Abstract
Objectives
This study aimed to compare short- and long-term results for patients undergoing either aortic valve-sparing reimplantation (David) procedure (AVr-D) or biological aortic root replacement (Bentall) procedure (ARr-B-bio) for aortic root pathology.
Methods
We compared outcomes for patients who underwent AVr-D (n = 261) or ARr-B-bio (n = 150) between 2000 and 2015 at our institution. The mean age of patients was 55 ± 13 years and 21.7% (n = 89) were female. ARr-B-bio patients were significantly older than AVr-D patients (58 ± 10 vs 53 ± 15 years, p < 0.001) and had a significantly lower incidence of connective tissue disorders (2.0% vs 16.9%, p < 0.001). Follow-up was complete in 88% of patients.
Results
Mortality at 30 days was 1.2% (n = 5) overall, at 0.4% (n = 1) significantly lower in the AVr-D group compared with 2.7% (n = 4) in the ARr-B-bio group (p = 0.04). Postoperative low cardiac output was more common in ARr-B-bio patients (n = 4) versus AVr-D patients (n = 0; p = 0.008). The occurrence of postoperative strokes was 2.2% (n = 9) in both groups, without significant differences (p = 0.84). Five- and ten-year survival was 93.7 ± 1.8% and 84.4 ± 4.7% in patients who received AVr-D and 90.9 ± 2.6% and 84.6 ± 5.4% for ARr-B-bio patients (log-rank p = 0.37). Using Cox regression analysis, age (HR 1.06; 95% CI 1.02–1.10, p = 0.002), smoking (HR 2.74; 95% CI 1.28–5.86, p = 0.01), and emergency surgery (HR 6.58; 95% CI 1.69–25.54, p = 0.007) were found to be independent predictors of long-term mortality.
There was no difference in freedom from reoperation between AVr-D (89.4 ± 3.4% at 10 years) and ARr-B-bio (80.4 ± 7.5% at 10 years, log-rank p = 0.66) patients, nor for freedom from stroke, bleeding, myocardial infarction, or endocarditis during follow-up.
Conclusions
Short-term outcomes for both AVr-D and ARr-B-bio are excellent in patients with aortic root pathology. The long-term outcomes were associated with comparable survival and freedom from reoperation. AVr-D may be preferable to ARr-B-bio in patients with suitable pathoanatomy.
Keywords: Elective aortic arch surgery, Outcome, Risk factors, Long-term results
Introduction
Surgical correction of aortic root pathology consists mostly of two widely used procedures: replacement of the entire aortic root (modified Bentall procedure) or aortic valve-sparing aortic root replacement (David procedure). The choice of procedure is important since adverse events, deterioration of valves, or conduit and lifestyle adjustments may have serious consequences for patients, especially younger individuals. Since the AVr-D procedure has shown promising outcomes without the need for anticoagulation, it is often the procedure of choice for patients with suitable aortic root pathoanatomy in specialised treatment centres [1]. A widely used alternative is the aortic root replacement Bentall (ARr-B) procedure, consisting of the replacement of the aortic root and native aortic valve with either a mechanical or biological conduit. Both the David and the biological Bentall (ARr-B-bio) procedures seem to offer similar advantages regarding long-term avoidance of anticoagulation and may be considered in select young patients [2, 3].
The aim of this study was to compare short- and long-term outcomes of ARr-B-bio versus AVr-D patients in a retrospective analysis.
Patients and methods
A total number of 1318 consecutive patients underwent surgical correction of aortic root pathology with an ARr-B (n = 1005) or AVr-D (n = 313) technique at our centre between 2000 and 2015. Patients with the previous replacement of the aortic valve, infective endocarditis at time of index operation, and concomitant valve surgery (e.g. mitral valve replacement or repair) were excluded. Propensity score matching was used to address differences in baseline variables between AVr-D and ARr-B patients, resulting in 301 AVr-D and 299 ARr-B patients. Subsequently, exclusion of mechanical ARr-B patients and patients with type A aortic dissection resulted in a total 261 AVr-D and 150 ARr-B-bio patients, which form the focus of this study.
A yearly follow-up to assess mortality and post-surgical complications was conducted. Follow-up was obtained by contacting the patient or treating physicians by mail and/or phone questionnaire. Follow-up was complete in 88% of patients after a period ranging between 1.0 and 16.1 years, and a mean of 4.9 years.
