Abstract
Coronary perforation is a rare complication of percutaneous coronary interventions and a challenging scenario which imposes prompt recognition and treatment. Although it may be successfully managed percutaneously, a surgical treatment may be preferable in some cases. We report the case of a patient with a coronary perforation with initial percutaneous treatment complicated with extravascular implantation of a covered stent and liver laceration, who was succesfully treated by cardiac surgery. This case suggests the importance of the proximity of an onsite cardiac surgery center when complex coronary artery percutaneous interventions are performed in hospitals with offsite surgical support.
Electronic supplementary material
The online version of this article (10.1007/s12055-019-00900-4) contains supplementary material, which is available to authorized users.
Keywords: Coronary perforation, Cath lab, Coronary complication
Introduction
Coronary artery perforation is an uncommon complication of percutaneous coronary interventions (PCI). It is associated with high morbidity and mortality [1]. In some cases, it can be successfully managed percutaneously. However, especially in case of Ellis III perforations, surgical management can be necessary. We report a case about a Ellis-type III [2] coronary artery perforation requiring surgical management, which did not have any further postoperative complications.
Case report
The patient was a 71-year-old man with several cardiovascular risk factors: ex-smoker, hypertension, and diabetes. A coronary angiography was performed due to the presence of apical ischemia on a scintigraphy and due to effort angina. The exam revealed a 3-vessel coronary artery disease with a chronic occlusion of the left anterior descending artery (LAD). A PCI of the LAD was attempted. During the procedure, a coronary artery perforation and a resulting tamponade occurred (Movie 1), which was initially treated percutaneously with the implantation of a covered stent (PK PAPYRUS 2.5 × 20 mm) (Movie 2) and percutaneous pericardial catheter drainage. Due to the persistence of blood extravasation despite the implantation of the covered stent, a balloon (RYUJIN Plus 2.0/20) was inflated proximal to the stent. After achieving hemodynamic stabilization, the patient was transferred to our center for surgical management.
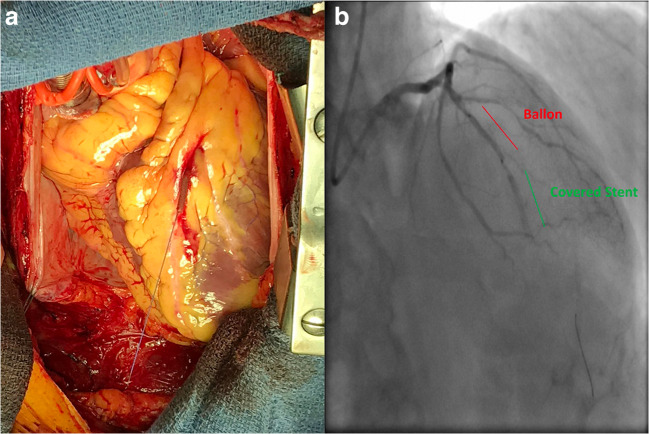
Intra-operative findings confirmed a coronary artery perforation in the LAD with extravascular implantation of the covered stent (Fig. 1) and extravascular placement of the guidewire. After installation of the extracorporeal circulation and aortic clamping, the stent, the balloon, and the guidewire were removed, and the LAD was ligated using 2-pledged stitches. Since the patient was haemodynamically stable, we decided to use bilateral internal thoracic arteries to create a Y-graft which is the preferred conduit strategy in our unit: the left thoracic artery on the LAD and on the first diagonal branch and the right thoracic artery on the posterior interventricular artery. Weaning from extracorporeal circulation was achieved without inotropic support; although, transfusion of plasma and platelets was required during the hemostasis. An accidental opening of the peritoneal cavity revealed a superficial perforation of the liver with the catheter of pericardial drainage and a hematoma. Hemostasis of the liver and the lavage of the abdominal cavity were performed by general surgeons. After, the patient was transferred to surgical reanimation. The postoperative course was uneventful and the patient was extubated at day 0.
Fig. 1.
Peroperatory findings. On the left: exit point of the stent from the LAD. On the right: angiographic positioning of the stent and ballon.
Discussion
The incidence of coronary artery perforation as cath lab complication varies between 0.71% and 8.8% in literature [1, 3, 4]. It is a potentially life-threatening complication, if not promptly recognized and treated. According to the Ellis classification, coronary perforations are classified as type I (extraluminal crater), type II (pericardial blushing), and type III (contrast streaming or cavity spilling). Types I and II coronary perforations are usually caused by stiff guidewires and can be treated by a prolonged balloon inflation. Type I has a benign prognosis, whereas type II coronary perforations have the potential to progress to tamponade. Type III coronary perforations are caused by balloons, stents, or other intracoronary devices and may lead to cardiac tamponade imposing pericardial drainage [2]. Type III perforation refers to a complete rupture of the coronary wall, with active bleeding in the pericardium, which has 14.8% of in-hospital mortality rate [5]. The management of this complication consists on the reversal of heparin, on platelet transfusion, and on pericardial drainage followed by the implantation of covered stents [6–8], which may be life-saving but increase the risk of thrombosis. Other “non-invasive” solutions have been also proposed, such as the use of coils, microspheres, and thrombin injection [9, 10]; they are embolizing materials that are effective, but mostly used for the treatment of type I or II perforations. The downside of the use of embolic materials is the potential permanent loss of the vessel lumen beyond the site of deployment, with subsequent infarction. In addition, foreign body reaction may lead to granulomatous arteritis and coronary occlusion. This case shows a pure percutaneous treatment might be not enough for the treatment of these complications, and therefore, a surgical evaluation might be valuable. Even if it is not as immediate as cath lab angiographic management, surgery allows hemostasis under direct vision and complete revascularization, and it is not burdened by increased infarction risk. Stent positioning and balloon inflation may be an effective treatment, but their management is unpredictable and may be failing as well. The cardiologist should, however, have experience with these techniques which allow him to gain time in case of complications. According to the AHA/ACC coronary lesion classification, type A lesions are susceptible of angioplasty, whereas occlusions are type B or C lesions, so respectively moderate risk procedures [11]. During the last years, cath lab activity underwent deep changes: it increased, dealing with both diagnosis and treatment of different cardiovascular pathologies. Technological and pharmacological evolution allowed more and more complex procedures, on difficult patients; particularly, cath lab activity became the gold standard for acute coronary syndromes. Experienced interventionists can use special dedicated devices, in case of complications, but cardiac surgery inside the hospital may be life-saving.
