Abstract
Objectives
This report describes a modified defibrillation technique during cardiac surgery using a combined internal (epicardial) and external (transthoracic) defibrillation system.
Methods
We routinely used 30 J (J) shock between the epicardial pad placed directly onto the right atrium and the left anterolateral transthoracic pad placed in the left anterolateral chest wall directly to the skin in the area of the cardiac apex under the nipple.
Results
Thirty-two patients whom developed ventricular fibrillation (VF) during surgery were managed in theatre using this method. A single 30 J shock was successfully given in 29 patients while the remaining three required an additional shock with the same amount (30 J).
Conclusions
We believe that this technique is safe and complications free. It is easy to perform especially in patients with difficult access such as redo operations.
Keywords: Arrhythmia therapy, Defibrillation, Re-operation, Shock
Introduction
Beck was the first physician to use direct current (DC) defibrillation on a human to treat ventricular fibrillation on a 14-year-old during cardiac surgery in 1947 [1], and Zoll et al. successfully terminated ventricular fibrillation in a patient using externally applied defibrillation counter shocks [2]. Delivery of DC counter shocks to the heart has since been used successfully to convert arrhythmia to sinus rhythm. The term defibrillation applies to the use of non-synchronized DC counter shock therapy in ventricular fibrillation, and the mechanism is not known exactly [3]. Defibrillator paddles can be used in different configurations which affect the success rate of defibrillation. According to the International Liaison Committee on Resuscitation (ILCOR) guidelines, the sternal paddle should be placed just to the right of the upper sternal border below the clavicle and the apical paddle to the left of the nipple with the centre of the electrode in the midaxillary line. Internally the paddles should be placed to the right atrium and to the left ventricle [4]. Here we report our experience in a combine defibrillation technique using an internal and an external paddle. Similar methods have not been previously reported in the literature.
Materials and methods
We performed a combine defibrillation technique using external and internal paddle in 32 patients who underwent cardiac surgery (6 of them underwent redo operation). The epicardial paddle (5 cm diameter) was placed on the right atrium during the operation at the time of defibrillation for VF after release of ascending aorta cross clamp (Fig. 1). Alternatively, the internal paddle was placed in 4 cases on the right pleura over the right atrium as the pleura was severely adherent to the atrium, and it was not felt that it is safe to fully dissected away (Fig. 2). The transthoracic paddle (5 cm diameter) was placed on the left anterolateral thoracic wall under the nipple with the centre of the electrode in the 5th intercostal space over the area of the cardiac apex (Fig. 3). Internal and external paddles were connected with the defibrillator as usual, and also the external paddle was marked using silk stitch to avoid internally usage (Fig. 2).
Fig. 1.

Internal (right atrium) external (transthoracic) defibrillation
Fig. 2.
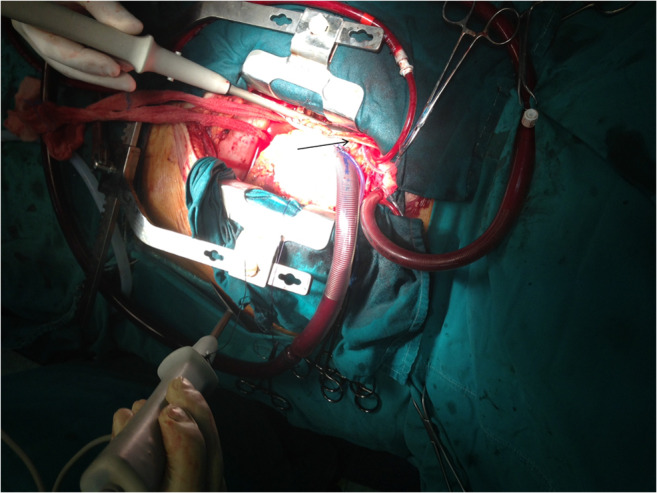
Internal paddle through the right pleura (black arrow indicates the pleura), external paddle was marked with silk stitch
Fig. 3.
