Abstract
Residential gardens make up 30% of urban space in the UK, yet unlike many other green space typologies, their role in the health and well-being agenda has largely been overlooked. A horticultural intervention introduced ornamental plants to 38 previously bare front gardens (≈ 10 m2) within an economically deprived region of North England, UK. Measures of perceived stress and diurnal cortisol profiles (as an indicator of health status) were taken pre- and post-intervention (over 3 months). Residents reported significant decreases in perceived stress post-intervention. This finding was aligned with a higher proportion of ‘healthy’ diurnal cortisol patterns post-intervention, suggesting better health status in those individuals. All residents derived one or more reported socio-cultural benefits as a result of the front garden plantings, although overall scores for subjective well-being did not increase to a significant level. Further qualitative data suggested that the gardens were valued for enhancing relaxation, increasing positive emotions, motivation, and pride of place. The results indicate that adding even small quantities of ornamental plants to front gardens within deprived urban communities had a positive effect on an individual’s stress regulation and some, but not all, aspects of subjective well-being. The research highlights the importance of residential front gardens to human health and well-being, and thus their contribution to the wider debates around city densification, natural capital and urban planning.
Keywords: Cortisol, Deprivation, Socio-cultural Benefits, Stress Regulation, Urban Green Space, Wellbeing
1. Introduction
An increasing body of research demonstrates that urban green space (UGS) has therapeutic value by allowing city dwellers to relax and engage with nature (Frumkin et al., 2017, Hartig et al., 2014). Especially in urbanised societies, exposure to green space has been shown to generate positive benefits in emotional well-being (Ballew and Omoto, 2018, Roe and Aspinall, 2011), cognitive functioning (Bratman et al., 2019), behaviour (Guéguen & Stefan, 2016) and physiological responses, including heart rate variability, pulse rate, blood pressure, skin conductance, cortical brain activity and diurnal cortisol profiles (Haluza et al., 2014, Neale et al., 2019, Roe et al., 2013, Roe et al., 2017, Toda et al., 2013). Exposure to green space/nature has been linked to enhancement of the immune system (Hansen, Jones, & Tocchini, 2017) and encouraging physical activity (Cameron and Hitchmough, 2016, de Vries, 2010).
Despite policy-makers having a growing understanding of the value of UGS from a health and well-being perspective, challenges remain as to where and what type of UGS should be incorporated into city planning. Previous research implies that factors including scale, accessibility, quality, biodiversity and activity within UGS influence the relative health benefits (Dallimer et al., 2012, Fischer et al., 2018, Keeler et al., 2019, Wood et al., 2018). Several reports suggest that larger (Mitchell, Astell-Burt, & Richardson, 2011), more naturalistic landscapes (Stott, Soga, Inger, & Gaston, 2015) with greater biodiversity (Cameron et al., 2020) promote more positive health effects. This might suggest that planners should prioritise larger, more informal parks or nature reserves over other forms of UGS, when considering ‘therapeutic’ or health-promoting landscapes (Cameron et al., 2020). Yet recent epidemiological studies also indicate health indices improve when homeowners possess a garden (Brindley et al., 2018, Dennis and James, 2017). This implies that smaller, more intimate and readily accessible green space may also have a role in promoting health for urban citizens, and provide an alternative strategy to providing therapeutic space within the urban matrix.
Surprisingly, the value of residential gardens (also known as ‘domestic’, ‘private’ or ‘home’ gardens) as a health intervention has largely been overlooked (Cameron et al., 2012). In a review of UGS and mental health, only approximately 1% of studies involved residential gardens (Wendelboe-Nelson, Kelly, Kennedy, & Cherrie, 2019) and more information is required on the merits of this landscape type. Moreover, in the context of ever-increasing urbanisation and city densification, there is evidence that some city planners see residential gardens as a dispensable luxury (Haaland & Konijnendijk van den Bosch, 2015). Residential garden size is getting smaller, and some planners/developers are omitting gardens in new housing schemes completely (Tahvonen & Airaksinen, 2018). Yet this may be folly if such features are enhancing human health and well-being. Moreover, residential gardening is a common pastime with 49% of UK adults (Department for Culture Media and Sport, 2017) and 78% of USA homeowners taking part in regular garden activities (Clayton, 2007). Thus, gardening holds much promise as an intervention for health and well-being. Indeed, the value of private residential gardens as therapeutic landscapes was brought to the fore during the Covid-19 virus outbreak (Sofo & Sofo, 2020), where residents were socially isolated and the only green space that could be accessed for long periods of time, were private gardens (for those that possessed them).
Despite the dominance of residential gardening as an activity, much of the literature on gardening with respect to health and well-being actually relates to communal gardening on public or semi-public land, possibly because this is easier for researchers to access. Communal gardening covers community garden schemes, allotments, hospices, prison gardens and horticultural therapy interventions. Although the data is still not extensive, there is a greater evidence-base for benefits associated with communal gardening. These include improvements in: physiological relaxation (Hassan, Qibing, & Tao, 2018), stress relief (Genter, Roberts, Richardson, & Sheaff, 2015), mental health (Soga, Gaston, & Yamaura, 2017b), mood (Grahn & Stigsdotter, 2010), social skills (Himmelheber, Mozolic, & Lawrence, 2018), self-esteem (Cammack, Waliczek, & Zajicek, 2002), confidence (Eum & Kim, 2016), creativity (Exner & Schützenberger, 2018), diet (Hale et al., 2011), and opportunity for physical exercise (Soga et al., 2017a). Although it would be logical to assume that benefits associated with communal gardening translate across to residential gardening (Cervinka et al., 2016), this needs testing, not least as a number of reports suggest that much of the benefits of communal gardening relate to social interactions, encouragement from peers and pride in producing produce. Aspects that perhaps, may not be so relevant to private residential gardening, although residential gardens that are overlooked and enjoyed by neighbours or passers-by may have their own distinct socio-cultural influences.
The research presented here aims to address the gaps in knowledge relating to private residential gardens and to help inform policy-makers and planners about their potential value in terms of well-being and socio-cultural relations. This is important because not only are gardens being omitted in some new developments, but existing gardens are also changing in terms of their land cover, with many being paved over to facilitate ‘off-road’ car parking or ease maintenance (Chalmin-Pui, Griffiths, Roe, & Cameron, 2019). In the UK, 87% of households have gardens (Davies et al., 2009) equating to 5,300 km2 or 30% of the total urban area (Office for National Statistics, 2018), yet recent studies suggest as much as 38% of this area is now hard-surfaced, with some ‘gardens’ having no plants at all (Bonham, 2019). In reality, there is little understanding of how garden design, as well as type and extent of vegetation influences well-being (Lin et al., 2017). Our research specifically focused on small, residential front gardens associated with high-density housing stock as these are the ones most frequently paved over. It looked to investigate the effects of introducing ornamental landscape plants to paved front gardens and then determining effects on the residents’ health and well-being. Ornamental plants were used exclusively, i.e. food crops were avoided, to ensure impacts related to aesthetics (Haviland-Jones, Rosario, Wilson, & Mcguire, 2005) rather than additional material benefits, such as enhanced nutritional value or financial savings associated with growing the plants. Previous research has shown that there is a positive relationship between aesthetic preference and well-being (Hoyle et al., 2017a, Hoyle et al., 2017b). As the intervention was in front gardens, i.e. adjacent to the public streetscape, we were keen to determine if any wider socio-cultural benefits might accrue too, for example, any influence on neighbours.
The research examined diurnal profiles of the hormone cortisol, within the residents who took part. The physiological stress response in humans is regulated by the hypothalamic-pituitaryadrenal (HPA) axis and its synthesis of cortisol (Ryan et al., 2017). The circadian cortisol pattern in healthy individuals is typified by a rapid rise in cortisol production on waking in the morning, a steady decrease until mid-day, followed by a progressively slower decline until evening; with levels reaching their lowest point just prior to an individual falling asleep at night. Variations in this pattern can indicate HPA dysfunction, a consequence of a wide range of mental and physical health problems (Adam et al., 2017); for example, less rapid declines may suggest prolonged fatigue or exhaustion caused by chronic stress (Roe et al., 2013). Monitoring these diurnal profiles is important as simply calculating daily averages can be misleading – thus, for example, the assumption that high mean levels of cortisol correlate to enhanced stress and conversely low levels relate to stress-free conditions is an oversimplification (Smyth, Hucklebridge, Thorn, Evans, & Clow, 2013). We compared residents’ cortisol diurnal profiles (i.e. the decline phase of the circadian pattern) here, in an attempt to determine if the garden intervention influenced physiological responses. Healthier cortisol patterns have been cited previously for those living in areas with higher levels of green space (Gidlow et al., 2016, Roe et al., 2013, Ward Thompson et al., 2012) and for participants exposed to a forest setting compared to an urban one (Lee et al., 2011).
Based on the above evidence the research examined the following key questions
Will a front garden horticultural intervention - introducing plants to paved front gardens overtime (3 months) affect residents by:
Q1 Reducing perceived stress?
Q2 Improving diurnal cortisol profiles, suggesting better HPA function/health status?
Q3 Improving subjective well-being?
Q4 Increasing physical activity?
Q5 Improving connectedness to nature?
Q6 Providing socio-cultural benefits such as enhanced community cohesion?
2. Methods
A front garden intervention was carried out in an economically deprived region of North England, UK with plants and planted containers being introduced to resident’s properties. Pre- and post- well-being measures (subjective well-being, perceived stress, diurnal cortisol) were captured over a 2-week data collection period prior to and for at least 3 months after each intervention, with the experiment being repeated over a two-year period, using two sub-populations of residents (i.e. Groups A and B, Fig. 1 ).