The ideal site for cath lab is in a cardiovascular unit, where intensive care unit and cardiac surgery are available and easily accessible. In case of coronary perforation, in fact, until some years ago, surgical revascularization was the treatment of choice. Cath lab protocols should be strict and aim to provide the quality standards required to maintain safety and the rational use of technologies and structural requirements. A more rational allocation of cath labs, based on the real need for procedures allows the optimization of the cardiovascular emergency network. According to the guidelines [12], even if surgery is not routinarily required, high-risk patients are clinically better served in cath labs with onsite cardiac surgery.
In conclusion, even if the optimal treatment is not established, the percutaneous coronary procedures supposed to be complex should preferentially be programmed in an onsite cardiac surgery center. If performed in an offsite cardiac surgery center, patients should be quickly sent for a full evaluation which takes account of the ongoing condition and of the potential corollary issues, not manageable in a cath lab.
Electronic supplementary material
(WMV 184 kb)
(WMV 254 kb)
Compliance with ethical standards
Funding
No funding was provided.
Consent
written consent was obtained from the patient involved.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
As it’s a retrospective case report, no ethical committee was required.
Statement of human and animal rights
This article is a case report regarding human participant and it does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lemmert ME, van Bommel RJ, Diletti R, et al. Clinical characteristics and management of coronary artery perforations: a single-center 11-year experience and practical overview. J Am Heart Assoc. 2017;6:e 007049. doi: 10.1161/JAHA.117.007049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994;90:2725–2730. doi: 10.1161/01.CIR.90.6.2725. [DOI] [PubMed] [Google Scholar]
- 3.Amat-Santos IJ, Martin-Yuste V, Fernández-Díaz JA, et al. Procedural, functional and prognostic outcomes following recanalization of coronary chronic total occlusions. Results of the Iberian registry. Rev Esp Cardiol (Engl Ed) 2019;72:373–382. doi: 10.1016/j.recesp.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Riley RF, Sapontis J, Kirtane AJ, et al. Prevalence, predictors, and health status implications of periprocedural complications during coronary chronic total occlusion angioplasty. EuroIntervention. 2018;14:e1199–e1206. doi: 10.4244/EIJ-D-17-00976. [DOI] [PubMed] [Google Scholar]
- 5.Al-Lamee R, Ielasi A, Latib A, et al. Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforation. JACC Cardiovasc Interv. 2011;4:87–95. doi: 10.1016/j.jcin.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 6.Briguori C, Nishida T, Anzuini A, Di Mario C, Grube E, Colombo A. Emergency polytetrafluoethylene-covered stent implantation to treat coronary ruptures. Circulation. 2000;102:3028–3031. doi: 10.1161/01.CIR.102.25.3028. [DOI] [PubMed] [Google Scholar]
- 7.Lansky AJ, Yang YM, Khan Y, et al. Treatment of coronary artery perforations complicating percutaneous coronary intervention with a polytetrafluoroethylene-covered stent graft. Am J Cardiol. 2006;98:370–374. doi: 10.1016/j.amjcard.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 8.Jamshidi P, Mahmoody K, Erne P. Covered stents: A review. Int J Cardiol. 2008;130:310–318. doi: 10.1016/j.ijcard.2008.04.083. [DOI] [PubMed] [Google Scholar]
- 9.Yeo KK, Rogers JH, Laird JR. Use of stent grafts and coils in vessel rupture and perforation. J Interv Cardiol. 2008;21:86–99. doi: 10.1111/j.1540-8183.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- 10.Pershad A, Yarkoni A, Biglari D. Management of distal coronary perforations. J Invasive Cardiol. 2008;20:E187–E191. [PubMed] [Google Scholar]
- 11.Ryan TJ, Faxon DP, Gunnar RM, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty) Circulation. 1988;78:486–502. doi: 10.1161/01.CIR.78.2.486. [DOI] [PubMed] [Google Scholar]
- 12.Bashore TM, Balter S, Barac A, et al. 2012 American College of Cardiology Foundation/Society for Cardiovascular Angiography and Interventions expert consensus document on cardiac catheterization laboratory standards update: A report of the American College of Cardiology Foundation Task Force on Expert Consensus documents developed in collaboration with the Society of Thoracic Surgeons and Society for Vascular Medicine. J Am Coll Cardiol. 2012;59:2221–2305. doi: 10.1016/j.jacc.2012.02.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(WMV 184 kb)
(WMV 254 kb)