Abstract
Background
The era of percutaneous aortic valve intervention has challenged the continuing indication for surgical aortic valve replacement (SAVR).
Aim
The aim of this study is to evaluate clinical outcomes of the elderly patients who underwent surgical aortic valve replacement via median sternotomy, in order to assess the impact of surgery on patient outcomes and discharge destination.
Methods
The study involves a retrospective observational analysis in a single centre, including all octogenarian patients who underwent aortic valve surgery between January of 2011 and July of 2016. The study assessed pre-operative co-morbidities and post-operative outcomes, including long-term mortality and discharge destination following on from surgery.
Results
The mean age of patients was 82.7 years (± 2.9), 67% of whom were male. The mean EuroSCORE II was 8.1 (± 7.6). The most common pre-operative co-morbidities were dyslipidaemia (82%), hypertension (80%), and ischaemic heart disease (78.8%). The median length of stay was 10 days (± 6.9 days). Discharge home occurred in 71.8% of patients, with 21.2% of patients requiring transfer to a rehabilitation facility, and 1.2% of patients required placement into an aged care facility. There were five peri-operative deaths, equating to 5.9% of the cohort.
Conclusion
Despite high EuroSCORE II values for the majority of our patients, our data adds to overall suggestions that the octogenarian population can be considered eligible for SAVR and should not be excluded due to age alone. The use of the EuroSCORE II index more accurately predicts adequacy for treatment however does not entirely predict overall course of events, and proceduralist discretion should still be used.
Keywords: AVR, Aortic valve replacement, Octogenarians
Introduction
In Australia, the average age of the population has consistently increased. The Australian Institute of Health and Wellbeing (AIHW) reports that the size of the population aged above 65 years in 2017 was 3.8 million (15%), a significant rise compared with that seen in 1977 which was 1.3 million (9%) [1, 2]. Aortic stenosis is seen more commonly with increases in age and much more frequently in the 80–89-year-old group (9.8%) [3]. The ageing population will inevitably lead to greater numbers of those presenting with degenerative aortic valve disease, adding pressures to the health care system [3]. The population group of octogenarians has become a well-studied group for candidacy for cardiac surgery; however, they are still considered a high-risk group for surgical intervention, largely owing to their perceived age-related frailty and multiple co-morbidities.
The pathogenesis of calcific valvular disease has been likened to an atherosclerotic process, where lipid deposition onto the valvular surface leads to an inflammatory process, resulting in chronic inflammation and leaflet calcification; this was previously described as a ‘degenerative’ process [4]. The increased prevalence of aortic valve disease has been linked to ageing [5]. Therefore, it is reasonable to assume that the incidence of significant aortic valve disease will continue to grow in proportion with the ageing population.
SAVR has long been accepted as the gold standard in treatment of significant aortic valve disease [6], as there is significant mortality associated with untreated aortic stenosis [7]. With significantly advancing techniques in aortic valve treatments, an evaluation of the current outcomes is important; it is important to provide ongoing evaluation of current data in the high-risk octogenarian population, as new developments in aortic valve treatments continue to emerge.
Percutaneous aortic valve implantation was developed at the start of this century, and steady improvement, coupled with much enthusiasm regarding this novel approach, has been shown in various publications [8]. Cardiac surgery is still considered the mainstay of treatment to appropriate candidates; however, procedures such as the transcatheter aortic valve implantation (TAVI) have made a significant mark in the treatment of severe aortic valve disease, with some promising features as an option for high-risk patients [9].
The EuroSCORE II risk stratification tool is a validated model for predicting mortality following cardiac surgery and, following its most recent revision, has been shown to yield improved accuracy in estimation for individual patient risk [10].
Aim of the study
The aim of this study is to evaluate the outcomes of octogenarians undergoing surgical aortic valve replacement, with the goal of identifying pre-operative prognostic factors for post-operative morbidity or mortality. Assessment of post-operative mobility and discharge destination was also assessed, something that has not previously been taken into consideration in octogenarians undergoing SAVR.
Methods and statistical analysis
Study design
A single-centre, retrospective observational study involved all 85 octogenarian patients who underwent aortic valve surgery between January of 2011 and July of 2016 at St George Hospital, a large metropolitan hospital in Sydney, Australia. Data were de-identified and a study number was assigned to each patient. Electronic and paper records were used.
Inclusion criteria
To minimise bias, consecutive patients meeting the selection criteria were enrolled, and individual patient data were extracted from the hospital database.
