | I | 120 | 2785 | .25 | .12 | .38 |
| Windham et al., 2004 | USA | 0–5 | 29% | M | A, D | Physical abuse, Self-esteem | Self-report | Self-report | I | 541 | .09 | −.02 | .19 | |
| Wong, et al., 2011 | USA | 12–18 | 47% | MF | AD | Suicidal thoughts, Self-harm | Self-report | Self-report | I | 96 | 392 | .02 | −.10 | .15 |
| Xie, et al., 2013 | China | 12–18 | missing | B | T | Tobacco | Child | Self-report | Q | 3572 | .08 | −.03 | .19 |
Note. N = average sample size available for analyses; Gender parents: M = mother, F = father, C = child, MF = mother and father separately, MFB = both parents included but not reported on separately; Parental consumption: T = tobacco, A = alcohol, D = drug use, DD = drug use disorder, AD = alcohol use disorder, A = any substance use; Method of assessment: I = interview, Q = Questionnaire.
Parental substance abuse and child well-being
The three-level random-effects meta-analysis yielded a statistically significant, small association between parental substance abuse and child well-being (r = .15), indicating that parental substance abuse was associated with poorer child well-being levels over time. Effect sizes differed significantly both between,  = .003; χ2(1) = 17.26, p < .001, and within,
= .003; χ2(1) = 17.26, p < .001, and within,  = .009; χ2 (1) = 14,804.78, p < .001, studies; 21% of the total variance was attributable to differences between studies, and 64% of the total variance was due to differences within studies.
= .009; χ2 (1) = 14,804.78, p < .001, studies; 21% of the total variance was attributable to differences between studies, and 64% of the total variance was due to differences within studies.
Moderator analyses
Table 2 presents the results for substantive and methodological moderators. Parental “drug use disorder” (n = 2), “any substance abuse” (n = 2), “social” (n = 1) and “economic” (n = 0) child well-being subgroups were excluded from moderator analyses due to an insufficient number of studies. Significant differences were found across parental substance abuse type, with pairwise comparisons revealing that the mean association was significantly stronger for parental drug use compared to alcohol use, t (205) = 3.75, p < .001, tobacco use, t (205) = 3.66, p < .001, and alcohol use disorder, t (205) = 2.83, p = .005. Other pairwise differences were not statistically different. Adding the parental substance abuse type moderator and the child well-being domain moderator explained 8.6% of the within-study variance. We did not find significant effects for the other substantive or methodological moderators. For substances other than tobacco or alcohol, cannabis was specifically identified in 71% of the drug-related category (k studies = 5; n (effect sizes) = 10). Sensitivity analysis yielded a significant effect of parental cannabis use on child well-being (r = .23, 95% CI [.14, .32], p < .001).
Table 2.
Results of the three-level meta-analysis models
| k studies | n | Effect Size | Test Statistic | ||
|---|---|---|---|---|---|
| r | 95% CI | ||||
| Random-effects model | |||||
| Overall effect size | 56 | 220 | .15 | [.12, .17] | t(219) = 12.94, p < .001 |
| Mixed-effects models Substantive Moderators | |||||
| Region | F(2, 208) = 1.01, p = .365 | ||||
| North America | 35 | 138 | .13 | [.10, .16] | |
| Europe | 9 | 46 | .16 | [.12, .21] | |
| Australasia | 9 | 27 | .17 | [.12, .22] | |
| Age of child | F(2, 215) = 0.62, p = .541 | ||||
| 0 to 5 years | 6 | 22 | .18 | [.11, .24] | |
| 6 to 11 years | 8 | 25 | .14 | [.08, .20] | |
| 12 to 18 years | 41 | 171 | .14 | [.11, .16] | |
| Gender of child (% female) | 41 | 181 | t(179) = -0.16, p = .873 | ||
| Gender of parent | F(2, 217) = 0.86, p = .426 | ||||
| Father | 25 | 82 | .16 | [.13, .19] | |
| Mother | 16 | 59 | .14 | [.10, .18] | |
| Both | 31 | 79 | .13 | [.10, .17] | |
| Parental substance abuse | F(3, 205) = 50.15, p = .002 | ||||
| Alcohola | 21 | 83 | .13 | [.09, .16] | |
| Tobaccob | 25 | 70 | .13 | [.10, .16] | |
| Drug usea,b,c,d | 8 | 14 | .25 | [.19, .31] | |
| Alcohol use disorderc | 11 | 42 | .14 | [.09, .19] | |
| Child well-being dimension | F(2, 214) = 20.65, p = .073 | ||||
| Physical | 38 | 162 | .15 | [.12, .17] | |
| Psychological | 16 | 42 | .15 | [.11, .19] | |
| Cognitive | 4 | 13 | .06 | [-.02, .14] | |
| Methodological Moderators | |||||
| Informant on parental substance abuse | t(212) = -10.08, p = .280 | ||||
| Parent self-report | 47 | 159 | .15 | [.13, .18] | |
| Child report | 7 | 55 | .12 | [.06, .17] | |
| Informant on child well-being | F(2, 203) = 10.53, p = .220 | ||||
| Child self-report | 42 | 166 | .13 | [.11, .16] | |
| Parent report | 12 | 33 | .17 | [.12, .22] | |
| Teacher report | 4 | 7 | .10 | [.02, .19] | |
| Shared informant | t(218) = 10.34, p = .182 | ||||
| Not shared | 44 | 142 | .14 | [.11, .16] | |
| Shared | 17 | 78 | .17 | [.13, .21] | |
| Mode parental substance abuse | t(169) = -0.29, p =.770 | ||||
| Interview | 24 | 83 | .15 | [.12, .18] | |
| Questionnaire | 27 | 88 | .14 | [.11, .18] | |
| Mode child well-being | t(174) = 0.02, p = .998 | ||||
| Interview | 17 | 57 | .14 | [.11, .18] | |
| Questionnaire | 26 | 119 | .14 | [.11, .17] | |
| Time lag association (months) | 51 | 195 | t(193) = -0.43, p = .667 | ||
Note. Some moderators were missing for certain studies. Each study can contribute multiple effect sizes, thus study sample size across subgroups can exceed the total study sample size for the Level 2 moderators. Within each moderator having more than two subgroups, identical letter superscripts indicate significant (p < .05) pairwise comparisons between subgroups.