Fig. 1.
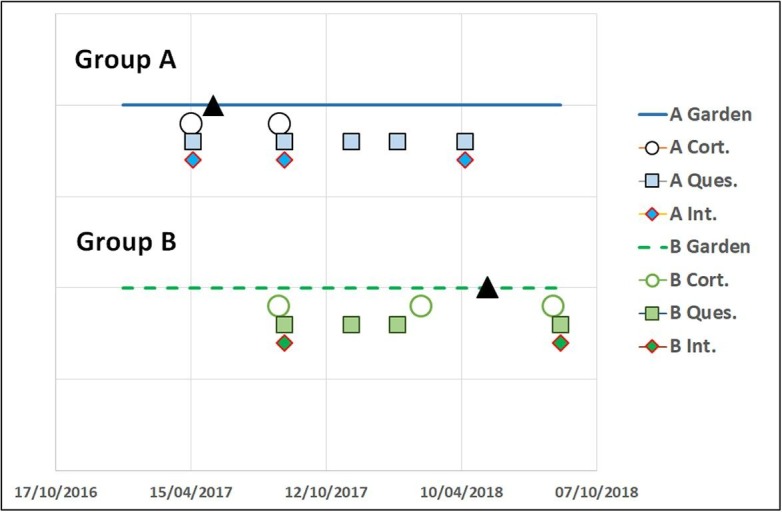
Timeline of engagement with residents. Group A (n = 25) received the garden intervention first (May 2017), with Group B (n = 17) acting as a Control. Group B received their own garden intervention in May 2018, allowing for a pre- and post- evaluation of this group, as well as for Group A. (▲=garden intervention; ○=cortisol samples; ■=questionnaires and ♦=interviews). Data was pooled for pre- and post-questionnaires due to not all residents completing questionnaires on each occasion. Where an individual resident repeated the questionnaire, e.g. after the intervention, then mean scores were used in the subsequent analyses.
2.1. Experimental design
Residents within Group A were provided with plants and containers first (May 2017), with Group B acting as a Control (i.e. a comparator group without plants/containers) over the subsequent summer and autumn. Residents within Group B received their intervention the following year (May 2018). Both groups were assessed on outcome measures pre- and post- the horticultural intervention (Fig. 1). The experimental design followed Reichardt (2006) “principle of parallelism” which recommends making multiple comparisons between groups over time (Mark & Reichardt, 2009). The quasi-experimental approach in a real-world setting acknowledged the lack of control over certain extraneous variables, including the lack of completely randomised groups (all residents showed some appetite to have a re-vegetated front garden).
2.2. Resident population and recruitment
The experiment was conducted in Salford, Greater Manchester, UK (Grid reference SJ 781999). Salford was chosen due to an abundance of 19th-century terrace houses, with small (10 m2) paved-over (non-vegetated) front gardens. The local housing association aided recruitment, with residents informed about the intervention via door to door leaflet dropping followed up via in-person door to door calls. Residents who participated were all selected from the same neighbourhood (within 4 km of each other), but divided into the two groups based on the street they lived in. Thus Group A (n = 25) was selected and pooled from 4 streets, and Group B (n = 17) derived and pooled from 4 different streets. This provided geographic separation between the two groups to avoid either group influencing the other. There was no geographic or obvious socio-economic bias associated with the group distributions, with all residents within socio-economic classes 6–8 in the National Statistics Socio-Economic Classification (i.e. employment status that varies from semi-routine work to long-term unemployed), and the neighbourhood ranked as within the 10% most deprived in the UK (Rose & Pevalin, 2003). Residents were selected on the basis of willingness to take part in a garden intervention that involved placing containers and plants in their front gardens.
2.3. The intervention
Participants received the same style of containers, range of plants and growing information, although the layout could vary based on the actual dimensions of individual front gardens or activities therein. For example, access to domestic bins, often situated in front of the property, had to be maintained. Residents were consulted on the types of plants they preferred and a standard list developed (Table 1 ), which were then used in the intervention (Fig. 2 ); all residents receiving the same plant taxa, the exception being choice of tree species - Amelanchier or Juniperus, or ability to decline a tree completely. Residents received one tree, one shrub, one climber, and enough sub-shrubs, bulbs, and bedding plants to fill the two containers. This provided diversity in structure, colour, and seasonality for each resident. Containers were planted by the researcher with no obligation for the resident to be involved with planting or subsequent management of these. All containers were ‘self-watering’ with a 22 L in-built reservoir of water. Although residents were not obliged to maintain the plants, active participation was encouraged and access to horticultural advice provided through the Royal Horticultural Society Advisory team. Residents were also given an information booklet written in a style accessible to non-gardeners.
Table 1.
Plant species/cultivar used in each garden.
| Plant type | Species/cultivar |
|---|---|
| Deciduous tree | Amelanchier canadensis ‘Glenn Form’ |
| Evergreen tree | Juniperus scopulorum ‘Blue Arrow’ |
| Shrubs | Rhododendron ‘Wombat’ |
| Climbers | Clematis ‘Jackmanii’ |
| Clematis ‘Ville de Lyon’ | |
| Sub-shrubs | Lavandula angustifolia ‘Hidcote’ |
| Rosmarinus officinalis Prostratus Group | |
| Geophytes (bulbs) | Galanthus nivalis f. pleniforus ‘Flore Pleno’ |
| Crocus sativus | |
| Narcissus ‘Tête-à-tête’ | |
| Bedding plants (annuals) | Petunia 'Surfinia Sky Blue' |
| Viola ‘Sorbet Series’ |
Fig. 2.
Typical garden design pre- (April 2017) and post-intervention (August 2017 & March 2018) with additional planted-up containers providing seasonal interest, and the option for residents to have one small tree planted.
2.4. Quantitative data sets and measured outcomes
A number of parameters were measured as indicators of health status through questionnaires and cortisol sampling and are linked to our original questions (Q1-4). These were-
Primary health outcome measures:
-
•
Perceived stress scale (Cohen, Kamarck, & Mermelstein, 1983) a 10-item scale scored on a Likert ranking of 5 (indicating higher stress) to 1 (indicating lower stress) (Q1).
-
•
Diurnal cortisol levels and profiles (Adam & Kumari, 2009 and see protocol outlined below) (Q2).
Secondary health outcome measures
-
•
Subjective well-being: Short Warwick and Edinburgh Mental Well-Being Scale - SWEMWB (Tennant et al., 2007); widely used in the health service sector with self-reported scores ranging from 7 (low) to 35 (high) mental well-being (Q3).
-
•
Physical activity levels (Likert 1–5 scale, 1 being inactive, 5 being fully active) (Q4).
The questionnaires were also used to provide additional information on connectedness to nature (Mayer & Frantz, 2004). This was a 14 item scale scored on a Likert ranking of 5 (completely agree) to 1 (completely disagree) relating to experiences of nature (Q5).
2.4.1. Protocol for salivary data collection
Salivary cortisol data was collected following the procedures outlined by Roe et al. (2013). This data allows the modelling of trends and changes in the daily lives of research participants (Schlotz, 2018). Diurnal cortisol profiles (declines after waking - see Introduction) were monitored by collecting saliva samples four times a day (3, 6, 9, and 12 h after waking) for each individual for two consecutive days with cotton swabs and Salivette collection tubes (Smyth et al., 2013). Participants were asked to confirm waking time on each day. To maximise participant adherence to the sampling protocol, they were subsequently sent SMS text reminders 30 min before a sample was due to avoid eating, drinking, or smoking (which can interfere with cortisol analyses), and when it was time to take the sample. Samples were stored in domestic refrigerators for up to 48 h before collection, then stored at −20 °C within a University laboratory prior to analysis. Cortisol concentration was determined by Enzyme Linked Immunosorbent Assay (ELISA) developed by Salimetrics LLC (USA). Assay characteristics: standard range = 0.33–82.77 nmol L−1, assay sensitivity = 0.19 nmol L−1 (lower limit of detection), correlation with serum cortisol = 0.91 (p < 0.0001, n = 47 samples). After centrifuging thawed samples at 3500 rpm for 10 min, duplicate analysis of samples was undertaken. The intra-assay coefficient of variation was < 10% for all samples.
Cortisol samples that indicated possible non-compliance with the sampling schedule were excluded following recommendations by Dmitrieva, Almeida, Dmitrieva, Loken, and Pieper (2013). These were extremely high values (≥60 nmol L−1) or samples that demonstrated a rapid increase from the previous value (≥10 nmol L−1). Four aggregate measures were calculated:
-
1.
Daily Average Concentration (DAC) (Nicolson, 2004), calculated as the daily mean of the four samples.
-
2.
Daily total secretion - Area Under the cortisol Curve with respect to ground level (AUCg), calculated using the trapezoid formula (Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003).
-
3.
Diurnal cortisol decline (slope profiles of cortisol curves)(Adam, Hawkley, Kudielka, & Cacioppo, 2006). Slope was calculated as the difference between cortisol concentrations at 12 and 3 h post-awakening.
-
4.