Operative technique
Patients undergoing ARr-B-bio received a biological conduit with the removal of the native aortic valve and the surrounding aortic wall and proximal ascending aorta [4]. A description of our operative technique for AVr-D has been previously provided [5]. The decision of whether a ARr-B-bio or AVr-D operation was performed depended on several variables including aortic cusp pathology, patient factors such as age and comorbidities, as well as lifestyle requirements and family planning, and the availability of an experienced surgeon. Due to intraoperative failure of aortic cusp reimplantation, one patient who was planned for AVr-D received ARr-B-bio instead. This patient was analysed in the AVr-D group, however, in accordance with the intention-to-treat principle.
Definitions
In accordance with STS guidelines, early mortality was defined as all-cause mortality at 30 days. Definitions of other outcomes have been previously described by our group [5, 6].
Statistical analysis
Data were imported to SPSS (SPSS Statistics 25.0; Chicago, IL, USA) for description and analysis. Categorical data are shown as total numbers and proportions in percent throughout the manuscript and were compared using the χ2 test or Fisher’s exact test as appropriate. Continuous variables are expressed as mean ± standard deviation (SD) and were compared using the Student’s t test or Wilcoxon-Mann-Whitney test as appropriate. Normal distribution of measurements was determined using the Shapiro-Wilk test. Furthermore, the Cox proportional hazard analysis was performed to determine the independent predictors of long-term mortality and freedom from reoperation, presented as hazard ratios (HR) and 95% confidence intervals (CIs). A p value < 0.05 was considered statistically significant.
Results
Preoperative characteristics
A summary of the patients’ preoperative baseline characteristics is given in (Table 1). The mean age at surgery was 55 ± 13 years for the entire cohort and 21.7% (n = 89) were female. Patients in the ARr-B-bio group were significantly older than AVr-D patients and had a significantly lower incidence of connective tissue disorders. In addition, ARr-B-bio patients were more likely to have a bicuspid aortic valve and undergo emergency surgery.
Table 1.
Preoperative clinical characteristics
| Total n = 411 |
AVr-D n = 261 |
ARr-B-bio n = 150 |
p | |
|---|---|---|---|---|
| Age (years) | 55 ± 13 | 53 ± 15 | 58 ± 10 | < 0.001* |
| Female | 89 (21.7) | 57 (21.8) | 32 (21.3) | 0.91 |
| COPD | 10 (2.4) | 7 (2.7) | 3 (2.0) | 0.67 |
| Pulmonary hypertension | 50 (12.2) | 30 (11.5) | 20 (13.3) | 0.58 |
| Dialysis | 3 (0.7) | 2 (0.8) | 1 (0.7) | 0.91 |
| Diabetes | 25 (6.1) | 15 (5.7) | 10 (6.7) | 0.71 |
| Hyperlipemia | 122 (29.7) | 67 (25.7) | 55 (36.7) | 0.019* |
| Arterial hypertension | 320 (77.9) | 191 (73.2) | 129 (86.0) | 0.003* |
| Peripheral vascular disease | 266 (64.7) | 165 (63.2) | 101 (67.3) | 0.4 |
| Previous myocardial infarction | 9 (2.2) | 4 (1.5) | 5 (3.3) | 0.23 |
| Smoker | 161 (39.2) | 99 (37.9) | 62 (41.3) | 0.50 |
| Cerebrovascular accident | 15 (3.6) | 7 (2.7) | 8 (5.3) | 0.17 |
| LVEF | 58 ± 9 | 58 ± 9 | 59 ± 10 | 0.67 |
| < 30% | 3 (0.7) | 2 (0.8) | 1 (0.7) | 0.91 |
| 30–50% | 88 (21.4) | 54 (20.7) | 34 (22.7) | 0.64 |
| > 50% | 320 (77.9) | 205 (78.5) | 115 (76.7) | 0.66 |