Risk of bias
Three-level mixed-effect models did not reveal a statistically significant effect on the parental substance abuse–child well-being association for the methodological moderators: power, t (218) = 0.97, p = .332; retention rate, t (159) = 0.06, p = .952; sample representativeness, t (122) = -1.92, p = .058; properties of the parental substance use assessment tool, t (212) = 0.11, p = .913; properties of the child well-being assessment tool, F (2, 215) = 0.17, p = .844); or adjustment for confounding, t (218) = 0.96, p =.336.
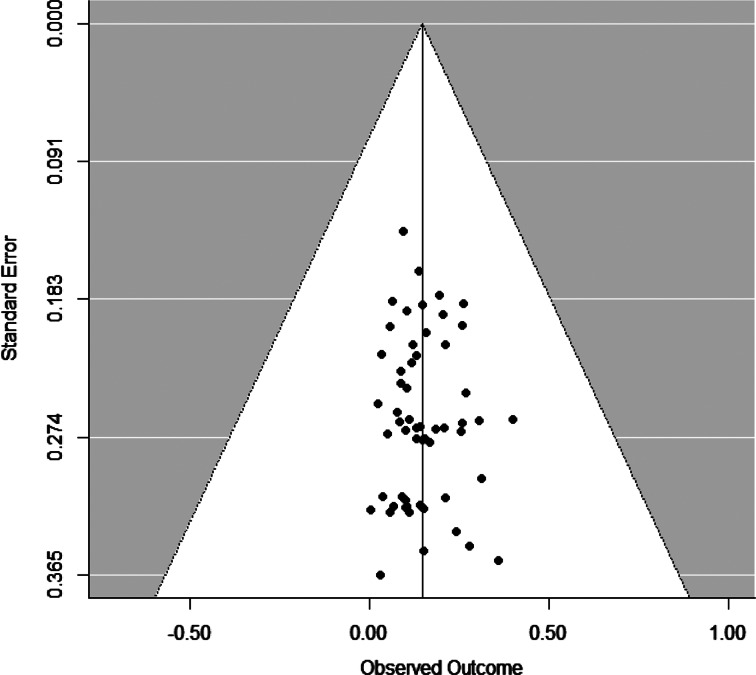
The funnel plot was funnel-shaped (Figure 2), and Egger's method found no statistically significant asymmetry, t (54) = 0.44, p = .664, suggesting no indication of publication bias. The sensitivity analyses corroborated these findings. Analyses revealed that the adjusted (r = .14) and unadjusted (r = .15) population effect size estimates were almost identical under different a priori weight functions. Overall, these analyses indicate that it is highly unlikely that publication bias influenced the meta-analytic results.
Figure 2.
Funnel plot for study-level mean effect sizes.
Discussion
We conducted a meta-analysis to examine the association between various indices of parental substance abuse and child well-being over time. A total of 56 studies yielding 220 dependent effect sizes met our inclusion criteria. We found a statistically significant, small longitudinal relationship between parental substance abuse and child well-being, with significant differences both between and within studies. The association between parental substance abuse and child well-being did not differ according to the length of the period between recording the parental substance abuse and the subsequent child well-being outcome, suggesting an enduring effect over time (Evans, Li, & Whipple, 2013). These results indicate that parental substance abuse is a risk factor for subsequent child well-being. The prevalence of substance use and parenthood points to the clinical significance of this risk factor. However, we caution readers to avoid interpreting parental substance abuse as a causal risk factor (see Kraemer et al., 1997 for a discussion of risk factor typology) and explicitly recognize that parental substance abuse and child well-being may be caused by the same third variable (e.g., financial or marital problems) or that both concepts can have a reciprocal relationship.
The longitudinal associations observed in the current meta-analysis were heterogeneous, with significant differences relating to the parental substance abuse type. Parental alcohol use (whether dependent or not) had similar secondary effects on children as parental tobacco use, suggesting that recreational alcohol use is as harmful for child well-being as secondary tobacco use and alcohol use disorder. Parental drug use yielded the strongest effect, which could (partially) be due to the illegal nature of these substances that could result in additional disruptive effects on families, such as fines, arrest, or custodial sentences. It should be noted that none of the studies considered prescription drug use, which is an important shortcoming given concerns over prescription opioids (Cicero, Ellis, Surratt, & Kurtz, 2014). Parental substance abuse had similar effects on the physical, psychological, and cognitive well-being of their children. The effects did not differ for fathers, mothers, sons, or daughters, nor according to the age of the child. Although small in magnitude, the effect of parental substance abuse on child well-being has a clear public health significance given the high prevalence of substance abuse (Cumming, 2014).