Proportion of healthy ‘i.e. normal’ diurnal cortisol profiles (Miller et al., 2016). Using discrete cortisol profiles (Dmitrieva et al., 2013), this assesses the proportion of curves that fit the normal diurnal cortisol profile. A cortisol profile is considered to be healthy if it peaks within the first hour of awakening, declines rapidly over the morning hours, and tapers off through the rest of the day, reaching its lowest point at night (Saxbe, 2008). Cortisol reference ranges were used to determine healthy diurnal cortisol profiles. Each resident’s raw diurnal cortisol profiles pre- and post-intervention were classified into one of four categories following Miller et al. (2016): 1) normal or healthy slope, 2) low slope, 3) irregular slope, 4) elevated evening slope. Changes in the number of samples showing a healthy profile were related to pre-/post-intervention times.
2.5. Additional questionnaire data
In addition to the formal scores generated for perceived stress, well-being, level of physical activity and connectedness to nature, the questionnaire also posed further questions relating to feelings of happiness, relaxation, anxiety or depression experienced over the period of the intervention (Q3); and any changes in social-cultural aspects such as perceptions about the local community or neighbourhood (Q6) or connectedness to nature (Q5). These complemented qualitative data collected via interview (see below).
2.6. Qualitative data collection
Qualitative data was collected through semi-structured in-depth interviews, before and after the intervention. Data included how residents felt about their lives, well-being, mental and physical health, street, neighbourhood, community, engagement with nature and gardening, attitudes towards the intervention, motivations for participation in the research and expectations regarding the outcomes of the intervention. Throughout the study period, additional qualitative data was collected about alterations to gardens (both experimental and otherwise) and based on informal conversations with passers-by and neighbours.
2.7. Data analysis
Residents were inconsistent in their responses to requests for questionnaire or salivary cortisol data, resulting in a larger population in Group A, than Group B (Table 2 ). As such, data for cortisol was pooled across both groups before comparing profiles pre- (2 weeks before) to those post-intervention (3 months after). Similarly, for well-being and perceived stress, data was pooled across the groups to allow for robust analysis of pre- and post-intervention effects. Missing datasets did not fit a pattern, and tended to be related to individuals forgetting to provide samples or not being at home when interviews had been arranged. There was no evidence that any particular socio-economic or health factors were influencing the data sets (e.g. missing values were not restricted to those with the poorest health), so although statistical power was reduced, no obvious bias was linked with this loss of data. A range of statistical tests (using ‘R’ version 3.4.3) were employed, as appropriate to the data, to determine statistical significance of the intervention. These included paired t-tests, McNemar's test, linear modelling, single and repeated measures ANOVA for pre- and post-intervention evaluation; a difference-in-difference regression model was used to compare results from intervention and control groups across different times. (Table 3 summarises the tests used for each parameter). Where appropriate to do so, statistical power was increased by augmenting with additional individuals who provided data at relevant time points or restricted comparisons (see n values below for each specific statistical test/model used in the results section).
Table 2.
Sample sizes for questionnaires and cortisol evaluations.
| Subjective well-being/socio-cultural (n = 42) | Diurnal cortisol (n = 31) | |||
|---|---|---|---|---|
| Complete responses | Pre and post | Only pre or post | Pre and post | Only pre or post |
| Group A | 14 | 11 | 8 | 8 |
| Group B | 14 | 3 | 8 | 7 |
| Total | 28 | 14 | 16 | 15 |
Table 3.
Specific statistical tests applied to the different measured parameters.
| Parameter measured | Statistical test employed |
|---|---|
| Demographics data | Fisher test for proportions |
| Perceived stress (PSS) (Q1) | Paired t-test |
| One way ANOVA to compare Aug 2017 data only | |
| A difference-in-difference regression model to compare the two populations over time | |
| Subjective well-being (SWEMWB) (Q3) | Paired t-test |
| Physical activity (Q4) | Paired t-test |
| Connectedness to nature (Q5) | Paired t-test |
| Diurnal salivary cortisol concentrations (Q2) | Repeated measures ANOVA (Log-transformed) |
| Salivary cortisol - Daily Average Concentration (DAC) (Q2) | Paired t-test |
| Simple linear regression (Log-transformed) | |
| Salivary cortisol – Total daily secretion (AUCg) (Q2) | Paired t-test |
| Simple linear regression | |
| Two-way repeated measures ANOVA (to determine effects of sampling time) | |
| Salivary cortisol concentration decline correlated with mental well-being (SWEMWB) (Q2 & Q3) | Simple linear regression |
| Proportion of normal diurnal cortisol profiles (Q2) | McNemar's test |
In the process of this statistical analysis, model checking was performed by consideration of standardised predicted values, standardised residuals and whether the data met the assumptions of homogeneity of variance and linearity. Transformations were carried out where appropriate to ensure compliance with these assumptions. For example, to correct for a positive skew in the cortisol data, data was log-transformed prior to statistical analysis.
Longitudinal qualitative data were analysed using interpretative phenomenological analysis (Smith, Jarman, & Osborn, 1999) with time (pre- and post-intervention) as the main topic of inquiry. To maintain anonymity yet provide context, residents are cited using their gender and age to illustrate the emerging emotional themes.
3. Results
After a total of 237 house-approaches, 42 (13%) residents took part in the research with the majority of residents (93%) being white (Table 4 ). Four residents who took part, co-habited, thus there were 38 horticultural interventions in total. Only 17 residents chose to have a tree planted (40%). Beyond watering, 14 residents actively engaged with their new gardens, such as deadheading flowers or adding plants (33%). In terms of data collection, 28 residents in total (14 Group A; 14 Group B) completed pre- and all post- interviews/questionnaires and 16 (8 Group A; 8 Group B) provided complete cortisol profiles pre- and post- the intervention.
Table 4.
Demographics (number and percent) of residents and significance level for comparisons within factors (p-values).
| Total | Group A | Group B | P-value | |
|---|---|---|---|---|
| N = 42 | n = 25 | n = 17 | ||
| Gender | 0.74 | |||
| Female | 27 (64%) | 17 (68%) | 10 (59% | |
| Male | 15 (36%) | 8 (32%) | 7 (41%) | |
| Age | 0.70 | |||
| 18–24 | 2 (5%) | 1 (4%) | 1 (6%) | |
| 25–34 | 7 (17%) | 6 (24%) | 1 (6%) | |
| 35–44 | 13 (31%) | 6 (24%) | 7 (41%) | |
| 45–54 | 11 (26%) | 6 (24%) | 5 (29%) | |
| 55–64 | 6 (14%) | 4 (16%) | 2 (12%) | |
| 65–74 | 2 (5%) | 1 (4%) | 1 (6%) | |
| 85 or older | 1 (2%) | 1 (4%) | 0 (0%) | |
| Ethnicity | 1.0 | |||
| African/Caribbean/ Black | 1 (2%) | 0 (0%) | 1 (6%) | |
| Arab | 2 (5%) | 1 (4%) | 1 (6%) | |
| White | 39 (93%) | 24 (96%) | 15 (88%) | |
| Education | 0.71 | |||
| GCSE | 11 (26%) | 7 (28%) | 4 (24%) | |
| A Levels | 7 (17%) | 5 (20%) | 2 (12%) | |
| Foundation degree | 4 (10%) | 2 (8%) | 2 (12%) | |
| Other qualification (e.g. teacher training, nursing…) | 6 (14%) | 3 (12%) | 3 (18%) | |
| Bachelors degree | 3 (7%) | 1 (4%) | 2 (12%) | |
| Masters degree | 1 (2%) | 0 (0%) | 1 (6%) | |
| Doctorate | 1 (2%) | 0 (0%) | 1 (6%) | |
| No response given | 9 (21%) | 7 (28%) | 2 (28%) | |
| Net annual income (£) | 0.18 | |||
| <15,000 | 15 (36%) | 11 (44%) | 4 (24%) | |
| 15,000–25,999 | 10 (24%) | 4 (16%) | 6 (35%) | |
| 26,000–34,999 | 7 (17%) | 5 (20%) | 2 (12%) | |
| More than 70,000 | 1 (2%) | 0 (0%) | 1 (6%) | |
| No response given | 9 (21%) | 5 (20%) | 4 (24%) | |
| Employment status | 0.75 | |||
| Employed full time | 16 (38%) | 8 (32%) | 8 (47%) | |
| Employed part time | 12 (29%) | 7 (28%) | 5 (29%) | |
| Self-employed | 2 (5%) | 2 (8%) | 0 (0%) | |
| Retired | 5 (12%) | 3 (12%) | 2 (12%) | |
| Unemployed | 7 (17%) | 5 (20%) | 2 (12%) | |
| Tenure | 0.015 | |||
| Resident owner | 18 (43%) | 7 (28%) | 11 (65%) | |
| Tenant | 23 (55%) | 18 (72%) | 5 (29%) | |
| Lodger | 1 (2%) | 0 (0%) | 1 (6%) | |
3.1. Quantitative data - perceived stress, well-being (SWEMWB), physical activity and connectedness to nature scores
Pooling data across both groups (n = 28) showed there was a significant decrease in perceived stress post-intervention, (paired t-test, t(27) = -2.44, p = 0.021; Q1) (Fig. 3 ). There were no significant effects though on subjective well-being (Q3), physical activity (Q4) or connectedness to nature scores (Q5).
Fig. 3.
