Abstract
Background
Addressing adolescents’ sexual and reproductive health and rights (SRHR) requires an understanding of the socio-cultural and spatial settings within which they live. One setting of particular importance is the informal settlements or ‘slums’ that are gradually dominating the urban space. We undertook a scoping review and synthesis of existing evidence on adolescent SRHR in slums in sub-Saharan Africa (SSA) focusing on the characteristics and nature of existing evidence.
Methods
The scoping review was conducted based on Arksey and O’Malley framework and in accordance with the guidance on scoping reviews from the Joanna Briggs Institute (JBI) and using PRISMA reporting guidelines for scoping reviews. A comprehensive search was undertaken in PubMed, POPLINE, African Journals Online (AJOL), Bioline International and Google Scholar. The search was confined to studies published in peer reviewed journals and reports published online between January 2000 and May 2019. Studies were included in the review if they addressed SRHR issues among adolescents living in urban slums in SSA.
Results
The review included a total of 54 studies. The majority (79.5%) of studies were quantitative. The bulk of studies (85.2%) were observational studies with only eight intervention studies. While half (27) of the studies focused exclusively on adolescents (10–19 years), 12 studies combined adolescents with other young people (10–24 years). The studies were skewed towards sexual behavior (44%) and HIV/AIDS (43%) with very few studies focusing on other SRHR issues such as contraception, abortion, gender-based violence and sexually transmitted infections (STIs) other than HIV. Most of the studies highlighted the significantly higher risks for poor SRHR outcomes among adolescents in slums as compared to their peers in other settlements.
Conclusion
Young people growing up in slums face tremendous challenges in relation to their SRHR needs resulting in poor outcomes such as early and unintended pregnancy, STIs, and sexual violence. The results of this review point to several potential target areas for programming, policy, and research aimed at improved adolescent SRHR in slums in SSA.
Keywords: Slums, SRHR, Adolescents, Scoping review, SSA
Plain English summary
Addressing adolescents’ sexual and reproductive health and rights (SRHR) requires an understanding of the socio-cultural and spatial settings within which they live. This is critical in the current context where informal settlements or ‘slums’ are gradually dominating the rapidly expanding urban space. In recognition of the unique challenges, this review highlights existing evidence on adolescent SRHR in slums in sub-Saharan Africa (SSA) with particular attention to available policy responses.
Following standard guidance on scoping reviews from the Joanna Briggs Institute (JBI) and using PRISMA reporting guidelines, data bases such as PubMed, POPLINE, African Journals Online (AJOL), Bioline and Google Scholar were searched. We confined the search to studies published in peer reviewed articles and online reports published between January 2000 and May 2019 and found a total of 54 eligible studies. Half of these studies focused exclusively on adolescents (10–19 years), while the other combined adolescents with other young people.
Results highlight significant risks for poor SRHR outcomes among adolescents in slums as compared to their peers in other settlements. Most studies examined sexual behavior (44%) and HIV/AIDS (43%) while SRHR issues such as contraception, abortion and gender-based violence were rarely considered. Overall, the findings show that young people growing up in slums face tremendous challenges in relation to their SRHR needs resulting in poor outcomes such as early and unintended pregnancy, STIs, and sexual violence.
The results point to several potential target areas for programming, policy, and research aimed at improved adolescent SRHR in slums in SSA.
Introduction
Globally, adolescents (ages 10–19 years) are a significant demographic block. In sub-Saharan Africa (SSA), adolescents account for more than 23% (or about 250 million) of the total population – a figure that is projected to increase rapidly in near future [1]. Adolescence is associated with physical, emotional and social changes that can increase vulnerability to poor sexual and reproductive health and rights (SRHR) outcomes and other risks associated with behavior change [2, 3].
Adolescents in low- and middle-income countries (LMICs) face tremendous challenges in relation to their SRHR needs. These include lack of access to SRHR information and services; lack of awareness about puberty, sexuality, and basic human rights; poverty; and inequitable gender norms that increase vulnerability to poor SRHR outcomes [4, 5]. Although adolescent SRHR is gaining global research and programmatic attention [6, 7], much of the research and program work overlooks adolescents in the fast growing urban slums in LMICs.
