Abstract
A 27-year-old male had an abdominal violation in a prison 14 years before the display of his symptoms and was misdiagnosed as massive haemothorax. The patient remained asymptomatic for 14 years and his symptoms were only a mild dyspnoea and mild dysphagia. This patient had a huge chronic postdiaphragmatic hernia with most of the abdominal organs in the left hemithorax. A left thoracotomy was performed and a mesh was used to close the huge posttraumatic diaphragmatic hernia (diameter of 15 cm), after repositioning the abdominal organs. The left lung was completely consolidated and required dissection of multiple adhesions and high pressure manual ventilation to reexpand normally. Blunt post-traumatic diaphragmatic ruptures may be misdiagnosed and become chronic asymptomatic hernias for several years. Once they become symptomatic, they have to be treated as soon as possible as major organ injuries may be hidden.
Electronic supplementary material
The online version of this article (10.1007/s12055-018-0658-7) contains supplementary material, which is available to authorized users.
Keywords: Traumatic diaphragmatic hernia, Diaphragmatic rupture, Dyspnoea
Introduction
Blunt diaphragmatic injuries (BDI) are quite uncommon (0.8–1.6%) [1, 2]. Usually, these are related to traffic collision [3]. These occur mainly on the left hemidiaphragm, as the right one is protected by the liver [4]. BDI are associated with chest and abdominal organ injuries and consequently with a high morbidity and mortality rate (18%) [5, 6]. The diagnosis of the diaphragmatic rupture may go unnoticed and may be delayed or misdiagnosed, increasing thus the morbidity and/or mortality, or becoming a chronic diaphragmatic hernia. The usual treatment in the acute phase is laparotomy with an abdominal incision [7], in order to treat any abdominal organ injuries and at the same time repair the diaphragmatic rupture [8, 9]. Repair of chronic diaphragmatic rupture is usually performed through an open thoracotomy or VATS procedure [10], as adhesions usually develop between abdominal and thoracic structures. In the literature, the number of case reports is small, and they concern mainly cases with acute diaphragmatic hernias.
Case report
A 27-year-old otherwise healthy man was referred to our clinic from a small peripheral hospital with acute symptoms of light dyspnoea and swallow difficulties, without any chest or abdominal infection or pain. They report that a radiographic abnormality on the left hemithorax looked like pleural effusion. On arrival to our hospital, the patient recounted that 14 years ago, he fell victim to a violent torture in a prison. Characteristically, he mentioned to us that he received multiple blows in his abdomen, and because of acute dyspnoea, he was transferred urgently to the prison hospital. He underwent a chest x-ray, and a drain had been inserted in his left hemithorax, in order to evacuate a large haemothorax. Also, he mentioned that he required a lot of blood transfusion at that time. As no post-drain insertion x-ray or other radiological examination was performed to the patient, the rupture of the left hemidiaphragm was misdiagnosed and treated as a left massive haemothorax.
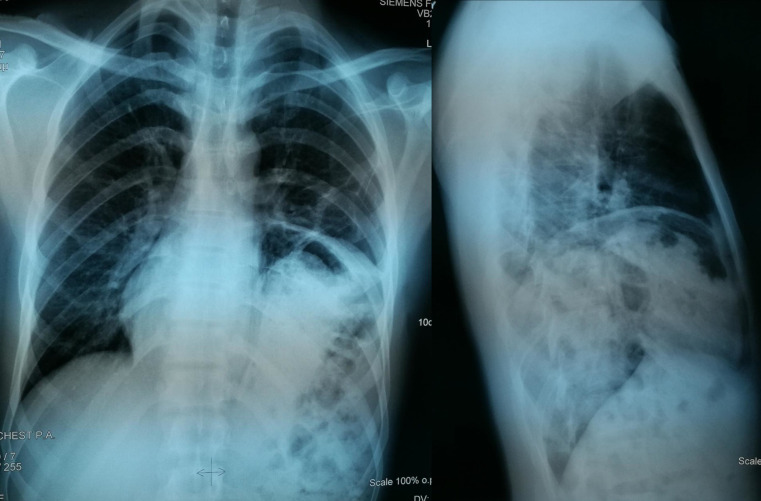
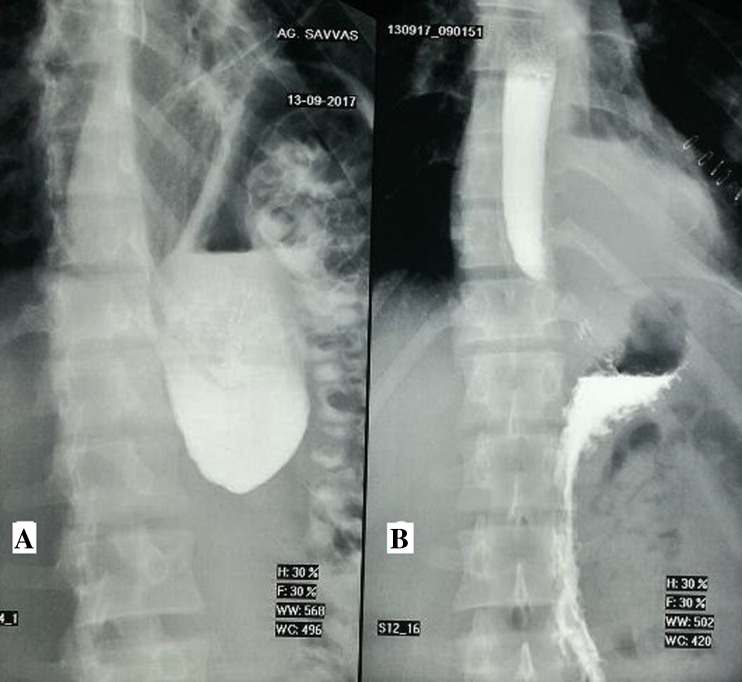
Once the patient consented, we performed an anteroposterior and lateral chest X-ray (CXR) which was clearly showing the presence of the stomach and the large bowel in the left hemithorax (Fig. 1). CT scan also showed the presence of the spleen, the small and the large bowel and the omentum inside the left hemithorax (Fig. 2). The spleen seemed enlarged and abnormal, having the image of a large haematoma. A fluoroscopy with barium swallow was performed preoperatively confirming all those findings described above (Fig. 3a) also shows paradoxical movement of the left hemidiaphragm. A preoperative spirometry was performed and was normal. Preoperative blood screen was normal.