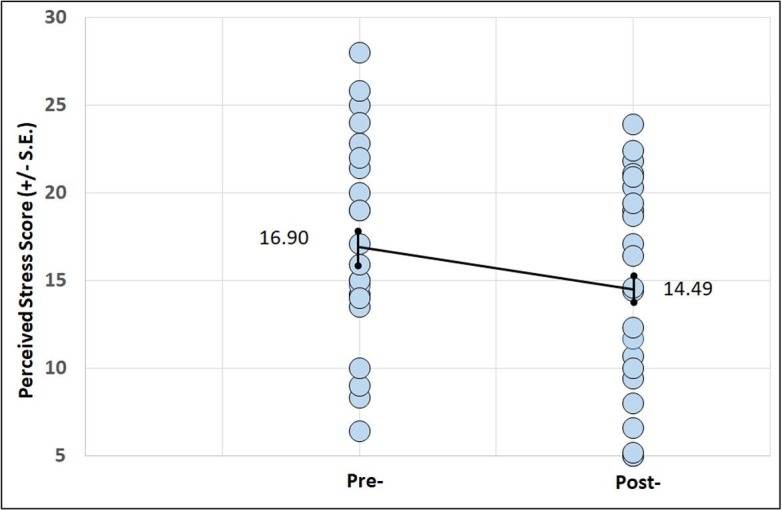
Mean perceived stress pre- and post-intervention (n = 28). Bars represent standard error (S.E.).
Restricting data to a single period (Aug 2017) when Group A (after the intervention) could be compared to Group B (control, i.e. no intervention) at the same time, resulted in mean perceived stress levels of 13.4 and 16.9, respectively. ANOVA showed this to be only significant, however at a 10% level, i.e. p = 0.092; possibly partially attributed to low replication (n = 17).
A difference-in-difference regression model showed that perceived stress levels overall decreased by 3.18 in the intervention group, whereas stress levels actually rose by 4.52 in the control group (Fig. 4 ). Although this result is not statistically significant (p = 0.129), it does suggest that the engagement with the researcher alone (control group) had no positive effect on perceived stress scores.
Fig. 4.
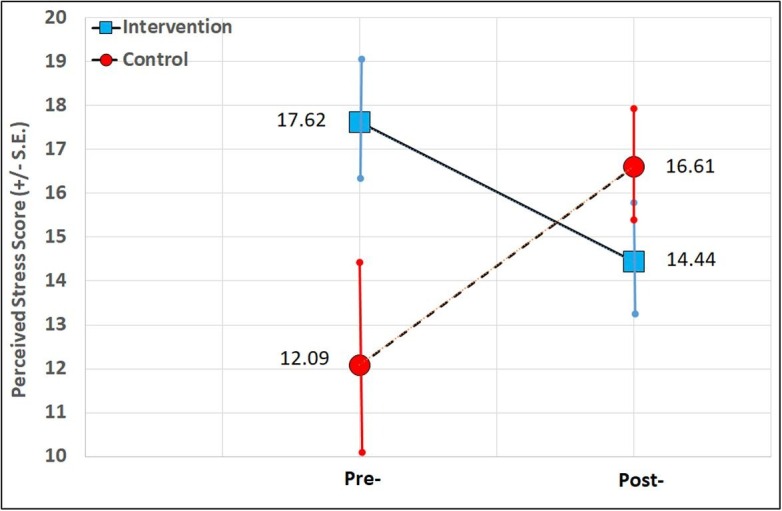
The effect of the front garden intervention on participants using differences-in-differences estimation (n = 23). Bars represent standard error (S.E.).
3.2. Cortisol measures
3.2.1. Diurnal salivary cortisol concentrations
A repeated-measures ANOVA factoring sample day and sample time revealed no significant order effect for day 1 or 2 of sampling using log-transformed values (n = 31). There was a significant main effect of sampling time (F = 4.39, df = 1, p = 0.037), indicating that cortisol means varied across the day. Both results suggested participant adherence to the required sampling protocol and legitimised averaging cortisol variables (DAC, AUCg and diurnal decline) across the two sampling days to give the most reliable measures (Roe et al., 2013).
3.2.2. Daily average concentration (DAC)
A paired t-test run on the residents with measures both pre- and post-intervention (n = 16) showed a marginally non-significant effect, with pre-intervention concentrations (3.01 nmol L−1 ± 0.51) lower than post-intervention ones (4.51 ± 0.59), t(15) = 1.99, p = 0.065. Further evaluations using simple linear regression (log-transformed values) indicated a significant relationship between the pre-/post- factor and DAC (t = -2.805, p = 0.006). DAC increased by 21% from pre- to post-intervention, and the adjusted r 2 value showed that 6.9% of the variation in DAC can be explained by the model, (p = 0.006). Before the intervention cortisol levels tended to be very low (≈3-4 mol L−1), but were higher post-intervention (≈4-6 mol L−1) (Fig. 5 ). These post-intervention values were closer to reference ranges from healthy participants of similar age and socio-economic status as this sample (Smyth et al., 2019).
Fig. 5.
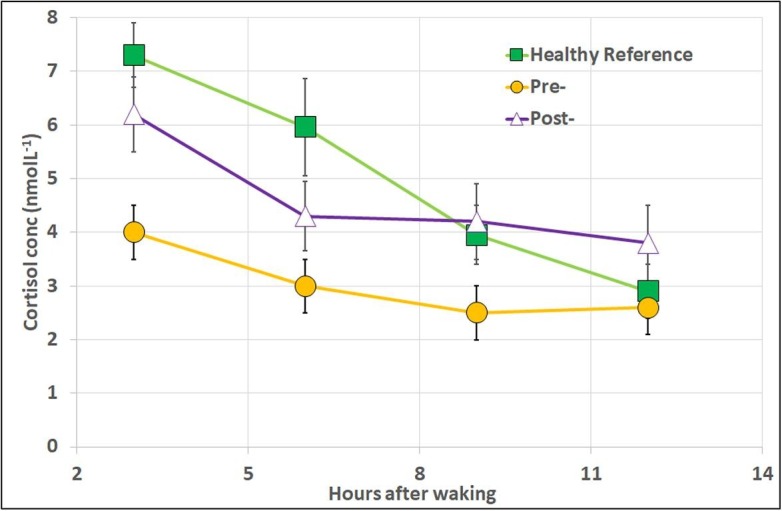
Salivary cortisol concentrations (mean ± standard error) pre- and post-intervention (n = 16). Data for healthy participants from laboratory reference data and included for illustrative purposes; n = 26, 15 women and 11 men aged 48.6 ± 11.7 years (but also see Smyth et al., 1997, Smyth et al., 2013, Smyth et al., 2019). Bars represent standard error (S.E.).
3.2.3. Total daily secretion (AUCg)
A paired t-test on AUCg data (n = 14) showed residents significantly increased their total secretion post-intervention (AUCg = 28.37 ± 3.63), compared to pre-intervention (AUCg = 18.60 ± 2.98); t(13) = 2.27, p = 0.041. Again linear regression showed a significant relationship between the pre-/post- factor and AUCg (t = -3.488, p < 0.001) with 13% of the variation in AUCg being explained by the model (p < 0.001).
3.2.4. Diurnal cortisol decline (cortisol slope profiles)
A paired t-test (n = 13) conducted on the diurnal decline (difference between concentrations at 12 and 3 h post-awakening) indicated that declines were significantly steeper post- (-3.40 ± 1.09) than pre-intervention (-2.52 ± 0.534); t(12) = -2.34, p = 0.038. Linear regression though, did not show a significant relationship between the pre-/post- factor and cortisol decline (t = -1.79, p = 0.078).
A two-way repeated measures ANOVA (n = 13) was also conducted to determine the effects of time (pre-or post-intervention) and sample (3 or 12 h post-awakening) on cortisol. This showed there was a significant two-way interaction between the effects of time and sample on cortisol: F(1, 13) = 5.112, p = 0.042; suggesting values were different at 3 h, but not necessarily at 12 h post-awakening (Fig. 5).
The cortisol decline post-intervention was strongly-negatively correlated with well-being scores. This was significant (r = -0.67, n = 14, p = 0.006); cortisol profiles in participants with higher well-being scores showed a steeper decline in cortisol concentration and in line with what would be expected in healthy individuals.
3.2.5. Proportion of healthy diurnal cortisol profiles
For residents providing both pre- and post- diurnal cortisol profiles (n = 16), the proportion of healthy slopes rose from 24% pre-intervention to 53% post-intervention. An exact McNemar's test showing this change to be significant, χ2 = 5.56, p = 0.018.
3.3. Additional questionnaire data
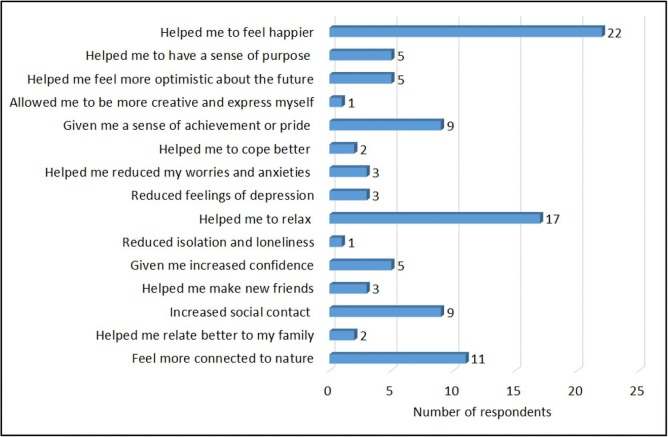
Analysing all post-intervention questionnaires (n = 42, i.e. pooling data across those that had and had not completed a pre-intervention questionnaire) indicated all residents (100%) felt somewhat or extremely happy with their new front garden, and 100% also reported that their health or well-being had improved as a result of the intervention. Twenty-two residents (52%) reported that the garden helped them to feel happier, 17 residents (40%) reported that the garden helped them to relax, and 11 residents (26%) reported that the garden made them feel more connected to nature (Fig. 6 ). Relatively few residents (3), however, reported that the gardens directly reduced feelings of depression, worry or anxiety. Moderate numbers reported an increased sense of pride (9) and more social contacts (9) through the questionnaire.