High rates of urbanization in SSA [1] amidst poor economic performance and weak governance has resulted in the growth of informal settlements, commonly referred to as slums. Currently, over half (55%) of urban dwellers in SSA reside in slums or slum-like environments that are characterized by dire poverty [8, 9]. Housing structures are temporary and are constructed from mud, iron sheets, cardboard boxes and polythene and plastic sheet tents. They are often located in undesirable parts of the city, such as steep hillsides, riverbanks or industrial areas [10]. The settlements are unregulated and unplanned and are thus characterized by overcrowding, poor sanitation, insecurity and poor access to social amenities. Because of their informal nature, government authorities are reluctant to provide social amenities and services such as schools, roads, and healthcare facilities. As a consequence, residents of slums have poorer health and socio-economic outcomes [10–12].
Urban slum residence creates a confluence of factors that place adolescents at heightened risk of poor SRHR outcomes [9]. For example, studies comparing SRHR outcomes between slum dwellers and non-slum dwellers in Nairobi show that slum residents are at greater risk for HIV infection, risky sexual behavior, early childbearing and maternal mortality [13–16]. Similarly, a study in Lagos, Nigeria shows that maternal mortality rates observed for two slum were higher than the figure estimated for the Lagos State [16].
Recognizing the unique challenges of urban poverty is critical in understanding the drivers of adolescent SRHR outcomes in the slum settings in order to implement effective programs for this critical age group. This review is motivated by the urgent need to understand the drivers of poor SRHR outcomes in slum settlements in SSA and inform prevention efforts. Understanding their SRHR is important for designing programs to improve health, education and employment outcomes among young people that are necessary to achieve the demographic dividend. By providing a comprehensive overview of available research and evidence on adolescent SRHR issues in slums in SSA, this review lay groundwork for a research agenda to explore key knowledge gaps concerning the nature and determinants of SRHR challenges among adolescent slum dwellers, and to inform interventions to address them.
Objective
The aims of the scoping review were to map and describe available research and evidence on adolescent SRHR in slums in SSA. Specifically, we describe the characteristics, scope, nature of existing evidence and knowledge gaps.
Methods
We conducted a scoping review method to identify and synthesize evidence on adolescent SRHR in slums in SSA. The review was conducted based on Arksey and O’Malley framework [17] and in accordance with the guidance on scoping reviews from the Joanna Briggs Institute (JBI) [18] and using PRISMA reporting guidelines for scoping reviews [19, 20]. We adopted the five-step method outlined by Arksey and O’Malley (2005): (1) identifying the research question; (2) identifying relevant studies/literature; (3) selecting studies; (4) charting the data; and (5) collating, summarizing, and reporting results.
In line with JBI guidelines, we outlined inclusion criteria for the population, concept, and context as follows:
Population
The population considered included adolescents/teenagers (ages 10–19 years), young people, general population in the slum areas.
Concept
Sexual and reproductive health outcomes such as sexual behavior; pregnancy and contraceptive use; HIV/AIDS, gender-based violence (GBV) (physical and sexual violence, intimate partner violence, female genital mutilation and early marriages).
Context
The review considered the SRHR of adolescents living in urban slums, informal settlements, inner cities or deprived neighborhoods in urban areas in SSA.
Search strategy
Prior to study selection and data abstraction, a review framework was developed to guide the identification of potentially relevant literature documents. A comprehensive search using databases was undertaken to locate articles published in peer reviewed journals and reports published online. An initial limited search of PubMed was done and text words contained in the titles and abstracts of relevant articles, and the index terms used to describe the articles were used to develop a full search strategy. Following this initial search, we searched the following databases: PubMed, POPLINE, African Journals Online (AJOL) and Bioline International and Google Scholar. The POPLINE website was retired on September 1, 2019 after our search was completed. Different combinations of the following search terms were used: Slums, informal settlements, deprived neighborhoods, inner city, sub-Saharan Africa, teenage/adolescent/ young women/people, young adolescents, SRHR of young people, sexual behavior; pregnancy, contraceptive use; HIV/AIDS, GBV (physical and sexual violence, female genital mutilation and early marriages).
