Abstract
A 37-year-old lady presented with difficulty in breathing, which had progressively worsened in the last few months. Investigations revealed dextrocardia, congenitally corrected transposition of aorta, severe left atrioventricular valve stenosis with regurgitation, and right atrioventricular valve regurgitation. Left atrioventricular valve stenosis with thickening of leaflets and commissural fusion were suggestive of rheumatic valvular heart disease. She underwent left atrioventricular valve replacement and right atrioventricular valve repair with annuloplasty ring. This is a unique association of rheumatic valvular disease in corrected transposition of great arteries with dextrocardia. Morphology made surgical correction very challenging. Surgical correction of such case has not been reported in literature so far.
Keywords: Dextrocardia, Corrected transposition of great arteries, Rheumatic valvular disease
Introduction
Tricuspid valve stenosis (TS) is rare, affecting less than 1% of patients in developed nations and approximately 3% of patients worldwide. Most commonly, TS results from rheumatic heart disease, and accounts for most surgically excised stenotic tricuspid valves.
Case report
A 37-year-old lady presented with difficulty in breathing, progressively worsening in the last few months. She had history of rheumatic fever with joint pains in childhood and was on penicillin injection every 3 weeks, stopped for the last 5 years. Chest X-ray revealed dextrocardia, cardiomegaly, and congested lung fields. Electrocardiogram showed normal sinus rhythm. Two-dimensional echocardiogram was done which showed Cor triatriatum, severe left atrioventricular valve (LAVV) stenosis with moderate regurgitation (mean gradient − 10 mmHg; Max 23 mmHg) and moderate right atrioventricular valve (RAVV) regurgitation with severe pulmonary artery hypertension (PAH), right ventricular systolic pressure − 87 mmHg; normal biventricular function (Fig. 1). Magnetic resonance imaging revealed dextrocardia, situs solitus , congenitally corrected transposition of the great arteries (CCTGA), atrioventricular discordance, and ventriculoarterial discordance; LAVV stenosis with moderate regurgitation; and moderate RAVV regurgitation. Morphological right ventricle (RV) has normal chamber dimensions; left ventricular end diastolic dimension (EDD) 4.7 cm; left ventricular end systolic dimension (ESD) 2.9 cm; interventricular septum thickness at end diastole (IVSD) 1.0 cm; and left ventricular posterior wall thickness at end diastole (PWD) 1.0 cm. Morphological left ventricle (LV) was normal in size and signal intensity. Right atrium showed hypointense septum dividing the chamber into two quadrants, possibility of Cor triatriatum. Septum measures 0.5 cm in thickness. Left atrium was dilated and measured 5.5 cm in AP diameter (Fig. 2A, B). Operative findings were dextrocardia, large dilated heart, aorta anterior to pulmonary artery, CCTGA, mitral valve on right side with cleft anterior leaflet, moderate regurgitation: tricuspid valve on left side with severe stenosis and moderate regurgitation, no membrane in any atria, no Cor- triatriatum, LAVV had diffuse fibrous thickening of the leaflets with fusion of all commissures. Due to malposition, the ventricular mass lied in front of the atria and vena cavae, which made surgical access to the atria difficult. After establishing cardiopulmonary bypass with aortobicaval cannulation and Del Nido Cardioplegia, anatomy of heart examined. LAVV was replaced with bileaflet mechanical valve, preserving septal leaflet through left atrial approach, by operating from left side of patient. RAVV cleft was repaired and ring annuloplasty performed through right atrium by flipping the heart to left side, which oriented the valve upside down—mural leaflet on top and septal leaflet at bottom. She came off bypass in normal sinus rhythm with minimal inotropic support.
Fig. 1.
Echocardiogram showing LAVV stenosis
Fig. 2.
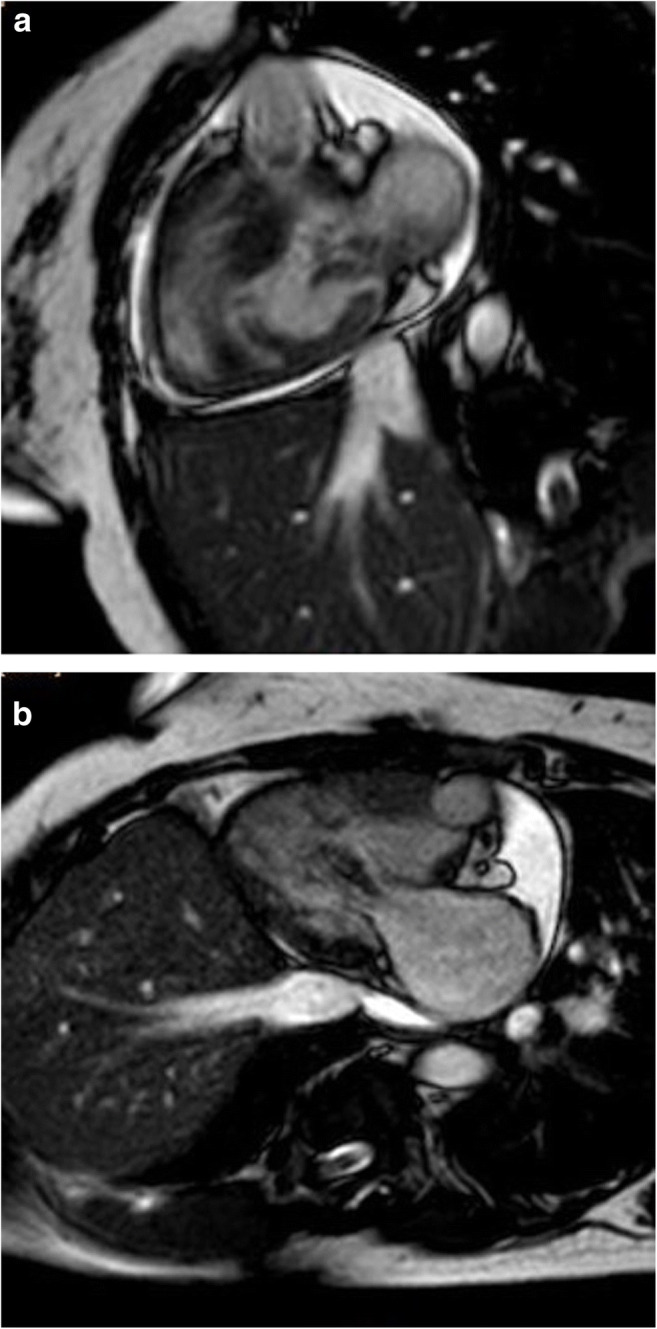
A MRI showing LAVV stenosis. B MRI showing RAVV regurgitation
She had uneventful postoperative recovery. Postoperative echocardiogram showed normal prosthetic valve function, no valve leak, and normal ventricular function. She had regular follow-up 1, 3, and 6 months after surgery. Last echo showed normal functioning prosthetic valve, no valvular and paravalvular leak, no RAVV, good LV/RV function. Mean gradient across LAVV − 3 mm.