Our findings corroborate the conjecture that the effect of parental substance abuse on child well-being manifests through the lens of the family environment, with broad detrimental effects on physical, psychological, and cognitive well-being. The substantial unexplained variance that remained in our meta-analysis combined with an effect across substance abuse types could arise from unmeasured factors influencing child well-being that are common across all types of parental substance abuse. If targeting parental substance abuse is to be used in family-centred interventions to improve child outcomes (Calhoun, Conner, Miller, & Messina, 2015), then it will be necessary to further investigate how parental substance abuse affects child outcomes through the parent-child environment. More generally, working with the context of substance abuse, including the family environment in activities is increasingly seen as important in supporting recovery (Friedmann, Hendrickson, Gerstein, & Zhang, 2004; Oser, Knudsen, Staton-Tindall, & Leukefeld, 2009), and this suggests that both child well-being and parental substance abuse can be addressed through targeting aspects of the family environment.
Strengths and limitations
This study is the first large-scale review to broadly summarize the longitudinal relationship between parental substance abuse and child well-being. We excluded studies that sampled from specific groups whose membership would be expected to be associated with the child well-being outcome. As such, the reported association might be considered conservative, albeit more representative of the general population by doing so. There was no evidence of publication bias or an effect of methodological (rigor) features on the strength of the association, which further underpins the robustness of the findings. The multilevel approach to meta-analysis allowed us to include all relevant effect sizes, to model between- and within-study heterogeneity, and potential moderators that could explain variance at both levels—features that cannot be addressed with a standard meta-analytic approach. Although the multilevel approach is a powerful technique, some moderator analyses may have suffered from low power due to unbalanced groups. In particular, the subgroup effect of parental substance abuse in very young children was slightly elevated, while the subgroup effect for cognitive well-being was less pronounced. The limited number of studies on these topics could have reduced the power of the omnibus test to statistically detect group differences.
Parents with problematic patterns of using an intoxicating substance are likely to show variation in their use patterns over time, including tolerance and consequent increased consumption of substances to achieve the desired effect. They may also go through repeated withdrawal and relapse. At least for chronic use, there is more than simply the presence or the absence of parental substance abuse that potentially affects child well-being—features that this meta-analysis was unable to consider, as this was not reported in the literature reviewed. Furthermore, there was considerable variation in the way parental substance abuse was measured across studies. Some combined substance abuse into a nebulous “any substance” category, some measured frequency, and others reported on recency of use. Given the investment in time and resources required by longitudinal studies, it is important that measurement is given careful consideration in future research and a range of metrics are taken to ensure that parental substance abuse can be appropriately captured. It is feasible that consumption heterogeneity in substances used (e.g., polysubstance abuse, frequency, dose, and physical dependence) would provide additional insights.
Although our results highlight that parental substance abuse is detrimental to children and adolescents, our findings are tempered by the limited number of studies that examined cognitive, social, or economic child well-being outcomes. Only three of the five dimensions of child well-being had sufficient data to be analyzed; therefore, the reported association should be interpreted as a deprecated form of child well-being rather than one that encompasses all aspects of well-being as we intended to quantify.
Within primary studies, well-being outcomes have likely been selected on a like-for-like basis such that parental substance abuse (e.g., tobacco) is expected to have implications for children's health (e.g., respiratory health), and parental alcohol use is expected to have implications for children's subsequent alcohol use, while educational attainment and other aspects of child well-being have been largely ignored. This is notable because the likely mechanisms—that parental substance abuse affects the parent-child relationship–suggests that a broader set of outcomes should be considered and that these gaps in the literature imply that child well-being is not sufficiently investigated to draw firm conclusions about all facets of well-being.
Moreover, as parental substance abuse measures were variously defined from “any substance abuse” to specific substances, there is potential variability in harm by substance type, other than alcohol and tobacco, which we were unable to capture due to a paucity of studies and poorly operationalized measures. Gender differences were also poorly operationalized, with many studies failing to separately capture father and mother differences between boys and girls. Just a third of the included studies considered mothers and fathers separately, only three studies differentiated between male and female children, and only a quarter considered children under 12 years of age. No study supplemented self-report data with objective outcomes, such as data from school or medical records. Therefore, future research needs to improve efforts to account for the multidimensionality of well-being, substance abuse, and features that could moderate effects, as it is possible that the effect of parental substance abuse is conditional on other factors that have not yet been formally documented. The generalizability of the results may also be limited due to a preponderance of studies emerging from North America. These biases and omissions in the research literature offer important opportunities to improve our understanding of the effects of parental substance abuse on child well-being.
Conclusion
This meta-analysis found that children exposed to parents who consume alcohol (both dependent and non-dependent), tobacco, or other psychoactive drugs experience a detrimental long-term effect on their well-being. However, there is a need for longitudinal studies that more accurately capture the effects of parental psychoactive substance abuse on the full scope of childhood well-being outcomes and integrate substance abuse into models that specify the precise conditions under which parental behavior determines child well-being. These results can inform the development of family-oriented initiatives directed at improving child well-being that may also assist parental recovery.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0954579419000749.
click here to view supplementary material
References
References marked with an asterisk indicate studies included in the meta-analysis.