Exclusion criteria
All non-octogenarian patients, in conjunction with all those who had not undergone surgical aortic valve replacement, were also excluded.
Variables and data included
Data items included patient demographics, pre-operative co-morbidities, functional status, echocardiographic and angiographic results, operative information, post-operative outcomes, and discharge destination. Intra-operative details and cardiopulmonary bypass details were also included. Post-operative data included complications, functional assessments, ICU length of stay, days of bed rest, total length of stay, and discharge destination.
The EuroSCORE II online calculator was used for risk stratification [11]. Scores are displayed as a percentage dictating chance of in-hospital mortality [12].
Patient mortality data were acquired in two ways. First, the data were obtained from our health district electronic medical records system (Cerner eMR Powerchart©), which details the date and cause of death for patients who have presented to the hospital and subsequently died during their admission. Second, the Ryerson index was used for all additional cases. The Ryerson index is an online database [13] that collates dates of death from published obituaries Australia-wide, inclusive of full name, date of birth, and home address.
Primary and secondary outcomes
The primary endpoint was defined as all-cause mortality during the peri-procedural period (30 days) or during same hospitalisation, whichever is longer. Secondary endpoints were defined as all-cause mortality at 1 year and all-cause mortality beyond 1 year.
Statistical analysis
A descriptive analysis of patient characteristics, pre-operative echocardiographic findings, and operative outcomes was undertaken by summarising means and standard deviations for continuous variables and frequencies and percentages for categorical variables.
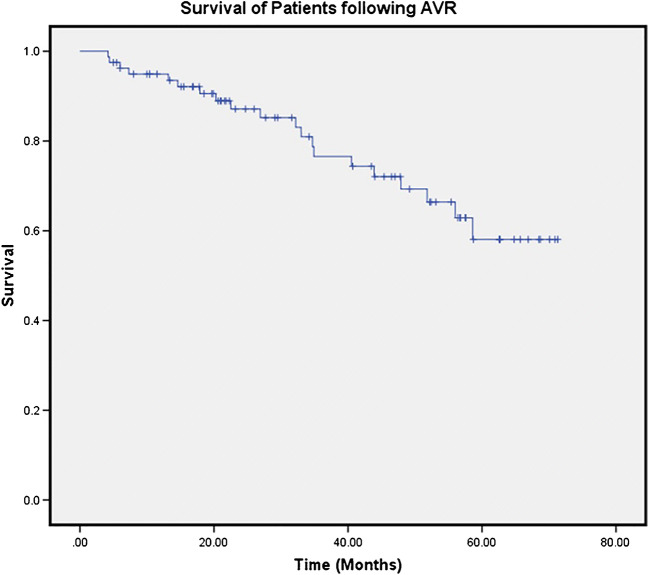
The Kaplan-Meier curve analysed survival time following AVR. Long-term survival was obtained by use of an electronic medical records system which encompasses a large area, in conjunction with the Ryerson index
To assess factors associated with operative outcomes, Student’s t test was used to compare age and other factors measured on a continuous scale with length of stay; and a one way ANOVA test was used to compare means where three or more independent groups were being analysed. In order to compare pre-operative co-morbidities with post-operative complications, a chi-square test was used where two categorical samples were being analysed, and similarly, Student’s t test was used when two continuous samples were being analysed.
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS). P values < 0.05 were considered statistically significant.
Results
A total of 85 patients between January of 2011 and July of 2016, aged 80 years and above, were identified as undergoing aortic valve surgery at St George Hospital. The group’s mean age was 82.7 years (± 2.9), 67% of whom were male. The mean EuroSCORE II was 8.1 (± 7.6), with a mean BMI of 33.0 (± 10.5). Patients’ pre-operative co-morbidities are listed in Table 1. The most common co-morbidities were dyslipidaemia, hypertension, angiographically demonstrated significant ischaemic heart disease, and moderate pulmonary hypertension (82.4%, 82.4%, 78.8%, and 58.8%, respectively). Of note, smoking status was not able to be obtained for 5 patients on review of medical records. Males were more likely to have been smokers and have ischaemic heart disease (P = 0.003 and 0.021, respectively). However, no single pre-operative co-morbidity was a significant predictor of post-operative issues or discharge destination.
Table 1.