Only articles written in English language published between January 2000 and May 2019 were considered. We also limited our review to studies that included adolescent girls and boys (aged 10–19 years) in their sample. We also reviewed the bibliographies of studies from the database searches to identify additional articles. Citation searches were also utilized which yielded new studies. We used Google to search for grey literature.
Study selection
Studies identified from the initial search underwent title and abstract screening. After a full-text review, data were extracted from all selected studies, including the year of publication, country and city of origin, the age and sex category of the study population, the design and type of study, whether it was a single or multi-site study, whether it was a single or multi-topic study, type of SRHR primary outcome. Studies that focused on general urbanization and/or urban poverty and health were reviewed separately and information on the substantive issue was extracted. Included papers were critically appraised using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses—Extension for Scoping Review (PRIMSMA-ScR) guideline [20].
Results
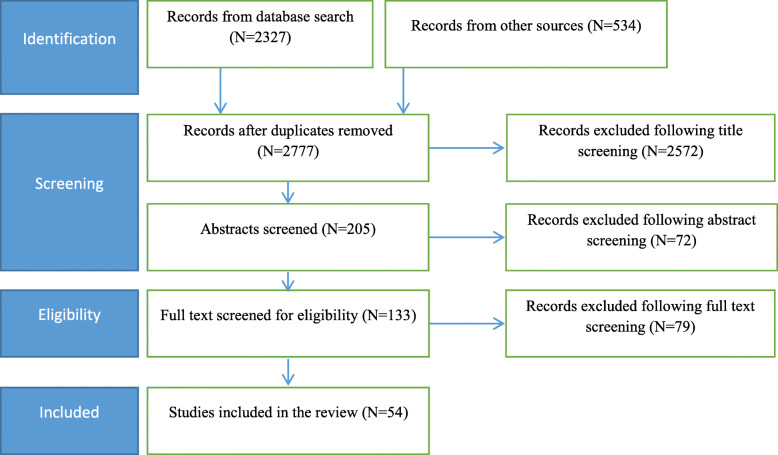
The initial search yielded a total of 2861 studies. After removing duplicates, 2777 records were left for screening. Upon completion of title and abstract screening, 72 were excluded leaving 133 full-texts deemed potentially relevant for review. Subsequently, 54 documents fulfilled our eligibility criteria and were included in this review (Fig. 1).
Fig. 1.
Study selection procedure for the scoping
The studies identified were reviewed and grouped according to the following categories: sexual behavior; pregnancy and contraceptive use; HIV/AIDs, GBV (physical and sexual violence, female genital mutilation and early marriages). These categories were subsequently used to structure the presentation of results in a systematic manner. It is worth noting that several studies addressed more than one category.
The studies encompassed a variety of study designs including cross-sectional studies, pre–post designs, randomized controlled trials, retrospective and prospective cohort studies and case–control studies (Table 1). We organize our results systematically, beginning with studies on urbanizations, slums and adolescent health in general, then we focus on specific substantive SRHR topics before turning to interventions on adolescent SRHR.
Table 1.
characteristics of studies included in the review
| Area of Focus | Number | % |
|---|---|---|
| Country | ||
| Kenya | 31 | 57.4% |
| South Africa | 9 | 16.7% |
| Ethiopia | 4 | 7.4% |
| Nigeria | 3 | 5.4% |
| Uganda | 2 | 3.7% |
| Zimbabwe | 2 | 3.7% |
| Ghana | 1 | 1.9% |
| Tanzania | 1 | 1.9% |
| Malawi | 1 | 1.9% |
| Design/ Method | ||
| Quantitative | 41 | 79.5 |
| Qualitative | 7 | 13.0% |
| Mixed method | 6 | 11.1% |
| Type | ||
| Observational | 46 | 85.2% |
| Intervention/Implementation Research | 8 | 14.8% |
| Population | ||
| Girls | 26 | 48.1 |
| Boys and Girls | 28 | 51.9 |
| Age groups | ||
| 10–19 | 18 | 33.3 |
| 15–19 | 9 | 16.7 |
| 10–24 | 12 | 22.2 |
| 15–49 | 15 | 27.8 |
| Period | ||
| 2000–2004 | 5 | 9.3 |
| 2005–2009 | 9 | 16.7 |
| 2010–2014 | 24 | 44.4 |
| 2015–2019 | 16 | 29.6 |
| Total | 54 | 100 |
Characteristics of studies on adolescent SRHR in slums
Among the studies that focused on the substantive topic of adolescent SRHR in slums in SSA, more than half (n = 31; 57.4%) were based on slums in Nairobi, Kenya’s capital city (Viwandani, Korogocho and Kibera). Nine (16.7%) studies covered settlements in South Africa (Cape Town, Johannesburg and Durban), while four (7.4%) covered Ethiopia (Addis Ababa) and three, Nigeria (Ibadan). Two studies each were based on slums in Uganda (Kampala) and Zimbabwe (Harare) while one study covered slums in Ghana (Accra), Tanzania (Dar es Salaam) and Malawi (Blantyre).