Fig. 1.
Preoperative x-rays show clearly the presence of abdominal organs inside the left hemithorax
Fig. 2.
Preoperative CT scan shows clearly the presence of the stomach, the large bowel and the spleen inside the left hemithorax
Fig. 3.
Barium swallow x-rays. a Preoperative. The stomach and the large bowel seem clearly inside the left hemithorax. b Postoperative. The left hemidiaphragm and all abdominal organs are in normal position
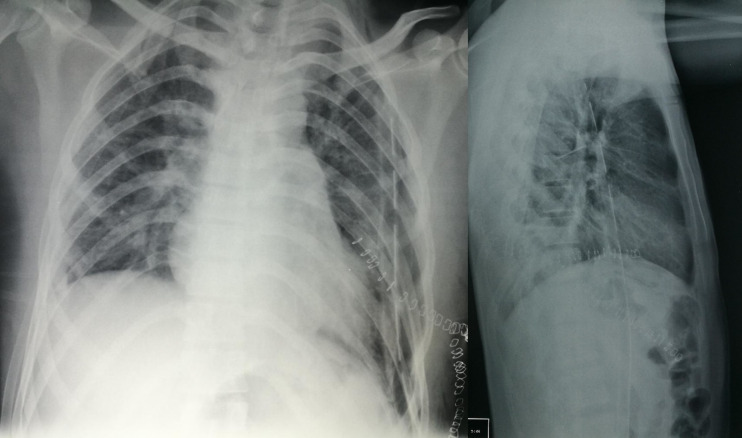
After the preoperative evaluation and under general anaesthesia, the patient was intubated with a double-lumen endotracheal tube, and once placed in right lateral position, a left posterolateral thoracotomy was performed at the seventh intercostal space. A lot of adhesions were found and dissected between the abdominal organs and the chest wall. The spleen was found to be enlarged with a post-traumatic aspect. The spleen, stomach, omentum and large and small intestines were found in the left pleura [video 1]. The diaphragmatic deficit had a diameter of 15 cm, and because of its very low position, the thoracic incision was extended anteriorly for another 5 cm. All abdominal organs were inserted carefully in the abdomen through the diaphragmatic deficit [video 2]. This was closed using a mesh with interrupted 3/0 silk sutures [video 3]. Releasing the anaesthetic block, the left lung was completely consolidated and a lot of adhesions were found and dissected between the lobes. It required several minutes of high pressure (30 mmHG) manual ventilation in order to re-expand totally the left lung (Fig. 4), as it had been consolidated for 14 years. One chest drain was put inside the thoracic cavity and the closure was done in layers. The patient was extubated in the operating room and was transferred to the ward with minimal oxygen support.
Fig. 4.
Postoperative chest x-rays. The left hemidiaphragm is in normal position and the left lung is full expanded
His post-operative period was uneventful, and a post-operative fluoroscopy with barium swallow showed normal position of the abdominal organs (Fig. 3b) and normal movement of the left hemidiaphragm. The patient was discharged on the fifth post-operative day without any signs of dyspnoea or swallowing difficulties. During follow-up, his clinical condition and all CXRs were normal.
Discussion
Diaphragmatic injury is an uncommon trauma and rarely occurs alone in blunt trauma. Usually, these injuries are related to traffic collision. The diaphragmatic rupture is associated with serious abdominal and thoracic injuries [4]. Seventy-five percent of the BDI occur on the left side of the diaphragm [1]. The diagnosis of diaphragmatic injuries is sometimes a challenge and requires a high index of suspicion. Early diagnosis is very important for the patient outcome as a delayed treatment may increase the morbidity and the mortality rate [8]. Diagnosis may become more difficult due to associated injuries, mainly because of presence of an excessive haemothorax or severe pulmonary contusion. The mortality rate of these injuries depends on the severity of associated injuries and the clinical condition of the patient [5]. A late diagnosis of a diaphragmatic injury may result in strangulation or obstruction of herniating abdominal organs into the thoracic cavity.