Pre-operative demographics and characteristics
| Mean | StDev | |
| Age (years) | 82.7 | ± 2.9 |
| EuroSCORE II (%) | 8.1 | ± 7.6 |
| BMI (kg/m2) | 33.0 | ± 10.5 |
| n | % | |
| Male | 57 | 67.1 |
| Hypertension | 70 | 82.4 |
| Dyslipidaemia | 70 | 82.4 |
| IHD | 67 | 78.8 |
| Previous smoker | 36 | 42.4 |
| Pulmonary hypertension | ||
| Mild (25–30 mmHg) | 11 | 12.9 |
| Moderate (31–55 mmHg) | 50 | 58.8 |
| Severe (> 55 mmHg) | 4 | 4.7 |
| CKD | 34 | 40.0 |
| Diabetes mellitus | 26 | 30.6 |
| Diabetes requiring insulin | 3 | 3.5 |
| CCF | 15 | 17.6 |
| PVD | 14 | 16.5 |
| Chronic lung disease | 12 | 14.1 |
| Neurological event | 11 | 12.9 |
StDev standard deviation, BMI body mass index, IHD ischaemic heart disease, RVSP right ventricular systolic pressure, PVD peripheral vascular disease, CCF congestive cardiac failure, CKD chronic kidney disease
Pre-Operatively, patients were evaluated via echocardiography for assessment of parameters (Table 2) including, but not limited to, left ventricular ejection fraction (LVEF), valvular function, and structure. LVEF and valvular impairment were defined as per the American Society of Echocardiography guidelines [14]. A bicuspid aortic valve was noted in 6 patients (7.1%).
Table 2.
Pre-operative echocardiographic findings
| n | % | |
|---|---|---|
| LVEF (%) | ||
| Normal | 53 | 62.4 |
| Mild | 18 | 21.2 |
| Moderate | 6 | 7.1 |
| Severe | 7 | 8.2 |
| Aortic valve | ||
| Stenosis: moderate or severe | 79 | 92.9 |
| Regurgitation: moderate or severe | 9 | 10.6 |
| Mitral valve | ||
| Stenosis: moderate or severe | 2 | 92.4 |
| Regurgitation: moderate or severe | 11 | 12.9 |
| Bicuspid valve | 6 | 7.1 |
LVEF left ventricular ejection fraction
Pulmonary artery systolic pressure (PASP) was estimated solely from the non-invasive pre-operative echocardiograms, with findings illustrated in Table 1. Pulmonary artery hypertension (PAH) ranges for severity of disease were defined as per the same ranges utilised in the EuroSCORE II algorithm. Fifty patients (58.8%) were noted to have moderate pulmonary hypertension, while four (4.7%) were classified as severe.
Table 3 demonstrates operation types including isolated AVR (n = 37, 43.5%), AVR with concomitant CABG (n = 39, 45.9%), and others which included concomitant mitral valve surgery (n = 4), left atrial appendage ligation (n = 1), and aortic surgery (n = 4). All procedures were performed via a median sternotomy. Just under one-quarter of all surgical interventions included redo sternotomy (23.5%). Elective procedures were performed in 45 cases (52.9%) where patients were admitted from their usual place of residence; 37 cases (46.5%) were classified as urgent where patients were brought to the hospital’s emergency department and were operated upon while on an inpatient, and on three occasions (3.5%), emergency surgery had to be performed. Two emergency operations were AVR with bypass grafting, and the third was an isolated AVR.
Table 3.
Operative details
| Type of surgery | n | % |
| AVR + CABG | 39 | 45.9 |
| Isolated AVR | 37 | 43.5 |
| AVR + other | 9 | 10.6 |
| Urgency classification | n | % |
| Elective | 45 | 52.9 |
| Urgent | 37 | 43.5 |
| Emergency surgery | 3 | 3.5 |
| Other peri-operative details | n | % |
| Redo sternotomy | 20 | 23.5 |
| Active infective endocarditis | 2 | 2.4 |
| Pre-op IABP | 8 | 9.4 |
| Post-op IABP | 3 | 3.5 |
| Operative times | Mean | StDev |
| Operation time (hours ± SD) | 4:14 | ± 1:08 |
| CPB time (minutes ± SD) | 135 | ± 46 |
| Cross-clamp time (minutes ± SD) | 96 | ± 31 |
AVR aortic valve replacement, CABG coronary artery bypass grafting, IABP intra-aortic balloon pump, CPB cardiopulmonary bypass, StDev standard deviation
The post-operative outcomes are presented in the table below (Table 4). Prolonged ventilation (> 24 h) was required in 14 cases (16.5%). Inotropic use for greater than 24 h was required in 27 patients (31.8%). Five cases (5.9%) required re-intubation; however, there were no tracheostomies required due to extended periods of ventilation. A cardiac arrest occurred in seven patients (8.2%), four of these events unfortunately resulted in death; specific details were not analysed; however, the rate of arrests is slightly higher when compared with other studies [8, 15, 16]. A neurological event, which included both cerebro-vascular accidents (CVAs) and transient ischaemic attacks (TIAs), was noted in 2 (2.4%) patients. Atrial arrhythmias were the abnormal rhythm most commonly noted, with new atrial fibrillation (AF) noted in 36 cases (42.4%). Pacemaker implantation while the patients remained in hospital was required in 5 cases (5.9%).