| Emergency surgery | 5 (1.2) | 0 (0.0) | 5 (3.3) | 0.003* |
| Previous cardiac surgery | 13 (3.2) | 8 (3.1) | 5 (3.3) | 0.88 |
| Connective tissue disease | 47 (11.4) | 44 (16.9) | 3 (2.0) | < 0.001* |
| Marfan syndrome | 34 (8.3) | 31 (11.9) | 3 (2.0) | < 0.001* |
| Symptomatic | 12 (2.9) | 12 (4.6) | 0 (0.0) | < 0.001* |
| Loeys-Dietz syndrome | 1 (0.2) | 1 (0.4) | 0 (0.0) | 0.45 |
| Bicuspid aortic valve | 118 (28.7) | 41 (15.7) | 77 (51.3) | < 0.001* |
| AI only | 310 (75.4) | 250 (95.8) | 60 (40.0) | < 0.001* |
| 1° | 67 (16.3) | 62 (23.8) | 5 (3.3) | < 0.001* |
| 2° | 149 (36.3) | 125 (47.9) | 24 (16.0) | < 0.001* |
| 3° | 92 (22.4) | 63 (24.1) | 29 (19.3) | 0.26 |
| 4° | 2 (0.5) | 0 (0.0) | 2 (3.3) | 0.06 |
| AS only | 33 (8.0) | 0 (0.0) | 33 (22.0) | < 0.001* |
| 1° | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 2° | 7 (1.7) | 0 (0.0) | 7 (4.7) | < 0.001* |
| 3° | 26 (6.3) | 0 (0.0) | 26 (17.3) | < 0.001* |
| 4° | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Combined AI and AS | 57 (13.9) | 0 (0.0) | 57 (38.0) | < 0.001* |
| Aortic diameters (mm) | ||||
| Root | 45 ± 9 | 45 ± 9 | 44 ± 10 | 0.18 |
| Ascending aorta | 51 ± 9 | 53 ± 9 | 47 ± 8 | < 0.001* |
All data shown as number of cases, unless specified differently. (%). AVr-D David aortic valve-sparing reimplantation, ARr-B-bio biological aortic root replacement–biological Bentall procedure, COPD chronic obstructive pulmonary disease, LVEF left ventricular ejection fraction, AI aortic insufficiency, AS aortic stenosis
*Statistically significant for p < 0.05
Operation data
The total length of surgery was significantly longer in AVr-D than ARr-B-bio patients (Table 2). In addition, aortic cross-clamp times and total cardiopulmonary bypass (CPB) times were significantly longer in the AVr-D group.
Table 2.
Operation data
| Total n = 411 |
AVr-D n = 261 |
ARr-B-bio n = 150 |
p | |
|---|---|---|---|---|
| Operation | ||||
| Length of surgery (min) | 221 ± 61 | 231 ± 54 | 204 ± 67 | < 0.001* |
| Aortic cross-clamp time (min) | 105 ± 34 | 114 ± 30 | 88 ± 34 | < 0.001* |
| Total cardiopulmonary bypass time (min) | 132 ± 45 | 142 ± 42 | 116 ± 46 | < 0.001* |
| Min. body temperature (Celsius) | 31.7 ± 5.0 | 30.9 ± 4.9 | 33.1 ± 4.9 | < 0.001* |
| Concomitant surgery | ||||
| CABG | 30 (7.3) | 18 (6.9) | 12 (8.0) | 0.68 |
| Correction of CHD | 11 (2.7) | 7 (2.7) | 4 (2.7) | 0.99 |
All data shown as number of cases, unless specified differently. (%). AVr-D David aortic valve-sparing reimplantation, ARr-B-bio biological aortic root replacement–biological Bentall procedure, CABG coronary artery bypass grafting, CHD congenital heart defect
*Statistically significant for p < 0.05
Early outcomes
Thirty-day mortality was 1.2% (n = 5) overall, with significantly more deaths in the Bentall group (2.7%, n = 4) than David group (0.4%, n = 1; p = 0.04). The total stroke rate was 2.2% (n = 9) and similar in both groups (p = 0.84). A low cardiac output was observed in the Bentall group, significantly more than in the patients who received AVr-D (p = 0.008). Furthermore, postoperative echocardiographic data showed significantly more cases of minimal aortic insufficiency in the postoperative period within the David group (23.8%, n = 62) compared with the Bentall group (8.0%, n = 12; p < 0.001). There was no significant difference between groups for any other reported early outcomes (Table 3).
Table 3.