Discussion
Incidence of CCTGA is less than 1% of all congenital heart defects and prevalence of 1/33,000 live births [1]. Mesocardia and dextrocardia occur in up to 20% cases of CCTGA. Systemic tricuspid valve lesions are present in up to 90% of patients with CCTGA [2, 3]. Around the 4th or 5th decade, symptoms of exercise intolerance and dyspnoea often develop and are mainly attributable to systemic atrioventricular incompetence and/or systemic ventricular failure [2–4].
TS is rare, affecting less than 1% of patients in developed nations and approximately 3% of patients worldwide. Most commonly, TS results from rheumatic heart disease, and accounts for most surgically excised stenotic tricuspid valves. Other less common causes of TS include congenital abnormalities (Ebstein’s anomaly; or isolated TS); metabolic or enzymatic abnormalities (Fabry’s disease, Whipple’s disease, carcinoid); or active infective endocarditis. Rheumatic tricuspid disease is characterized by diffuse fibrous thickening of the leaflets with fusion of two to three commissures [5]. Our patient had history of rheumatic fever in childhood and she was receiving penicillin injections; operative findings were suggestive of TS without any chamber dilatation in left sided ventricle.
There are very few case reports in literature [6, 7], but this is the first one to be reported which has undergone surgical correction. Also, RAVV had cleft, which made it unique.
Repair is seldom feasible because of the morphological abnormalities of tricuspid valves present in 90% of all CCTGA. Furthermore, if repair is attempted, high recurrence rate of tricuspid valve regurgitation is encountered [8]. Hence, we performed valve replacement with preservation of septal leaflet.
Patient has good biventricular function and severe PAH with preserved LV. Even though double switch operation with corrective valve surgery seems promising, it would be very challenging to do it in 3rd decade. Also, there are no long-term data showing its benefit over functional correction. Hence, we performed functional repair instead of anatomical correction.
Comments
We present here, very rare association of rheumatic valvular disease in patient with dextrocardia, corrected transposition of great arteries which was successfully managed surgically. Morphology made the operation very challenging. To our knowledge, it has not been reported in modern literature.
Compliance with ethical standards
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee.
Informed consent
Informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Samanek M, Voriskova M. Congenital heart disease among 815,569 children born between 1980 and 1990 and their 15-year survival: a prospective Bohemia survival study. Pediatr Cardiol. 1999;20:411–17. [DOI] [PubMed]
- 2.Graham TP Jr, Bernard YD, Mellen BG, et al. Long-term outcome in congenitally corrected transposition of the great arteries: a multi-institutional study. J Am Coll Cardiol. 2000;36:255–61. [DOI] [PubMed]
- 3.Prieto LR, Hordof AJ, Secic M, Rosenbaum MS, Gersony WM. Progressive tricuspid valve disease in patients with congenitally corrected transposition of the great arteries. Circulation. 1998;98:997–1005. [DOI] [PubMed]
- 4.Lundstrom U, Bull C, Wyse RK, Somerville J. The natural and “unnatural” history of congenitally corrected transposition. Am J Cardiol. 1990;65:1222–9 [DOI] [PubMed]
- 5.Waller BF, Howard J, Fess S. Pathology of tricuspid valve stenosis and pure tricuspid regurgitation—part II. Clin Cardiol. 1995;18:167–74. [DOI] [PubMed]
- 6.Parale GP, Jeurkar VN. Situs inversus with dextrocardia with corrected transposition of great vessels with rheumatic systemic atrio-ventricular valve regurgitation: A 63-year-old adult survivor. Indian Heart J. 1994;46:353–44. [PubMed]
- 7.Kukreti BB, Ramakrishnan S, Bhargava B. Situs inversus with levocardia and congenitally corrected transposition of great vessels with rheumatic tricuspid valve stenosis and regurgitation. Heart Views. 2011;12:178-80. [DOI] [PMC free article] [PubMed]
- 8.Scherptong RW, Vliegen HW, Winter MM, et al. Tricuspid valve surgery in adults with a dysfunctional systemic right ventricle: repair or replace? Circulation. 2009;119:1467–72. [DOI] [PubMed]