Table 4.
Post-operative complications
| Post-op complications | n | (%) |
|---|---|---|
| Prolonged inotropes | 27 | (31.8) |
| Prolonged ventilation | 14 | (16.5) |
| Chest drain | 5 | (5.9) |
| Re-intubations | 5 | (5.9) |
| Take back: sternal instability | 3 | (3.5) |
| Take back: haemodynamic instability | 1 | (1.2) |
| Sternal wound infection | 0 | (0.0) |
| Atrial fibrillation (AF) | ||
| New AF | 36 | (42.4) |
| Chronic AF | 10 | (11.8) |
| AKI | ||
| Stage 1: Creat > 0.5–1× baseline | 28 | (32.9) |
| Stage 2: Creat > 1–3× baseline | 7 | (8.2) |
| Stage 3:Creat > 3× baseline | 1 | (1.2) |
| New long-term dialysis | 3 | (3.5) |
| Delirium | 22 | (25.9) |
| Pneumonia | 9 | (10.6) |
| Arrest | 7 | (8.2) |
| PPM | 5 | (5.9) |
| Sepsis | 5 | (5.9) |
| Neurological event | 2 | (2.4) |
AKI acute kidney injury, Creat creatinine, PPM permanent pacemaker
Sepsis was noted in five cases (5.9%); all were of a respiratory or genitourinary source. There were nine occasions (10.6%) where pulmonary changes suggestive of pneumonia were noted and treatment commenced. Acute kidney injury where the creatinine value doubled was noted on seven instances (8.2%), a tripling in its value was seen on a single patient (1.2%), and new dialysis which extended beyond the period of admission was required for three patients (3.5%). Acute kidney injury staging was based on the KDIGO practice guidelines [17].
On a single occasion (1.7%), a patient required take back to theatre for haemostasis. Three patients (3.5%) required take back to theatre due to sternal instability. It is important to note that there were no sternal wound infections or deep vein thromboses (DVTs) for the entire cohort.
Patients underwent a repeat transthoracic echocardiogram on day 5 following operative management, results of which are demonstrated in Table 5. Aortic valves sizes were carefully selected by the operator to the optimal size according to each individual patient. Aortic mean gradients had normalised following surgical AVR, and it is important to note that there was minimal aortic regurgitation following on from the procedure.
Table 5.
Post-operative echocardiographic findings
| Median | StDev | |
| Valve size (mm) | 23 | ± 1.9 |
| AV peak gradient (mmHg) | 26 | ± 12.5 |
| AV mean gradient (mmHg) | 14 | ± 7.0 |
| AV DI ratio | 0.47 | ± 0.1 |
| n | % | |
| Post-implantation AR | ||
| No AR | 34 | 40.0 |
| Trivial AR | 32 | 37.6 |
| Mild AR | 10 | 11.8 |
| Moderate AR | 0 | 0 |
| Severe AR | 0 | 0 |
StDev standard deviation, AV aortic valve, DI dimensionless index, AR aortic regurgitation
Table 6 demonstrates the median length of stay in days, including days spent within the ICU and total length of stay in the hospital. Days of bed rest were assessed when a patient would be able to perform a sit-to-stand manoeuvre with the assistance of a doctor, nurse, or physiotherapist. Increased age was associated with increased overall length of stay (P = 0.049) however not for length of stay in the intensive care unit. When separated into discharge destination, EuroSCORE II was associated with discharge destination (p = 0.013), with lower scores predicting discharge home and higher scores predicting discharge to a rehabilitation facility or death. The individual mean EuroSCORE II for patients being discharged home, to a rehabilitation, and deceased were 6.8%, 12.3%, and 11.4% respectively.