Early postoperative outcomes for AVr-D vs ARr-B-bio
| Total n = 411 |
AVr-D n = 261 |
ARr-B-bio n = 150 |
p | |
|---|---|---|---|---|
| Respiratory failure | 30 (7.3) | 20 (7.7) | 10 (6.7) | 0.71 |
| Low cardiac output | 4 (1.0) | 0 (0.0) | 4 (2.7) | 0.008* |
| Myocardial infarction | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| New pacemaker | 15 (3.6) | 6 (2.3) | 9 (6.0) | 0.05 |
| Cerebrovascular accident | 9 (2.2) | 6 (2.3) | 3 (2.0) | 0.84 |
| Deep sternal wound infection | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Sepsis | 4 (1.0) | 3 (1.1) | 1 (0.7) | 0.63 |
| Dialysis | 5 (1.2) | 3 (1.2) | 2 (1.3) | 0.87 |
| Reoperation for bleeding | 25 (6.1) | 18 (6.9) | 7 (4.7) | 0.36 |
| Redo surgery | 5 (1.2) | 3 (1.1) | 2 (1.3) | 0.87 |
| AI† | 75 (18.2) | 63 (24.1) | 12 (8.0) | < 0.001* |
| 1° | 74 (18.0) | 62 (23.8) | 12 (8.0) | < 0.001* |
| 2° | 1 (0.2) | 1 (0.4) | 0 (0.0) | 0.45 |
| AS† | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Aortic diameters (mm)† | ||||
| Root | 30 ± 3 | 31 ± 3 | 29 ± 3 | < 0.001* |
| Ascending aorta | 29 ± 3 | 30 ± 3 | 28 ± 3 | < 0.001* |
| LVEF† (%) | 56 ± 10 | 57 ± 8 | 55 ± 12 | 0.02* |
| < 30% | 4 (1.0) | 0 (0.0) | 4 (2.7) | 0.008* |
| 30–50% | 106 (25.8) | 64 (24.5) | 42 (28.0) | 0.44 |
| > 50% | 300 (73.0) | 197 (75.5) | 103 (68.7) | 0.13 |
| 30-day mortality | 5 (1.2) | 1 (0.4) | 4 (2.7) | 0.04* |
| In-hospital mortality | 4 (1.0) | 1 (0.4) | 3 (2.0) | 0.11 |
| Hospital stay length (days) | 11 ± 6 | 12 ± 7 | 11 ± 5 | 0.34 |
All data shown as number of cases, unless specified differently. (%). AVr-D David aortic valve-sparing reimplantation, ARr-B-bio biological aortic root replacement–biological Bentall procedure, AI aortic insufficiency, AS aortic stenosis
*Statistically significant for p < 0.05
†Four patients died before postoperative echocardiographic data could be obtained
Medium- and long-term outcomes
In terms of medium- and long-term outcomes, there was no observable advantage for AVr-D or ARr-B-bio (log-rank p = 0.37, Fig. 1) with respect to survival. Five- and ten-year survival of the entire cohort was 92.7 ± 1.5% and 84.6 ± 3.5%, respectively. Independent predictors of mortality were age at surgery (HR 1.06; 95% CI 1.02–1.10, p = 0.002), smoking (HR 2.74; 95% CI 1.28–5.86, p = 0.01), and emergency surgery (HR 6.58; 95% CI 1.69–25.54, p = 0.007).
Fig. 1.
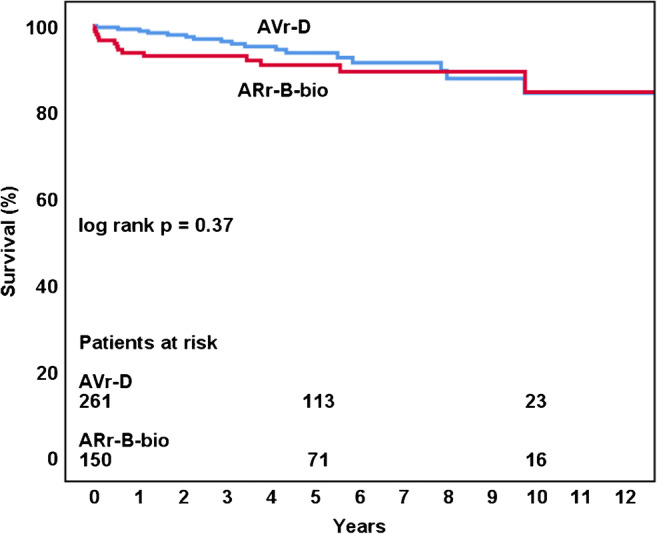
Long-term mortality: David operation (AVr-D) vs biological aortic root replacement (ARr-B-bio)
Aortic valve reoperation was necessary in 23 patients: 8 for endocarditis, 10 for aortic insufficiency, and 5 for aortic stenosis, without significant difference in incidence for both groups. Freedom from reoperation at 5- and 10-years was 95.7 ± 1.3% and 85.9 ± 3.7% for all patients (Fig. 2), with no difference between groups (log-rank p = 0.66). During follow-up, 5- and 10-year freedom from reoperation was significantly lower for patients with bicuspid aortic valves compared with patients with tricuspid valves: 91.4 ± 3.3% and 79.2 ± 7.4% vs 97.3 ± 1.2% and 87.8 ± 4.3%, respectively (log-rank p = 0.048). A sub-analysis of all patients with bicuspid aortic valves did not show a significant difference in freedom from reoperation for AVr-D and ARr-B-bio (log-rank p = 0.13). There was no difference for patients with or without connective tissue disease (log-rank p = 0.58). Cox regression analysis did not reveal a significant independent predictor of freedom from reoperation.
