Abstract
The presence of interatrial communication is considered obligatory in total anomalous pulmonary venous connection (TAPVC). Even a restriction in this communication leads to obstructive TAPVC. We report a rare case of obstructed supracardiac TAPVC with the absence of interatrial communication and with multiple ventricle septal defects (VSDs) in a 3-month-old child.
Keywords: Total anomalous pulmonary venous connection, Ventricle septal defects, Cardiopulmonary bypass
Introduction
Communication between systemic and pulmonary circulation is essential for survival in patients with total anomalous pulmonary venous connection. We report such a case wherein there was obstructed supracardiac total anomalous pulmonary venous connection with intact interatrial septum and multiple ventricle septal defects in a 3-month-old child. We have also discussed pathway of pulmonary blood flow and mechanism of its obstruction.
Case report
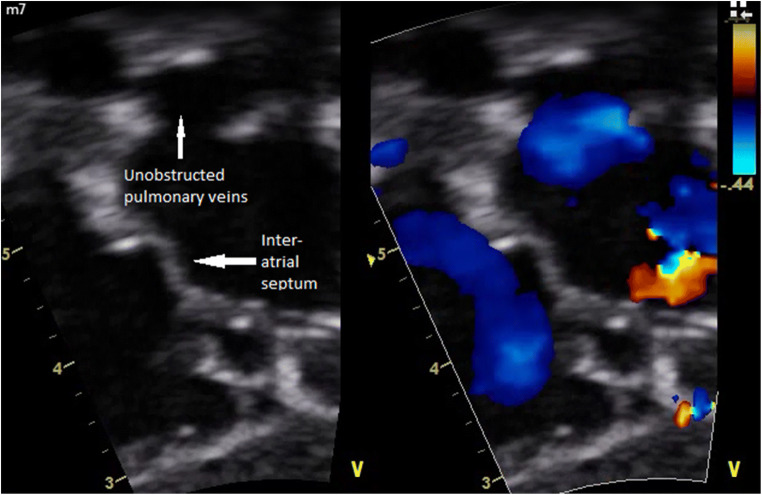
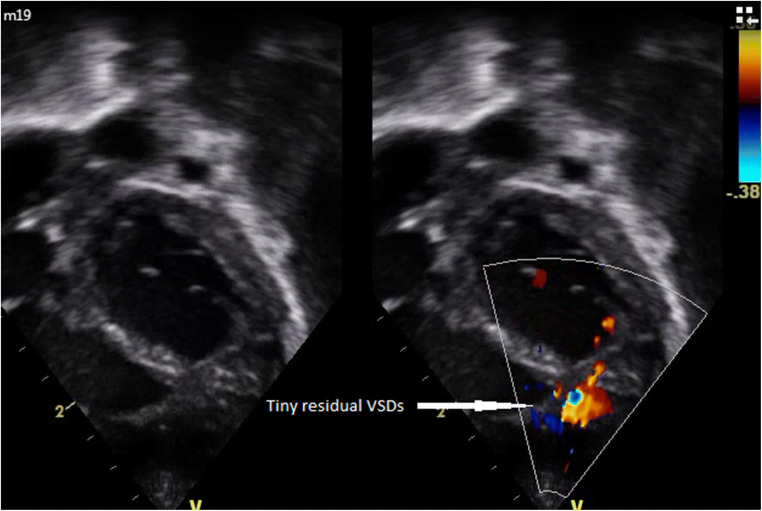
A 3-month female child presented with rapid breathing and bluish discoloration since 1 week. On examination, there was marked cyanosis, normal sized heart with parasternal heave, normal first sound, normally split second sound with accentuated pulmonic component, and insignificant murmurs. The chest X-ray showed not much cardiomegaly with pulmonary venous congestion (Fig. 1). Transthoracic echocardiography revealed supracardiac total anomalous pulmonary venous connection (TAPVC) with a vertical vein draining to the right superior vena cava. Interatrial septum was intact and bulging to left. Interventricular septum showed multiple muscular ventricular septal defect (VSD) with right to left shunt and no patent ductus arteriosus (PDA). The surgery was performed under cardiopulmonary bypass with aorto-bicaval cannulation and moderate hypothermia (30 °C). Under cardioplegic arrest, the right atrium was opened, and the absence of interatrial communication was confirmed. The apex of the heart was flipped to right pleural cavity. Left atrium was opened. The pulmonary venous chamber was opened transversely and anastomosed to the left atrium. Tricuspid valve was retracted, and moderate size mid muscular VSD was closed with a polytetrafluoroethylene patch. On injecting saline across the interatrial septum and mitral valve, left ventricle was filled and additional two tiny apical VSDs localized and were closed directly through right atrium. The patient was weaned off bypass with adrenaline (0.1 μg/kg/min) and milrinone (0.5 μg/kg/min) support, with acceptable hemodynamics. Vertical vein was ligated. The chest was closed, and patient was shifted to recovery room with stable. The patient was weaned off ventilator on 3rd postoperative day. Inotropes were tapered off by 5th postoperative day. Oral sildenafil was started and continued for 4 weeks postoperatively. The patient was discharged on 10th postoperative day. Postoperative transthoracic echocardiography done on postoperative days 1 and 7 showed no pulmonary venous obstruction, moderate pulmonary arterial hypertension, one tiny residual apical VSD, and good biventricular function (Figs. 2 and 3). At 6 months follow-up, the child is doing well with echocardiogram showing unobstructed pulmonary veins, tiny apical VSD, and mild pulmonary arterial hypertension.