Table 6.
Discharge destination
| Median | StDev | |
| Total length of stay (days) | 10 | ± 6.9 |
| Total ICU length of stay (days) | 4 | ± 3.1 |
| Total days of bed rest (days) | 3 | ± 3.0 |
| Discharge destination | n | % |
| Home | 61 | 71.8 |
| Rehabilitation | 18 | 21.2 |
| Nursing home | 1 | 1.2 |
| Deceased | 5 | 5.9 |
| Re-admission within 30 days | 11 | 12.9 |
| 30-day mortality | 5 | 5.9 |
StDev standard deviation, ICU intensive care unit
There were five in-hospital deaths documented during the study period, all of which were related to cardiorespiratory causes, and total 30-day mortality remains unchanged from the five in-hospital deaths that we observed.
Long-term survival was obtained by use of an electronic medical records system which encompasses a large area, in conjunction with the Ryerson index. The Kaplan-Meier survival curves for the length of time post-SAVR for the octogenarian population until occurrence of the primary endpoint were presented in Fig. 1. The survival graph (Fig. 1) demonstrates graphs recorded events where patients have died, and allows for an estimation of survival in the post-SAVR octogenarian population. It is important to note that 25 patients had data to time of death, and fifty-two patients showed survival beyond 1 year. Eight patients had less than 6 months’ worth of follow-up data post-surgical intervention. According to the graph below, survival following the procedure is estimated at 92% at 1 year and 85% at 2 years..
Fig. 1.
Kaplan-Meier survival graph
Table 7 below provides specific data surrounding the five patients who passed away within 30 days of operation. Four cases were urgent procedures and two were isolated AVRs. The EuroSCORE II ranged from 1 to 17, with higher scores noted in the urgent cases. The most significant co-morbidities were that of significant pulmonary hypertension or poor left ventricular function pre-operatively. An intra-aortic balloon pump was required in three cases.
Table 7.
Individual mortality details
| Age/gender | 81/F | 82/F | 80/F | 81/M | 81/M |
| Operation type | AVR | AVR | AVR+CABG | AVR+CABG | AVR+MVR |
| Urgency classification | Elective | Urgent | Urgent | Urgent | Urgent |
| EuroSCORE II | 1.5 | 14.0 | 17.7 | 12.1 | 12.1 |
| Length of stay in ICU | 19 | 2 | 12 | 6 | 7 |
| Days of bed rest | 20 | 2 | 12 | 8 | 7 |
| Post-op complications |
Post-op IABP AKI Delirium Sepsis Cardiac arrest |
Pre-op Mod Pulm HTN Post-op IABP 8-h Op time AKI AF Cardiac arrest |
Pre-op Severe LVEF Pre-op Mod Pulm HTN AKI Re-intubation AF Cardiac arrest |
Pre-op severe LVEF Pre-op Mod Pulm HTN Pre-op IABP Pneumonia Delirium Re-intubation Cardiac arrest |
Pre-op Mod Pulm HTN 7-h OP time Pneumonia AKI AF |
| Days in hospital | 20 | 15 | 14 | 9 | 7 |
F female, M male, AVR aortic valve replacement, CABG coronary artery bypass grafting, MVR mitral valve replacement, ICU intensive care unit, Pre-op pre-operative, Post-op post-operative, Op time operative time, IABP intra-aortic balloon pump, AKI acute kidney injury, Mod Pulm HTN moderate pulmonary hypertension, AF atrial fibrillation, LVEF left ventricular ejection fraction
Discussion
Results from this study show favourable outcomes for the octogenarian population and are in keeping with previously reported data in this age group. Mortality is within expected limits (5.9%) and comparable with data published in this age group undergoing aortic valve surgery [15, 16, 18–21]. A great majority of patients were well enough to be discharged directly to their homes (71.8%), with encouragingly short admission times, a median of 10 days.
Despite high EuroSCORE II values for the majority of our patients, our data adds to overall suggestions that the octogenarian population can be considered eligible for SAVR and should not be excluded due to age alone.
The total length of time spent in the dedicated coronary intensive care unit (CICU) showed a median of 4 days (± 3.4) until transfer to the ward. The number of Days of bed rest was defined as the first post-operative day in which a patient was noted to march on the spot during their once daily mobility assessment, which was found to be a median of 3 days (± 3.3). The total length of stay for patients who underwent aortic valve surgery was a median of 10 days (± 7.5).