Fig. 6.
Responses from residents to the questionnaire (n = 42) following the horticultural intervention.
3.4. Qualitative data collection
Four key themes emerged from the qualitative data analysis (interviews). Introducing plants elicited feelings related to motivation, relaxation, pride and positive emotions.
3.4.1. Motivation
The intervention motivated residents to engage with their new planters, add additional plants (10 residents) or garden furniture, and renovate other parts of the house/garden. One participant (male, 60) bought a paddling pool for his dog to play in, while spending time in the front garden. A participant with paranoid schizophrenia described the importance of seeing positive change for her home:
“It's the one part of the house that's nice at the moment, so it makes a difference. It definitely makes you think about the rest of the house and getting on top of things, so I'm having the back garden done next week. It's started me off; if you get a lift up, it sort of spurs you on. It definitely gets you motivated a bit more” - Female, 42.
Residents also stated they were encouraged by the responsibility to care for the plants. This was especially the case for residents with chronic depression and other mental illnesses, who appreciated change in small steps. One participant described feeling “like a normal human being” when seeing the plants outside her door (female, 51). The intervention influenced neighbours who had not directly participated in the research, and these purchased plants, containers and artificial grass for their own properties. One resident requested a ‘plant list’ so she could have a matching display for her own front garden.
3.4.2. Relaxation
The majority of residents reported that it was relaxing to view the plants, come home to them, and watch them grow.
“One of the big things that I've noticed, is when I come back from work and see all the daffodils, it switches me into home mode. It's like a buffer zone between work and home.” - Male, 37.
One participant caring both for her ill mother and granddaughter amidst her own relationship problems, explained that sitting on her front step, next to the plants, with her morning coffee helped her cope when she did not otherwise have time for herself (female, 42).
3.4.3. Pride
The new plantings gave residents a sense of pride in their home. The interventions took place in areas with frequent fly-tipping and theft. A large proportion of participants explained that the “nice planters” would improve people’s perception of the area, as well as their own.
“You don't want visitors to think you live in a dump, you don't want them to pity you. […] It gives you pride, not just in your house but in the whole area. It makes it look like your area has not just been left to rot.” - Male, 40.
Residents noted that the colourful planters became an indicator of care, and a catalyst to pay more attention to the neighbourhood. One resident (male, 47) was inspired to become a local council ‘street champion’ and took part in litter picks. This improved ‘sense of pride’ was cited as improving communication between residents and contributing to a genuine sense of community. Some residents also felt an increased sense of responsibility for the plants themselves.
“It is quite relaxing, but I never thought I'd say this. I'm quite attached to them now. It sounds weird because they're only plants, but they're not. They're mine. And they are living things, so you've got to look after them. It's like having a little pet.” Female, 37.
3.4.4. Positive emotions
All residents reported that the plants made them feel more cheerful and lifted their emotions when viewing them. They talked about better moods upon leaving/returning to the house. Though experienced by all, qualitative assessment of emotional intensity during interviews suggested that this was most acutely appreciated by people struggling with poor mental health.
“It’s lovely. It really cheers me up, honestly […] I love nature, and I see so little of it. So every time I get out of the house, I get a little wave of pride. It gives me a lift, a little swing in my step. Every time.” - Female, 51.
The importance of the visual impact/flower colour was explained by several residents, and residents’ home visitors also noticed the changes.
“It’s just nice to see the different colours. Otherwise, it looks dead bare. It made me feel brighter in myself” - Female, 86.
4. Discussion
4.1. Results that support health, well-being and socio-cultural benefits
Results from the intervention support the notion that small-scale ornamental plantings improved residents’ mood and self-reported health with respect to perceived stress (Fig. 3). Improvements in participant self-reported data were supported by aggregate measures of salivary cortisol concentrations, with a number of cortisol parameters suggesting significant improvements in cortisol patterns and traits associated with better health (Q2) (6 out of 8 of our cortisol analyses showed a statistically significant difference at the 5% level).
The significantly steeper declines in cortisol slopes observed post-intervention indicate better health through more effective regulation of circadian and hormonal mechanisms, i.e. a likely consequence of reduced stress. The proportion of cortisol curves showing a healthy pattern increased significantly (by 29%) after plants were provided to residents. Indeed, empirical values post-intervention (53% normal) were comparable to other studies for healthy individuals in similar demographic groups (Ice et al., 2004, Ryan et al., 2017, Smyth et al., 1997).
Improvements in cortisol profiles were mirrored by significant increases in total daily cortisol secretion (AUCg) after the horticultural intervention. Very low values of AUCg are often associated with chronically low socio-economic status and poorer health (Desantis, Kuzawa, & Adam, 2015), and increases in this parameter also suggest improvements in health status. Finally, we noted an increase in the daily average concentrations (DAC) of cortisol after the intervention, again to levels consistent with populations of healthy individuals. Higher DAC is associated with a higher cortisol awakening response, which in turn has been linked to lower perceived stress (O’Connor et al., 2009).
Overall our data suggests that for this population cortisol levels and profiles were considered ‘healthy’ post-intervention, but indicated poor health status pre-intervention (Smyth et al., 2019). Indeed, the ‘blunted’ cortisol levels below reference ranges encountered pre-intervention are linked to depression (Adam et al., 2017), post-traumatic stress disorder (Bechard, 2017), suicide attempts (Keilp et al., 2016) and childhood adversity (Koss & Gunnar, 2018) through the down-regulation of the hypothalamic-pituitaryadrenal (HPA) axis after prolonged exposure to chronic stress. Overall, the increase in the number of cortisol curves with a healthy pattern after the intervention suggests that more residents were experiencing less HPA fatigue, stress, anxiety, sleep disturbances, or irritability. Comparing the data on perceived stress in this study to others, the positive effects due to the horticultural intervention were approximately equivalent to 8 weekly mindfulness sessions (as measured after 6 months) (van Wietmarschen, Tjaden, van Vliet, Battjes-Fries, & Jong, 2018). Thus, the data addresses Q1 and Q2, indicating the intervention reduced perceived stress levels, improved cortisol profiles and thereby had a positive effect on the residents’ health status.
Although there was no significant increase in SWEMWB scores per se (Q3), lower perceived stress and positive physiological responses after the planting intervention were supported by positive statements in the questionnaire. All 42 residents reported that their health or well-being had changed for the better due to the new front gardens; the gardens were also reported to help residents feel happier (52%), more relaxed (40%) or more connected to nature (26%) (Fig. 6). Moreover, many or the qualitative personal statements clearly articulated the positive influence the gardens had on peoples’ outlook on life, with strong themes developing around more positive attitudes in general, a sense of pride and an enhanced motivation to improve the local environment, as well as the gardens being valued as a place to relax. Therefore, there is some evidence the intervention provided socio-cultural benefits (Q6).
4.2. Results that do not support health, well-being and socio-cultural benefits
The intervention did not show any significant differences on either subjective well-being (SWEMWB) (Q3), enhanced physical activity (Q4) or connectedness to nature outcome measures (Q5). The lack of direct relationship between the horticultural intervention and subjective well-being score is surprising; especially as it at odds with the data on stress, a potential precursor of certain aspects of poor mental health (Toussaint, Shields, Dorn, & Slavich, 2016). This suggests that the intervention might relieve stress, but not necessarily be influencing other aspects of well-being, such as feeling loved or having increased confidence (aspects covered within the SWEMWB scoring). Certainly, other studies on therapeutic gardens and engagement with nature have suggested that there can be misalignment between the positive effects on day to day stress management and such activities being an antidote to deeper or longer-term mental health problems (Toussaint et al., 2016).
The lack of any enhancement in connectedness to nature score (Q5) from the intervention is interesting too. This may partially due to the fact that the residents who chose to take part, already had some desire to have plants in their garden, possibly suggesting a higher nature connection level than a genuinely random control group. This skew in participants may be one reason why the nature connection measure did not change from pre-installation to post.
It is also possible that an interest in gardening and nature connectedness are not exactly aligned. Although on the one hand, gardening, is by definition, working and being in close proximity to nature through the medium of plants (and predominately cultivated forms of plants), it is not necessarily engagement with ‘wild nature’ per se. We saw no strong evidence of residents showing wider engagement with other aspects of urban wildlife, or mentioning taxa other than plants. It is possible that the horticultural intervention was inducing positive affect, as indicated by the qualitative data, but not necessarily just that associated with biophilic responses (Wolf, Ermgassen, Balmford, White, & Weinstein, 2017) or biodiversity (Richardson, 2019). Gardens have been linked to an enhanced sense of self-worth through the opportunity for increased creativity, and self-expression (Clayton, 2007). As mentioned above, they can also be a source of pride (Clayton, 2007) or improve a sense of place (Freeman, Dickinson, Porter, & van Heezik, 2012) as this study confirms. These positive aspects of gardens in socio-cultural terms require further investigation using additional outcomes measures that capture these dimensions.
4.3. Implications for gardens and health
As far as we are aware, this is the first study to evaluate the health benefits of a small-scale front garden horticultural intervention. Moreover, the research was innovative in that ornamental landscape plants were used exclusively in an attempt to differentiate responses based on emotion to those of material need (i.e. food). Many previous garden studies indicate food crops were grown, yet the motivations to grow food and non-food plants may be different. The focus here was purely on an aesthetic transformation to the front garden.