Fig. 1.

Chest X-ray showing no cardiomegaly with severe pulmonary arterial hypertension
Fig. 2.
2D echocardiogram showing intact interatrial septum and unobstructed pulmonary veins
Fig. 3.
2D echocardiogram showing multiple VSDs
Discussion
Right-to-left shunt is obligatory for survival in patients with TAPVC. Usually, this shunt is at atrial level in form of an atrial septal defect or a patent foramen ovale. On rare occasions, the interatrial connection is absent. In those occasions, some other form of connection like a VSD or a PDA helps to sustain life. Very few such cases have been reported till date. Delisle and colleagues performed autopsy in 93 cases of total anomalous pulmonary venous connection. There was only one such case in their review [1]. In a case reported by Hastreiter et al., there was postmortem detection of the absence of an atrial level communication in a case of infradiaphragmatic TAPVC with PDA, which did not survive beyond 6 weeks [2]. Mishra et al. successfully operated a child with infracardiac TAPVC with intact interatrial septum at the age of 9 months. The right ventricle was supporting both systemic and coronary circulations via PDA [3]. In our patient, there was no patent foramen ovale, atrial septal defect, PDA, or levoatriocardinal vein. Instead, multiple VSDs were supporting systemic and coronary circulation. We believe this is the first reported case of successful surgery in TAPVC with intact interatrial septum and multiple VSDs. The probable mechanism of late obstruction in current case was gradual restriction of existing muscular VSDs as muscular ventricle septal defects have tendency to get restricted over the time. [4] These types of patients may present later than patients with other types of obstructed TAPVC due to gradual restriction of muscular VSDs over the time. When the obstruction gets severe enough, these patients present with symptoms of TAPVC and require urgent surgery. Postoperative recovery is excellent.
Funding
This work was supported by U.N.Mehta Institute of Cardiology and Research Center itself and received no specific grant from any funding agency, commercial or not-for-profit sectors.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights/ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional ethics committee for this study; formal ethics committee clearance was not required.
Informed consent
Informed consent was obtained from the patient.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Delisle G, Ando M, Calder AL, et al. Total anomalous pulmonary venous connection: report of 93 autopsied cases with emphasis on diagnostic and surgical consideration. Am Heart J. 1976;91:99–122. [DOI] [PubMed]
- 2.Hastreiter AR, Paul MH, Molthan ME, Miller RA. Total anomalous pulmonary venous correction with severe pulmonary venous obstruction. A clinical entity. Circulation. 1962;25:916–28. [DOI] [PubMed]
- 3.Mishra A, Garg R, Raghunath, Maheswari S, Sharma R. Total anomalous pulmonary venous connection with intact interatrial septum. Ann Thorac Surg. 2006;81:739–40. [DOI] [PubMed]
- 4.Zhang J, Ko JM, Guileyardo JM, Roberts WC. A review of spontaneous closure of ventricular septal defect. Proc (Bayl Univ Med Cent). 2015;28:516–520. [DOI] [PMC free article] [PubMed]