The majority of our cohorts’ discharge destination was back to their home, with 61 patients (71.8%) of the entire group doing so. Eighteen patients (21.2%) required longer term in-hospital rehabilitation, while only a single patient (1.2%) was discharged to a higher level care facility. Re-admission rates within 4 weeks were relatively low, with 11 patients (12.9%) requiring re-hospitalisation for any reason.
Overall, our study suggests similar findings in post-operative complications to previously published data. The most commonly noted post-operative issue was that of new onset post-operative atrial arrhythmias, such as atrial fibrillation. This was noted in 42.4% of our patients, which is within normal reported values from previous studies [15, 19]. Post-operative delirium was noted in 25.9% of patients, and despite a significant proportion of patients experiencing delirium, it did not seem to alter clinical endpoints.
In our 5.5-year time period, four patients required unplanned return to theatre, three of whom required sternal re-wiring, and a single patient was returned to theatres to achieve haemostasis. It is important to note that there were no sternal wound infections for the entire cohort, which reflects careful consideration and management of the multiple factors associated with wound care.
Patients with any significant cardiac ventricular failure were assessed for their requirement for intra-aortic balloon pump (IABP) insertion. Nine patients required pre-operative insertion of an IABP, and a further 3.5% required post-operative IABP insertion in instances where weaning from cardiopulmonary bypass proved difficult; and patients were thought to benefit from counter-pulsation. Two out of the three deaths noted in this time period were those of patients who required post-operative insertion of an IABP, while the other patient who died required pre-operative insertion of an IABP.
Complications that have long-term to lifelong impact on patient’s quality of life are those of greatest concern for most patients. There were 7 cardiac arrests (8.2%) noted in our cohort, which was the ultimate cause of death in three of the patients, in addition to their other co-morbidities and complications. It is important to note that there were only two neurological events, which encompass a transient ischaemic attack (TIA) or cerebro-vascular accident (CVA), throughout our entire period of observation. Neurological sequelae to cardiac operations are an often discussed factor; however, our study demonstrates low numbers of events for CVAs and TIAs combined. Pacemaker insertion rates were noted to be slightly above the reported average, with a rate of 5.9% in our cohort, ranges reported in the literature ranging between 3.5–6.6% [15, 18–20]. Dialysis extending beyond the period of admission was required for three patients, comprising 3.5% of our population.
Short-term mortality, defined as 30 days following discharge, remained unchanged from the five in-hospital deaths we observed. Following on, long-term survival curves have shown similar rates of mortality to other comparable studies published. Within the first year, survival is expected to be above 90% and around 85% at 2 years, figures which remain consistent throughout published data [15, 19–21]. Follow-up showed that 52 patients were alive at the 1-year mark. This finding is better than those reported in the large-scale high-risk TAVI vs SAVR studies [8] and is very likely due to careful patient selection, with some potential contributions from attrition of data when collecting long-term survival data.
Limitations
Limitations of our study include a small sample size, no randomisation, and no control group. Selection bias would have played a role, where only patients who required surgery and were fit to do so would be offered surgical management. Performance bias was addressed by having a continuous inclusion of all octogenarians having undergone surgery during the specified time period. Reporting bias is difficult to account for, as information collected is reliant on accurate reporting of the variables of interest. Patients included only represent the interventional arm, which is aortic valve replacement, with no direct comparators. Attrition bias was present in the collection of smoking status for five patients, and post-operative echocardiograms for eight patients, five of whom were deceased, where issues obtaining appropriate imaging limited our reported findings. Post-operative prosthesis mismatch was not included in the post-operative analysis. Long-term survival data was collected from electronic medical records which are not all inclusive but however encompass the health districts to which our patients are more likely to attend. In conjunction with the electronic medical records, patient data which we could not account for was cross-referenced with the Ryerson index, a database which was used to determine further mortality of patients.
Conclusions
In conclusion, morbidity and mortality in octogenarians following aortic valve surgery remains low and our institution’s findings lie within previously reported ranges. Age alone should not be considered a predictive factor for consideration of surgery. The use of the EuroSCORE II index accurately predicts adequacy to undergo surgery; however, even high-risk scores do not entirely predict overall course of events, and proceduralist discretion should still be used. At the time of this study, TAVI was rarely available and still was in its early stages. TAVI continues to gain traction in Australia and even at this stage continues to find its place in the Australian health care system, with greater degree of availability with each year that passes.