Fig. 2.
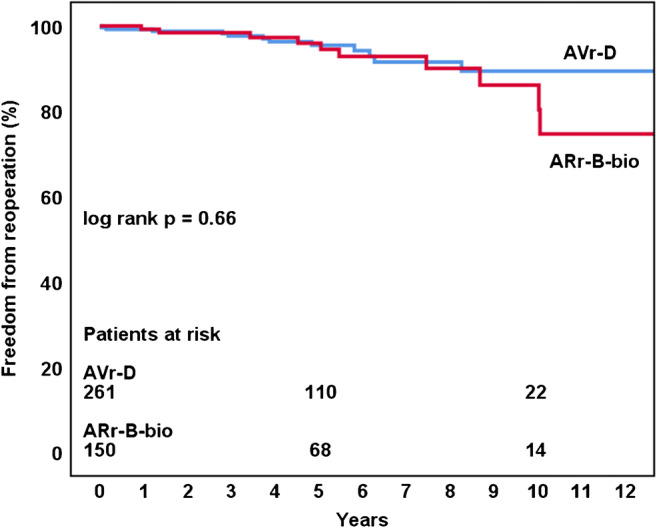
Freedom from reoperation: David operation (AVr-D) vs biological aortic root replacement (ARr-B-bio)
During the follow-up period, there were no significant differences between groups with regard to freedom from stroke, bleeding, myocardial infarction, or endocarditis.
Discussion
Our study compared early and long-term outcomes in patients undergoing AVr-D versus ARr-B-bio surgery for aortic root pathology. Both procedures show excellent outcomes with regard to survival and reoperation rates, as well as low occurrences of strokes, bleeding events, myocardial infarction, and endocarditis during the follow-up period. Although there was no significant difference between the two procedures with regard to any of these outcomes, we recorded a significantly higher 30-day mortality for patients who received ARr-B-bio, as well as a higher incidence of low cardiac output post-surgery in the same group. While these findings are suggestive of a superior outcome for AVr-D procedures, it is likely that the significant difference in emergency procedures contributed to that result, as two of the patients with low cardiac output were treated in an emergency situation, of which one died within 30 days. A trend for higher risk of reoperation for ARr-B has previously been shared by other authors [2, 3]. It should be noted that AVr-D patients had a markedly higher incidence of connective tissue disorders in our study, which may have impacted long-term survival rates. Furthermore, deaths during follow-up in the AVr-D group included four tumour-related deaths, such as prostatic, bowel, and brain cancer, as well as one death due to epilepsy.
Since AVr-D and ARr-B-bio are often used to treat similar conditions in comparable patient populations, deciding on a treatment for individual patients can be challenging. Age, comorbidities, lifestyle, and patient preference—among others—may influence the choice of procedure performed. AVr-D avoids the known disadvantages associated with prosthetic valve replacement but is technically more difficult to perform than ARr-B-bio and associated with longer ischemic and CPB times.
Several recent studies have suggested that the AVr-D procedure can be applied to a wider range of anatomical variations, with bicuspid aortic valves showing a similar outcome to tricuspid valves [7]. In our study, we observed an increased number of reoperartions for patients with bicuspid aortic valves, although the number of bicuspid patients among the AVr-D group was relatively small (n = 41) compared with patients in the ARr-B-bio group (n = 77).