- *Adalbjarnardottir S., & Rafnsson F. D. (2002). Adolescent antisocial behavior and substance use: Longitudinal analyses. Addictive Behaviors, 27, 227–240. [DOI] [PubMed] [Google Scholar]
- Bandiera F. C., Richardson A. K., Lee D. J., He J.-P., & Merikangas K. R. (2011). Secondhand smoke exposure and mental health among children and adolescents. Archives of Pediatrics & Adolescent Medicine, 165, 332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Barman S. K., Pulkkinen L., Kaprio J., & Rose R. J. (2004). Inattentiveness, parental smoking and adolescent smoking initiation. Addiction, 99, 1049–1061. [DOI] [PubMed] [Google Scholar]
- Barnard M., & McKeganey N. (2004). The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction, 99, 552–559. [DOI] [PubMed] [Google Scholar]
- *Barnow S., Schuckit M., Smith T., Spitzer C., & Freyberger H. J. (2007). Attention problems among children with a positive family history of alcohol abuse or dependence and controls—Prevalence and course for the period from preteen to early teen years. European Addiction Research, 13(1), 1–5. [DOI] [PubMed] [Google Scholar]
- Beck F., Guignard R., & Legleye S. (2014). Does computer survey technology improve reports on alcohol and illicit drug use in the general population? A comparison between two surveys with different data collection modes in France. PloS One, 9(1), e85810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger L. M., Paxson C., & Waldfogel J. (2009). Income and child development. Children and Youth Service Reviews, 31, 978-989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bor W., McGee T. R., & Fagan A. A. (2004). Early risk factors for adolescent antisocial behaviour: An Australian longitudinal study. Australian and New Zealand Journal of Psychiatry, 38, 365–372. [DOI] [PubMed] [Google Scholar]
- Bountress K., & Chassin L. (2015). Risk for behavior problems in children of parents with substance use disorders. American Journal of Orthopsychiatry, 85, 275–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw J. (2016). The Well-being of Children in the UK. Bristol: Policy Press. [Google Scholar]
- *Brook J. S., Brook D. W., Arencibia-Mireles O., Richter L., & Whiteman M. (2001). Risk factors for adolescent marijuana use across cultures and across time. Journal of Genetic Psychology, 162, 357–374. [DOI] [PubMed] [Google Scholar]
- *Bufferd S. J., Dougherty L. R., Olino T. M., Dyson M. W., Laptook R. S., Carlson G. A., & Klein D. N. (2014). Predictors of the onset of depression in young children: A multi-method, multi-informant longitudinal study from ages 3 to 6. Journal of Child Psychology and Psychiatry and Allied Disciplines, 55, 1279–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Burke V., Beilin L. J., & Dunbar D. (2001). Family lifestyle and parental body mass index as predictors of body mass index in Australian children: A longitudinal study. International Journal of Obesity and Related Metabolic Disorders, 25, 147–157. [DOI] [PubMed] [Google Scholar]
- Calhoun S., Conner E., Miller M., & Messina N. (2015). Improving the outcomes of children affected by parental substance abuse: A review of randomized controlled trials. Substance Abuse and Rehabilitation, 6, 15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chaffin M., Kelleher K., & Hollenberg J. (1996). Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse and Neglect, 20, 191–203. [DOI] [PubMed] [Google Scholar]
- Cheung S. F., & Chan D. K.-S. (2004). Dependent effect sizes in meta analysis: Incorporating the degree of interdependence. Journal of Applied Psychology, 89, 780–791. [DOI] [PubMed] [Google Scholar]
- Cicero T. J., Ellis M. S., Surratt H. L., & Kurtz S. P. (2014). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry, 71, 821–826. [DOI] [PubMed] [Google Scholar]
- *Colder C. R., Chassin L., Stice E. M., & Curran P. J. (1997). Alcohol expectancies as potential mediators of parent alcoholism effects on the development of adolescent heavy drinking. Journal of Research on Adolescence, 7, 349–374. [Google Scholar]
- Collins L. M., & Horn J. L. (Eds.) (1991). Best methods for the analysis of change: Recent advances, unanswered questions, future directions. Washington: American Psychological Association. [Google Scholar]
- *Connolly G. M., Casswell S., Stewart J., & Silva P. A. (1992). Drinking context and other influences on the drinking of 15-year-old New Zealanders. British Journal of Addiction, 87, 1029–1036. [DOI] [PubMed] [Google Scholar]
- *Crandall M., Chiu B., & Sheehan K. (2006). Injury in the first year of life: Risk factors and solutions for high-risk families. Journal of Surgical Research, 133(1), 7–10. [DOI] [PubMed] [Google Scholar]
- *Cranford J. A., Zucker R. A., Jester J. M., Puttler L. I., & Fitzgerald H. E. (2010). Parental alcohol involvement and adolescent alcohol expectancies predict alcohol involvement in male adolescents. Psychology of Addictive Behaviors, 24, 386–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming G. (2014). The new statistics: Why and how. Psychological Science, 25, 7–29. [DOI] [PubMed] [Google Scholar]
- De Goede I. H., Branje S. J., Delsing M. J., & Meeus W. H. (2009). Linkages over time between adolescents' relationships with parents and friends. Journal of Youth and Adolescence, 38, 1304–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A., Augenstein T. M., Wang M., Thomas S. A., Drabick D. A., Burgers D. E., & Rabinowitz J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141, 858–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E., Oishi S., & Lucas R. E. (2003). Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annual Review of Psychology, 54, 403–425. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction (2008). Drugs and Vulnerable Groups of Young People. Luxembourg: Office for Official Publications of the European Communitie. [Google Scholar]
- *Dwyer T., Ponsonby A.-L., & Couper D. (1999). Tobacco smoke exposure at one month of age and subsequent risk of SIDS: A prospective study. American Journal of Epidemiology, 149, 593–602. [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G. D., Schneider M., & Minder C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Eiden R. D., Edwards E. P., & Leonard K. E. (2007). A conceptual model for the development of externalizing behavior problems among kindergarten children of alcoholic families: Role of parenting and children's self-regulation. Developmental Psychology, 43, 1187–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ellickson P. L., Tucker J. S., Klein D. J., & McGuigan K. A. (2001). Prospective risk factors for alcohol misuse in late adolescence. Journal of Studies on Alcohol, 62, 773–782. [DOI] [PubMed] [Google Scholar]
- Evans G. W., Li D., & Whipple S. S. (2013). Cumulative risk and child development. Psychological Bulletin, 139, 1342–1396. [DOI] [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse (CASA). (2005). Family matters: Substance abuse and the American family. Retrieved from https://www.centeronaddiction.org/sites/default/files/Family-matters-substance-abuse-and-the-american-family_0.pdf.
