Sir,
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a global health concern since December 2019. It was feared that intermittent positive cases may indicate a reinfection as there were a number of patients who had positive reverse-transcriptase–polymerase-chain-reaction (RT-PCR) after an initial negative test [1]. The diagnosis of COVID-19 is based on detection of SARS-CoV-2 by real-time RT-PCR assay [2]. The sensitivity of RT-PCR is low in the early course of the disease, ranging between 45 and 60%, and thus may require more testing to reach a diagnosis [3]. Hospitalized COVID-19 patients had a median duration for viral conversion of 20 days after onset of symptoms [4]. One study showed that the median duration from onset of symptoms to negative RT-PCR was 24 days (interquartile range (IQR), 18–31 days) [5]. At weeks 4 and 5, the rates of positive RT-PCR were 32.1% and 5.4%, respectively [5]. Here, we describe the occurrence of intermittent positive PCR and the duration of viral PCR positivity in patients with SARS-CoV-2 infection in patients admitted to Qatif Central Hospital, Saudi Arabia.
The study included adult (>14 years of age) hospitalized patients with confirmed SARS-COV-2 infection from 1st March 2020 to 8th May 2020 who underwent multiple SARS-CoV-2 tests of respiratory tract samples, mainly nasopharyngeal swabs, by RT-PCR. Laboratory diagnosis relied on repeat testing after 48 h if patients became asymptomatic and had no documented fever for more than 3 days; and then repeat testing was done every fifth day if the initial test was positive. For removal from isolation, patients were required to have two negative consecutive tests 24 h apart with clinical improvement or stabilization.
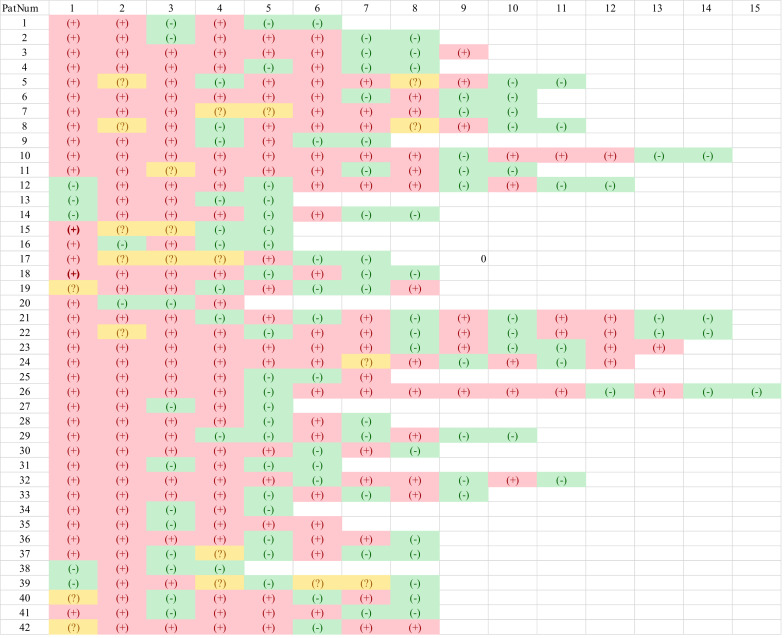
The respiratory samples were tested using RT-PCR amplification targeting the upstream E gene and S gene. The test was based on the RealStar® SARS-CoV-2 RT-PCR Kit 1.0 (Altona Diagnostics, Hamburg, Germany). The study was approved by the institutional research ethics committee of Qatif Central Hospital (QCH), Eastern Province, Saudi Arabia (4271T8361000). Positive test was defined as positivity for E and S genes; negative test was defined as negative E and S genes; and possible test was defined as negative E but positive S genes. During the study period, there were 82 confirmed COVID-19 patients and of those 42 (51%) had intermittent positive PCR tests (Figure 1 ). Of those with intermittent positive tests, 24 (57%) had eventually two consecutive negative tests and were cleared. The mean and median days to clearance were 28.9 and 31 days, respectively. In addition, 90% of patients had negative samples at day 40 from the first positive swab.