Taken in the round, these datasets indicate the horticultural intervention reduced the level of stress in residents (as captured by both self-reporting Q1 and a physiological biomarker Q2) at least in the short-medium term (over a 3 month period).
The positive findings from this study have wider implications for urban planning. As outlined above, there is a trend in urban planning to save space by providing housing with little or even no garden space (Ltd, 2007). Most research on salutogenic aspects of UGS have focussed on parks (Wolf & Wohlfart, 2014), nature reserves (Adjei & Agyei, 2015) and urban forests (Panagopoulos, González Duque, & Bostenaru Dan, 2016), including trees close to residential properties (Taylor, Wheeler, White, Economou, & Osborne, 2015) and policy makers are beginning to acknowledge the value of such spaces in this respect (Lee, Jordan, & Horsley, 2015). Policymakers and planners should not feel, however, that such places can necessarily directly substitute for private gardens and the health benefits they provide. Private gardens are distinct from other forms of UGS in a number of important ways. They provide an opportunity for citizens to engage with the natural world in an immediately accessible manner, while also being imbued with social and cultural elements. The privacy component alone allows autonomy and opportunities to be creative or reflective in a way that would rarely be feasible in public UGS. Even the social dynamics around domestic gardens may be different from that of communal gardens or allotments, despite the physical activities being very similar. They are also intrinsically linked with the domestic property and can enhance (or if poorly maintained, undermine) the sense of pride that can be aligned with homeownership. One of the principal findings from this research was the capacity for ornamental gardens to provide an immediate, accessible and easily sought place for relaxation. In effect, an important location for some ‘down time’ and a place to find respite from the stress and strains of urban life. The surprising element, perhaps, was how little green space was actually required to accrue these benefits.
4.4. Limitations of the study
The key limitation was attrition in sample size over time; a common problem in longitudinal studies. The logistics of carrying out a longitudinal study in a deprived urban community included participants’ failure to respond at specific sampling times, forgetting to take samples or meet for interviews (despite being prompted). Data was tested to ensure those residents who omitted samples/missed interviews were not atypical of the population in general. For example, residents who dropped out were not correlated with more irregular cortisol profiles than those who finished the evaluation. Further studies, however, should take care to ensure that later omissions are not in themselves associated with poorer health or greater stress levels. It is recommended that similar studies are conducted with larger sample sizes for higher sample power.
The horticultural intervention relied on a relatively small volume of new plantings, and was facilitated by both the local housing association and the Royal Horticultural Society. Questions remain as to the impact of the number of plants used, garden style adopted, and social context (community grassroots initiatives vs. top-down local authority programmes). It should also be noted that although our data showed a positive trend between the garden intervention and i. perceived stress, ii. cortisol profiles that relate to less stress and iii. improvements in mood (trends not found in our control population), sample sizes were small, and we cannot categorically claim ‘cause and effect’; other factors external to the project could also have been influencing these trends. Although our groups A and B were chosen to be similar in socio-demographics, and by and large were, there was a higher proportion of homeowners in group A than B (as compared to tenants), and this may have influenced results. Further research is required to note any particular influences in owning a garden as to managing one that is part of a rented property.
Finally, data from the connectedness to nature section of the questionnaire did not correspond well to some people’s response to their own garden and this may relate to a mismatch between larger, theoretical components around nature and the more intimate feelings residents had for their familiar, small scale ‘patch’. For example, residents may rarely have considered their garden when trying to address questions such as “When I think of my place on Earth, I consider myself to be a top member of a hierarchy that exists in nature”. Perhaps a stratified or modified questionnaire is required when attempting to assess affinity to green space or urban nature per se?
5. Conclusions
The data presented suggests that adding plants and containers to residents’ front gardens was associated with significant reductions in perceived stress (Q1) which was reflected in improved diurnal cortisol patterns (Q2) post-intervention (i.e. steeper diurnal declines, increased daily average concentration and total secretions compared to ‘blunted’ levels pre-intervention). Qualitative data also showed residents being happier, more relaxed, and having greater motivation to improve and feel a sense of pride in their living environment. We did not detect a significant improvement, however, in the subjective well-being scale – SWEMWB post-intervention (Q3). In reality, it may be that certain components of well-being were improved but not others. Data from the study also indicated that there were some socio-cultural benefits associated with the intervention (Q6), for example being more motivated and taking a greater sense of pride in the home-environment and neighbourhood. Gardening has been quoted as ‘therapeutic’, but we believe this is the first empirical study to demonstrate that enhancing a residential garden through planting has a positive impact on stress regulation. The study highlights the importance of residential gardens as a potential resource for public health and the need for gardens to be brought more forcefully into the debates around housing, city densification, and the value of different types of green infrastructure. On a national, regional, and city scale, residential gardens could provide a public health benefit by contributing to preventing mental ill-health.
Funding
This research was funded by the Royal Horticultural Society, with contributions from ForHousing and United Utilities. The authors declare no conflict of interest.
References
- Adam E.K., Hawkley L.C., Kudielka B.M., Cacioppo J.T. Day-to-day dynamics of experience - Cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam E.K., Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Adam E.K., Quinn M.E., Tavernier R., McQuillan M.T., Dahlke K.A., Gilbert K.E. Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2017;83:25–41. doi: 10.1016/j.psyneuen.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adjei P.O.W., Agyei F.K. Biodiversity, environmental health and human well-being: Analysis of linkages and pathways. Environment, Development and Sustainability. 2015;17(5):1085–1102. doi: 10.1007/s10668-014-9591-0. [DOI] [Google Scholar]
- Ballew M.T., Omoto A.M. Absorption: How nature experiences promote awe and other positive emotions. Ecopsychology. 2018;10(1):26–35. doi: 10.1089/eco.2017.0044. [DOI] [Google Scholar]
- Bechard B. Translocator protein (18kDa) downregulation contributes to low cortisol and neurosteroid levels in patients with post traumatic stress disorder. Medical Hypotheses. 2017;104:72. doi: 10.1016/j.mehy.2017.05.019. [DOI] [PubMed] [Google Scholar]
- Bonham, C. (2019). Green spaces in residential gardens. Retrieved July 23, 2019, from Data Science Campus, Office of National Statistics website: https://datasciencecampus.ons.gov.uk/projects/green-spaces-in-residential-gardens/.
- Bratman G.N., Anderson C.B., Berman M.G., Cochran B., de Vries S., Flanders J., Folke C., Frumkin H., Gross J.J., Hartig T., Kahn P.H. Nature and mental health: An ecosystem service perspective. Science Advances. 2019;5(7) doi: 10.1126/sciadv.aax0903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brindley P., Jorgensen A., Maheswaran R. Domestic gardens and self-reported health: A national population study. International Journal of Health Geographics. 2018;17:31. doi: 10.1186/s12942-018-0148-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook Lyndhurst Ltd. (2007). Lifestyle scenarios & waste composition - The core report for defra waste & resources R&D programme. Retrieved July 15, 2019, from http://sciencesearch.defra.gov.uk/Document.aspx?Document=WR0104_7293_FRP.pdf.
- Cameron, R. W. F. & Hitchmough, J. (2016). Environmental horticulture - Science and management of green landscapes. CABI.
- Cameron, R. W. F., Blanusa, T., Taylor, J. E., Salisbury, A., Halstead, A. J., Henricot, B. & Thompson, K. (2012). The domestic garden - its contribution to urban green infrastructure. Urban Forestry & Urban Greening, 11, 129–137. doi:10.1016/j.ufug.2012.01.002.
- Cameron, R. W. F., Brindley, P., Mears, M. McEwan, K., Ferguson, F., Sheffield, D., Jorgensen, A., Riley, J. Goodrick, J., Ballard, E., Richardson, M. (2020). Where the wild things are! Do urban green spaces with greater avian biodiversity promote more positive emotions in humans? Urban Ecosystems, 22, 1–7. https://doi.org/10.1007/s11252-020-00929-z.
- Cammack C., Waliczek T.M., Zajicek J.M. The Green Brigade: The psychological effects of a community-based horticultural program on the self-development characteristics of juvenile offenders. HortTechnology. 2002;12(1):82–86. [Google Scholar]
- Cervinka R., Schwab M., Schönbauer R., Hämmerle I., Pirgie L., Sudkamp J. My garden - My mate? Perceived restorativeness of private gardens and its predictors. Urban Forestry and Urban Greening. 2016;16:182–187. doi: 10.1016/J.UFUG.2016.01.013. [DOI] [Google Scholar]
- Chalmin-Pui L.S., Griffiths A., Roe J.J., Cameron R.W.F. Bringing fronts back: A research agenda to investigate the health and well-being impacts of front gardens. Challenges. 2019;10(37) [Google Scholar]
- Clayton S. Domesticated nature: Motivations for gardening and perceptions of environmental impact. Journal of Environmental Psychology. 2007;27(3):215–224. doi: 10.1016/j.jenvp.2007.06.001. [DOI] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Dallimer M., Irvine K.N., Skinner A.M.J., Davies Z.G., Rouquette J.R., Maltby L., Warren P.H., Armsworth P.R., Gaston K.J. Biodiversity and the feel-good factor: Understanding associations between self-reported human well-being and species richness. BioScience. 2012;62(1):47–55. doi: 10.1525/bio.2012.62.1.9. [DOI] [Google Scholar]
- Davies Z.G., Fuller R.A., Loram A., Irvine K.N., Sims V., Gaston K.J. A national scale inventory of resource provision for biodiversity within domestic gardens. Biological Conservation. 2009;142(4):761–771. doi: 10.1016/j.biocon.2008.12.016. [DOI] [Google Scholar]
- de Vries S. In: Innovative approaches to researching landscape and health - Open space: People space 2. Ward Thompson C., Bell S., Aspinall P., editors. Routledge; 2010. Nearby nature and human health: Looking at mechanisms and their implications; pp. 77–96. [Google Scholar]
- Dennis M., James P. Ecosystem services of collectively managed urban gardens: Exploring factors affecting synergies and trade-offs at the site level. Ecosystem Services. 2017;26:17–26. doi: 10.1016/j.ecoser.2017.05.009. [DOI] [Google Scholar]
- Department for Culture Media and Sport. (2017). Adult (16+) participation in gardening, 2015/16. Retrieved May 13, 2019, from https://www.gov.uk/government/collections/taking-part.