It can be argued that the main advantage of AVr-D is the lifelong avoidance of anticoagulation and hence reduction of bleeding incidents, which may be particularly appealing in young patients and those with connective tissue disorders. Our study shows no clear advantage for AVr-D over ARr-B-bio with regard to bleeding incidents during the follow-up period. Instead, we found a significantly lower 30-day mortality for AVr-D procedures (p = 0.04), as well as a higher incidence of low cardiac output after ARr-B-bio procedures (p = 0.008) as discussed above.
One of the disadvantages of AVr-D is its complexity and difficulty to perform, reflected by prolonged operation times [8]. Long operation times may pose a problem for some patients, especially the elderly or those with left ventricular dysfunction, who cannot tolerate long ischemic times. Comparison of the left ventricular ejection fraction before and after the procedure shows that both procedures have good postoperative outcomes, but the cardiac output was slightly better in the AVr-D group. It is still advisable that those patients who are at greater risk of adverse outcome due to prolonged operation times should undergo the ARr-B-bio operation.
AVr-D requires specially trained surgeons and teams in order to be performed safely and effectively. This has long been a concern with AVr-D and the proposed solution has usually been to defer treatment to specialised centres with public reporting of outcomes [9, 10]. Indeed, consistently good outcomes for aortic root surgery can more readily be achieved in large volume centres [11], even in complex patients such as those presenting with type A aortic dissection [12]. Nonetheless, efforts should be made to make AVr-D more available and outcomes more comparable between centres [13]. To achieve this, an increase in trained surgeons and training opportunities are necessary, as well as more public reporting of outcomes in a standardised manner.
As another recent study has shown, AVr-D might also be a superior procedure to ARr-B-bio in regard to reoperation during follow-up [3]. This is contrary to previous concerns over a higher incidence of progressive aortic regurgitation after AVr-D procedures [14]. Our postoperative echocardiographic data indeed shows a higher incidence of minimal aortic insufficiency postoperatively for AVr-D compared with ARr-B-bio, but there was no significant difference shown between groups in regard to freedom from reoperation after 10 years. Although we were unable to demonstrate a lower reoperation rate in the AVr-D patients, this may have been secondary to our relatively small sample size, as well as our relatively short follow-up period over 10 years, as other studies have shown that biological replacements of the aortic valve are more likely to deteriorate after 10 years; as such, a longer follow-up period might have shown clearer differences [15, 16].
Considering our findings of similarly good outcomes regarding mortality and reoperation among patients who received either AVr-D or ARr-B-bio, we recommend AVr-D for all patients requiring correction of aortic root pathology given favourable pathoanatomic conditions and preoperative patient status.
Study limitations
Our study compared early- and long-term results between AVr-D and ARr-B-bio. For this, we used a subgroup analysis of a propensity score matched comparison of AVr-D vs ARr-B, followed by exclusions of mechanical ARr-B patients. Unaccounted variables in the assignment of propensity scores and surgeon preference may have contributed to selection bias. A randomised controlled trial would alleviate most concerns regarding selection biases, but such a trial is unlikely to be performed in the near future. Also, our follow-up period may not have been long enough to show clearer advantages for either procedure.
Conclusion
AVr-D and ARr-B-bio are associated with very good early- and long-term results in patients with aortic root pathology. While mortality and freedom from reoperation were excellent in both groups. We therefore recommend AVr-D surgery in patients with aortic root pathology, given that aortic valve cusp pathology is suitable. ARr-B-bio remains an appropriate alternative, especially for older patients or those with comorbidities that may result in decreased ability to tolerate longer myocardial ischemic and cardiopulmonary bypass times.
Funding
No funding
Compliance with ethical standards
The local ethics committee approved the study and waived individual patient consent for retrospective review. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
Lukas Schamberger declares that he has no conflict of interest.
Sergey Leontyev receives proctoring honoraria fees from Medtronic, Abott (St. Jude Medical).
Piroze M. Davierwala declares that he has no conflict of interest.
Konstantin Von Aspern declares that he has no conflict of interest.
Sven Lehmann receives honoraria fees from Abott (St. Jude Medical).
Martin Misfeld declares that he has no conflict of interest.
Michael Borger receives speakers’ honoraria/consulting fees from Edwards Lifesciences, Medtronic, Abott (St. Jude Medical), and CryoLife.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lukas Schamberger and Sergey Leontyev contributed equally to this work.