- Faragher E. B., Cass M., & Cooper C. L. (2005). The relationship between job satisfaction and health: A meta-analysis. Occupational and Environmental Medicine, 62, 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon R., Bakermans-Kranenburg M. J., Van Iizendoorn M. H., Lapsley A. M., & Roisman G. I. (2010). The significance of insecure attachment and disorganization in the development of children's externalizing behavior: A meta-analytic study. Child Development, 81, 435–456. [DOI] [PubMed] [Google Scholar]
- *Fergusson D. M., Horwood L. J., & Lynskey M. (1994). The childhoods of multiple problem adolescents: A 15-year longitudinal study. Journal of Child Psychology and Psychiatry and Allied Disciplines, 35, 1123–1140. [DOI] [PubMed] [Google Scholar]
- *Fergusson D. M., Horwood L. J., & Lynskey M. T. (1993). Maternal smoking before and after pregnancy: Effects on behavioral outcomes in middle childhood. Pediatrics, 92, 815–822. [PubMed] [Google Scholar]
- *Fergusson D. M., Lynskey M. T., & Horwood L. J. (1996). Comorbidity between depressive disorders and nicotine dependence in a cohort of 16-year-olds. Archives of General Psychiatry, 53, 1043–1047. [DOI] [PubMed] [Google Scholar]
- *Frank D. A., Kuranz S., Appugliese D., Cabral H., Chen C., Crooks D., … Rose-Jacobs R. (2014). Problematic substance use in urban adolescents: Role of intrauterine exposures to cocaine and marijuana and post-natal environment. Drug and Alcohol Dependence, 142, 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann P. D., Hendrickson J. C., Gerstein D. R., & Zhang Z. (2004). The effect of matching comprehensive services to patients’ needs on drug use improvement in addiction treatment. Addiction, 99, 962–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu R., Gartlehner G., Grant M., Shamliyan T., Sedrakyan A., Wilt T. J., … Trikalinos T. A. (2011). Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. Journal of Clinical Epidemiology, 64, 1187–1197. [DOI] [PubMed] [Google Scholar]
- *Fuller B. E., Chermack S. T., Cruise K. A., Kirsch E., Fitzgerald H. E., & Zucker R. A. (2003). Predictors of aggression across three generations among sons of alcoholics: Relationships involving grandparental and parental alcoholism, child aggression, marital aggression and parenting practices. Journal of Studies on Alcohol, 64, 472–483. [DOI] [PubMed] [Google Scholar]
- Gallagher M. W., Lopez S. J., & Preacher K. J. (2009). The hierarchical structure of well-being. Journal of Personality, 77, 1025–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giesbrecht N., Cukier S., & Steeves D. (2010). Collateral damage from alcohol: Implications of ‘second-hand effects of drinking’ for populations and health priorities. Addiction, 105, 1323–1325. [DOI] [PubMed] [Google Scholar]
- *Griesler P. C., Hu M. C., Schaffran C., & Kandel D. B. (2011). Comorbid psychiatric disorders and nicotine dependence in adolescence. Addiction, 106, 1010-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Gritz E. R., Prokhorov A. V., Hudmon K. S., Jones M. M., Rosenblum C., Chang C. C., … de Moor C. (2003). Predictors of susceptibility to smoking and ever smoking: A longitudinal study in a triethnic sample of adolescents. Nicotine and Tobacco Research, 5, 493–506. [DOI] [PubMed] [Google Scholar]
- *Hanewinkel R., Sargent J. D., Hunt K., Sweeting H., Engels R. C., Scholte R. H., … Morgenstern M. (2014). Portrayal of alcohol consumption in movies and drinking initiation in low-risk adolescents. Pediatrics, 133, 973–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Heron J., Barker E. D., Joinson C., Lewis G., Hickman M., Munafo M., & Macleod J. (2013). Childhood conduct disorder trajectories, prior risk factors and cannabis use at age 16: Birth cohort study. Addiction, 108, 2129–2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J. P. T., & Green S. (Ed.) (2011). Cochrane Handbook for Systematic Reviews of Interventions (Vol. 4): Chichester, UK: Wiley. [Google Scholar]
- Hoeve M., Stams G. J. J., van der Put C. E., Dubas J. S., van der Laan P. H., & Gerris J. R. (2012). A meta-analysis of attachment to parents and delinquency. Journal of Abnormal Child Psychology, 40, 771–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hoffmann J. P., & Cerbone F. G. (2002). Parental substance use disorder and the risk of adolescent drug abuse: An event history analysis. Drug and Alcohol Dependence, 66, 255–264. [DOI] [PubMed] [Google Scholar]
- *Hussong A. M., & Chassin L. (1997). Substance use initiation among adolescent children of alcoholics: Testing protective factors. Journal of Studies on Alcohol, 58, 272–279. [DOI] [PubMed] [Google Scholar]
- Hussong A. M., Bauer D. J., Huang W., Chassin L., Sher K. J., & Zucker R. A. (2008). Characterizing the life stressors of children of alcoholic parents. Journal of Family Psychology, 22, 819–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong A. M., Huang W., Curran P. J., Chassin L., & Zucker R. A. (2010). Parent alcoholism impacts the severity and timing of children's externalizing symptoms. Journal of Abnormal Child Psychology, 38, 367–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Johnson J. L., & Leff M. (1999). Children of substance abusers: Overview of research findings. Pediatrics, 103(5 Pt 2), 1085–1099. [PubMed] [Google Scholar]