- Desantis A.S., Kuzawa C.W., Adam E.K. Developmental origins of flatter cortisol rhythms: Socio-economic status and adult cortisol activity. American Journal of Human Biology. 2015;27(4):458–467. doi: 10.1002/ajhb.22668. [DOI] [PubMed] [Google Scholar]
- Dmitrieva N.O., Almeida D.M., Dmitrieva J., Loken E., Pieper C.F. A day-centered approach to modeling cortisol: Diurnal cortisol profiles and their associations among U.S. adults. Psychoneuroendocrinology. 2013;38(10):2354–2365. doi: 10.1016/j.psyneuen.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eum E.-Y., Kim H.-S. Effects of a horticultural therapy program on self-efficacy, stress response, and psychiatric symptoms in patients with schizophrenia. Journal of Korean Academy of Psychiatric and Mental Health Nursing. 2016;25(1):48. [Google Scholar]
- Exner, A. & Schützenberger, I. (2018). Creative Natures. Community gardening, social class and city development in Vienna. Geoforum. https://doi.org/10.1016/j.geoforum.2018.04.011.
- Fischer L.K., Honold J., Cvejić R., Delshammar T., Hilbert S., Lafortezza R.…Kowarik I. Beyond green: Broad support for biodiversity in multicultural European cities. Global Environmental Change. 2018;49:35–45. doi: 10.1016/j.gloenvcha.2018.02.001. [DOI] [Google Scholar]
- Freeman C., Dickinson K.J.M., Porter S., van Heezik Y.M. ‘My garden is an expression of me’: Exploring householders’ relationships with their gardens. Journal of Environmental Psychology. 2012;32(2):135–143. doi: 10.1016/j.jenvp.2012.01.005. [DOI] [Google Scholar]
- Frumkin H., Bratman G.N., Breslow S.J., Cochran B., Kahn P.H., Jr, Lawler J.J., Levin P.S., Tandon P.S., Varanasi U., Wolf K.L., Wood S.A. Nature contact and human health: A research agenda. Environmental Health Perspectives. 2017;125 doi: 10.1289/EHP1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genter C., Roberts A., Richardson J., Sheaff M. The contribution of allotment gardening to health and well-being: A systematic review of the literature. British Journal of Occupational Therapy. 2015;78(10):593–605. doi: 10.1177/0308022615599408. [DOI] [Google Scholar]
- Gidlow C.J., Randall J., Gillman J., Smith G.R., Jones M.V. Natural environments and chronic stress measured by hair cortisol. Landscape and Urban Planning. 2016;148:61–67. doi: 10.1016/j.landurbplan.2015.12.009. [DOI] [Google Scholar]
- Grahn P., Stigsdotter U.K. The relation between perceived sensory dimensions of urban green space and stress restoration. Landscape and Urban Planning. 2010;94(3–4):264–275. doi: 10.1016/j.landurbplan.2009.10.012. [DOI] [Google Scholar]
- Guéguen N., Stefan J. “Green Altruism”: Short immersion in natural green environments and helping behavior. Environment and Behavior. 2016;48(2):324–342. doi: 10.1177/0013916514536576. [DOI] [Google Scholar]
- Haaland C., Konijnendijk van den Bosch C. Challenges and strategies for urban green-space planning in cities undergoing densification: A review. Urban Forestry and Urban Greening. 2015;14(4):760–771. doi: 10.1016/j.ufug.2015.07.009. [DOI] [Google Scholar]
- Hale J.W., Knapp C., Bardwell L., Buchenau M., Marshall J.A., Sancar F., Litt J.S. Connecting food environments and health through the relational nature of aesthetics: Gaining insight through the community gardening experience. Social Science and Medicine. 2011;72(11):1853–1863. doi: 10.1016/j.socscimed.2011.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haluza D., Schönbauer R., Cervinka R. Green perspectives for public health: A narrative review on the physiological effects of experiencing outdoor nature. International Journal of Environmental Research and Public Health. 2014;11(5):5445–5461. doi: 10.3390/ijerph110505445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen M.M., Jones R., Tocchini K. Shinrin-yoku (forest bathing) and nature therapy: A state-of-the-art review. International Journal of Environmental Research and Public Health. 2017;14:851. doi: 10.3390/ijerph14080851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartig T., Mitchell R., De Vries S., Frumkin H. Nature and health. Annual Review of Public Health. 2014;35:207–228. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- Hassan A., Qibing C., Tao J. Physiological and psychological effects of gardening activity in older adults. Geriatrics and Gerontology International. 2018;18(8):1147–1152. doi: 10.1111/ggi.13327. [DOI] [PubMed] [Google Scholar]
- Haviland-Jones J., Rosario H.H., Wilson P., Mcguire T.R. An environmental approach to positive emotion: Flowers. Evolutionary Psychology. 2005;3:104–132. doi: 10.1177/147470490500300109. [DOI] [Google Scholar]
- Himmelheber S., Mozolic J., Lawrence L.A. Why Camp? Adolescents with intellectual horticulture therapy camp for evaluating the impact of intellectual and developmental disabilities. Journal of Therapeutic Horticulture. 2018;28(2):2–12. [Google Scholar]
- Hoyle, H., Jorgensen, A., Warren, P., Dunnett, N., & Evans, K. (2017b). “Not in their front yard” the opportunities and challenges of introducing perennial urban meadows: A local authority stakeholder perspective. Urban Forestry and Urban Greening. https://doi.org/10.1016/j.ufug.2017.05.009.
- Hoyle H., Hitchmough J., Jorgensen A. All about the ‘wow factor’? The relationships between aesthetics, restorative effect and perceived biodiversity in designed urban planting. Landscape and Urban Planning. 2017 doi: 10.1016/j.landurbplan.2017.03.011. [DOI] [Google Scholar]
- Ice G.H., Katz-Stein A., Himes J., Kane R.L. Diurnal cycles of salivary cortisol in older adults. Psychoneuroendocrinology. 2004 doi: 10.1016/S0306-4530(03)00034-9. [DOI] [PubMed] [Google Scholar]
- Keeler B.L., Hamel P., McPhearson T., Hamann M.H., Donahue M.L., Prado K.A.M., Arkema K.K., Bratman G.N., Brauman K.A., Finlay J.C., Guerry A.D. Social-ecological and technological factors moderate the value of urban nature. Nature Sustainability. 2019;2(1):29–38. doi: 10.1038/s41893-018-0202-1. [DOI] [Google Scholar]
- Keilp J.G., Stanley B.H., Beers S.R., Melhem N.M., Burke A.K., Cooper T.B., Oquendo M.A., Brent D.A., Mann J.J. Further evidence of low baseline cortisol levels in suicide attempters. Journal of Affective Disorders. 2016;190:187–192. doi: 10.1016/j.jad.2015.10.012. [DOI] [PubMed] [Google Scholar]
- Koss K.J., Gunnar M.R. Annual Research Review: Early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2018;59(4):327–346. doi: 10.1111/jcpp.12784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A., Jordan H., Horsley J. Value of urban green spaces in promoting healthy living and well-being: Prospects for planning. Risk Management and Healthcare Policy. 2015;8:131–137. doi: 10.2147/RMHP.S61654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Park B.J., Tsunetsugu Y., Ohira T., Kagawa T., Miyazaki Y. Effect of forest bathing on physiological and psychological responses in young Japanese male subjects. Public health. 2011;125:93–100. doi: 10.1016/j.puhe.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Lin B.B., Gaston K.J., Fuller R.A., Wu D., Bush R., Shanahan D.F. How green is your garden?: Urban form and socio-demographic factors influence yard vegetation, visitation, and ecosystem service benefits. Landscape and Urban Planning. 2017;157:239–246. doi: 10.1016/j.landurbplan.2016.07.007. [DOI] [Google Scholar]
- Mark, M. M. & Reichardt, C. S. (2009). Quasi-experimentation. In L. Bickman & D. J. Rog (Eds.), The SAGE handbook of applied social research methods (pp. 182–214). https://doi.org/10.4135/9781483348858.n6.