Funding
Nil.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (SESLHD NSW Health Ethics Committee – HREC ref. no. 16/088 (LNR/16/POWH/173)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Taken and complied.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Australian Bureau of Statistics (ABS) 2014. Australian historical population statistics, 2014. ABS cat. No. 3105.0.65.001. Canberra: ABS.
- 2.ABS 2017. Australian demographic statistics, Jun 2016. ABS cat. No. 3101.0. Canberra: ABS.
- 3.Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The Tromsø Study Heart. 2012;99:396–400. doi: 10.1136/heartjnl-2012-302265. [DOI] [PubMed] [Google Scholar]
- 4.Freeman RV, Otto CM. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111:3316–3326. doi: 10.1161/CIRCULATIONAHA.104.486738. [DOI] [PubMed] [Google Scholar]
- 5.Seco M, Edelman JJ, Forrest P, et al. Geriatric cardiac surgery: chronology vs. biology. Heart Lung Circ. 2014;23:794–801. doi: 10.1016/j.hlc.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Walther T, Blumenstein J, van Linden A, Kempfert J. Contemporary management of aortic stenosis: surgical aortic valve replacement remains the gold standard. Heart. 2012;98:iv23–iv29. doi: 10.1136/heartjnl-2012-302399. [DOI] [PubMed] [Google Scholar]
- 7.Melby SJ, Zierer A, Kaiser SP, et al. Aortic valve replacement in octogenarians: risk factors for early and late mortality. Ann Thorac Surgery. 2007;83:1651–1656. doi: 10.1016/j.athoracsur.2006.09.068. [DOI] [PubMed] [Google Scholar]
- 8.Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien SM, Shahian DM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2—isolated valve surgery. Ann Thorac Surg. 2009;88:S23–S42. doi: 10.1016/j.athoracsur.2009.05.056. [DOI] [PubMed] [Google Scholar]
- 10.Noyez L, Kievit PC, van Swieten HA, de Boer MJ. Cardiac operative risk evaluation: the euro SCORE II, does it make a real difference? Neth Heart J. 2012;20:494–498. doi: 10.1007/s12471-012-0327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.New EuroSCORE II (2011). [Internet] Euroscore.org. Cited 5 November 2018, from http://www.euroscore.org/calc.html
- 12.Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–744. doi: 10.1093/ejcts/ezs043. [DOI] [PubMed] [Google Scholar]
- 13.THE RYERSON INDEX [Internet]. Ryersonindex.org. 2018 [cited 5 November 2018]. Available from: https://www.ryersonindex.org/.
- 14.Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22:1–23. doi: 10.1016/j.echo.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 15.Ditchfield JA, Granger E, Spratt P, et al. Aortic valve replacement in octogenarians. Heart Lung Circ. 2014;23:841–846. doi: 10.1016/j.hlc.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Ho Edwin, Mathur Manu N., Brady Peter W., Marshman David, Brereton Russell J., Ross Donald E., Bhindi Ravinay, Hansen Peter S. Surgical Aortic Valve Replacement in Very Elderly Patients Aged 80 Years and Over: Evaluation of Early Clinical Outcomes. Heart, Lung and Circulation. 2014;23(3):242–248. doi: 10.1016/j.hlc.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 18.Harris RS, Yan TD, Black D, et al. Outcomes of surgical aortic valve replacement in octogenarians. Heart Lung Circ. 2013;22:618–626. doi: 10.1016/j.hlc.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 19.Dell'Amore A, Aquino TM, Pagliaro M, Lamarra M, Zussa C. Aortic valve replacement with and without combined coronary bypass grafts in very elderly patients: early and long-term results. Eur J Cardiothorac Surg. 2012;41:491–498. doi: 10.1093/ejcts/ezr029. [DOI] [PubMed] [Google Scholar]
- 20.Timek TA, Turfe Z, Hooker RL, et al. Aortic valve replacement in octogenarians with prior cardiac surgery. Ann Thorac Surg. 2015;99:518–523. doi: 10.1016/j.athoracsur.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Wang T, Choi D, Ramanathan T, Ruygrok P. Eight-year cohort study of octogenarians undergoing aortic valve replacement with or without concurrent coronary artery bypass grafting. Heart Lung Circ. 2015;24:S96. doi: 10.1016/j.hlc.2015.06.818. [DOI] [PubMed] [Google Scholar]