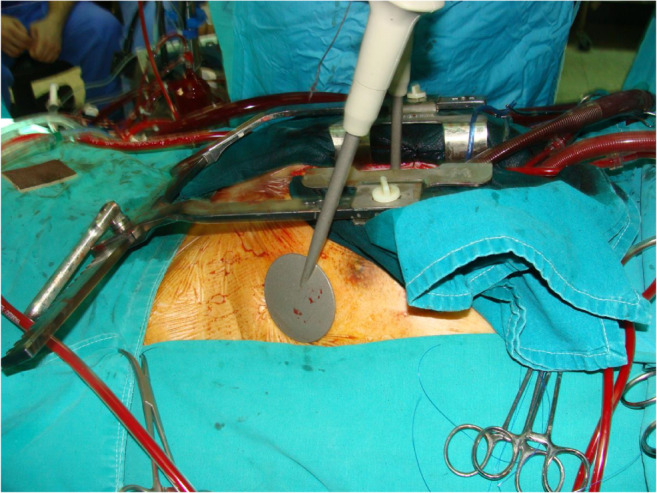
Transthoracic paddle under the right nipple
Results
An initial energy level of 30 J was successful in 29 patients (90%) including the 4 cases with the DC counter shock through the right pleura. In the remaining three cases, an additional shock of 30 J was given to establish sinus rhythm. Recurrent VF during cardiopulmonary bypass reoccurred in 1 case (3%). The core temperature during cross clamp period was 28 °C, and the defibrillation was performed during the re-warming period with a core temperature above 30 °C and after careful de-airing of the heart. Care was taken to correct hypokalaemia and acid-base balance prior to defibrillation. There were no complications such as non-sustained ventricular tachycardia, atrial arrhythmia, heart block, bradycardia, transient left bundle branch block, skin burn during or after the procedure, and no evidence of wound or chest infection postoperatively.
Discussion
The current external electrical defibrillation techniques rely on the application of a selected amount of high energy, which is generally between 150 and 360 J, via paddles. In contrary, internal DC shock or direct defibrillation, with two paddles, requires far less energy than external defibrillation, and the optimal initial energy for open-chest defibrillation is 10 to 30 J [2]. Defibrillation during cardiac surgery is influenced by a number of variables including perfusion temperature, oxygenation, serum electrolyte levels, and disease process [2]. It is known that high energy electrical shocks are damaging to the myocardium causing myocardial necrosis and release creatinine phosphokinase (CPK) [2]. Other potential complications include non-sustained ventricular tachycardia, atrial arrhythmia, heart block, bradycardia, transient left bundle branch block, transient hypotension, pulmonary oedema, and skin burn can occur in both cases [5]. However, multiple low energy shocks can be more damaging than a single high energy shocks [6]. The ability of delivering combined internal and external defibrillation in open chest surgery was not previous described, but the success of electric delivery in heart by combined internal and external implantable defibrillator was previously reported [7].
In this report, we demonstrated that the majority of arrhythmia will be terminated using the combined internal and external technique with 30 J. We believe that this can of pivotal importance when excessive left heart dissection in redo cases is not essential for the operation.
In conclusion, we would recommend the use of low energy DC counter shock with this technique as it is safe, reproducible, and easy to perform with satisfactory outcome.
Compliance with ethical standards
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zoll PM, Linenthal AJ, Gibson W, Paul MH, Norman LR. Termination of ventricular fibrillation in man by externally applied electric counter shock. N Engl J Med. 1956;254:727–732. doi: 10.1056/NEJM195604192541601. [DOI] [PubMed] [Google Scholar]
- 2.Lown B. Defibrillation and cardioversion. Cardiovascular Research. 2002;55(2):220–224. doi: 10.1016/S0008-6363(02)00416-9. [DOI] [PubMed] [Google Scholar]
- 3.Zipes Douglas P., Fischer John, King Robert M., deB. Nicoll Ann, Jolly Walter W. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. The American Journal of Cardiology. 1975;36(1):37–44. doi: 10.1016/0002-9149(75)90865-6. [DOI] [PubMed] [Google Scholar]
- 4.Kimura S, Bassett AL, Kohya T, Kozlovskis PL, Myerburg RJ. Simultaneous recording of action potentials from endocardium and epicardium during ischemia in the isolated cat ventricle: relation of temporal electrophysiologic heterogeneities to arrhythmias. Circulation. 1986;74:401–409. doi: 10.1161/01.CIR.74.2.401. [DOI] [PubMed] [Google Scholar]
- 5.Sucu Murat, Davutoglu Vedat, Ozer Orhan. Electrical Cardioversion. Annals of Saudi Medicine. 2009;29(3):201–206. doi: 10.5144/0256-4947.51775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pugsley WB, Baldwin T, Treasure T, Sturridge MF. Low energy level internal defibrillation during cardiopulmonary bypass. Eur J Cardiothorac Surg. 1989;3:273–275. doi: 10.1016/1010-7940(89)90079-1. [DOI] [PubMed] [Google Scholar]
- 7.FREDMAN CAREY S., BIERMANN KURT M., BAROLD S. SERGE, DOLAN PATRICK H., MARBARGER JOHN P., GARRETT TED E. Treatment of Refractory Ventricular Fibrillation by Combined Internal (Epicardial) and External (Transthoracic) Defibrillation. Pacing and Clinical Electrophysiology. 1996;19(6):1003–1005. doi: 10.1111/j.1540-8159.1996.tb03401.x. [DOI] [PubMed] [Google Scholar]