According to a study, 89% of acute diaphragmatic injuries are associated with intraabdominal injuries [2]. The spleen is the most frequently damaged organ on the left side and the liver on the right side. Chest injuries also participate to the BDI. In case of a left side diaphragmatic rupture, abdominal organs such as spleen, stomach, small bowel, large bowel and omentum may herniate in the left chest. In case of a right side diaphragmatic hernia, liver, large bowel and omentum may herniate in the right chest [5].
Delayed diagnosis of BDI is not uncommon in the emergency department. In most cases, once the diagnosis is made, an urgent laparotomy is required in order to control the intraabdominal haemorrhage. The consequence of an untreated acute diaphragmatic rupture is diaphragmatic hernia. The best approach for the latent phase of a diaphragmatic rupture is thoracotomy, because of the adhesions between the herniated abdominal and intrathoracic structures. The majority of post-operative morbidity in acute and chronic diaphragmatic repair is due to pulmonary complications [2].
However, there exist cases that chronic BDI may remain asymptomatic and may develop symptoms due to either the consolidated lung, such as recurrent infections and dyspnoea, or strangulated/obstructed organs.
Conclusion
Post-traumatic diaphragmatic hernias, even big ones, may be misdiagnosed in the acute phase and remain asymptomatic for several years. We suggest that these cases, once they become symptomatic, must be treated as soon as possible as they can hide chronic severe organ damage, such as massive lung consolidation.
Electronic supplementary material
(MP4 6030 kb)
(MP4 670 kb)
(MP4 1174 kb)
Acknowledgements
We would like to thank Mr. Iraklis Katsoulis, a general surgeon of our hospital, for his consultation and his help with this case.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The procedure performed in studies involving human participants was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient included in the study.
Contributor Information
Serafeim Chlapoutakis, Email: chlapoutakis@yahoo.com.
Vassileios Vassileiadis, Email: vnvassiliadis@gmail.com.
References
- 1.Ward RE, Flynn TC, Clark WP. Diaphragmatic disruption secondary to blunt abdominal trauma. J Trauma. 1981;21:35–38. doi: 10.1097/00005373-198101000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Shah R, Sabanathan S, Mearns AJ, Choudhury AK. Traumatic rupture of diaphragm. Ann Thorac Surg. 1995;60:1444–1449. doi: 10.1016/0003-4975(95)00629-Y. [DOI] [PubMed] [Google Scholar]
- 3.Kuo I-Ming, Liao Chien-Hung, Hsin Ming-Che, Kang Shih-Ching, Wang Shang-Yu, Ooyang Chun-Hsiang, Fang Jen-Feng. Blunt diaphragmatic rupture - a rare but challenging entity in thoracoabdominal trauma. The American Journal of Emergency Medicine. 2012;30(6):919–924. doi: 10.1016/j.ajem.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Feliciano DV, Cruse PA, Mattox KL, et al. Delayed diagnosis of injuries to the diaphragm after penetrating wounds. J Trauma. 1988;28:1135–1144. doi: 10.1097/00005373-198808000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Hanna WC, Ferri LE, Fata P, Razek T, Mulder DS. The current status of traumatic diaphragmatic injury: lessons learned from 105 patients over 13 years. Ann Thorac Surg. 2008;85:1044–1048. doi: 10.1016/j.athoracsur.2007.10.084. [DOI] [PubMed] [Google Scholar]
- 6.Fair KA, Gordon NT, Barbosa RR, Rowell SE, Watters JM, Schreiber MA. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: a new examination of a rare diagnosis. Am J Surg. 2015;209:864–868. doi: 10.1016/j.amjsurg.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 7.Ties Jill S., Peschman Jacob R., Moreno Andres, Mathiason Michelle A., Kallies Kara J., Martin Ronald F., Brasel Karen J., Cogbill Thomas H. Evolution in the management of traumatic diaphragmatic injuries. Journal of Trauma and Acute Care Surgery. 2014;76(4):1024–1028. doi: 10.1097/TA.0000000000000140. [DOI] [PubMed] [Google Scholar]
- 8.Mansour KA. Trauma to the diaphragm. Chest Surg Clin N Am. 1997;7:373–383. [PubMed] [Google Scholar]
- 9.Rosati C. Acute traumatic injury of the diaphragm. Chest Surg Clin N Am. 1998;8:371–379. [PubMed] [Google Scholar]
- 10.Scharff JR, Naunheim KS. Traumatic diaphragmatic injuries. Thorac Surg Clin. 2007;17:81–85. doi: 10.1016/j.thorsurg.2007.03.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(MP4 6030 kb)
(MP4 670 kb)
(MP4 1174 kb)