- *Kaplow J. B., Curran P. J., & Dodge K. A. (2002). Child, parent, and peer predictors of early-onset substance use: A multisite longitudinal study. Journal of Abnormal Child Psychology, 30, 199–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes C. L. (2009). The nature and importance of positive mental health in America's adolescents In Gilmen R., Huebner E. S., & Furlong M. J. (Eds.), Handbook of Positive Psychology in Schools (pp. 9–23). New yYork: Routlegde. [Google Scholar]
- *Knudsen A. K., Ystrom E., Skogen J. C., & Torgersen L. (2015). Maternal heavy alcohol use and toddler behavior problems: a fixed effects regression analysis. European Child and Adolescent Psychiatry, 24, 1269–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Korhonen T., Huizink A. C., Dick D. M., Pulkkinen L., Rose R. J., & Kaprio J. (2008). Role of individual, peer and family factors in the use of cannabis and other illicit drugs: A longitudinal analysis among Finnish adolescent twins. Drug and Alcohol Dependence, 97, 33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Kotch J. B., Smith J., Margolis B., Black M. M., English D., Thompson R., … Bangdiwala S. I. (2014). Does social capital protect against the adverse behavioral outcomes of child neglect? Child Abuse Review, 23, 246–261. [Google Scholar]
- Kraemer H. C., Kazdin A. E., Offord D. R., Kessler R. C., Jensen P. S., & Kupfer D. J. (1997). Coming to terms with the terms of risk. Archives of General Psychiatry, 54, 337–343. [DOI] [PubMed] [Google Scholar]
- Kuppens S., Grietens H., Onghena P., & Michiels D. (2009a). A longitudinal study of childhood social behavior: Inter-informant agreement, inter-context agreement, and social preference linkages. Journal of Social and Personal Relationships, 26, 769–792. [Google Scholar]
- Kuppens S., Grietens H., Onghena P., & Michiels D. (2009b). Measuring parenting dimensions in middle childhood: Multitrait-multimethod analysis of child, mother, and father ratings. European Journal of Psychological Assessment, 25, 133–140. [Google Scholar]
- Lander L., Howsare J., & Byrne M. (2013). The impact of substance use disorders on families and children: From theory to practice. Social Work in Public Health, 28, 194–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Lessard J., Henrie J., Livingston J. A., Leonard K. E., Colder C. R., & Eiden R. D. (2014). Correlates of ever having used electronic cigarettes among older adolescent children of alcoholic fathers. Nicotine and Tobacco Research, 16, 1656–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Li C., Pentz M. A., & Chou C. P. (2002). Parental substance use as a modifier of adolescent substance use risk. Addiction, 97, 1537–1550. [DOI] [PubMed] [Google Scholar]
- *Lindsey M. A., Browne D. C., Thompson R., Hawley K. M., Graham J., Weisbart C., … Kotch J. B. (2008). Caregiver mental health, neighborhood, and social network influences on mental health needs among African American children. Social Work Research, 32, 79–88. [Google Scholar]
- Lipari R. N. and Van Horn S. L. (2017). Children living with parents who have a substance use disorder. The CBHSQ Report: August 24, 2017. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD: Retrieved from https://www.samhsa.gov/data/sites/default/files/report_3223/ShortReport-3223.html [PubMed] [Google Scholar]
- Littell R. C., Milliken G. A., Stroup W. W., Wolfinger R. D., & Schabenberger O. (2006). SAS for Mixed Models (2nd Ed.). Cary, NC: SAS Institute. [Google Scholar]
- *Loukas A., Fitzgerald H. E., Zucker R. A., & von Eye A. (2001). Parental alcoholism and co-occurring antisocial behavior: Prospective relationships to externalizing behavior problems in their young sons. Journal of Abnormal Child Psychology, 29, 91–106. [DOI] [PubMed] [Google Scholar]
- Mallett S., Rosenthal D., & Keys D. (2005). Young people, drug use and family conflict: Pathways into homelessness. Journal of Adolescence, 28, 185–199. [DOI] [PubMed] [Google Scholar]
- *Malone S. M., Iacono W. G., & McGue M. (2002). Drinks of the father: Father's maximum number of drinks consumed predicts externalizing disorders, substance use, and substance use disorders in preadolescent and adolescent offspring. Alcoholism: Clinical and Experimental Research, 26, 1823–1832. [DOI] [PubMed] [Google Scholar]
- Martin A., Razza R. A., & Brooks-Gunn J. (2012). Specifying the links between household chaos and preschool children's development. Early Child Development and Care, 182, 1247–1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath C. E., Watson A. L., & Chassin L. (1999). Academic achievement in adolescent children of alcoholics. Journal of Studies on Alcohol, 60, 18-26. [DOI] [PubMed] [Google Scholar]
- *McGrath C. E., Watson A. L., & Chassin L. (1999). Academic achievement in adolescent children of alcoholics. Journal of Studies on Alcohol, 60, 18–26. [DOI] [PubMed] [Google Scholar]
- *Miller J. E. (2001). Predictors of asthma in young children: Does reporting source affect our conclusions? American Journal of Epidemiology, 154, 245–250. [DOI] [PubMed] [Google Scholar]