- Mayer F.S., Frantz C.M.P. The connectedness to nature scale: A measure of individuals’ feeling in community with nature. Journal of Environmental Psychology. 2004 doi: 10.1016/j.jenvp.2004.10.001. [DOI] [Google Scholar]
- Miller R., Stalder T., Jarczok M., Almeida D.M., Badrick E., Bartels M., Boomsma D.I., Coe C.L., Dekker M.C., Donzella B., Fischer J.E. The CIRCORT database: Reference ranges and seasonal changes in diurnal salivary cortisol derived from a meta-dataset comprised of 15 field studies. Psychoneuroendocrinology. 2016;73:16–23. doi: 10.1016/j.psyneuen.2016.07.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell R., Astell-Burt T., Richardson E.A. A comparison of green space indicators for epidemiological research. Journal of Epidemiology and Community Health. 2011;65(10):853–858. doi: 10.1136/jech.2010.119172. [DOI] [PubMed] [Google Scholar]
- Neale, C., Aspinall, P., Roe, J., Tilley, S., Mavros, P., Cinderby, S., Coyne, R., Thin, N. & Ward Thompson, C. (June, 2019). The impact of walking in different urban environments on brain activity in older people. Cities & Health, 1–13. https://doi.org/10.1080/23748834.2019.1619893.
- Nicolson N.A. Childhood parental loss and cortisol levels in adult men. Psychoneuroendocrinology. 2004 doi: 10.1016/j.psyneuen.2003.09.005. [DOI] [PubMed] [Google Scholar]
- O’Connor D.B., Hendrickx H., Dadd T., Elliman T.D., Willis T.A., Talbot D., Mayes A.E., Thethi K., Powell J., Dye L. Cortisol awakening rise in middle-aged women in relation to psychological stress. Psychoneuroendocrinology. 2009;34(10):1486–1494. doi: 10.1016/j.psyneuen.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics. (2018). UK natural capital: ecosystem accounts for urban areas. Retrieved from https://www.ons.gov.uk/economy/environmentalaccounts/bulletins/uknaturalcapital/ecosystemaccountsforurbanareas.
- Panagopoulos T., González Duque J.A., Bostenaru Dan M. Urban planning with respect to environmental quality and human well-being. Environmental Pollution. 2016 doi: 10.1016/j.envpol.2015.07.038. [DOI] [PubMed] [Google Scholar]
- Pruessner J.C., Kirschbaum C., Meinlschmid G., Hellhammer D.H. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–931. doi: 10.1016/S0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Reichardt C.S. The principle of parallelism in the design of studies to estimate treatment effects. Psychological Methods. 2006;11(1):1–18. doi: 10.1037/1082-989X.11.1.1. [DOI] [PubMed] [Google Scholar]
- Richardson M. Beyond restoration: Considering emotion regulation in natural well-being. Ecopsychology. 2019;11(2) doi: 10.1089/eco.2019.0012. [DOI] [Google Scholar]
- Roe J.J., Aspinall P. The emotional affordances of forest settings: An investigation in boys with extreme behavioural problems. Landscape Research. 2011;36(5):535–552. doi: 10.1080/01426397.2010.543670. [DOI] [Google Scholar]
- Roe J.J., Aspinall P.A., Ward Thompson C. Coping with stress in deprived urban neighborhoods: What is the role of green space according to life stage? Frontiers in Psychology. 2017;8:1–17. doi: 10.3389/fpsyg.2017.01760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roe J.J., Ward Thompson C., Aspinall P.A., Brewer M.J., Duff E.I., Miller D., Mitchell R., Clow A. Green space and stress: Evidence from cortisol measures in deprived urban communities. International Journal of Environmental Research and Public Health. 2013;10(9):4086–4103. doi: 10.3390/ijerph10094086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose D., Pevalin D.J. SAGE Publications Ltd; London: 2003. A researcher’s guide to the national statistics socio-economic classification. [Google Scholar]
- Ryan R., Clow A., Spathis A., Smyth N., Barclay S., Fallon M., Booth S. Salivary diurnal cortisol profiles in patients suffering from chronic breathlessness receiving supportive and palliative care services: A cross-sectional study. Psychoneuroendocrinology. 2017;79:134–145. doi: 10.1016/j.psyneuen.2017.01.025. [DOI] [PubMed] [Google Scholar]
- Saxbe D.E. A field (researcher’s) guide to cortisol: Tracking HPA axis functioning in everyday life. Health Psychology Review. 2008;2:163–190. doi: 10.1080/17437190802530812. [DOI] [Google Scholar]
- Schlotz W. Investigating associations between momentary stress and cortisol in daily life: What have we learned so far? Psychoneuroendocrinology. 2018;105:105–116. doi: 10.1016/j.psyneuen.2018.11.038. [DOI] [PubMed] [Google Scholar]
- Smith, J. A., Jarman, M., & Osborn, M. (1999). Doing interpretative phenomenological analysis. In Qualitative health psychology: theories and methods (pp. 218–240). London: SAGE Publications.
- Smyth N., Hucklebridge F., Thorn L., Evans P., Clow A. Salivary cortisol as a biomarker in stress research. Social and Personality Psychology Compass. 2013;7(9):605–625. doi: 10.1016/j.psyneuen.2008.10.026. [DOI] [Google Scholar]
- Smyth J.M., Ockenfels M.C., Gorin A.A., Catley D., Porter L.S., Kirschbaum C., Hellhammer D.H., Stone A.A. Individual differences in the diurnal cycle of cortisol. Psychoneuroendocrinology. 1997 doi: 10.1016/S0306-4530(96)00039-X. [DOI] [PubMed] [Google Scholar]
- Smyth N., Skender E., David F.J., Munoz M.J., Fantuzzi G., Clow A., Goldman J.G., Corcos D.M. Endurance exercise reduces cortisol in Parkinson’s disease with mild cognitive impairment. Movement Disorders. 2019;1–2 doi: 10.1002/mds.27719. [DOI] [PubMed] [Google Scholar]
- Sofo A., Sofo A. Converting home spaces into food gardens at the time of covid-19 quarantine: All the benefits of plants in this difficult and unprecedented period. Human Ecology. 2020;2020:1–9. doi: 10.1007/s10745-020-00150-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soga M., Cox D.T.C., Yamaura Y., Gaston K.J., Kurisu K., Hanaki K. Health benefits of urban allotment gardening: Improved physical and psychological well-being and social integration. International Journal of Environmental Research and Public Health. 2017;14(1) doi: 10.3390/ijerph14010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soga M., Gaston K.J., Yamaura Y. Gardening is beneficial for health: A meta-analysis. Preventive Medicine Reports. 2017;5:92–99. doi: 10.1016/j.pmedr.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott I., Soga M., Inger R., Gaston K.J. Land sparing is crucial for urban ecosystem services. Frontiers in Ecology and the Environment. 2015;13(7):387–393. doi: 10.1890/140286. [DOI] [Google Scholar]
- Tahvonen O., Airaksinen M. Low-density housing in sustainable urban planning – Scaling down to private gardens by using the green infrastructure concept. Land Use Policy. 2018 doi: 10.1016/j.landusepol.2018.04.017. [DOI] [Google Scholar]
- Taylor M.S., Wheeler B.W., White M.P., Economou T., Osborne N.J. Research note: Urban street tree density and antidepressant prescription rates—A cross-sectional study in London, UK. Landscape and Urban Planning. 2015;136:174–179. doi: 10.1016/j.landurbplan.2014.12.005. [DOI] [Google Scholar]
- Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., Parkinson J., Secker J., Stewart-Brown S. The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health and Quality of Life Outcomes. 2007;5:1–13. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toda M., Den R., Hasegawa-Ohira M., Morimoto K. Effects of woodland walking on salivary stress markers cortisol and chromogranin A. Complementary Therapies in Medicine. 2013 doi: 10.1016/j.ctim.2012.11.004. [DOI] [PubMed] [Google Scholar]
- Toussaint L., Shields G.S., Dorn G., Slavich G.M. Effects of lifetime stress exposure on mental and physical health in young adulthood: How stress degrades and forgiveness protects health. Journal of Health Psychology. 2016;21(6):1004–1014. doi: 10.1177/1359105314544132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Wietmarschen H., Tjaden B., van Vliet M., Battjes-Fries M., Jong M. Effects of mindfulness training on perceived stress, self-compassion, and self-reflection of primary care physicians: A mixed-methods study. BJGP Open. 2018;2(4) doi: 10.3399/bjgpopen18X101621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward Thompson C., Roe J., Aspinall P., Mitchell R., Clow A., Miller D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landscape and Urban Planning. 2012;105:221–229. doi: 10.1016/j.landurbplan.2011.12.015. [DOI] [Google Scholar]
- Wendelboe-Nelson, C., Kelly, S., Kennedy, M. & Cherrie, J. W. (2019). A scoping review mapping research on green space and associated mental health benefits. http://dx.doi.org/10.3390/ijerph16122081. [DOI] [PMC free article] [PubMed]
- Wolf L.J., Ermgassen S., Balmford A., White M., Weinstein N. Is variety the spice of life? An experimental investigation into the effects of species richness on self-reported mental well-being. PLoS ONE. 2017;12(1):1–17. doi: 10.1371/journal.pone.0170225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf I.D., Wohlfart T. Walking, hiking and running in parks: A multidisciplinary assessment of health and well-being benefits. Landscape and Urban Planning. 2014;130:89–103. doi: 10.1016/j.landurbplan.2014.06.006. [DOI] [Google Scholar]
- Wood E., Harsant A., Dallimer M., de Chavez A.C., McEachan R.R.C., Hassall C. Not all green space is created equal: Biodiversity predicts psychological restorative benefits from urban green space. Frontiers in Psychology. 2018;9:1–13. doi: 10.3389/fpsyg.2018.02320. [DOI] [PMC free article] [PubMed] [Google Scholar]