Figure 1.
The course of patients with intermittent positive SARS-CoV-2 polymerase chain reaction (PCR). Each patient is represented by a row and the columns represent the number of PCR tests since the initial encounter. Red indicates positive (+) tests; yellow possible (?) tests, and green negative (-) tests.
There are possible explanations for the appearance of positive tests after negative tests. These explanations include: initial false negative tests due to the presence of PCR reaction inhibitors or due to the sampling methodology, the first sample being below the level of detection, or false-positive tests. Previous WHO recommendations called for the discharge of COVID-19 patients after clearance of infection based on two negative RT-PCR results on sequential samples taken at least 24 h apart. However, these criteria were changed to a time-based strategy which is 10 days from the first positive sample, provided that the patient had no symptoms for at least 3 days.
Here, we observed that 51% had recurrence of a positive PCR after a negative test. In a previous study, 14.5% of COVID-19 patients had positive RT-PCR testing following discharge [6]. Similarly, in a study of 209 discharged patients 10.5% had appearance of positive PCR after initial negative tests 4.7 days after discharge [7]. Moreover, in a study of 70 COVID-19 patients, 21.4% re-tested positive after two consecutive negative PCR tests [8]. That study showed no difference in age, severity of illness or gender between those who had intermittent positive and those who did not [8].
In this study, the mean and median days to negative in those with intermittent positive was 28.9 and 31 days, respectively. Similarly, a previous study of such patients found that median time was 36 (28–40) days [8]. Kinetics of viral load in 12 severely ill COVID-19 patients requiring mechanical ventilation and 11 mild COVID-19 patients showed that viral shedding lasted about 10 days in most of the mild patients and 20–40 days in most severely affected patients [9].
In conclusion, we observed intermittent positive PCR tests for SARS-CoV-2. The study however did not address the viability of the virus as we did not have viral cultures. The persistence of SARS-CoV-2 and the development of intermittent positive tests may merely indicate the detection of viral RNA. The prolonged shedding of the virus is not an indication of continued infection without viral cultures. It is also important to understand viral dynamics in other tissues such as urine, blood and others.
Author contributions
J.M.A. gathered the data and finalized the manuscript; J.A.A. was responsible for concept design, data analysis and writing the manuscript.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Peng J., Wang M., Zhang G., Lu E. Seven discharged patients turning positive again for SARS-CoV-2 on quantitative RT-PCR. Am J Infect Control. 2020;48 doi: 10.1016/j.ajic.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang Y., Chen S., Yang Z., Guan W., Liu D., Lin Z. SARS-CoV-2 viral load in clinical samples of critically ill patients. Am J Respir Crit Care Med. 2020;201 doi: 10.1164/rccm.202003-0572LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Tawfiq J.A., Memish Z.A. Diagnosis of SARS-CoV-2 Infection based on CT scan vs. RT-PCR: Reflecting on Experience from MERS-CoV. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xiao A.T., Tong Y.X., Gao C., Zhu L., Zhang Y.J., Zhang S. Dynamic profile of RT-PCR findings from 301 COVID-19 patients in Wuhan, China: A descriptive study. J Clin Virol. 2020:127. doi: 10.1016/j.jcv.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao A.T., Tong Y.X., Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan J., Kou S., Liang Y., Zeng J.F., Pan Y., Liu L. PCR assays turned positive in 25 discharged COVID-19 patients. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang X., Zhao S., He D., Yang L., Wang M.H., Li Y. Positive RT-PCR tests among discharged COVID-19 patients in Shenzhen, China. Infect Control Hosp Epidemiol. 2020:1–7. doi: 10.1017/ice.2020.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiao A.T., Tong Y.X., Zhang S. False-negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: Rather than recurrence. J Med Virol. 2020 doi: 10.1002/jmv.25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y., Zhang L., Sang L., Ye F., Ruan S., Zhong B. Kinetics of viral load and antibody response in relation to COVID-19 severity. J Clin Invest. 2020 doi: 10.1172/JCI138759. [DOI] [PMC free article] [PubMed] [Google Scholar]