- Mitchell E. A., Beasley R., Keil U., Montefort S., Odhiambo J., & Group I. P. T. S. (2012). The association between tobacco and the risk of asthma, rhinoconjunctivitis and eczema in children and adolescents: Analyses from Phase Three of the ISAAC programme. Thorax, 67, 941–949. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., & The P. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Morgenstern M., Sargent J. D., Isensee B., & Hanewinkel R. (2013). From never to daily smoking in 30 months: The predictive value of tobacco and non-tobacco advertising exposure. BMJ Open, 3(6), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison A., Polisena J., Husereau D., Moulton K., Clark M., Fiander M., … Rabb D. (2012). The effect of English-language restriction on systematic review-based meta-analyses: A systematic review of empirical studies. International Journal of Technology Assessment in Health Care, 28, 138–144. [DOI] [PubMed] [Google Scholar]
- *Naicker K., Wickham M., & Colman I. (2012). Timing of first exposure to maternal depression and adolescent emotional disorder in a national Canadian cohort. PLoS ONE, 7(3), e33422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman D. B., Tay L., & Diener E. (2014). Leisure and subjective well-being: A model of psychological mechanisms as mediating factors. Journal of Happiness Studies, 15, 555–578. [Google Scholar]
- *Nigg J. T., Wong M. M., Martel M. M., Jester J. M., Puttler L. I., Glass J. M., … Zucker R. A. (2006). Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 468–475. [DOI] [PubMed] [Google Scholar]
- Öberg M., Jaakkola M. S., Woodward A., Peruga A., & Prüss-Ustün A. (2011). Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet, 377(9760), 139–146. [DOI] [PubMed] [Google Scholar]
- Oser C., Knudsen H., Staton-Tindall M., & Leukefeld C. (2009). The adoption of wraparound services among substance abuse treatment organizations serving criminal offenders: The role of a women-specific program. Drug and Alcohol Dependence, 103, S82–S90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Pagani L. S., Nguyen A. K., & Fitzpatrick C. (2016). Prospective associations between early long-term household tobacco smoke exposure and subsequent indicators of metabolic risk at age 10. Nicotine and Tobacco Research, 18, 1250–1257. [DOI] [PubMed] [Google Scholar]
- Parsons J. E., Adler T. F., & Kaczala C. M. (1982). Socialization of achievement attitudes and beliefs: Parental influences. Child Development, 53, 310–321. [Google Scholar]
- Peterson A. V., Leroux B. G., Bricker J., Kealey K. A., Marek P. M., Sarason I. G., & Andersen M. R. (2006). Nine-year prediction of adolescent smoking by number of smoking parents. Addictive Behaviors, 31, 788–801. [DOI] [PubMed] [Google Scholar]
- Podsakoff P. M., MacKenzie S. B., Lee J.-Y., & Podsakoff N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88, 879–903. [DOI] [PubMed] [Google Scholar]
- Pollard E. L., & Lee P. D. (2003). Child well-being: A systematic review of the literature. Social Indicators Research, 61, 5978. [Google Scholar]
- *Power T. G., Stewart C. D., Hughes S. O., & Arbona C. (2005). Predicting patterns of adolescent alcohol use: A longitudinal study. Journal of Studies on Alcohol, 66, 74–81. [DOI] [PubMed] [Google Scholar]
- Puttler L. I., Zucker R. A., Fitzgerald H. E., & Bingham C. R. (1998). Behavioral outcomes among children of alcoholics during the early and middle childhood years: Familial subtype variations. Alcoholism: Clinical and Experimental Research, 22, 1962–1972. [PubMed] [Google Scholar]
- Raudenbush S. W., & Bryk A. S. (2002). Hierarchical Linear Models: Applications and Data Analysis Methods (2nd ed.). London: Sage. [Google Scholar]
- *Roosa M. W., Beals J., Sandler I. N., & Pillow D. R. (1990). The role of risk and protective factors in predicting symptomatology in adolescent self-identified children of alcoholic parents. American Journal of Community Psychology, 18, 725–741. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. (1991). Meta-Analytic Procedures for Social Research. Newbury Park, CA: Sage. [Google Scholar]
- Rossow I., Keating P., Felix L., & McCambridge J. (2016). Does parental drinking influence children's drinking? A systematic review of prospective cohort studies. Addiction, 111, 204-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C. D., & Keyes C. L. M. (1995). The structure of psychological well-being revisited. Journal of Personality and Social Psychology, 69, 719-727. [DOI] [PubMed] [Google Scholar]
- Saulyte J., Regueira C., Montes-Martínez A., Khudyakov P., & Takkouche B. (2014). Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: A systematic review and meta-analysis. PLoS Medicine, 11(3), e1001611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Selya A. S., Dierker L. C., Rose J. S., Hedeker D., & Mermelstein R. J. (2012). Risk factors for adolescent smoking: Parental smoking and the mediating role of nicotine dependence. Drug and Alcohol Dependence, 124, 311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Shortt A. L., Hutchinson D. M., Chapman R., & Toumbourou J. W. (2007). Family, school, peer and individual influences on early adolescent alcohol use: First-year impact of the Resilient Families programme. Drug and Alcohol Review, 26, 625–634. [DOI] [PubMed] [Google Scholar]
- Siddaway A. P., Taylor P. J., & Wood A. M. (2018). Re-conceptualizing anxiety as a continuum that ranges from high calmness to high anxiety: The joint importance of reducing distress and increasing well-being. Journal of Personality and Social Psychology, 114, e1–e11. [DOI] [PubMed] [Google Scholar]