References
- 1.Ouzounian M, Rao V, Manlhiot C, et al. Valve-sparing root replacement compared with composite valve graft procedures in patients with aortic root dilation. J Am Coll Cardiol. 2016;68:1838–1847. doi: 10.1016/j.jacc.2016.07.767. [DOI] [PubMed] [Google Scholar]
- 2.De Paulis R, Scaffa R, Salica A, Weltert L, Chirichilli I. Biological solutions to aortic root replacement: valve-sparing versus bioprosthetic conduit. J Vis Surg. 2018;4:94. doi: 10.21037/jovs.2018.04.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaudino M, Di Franco A, Ohmes LB, et al. Biological solutions to aortic root replacement: valve-sparing versus bioprosthetic conduit. Interact Cardiovasc Thorac Surg. 2017;24:855–861. doi: 10.1093/icvts/ivx010. [DOI] [PubMed] [Google Scholar]
- 4.Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23:338–339. doi: 10.1136/thx.23.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leontyev S, Trommer C, Subramanian S, et al. The outcome after valve-sparing (David) operation in 179 patients: a single-Centre experience. Eur J Cardiothorac Surg. 2012;42:261–266. doi: 10.1093/ejcts/ezs011. [DOI] [PubMed] [Google Scholar]
- 6.Leontyev S, Misfeld M, Daviewala P, et al. Early- and medium-term results after aortic arch replacement with frozen elephant trunk techniques—a single center study. Ann Cardiothorac Surg. 2013;2:606–611. doi: 10.3978/j.issn.2225-319X.2013.09.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borger MA, Fedak PWM, Stephens EH, et al. The American Association for Thoracic Surgery consensus guidelines on bicuspid aortic valve–related aortopathy: executive summary. J Thorac Cardiovasc Surg. 2018;156:473–480. doi: 10.1016/j.jtcvs.2017.10.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arabkhani B, Mookhoek A, Di Centa I, et al. Reported outcome after valve-sparing aortic root replacement for aortic root aneurysm: a systematic review and meta-analysis. Ann Thorac Surg. 2015;100:1126–1131. doi: 10.1016/j.athoracsur.2015.05.093. [DOI] [PubMed] [Google Scholar]
- 9.Gaudino M, Lau C, Munjal M, Avgerinos D, Girardi LN. Contemporary outcomes of surgery for aortic root aneurysms: a propensity-matched comparison of valve-sparing and composite valve graft replacement. J Thorac Cardiovasc Surg. 2015;150:1120–1129. doi: 10.1016/j.jtcvs.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Svensson LG, Pillai ST, Rajeswaran J, et al. Long-term survival, valve durability, and reoperation for 4 aortic root procedures combined with ascending aorta replacement. J Thorac Cardiovasc Surg. 2016;151:764–774. doi: 10.1016/j.jtcvs.2015.10.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stamou SC, Williams ML, Gunn TM, Hagberg RC, Lobdell KW, Kouchoukos NT. Aortic root surgery in the United States: a report from the Society of Thoracic Surgeons database. J Thorac Cardiovasc Surg. 2015;149:116–122. doi: 10.1016/j.jtcvs.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 12.Subramanian S, Leontyev S, Borger MA, Trommer C, Misfeld M, Mohr FW. Valve-sparing root reconstruction does not compromise survival in acute type a aortic dissection. Ann Thorac Surg. 2012;94:1230–1234. doi: 10.1016/j.athoracsur.2012.04.094. [DOI] [PubMed] [Google Scholar]
- 13.Kunihara T. Toward standardization of valve-sparing root replacement and annuloplasty. Gen Thorac Cardiovasc Surg. 2018;66:685–691. doi: 10.1007/s11748-018-1015-x. [DOI] [PubMed] [Google Scholar]
- 14.Kari FA, Doll KN, Hemmer W, et al. Residual and progressive aortic regurgitation after valve-sparing root replacement: a propensity-matched multi-institutional analysis in 764 patients. Ann Thorac Surg. 2016;101:1500–1506. doi: 10.1016/j.athoracsur.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Johnston DR, Soltesz EG, Vakil N, et al. Long-term durability of bioprosthetic aortic valves: implications from 12,569 implants. Ann Thorac Surg. 2015;99:1239–1247. doi: 10.1016/j.athoracsur.2014.10.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bourguignon T, Lhommet P, El Khoury R, et al. Very long-term outcomes of the Carpentier-Edwards Perimount aortic valve in patients aged 50–65 years. Eur J Cardiothorac Surg. 2016;49:1462–1468. doi: 10.1093/ejcts/ezv384. [DOI] [PubMed] [Google Scholar]