- Siddaway A. P., Wood A. M., & Taylor P. J. (2017). The Centre for Epidemiologic Studies-Depression (CES-D) scale measures a continuum from well-being to depression: Testing two key predictions of Positive Clinical Psychology. Journal of Affective Disorders, 213, 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddaway A. P., Wood A. M., & Hedges L. V. (2019). How to do a systematic review: A best practice guide to conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annual Review of Psychology, 70, 747–770. [DOI] [PubMed] [Google Scholar]
- Størksen I., Røysamb E., Moum T., & Tambs K. (2005). Adolescents with a childhood experience of parental divorce: A longitudinal study of mental health and adjustment. Journal of Adolescence, 28, 725–739. [DOI] [PubMed] [Google Scholar]
- Straussner S. L. A. (1994). The impact of alcohol and other drug abuse on the American family. Drug and Alcohol Review, 13, 393–399. [DOI] [PubMed] [Google Scholar]
- Straussner S. L. A. (2004). Assessment and treatment of clients with alcohol and other drug abuse problems In Straussner S. L. A. (Ed.), Clinical Work with Substance-Abusing Clients (pp. 3–36). New York: Guildford. [Google Scholar]
- Straussner S. L. A., & Fewell C. H. (2011). Children of Substance-abusing Parents: Dynamics and Treatment. New York: Springer Publishing Company. [Google Scholar]
- Stroup D. F., Berlin J. A., Morton S. C., Olkin I., Williamson G. D., Rennie D., … Thacker S. B. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA, 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- *Thacher J. D., Gruzieva O., Pershagen G., Neuman A., van Hage M., Wickman M., … Bergstrom A. (2016). Parental smoking and development of allergic sensitization from birth to adolescence. Allergy, 71, 239–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Thompson K. M., & Wilsnack R. W. (1987). Parental influence on adolescent drinking: Modeling, attitudes, or conflict? Youth and Society, 19, 22–43. [Google Scholar]
- *Ting T. T., Chen W. J., Liu C. Y., Lin Y. C., & Chen C. Y. (2015). Peer influences on alcohol expectancies in early adolescence: A study of concurrent and prospective predictors in Taiwan. Addictive Behaviors, 40, 7–15. [DOI] [PubMed] [Google Scholar]
- *Tjora T., Hetland J., Aaro L. E., & Overland S. (2011). Distal and proximal family predictors of adolescents' smoking initiation and development: A longitudinal latent curve model analysis. BMC Public Health, 11, 911–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torgerson C. J. (2006). Publication bias: the achilles' heel of systematic reviews? British Journal of Educational Studies, 54, 89–102. [Google Scholar]
- Tourangeau R., & Yan T. (2007). Sensitive questions in surveys. Psychological Bulletin, 133, 859–883. [DOI] [PubMed] [Google Scholar]
- *Unger J. B., Shakib S., Gallaher P., Ritt-Olson A., Mouttapa M., Palmer P. H., & Johnson C. A. (2006). Cultural/interpersonal values and smoking in an ethnically diverse sample of Southern California adolescents. Journal of Cultural Diversity, 13, 55–63. [PubMed] [Google Scholar]
- Van den Noortgate W., Lopez-Lopez J. A., Marin-Martinez F., & Sanchez-Meca J. (2013). Three-level meta-analysis of dependent effect sizes. Behavioral Research Methods, 45, 576–594. [DOI] [PubMed] [Google Scholar]
- *Van Der Vorst H., Krank M., Engels R. C., Pieters S., Burk W. J., & Mares S. H. (2013). The mediating role of alcohol-related memory associations on the relation between perceived parental drinking and the onset of adolescents' alcohol use. Addiction, 108, 526–533. [DOI] [PubMed] [Google Scholar]
- *Vella S. A., Magee C. A., & Cliff D. P. (2015). Trajectories and predictors of health-related quality of life during childhood. Journal of Pediatrics, 167, 422–427. [DOI] [PubMed] [Google Scholar]
- Vevea J. L., & Woods C. M. (2005). Publication bias in research synthesis: Sensitivity analysis using a priori weight functions. Psychological Methods, 10, 428–443. [DOI] [PubMed] [Google Scholar]
- Wilson D. B. (2017). Comprehensive Meta-Analysis (Version 3). Englewood, NJ: Biostat. [Google Scholar]
- *Windham A. M., Rosenberg L., Fuddy L., McFarlane E., Sia C., & Duggan A. K. (2004). Risk of mother-reported child abuse in the first 3 years of life. Child Abuse and Neglect, 28, 645–667. [DOI] [PubMed] [Google Scholar]
- *Wong M. M., Brower K. J., & Zucker R. A. (2011). Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. Journal of Psychiatric Research, 45, 505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong W. C., Cheung C. S., & Hart G. J. (2008). Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerging Themes in Epidemiology, 5, 23–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2004). Promoting mental health: Concepts, emerging evidence, practice. Geneva: World Health Organization. [Google Scholar]
- *Xie B., Palmer P., Li Y., Lin C., & Johnson C. A. (2013). Developmental trajectories of cigarette use and associations with multilayered risk factors among Chinese adolescents. Nicotine and Tobacco Research, 15, 1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0954579419000749.
click here to view supplementary material