Majority 41(79.5%) were quantitative studies while qualitative and mixed methods studies accounted for 13% (n = 7) and 11% (n = 6) respectively. The bulk of studies (n = 46; 85.2%) were observational, cross-sectional studies while 14.8% (n = 8) reported on interventions or implementation research.
In terms of study population, many of the studies reviewed did not strictly adhere to the World Health Organization (WHO) definition of adolescents (i.e., those aged 10–19 years). Rather, they combined adolescents with other age groups such as young people (10–24); youths (15–24 years) and women of reproductive age (15–49 years). About half of the studies (27) focused exclusively on adolescents (10–19 years). Twelve studies combined adolescents with other young people (10–24 years), while fifteen treated them as a category in the reproductive age group (15–49 years). For half of the studies, the respondents were girls or young women while the other half combined boys and girls.
It is evident that literature on the adolescent SRHR in slums in SSA has been growing steadily over the last two decades. Dividing the period under consideration into five-year intervals, we noted that 9.3% were conducted between 2000 and 2004. About 44% of the studies on adolescent SRHR in the slums in SSA were done between 2010 and 2014. Majority (74%) of studies were conducted over the last decade (from 2010 to date).
Adolescent sexual behavior in slums
This review identified 24 studies (44%) that investigated sexual behavior among adolescent in the slums of SSA cities. The majority of these studies were quantitative, observational and from Nairobi City slums (Table 2). Most of these studies assessed “risky” sexual behavior, virtually to the exclusion of other sexual behavior among young people.
Table 2.
Studies on adolescent sexual behavior
| Study | Slum Name | City | Population | Age group | Study Type | Design | Sample size |
|---|---|---|---|---|---|---|---|
| Abebe, 2006 | Teklehamanot | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant. | 186 |
| Adebola A. and Odutolu 2007 | Not specified | Ibadan | Girls & Boys | 15–24 | Obs. | Quant. | 1042 |
| Amuyunzu-Nyamongo and Magadi 2006 | Korogocho & Viwandani | Nairobi | Girls & Boys | 13–50 | Obs. | Qual. | 40 |
| Austrian et al. 2015 | Kibera | Nairobi | Girls | 18–25 | Interv | Qual | 128 |
| Beguy, et al. 2013 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–22 | Obs. | Mixed | 4058 |
| Beguy et al. 2009 | Korogocho &Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant. | 2324 |
| Carolina for Kibera 2007 | Kibera | Nairobi | Girls | 11–18 | Interv | Quant | 222 |
| Dodoo, Zulu, and Ezeh 2007 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Mixed method | 15,315 |
| Erulkar and Ferede 2009 | Not Specified | AAa,BDb & Gondar | Girls | 10–19 | Obs. | Quant | 1839 |
| Erulkar et al. 2013 | Not Specified | Addis Ababa | Girls | 10–19 | Interv | Quant | 1172 |
| Erulkar et al. 2004 | Merkato & Kazanchis | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant. | 1076 |
| Kabiru et al. 2010 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant. | 2134 |
| Khoza et al. 2018 | Hillbrow, Berea, & Yeoville | Johannesburg | Girls & Boys | 16–18 | Interv | Qual. | 120 |
| Marston et al. 2013 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–19 | Obs. | Quant | 1754 |
| Mphatso Kamndaya et al. 2015 | Mbayani and Mtopwa | Blantyre, Malawi | Girls & Boys | 10–24 | Obs. | Qual | 60 |
| Motsomi et al. 2016 | Zandspruit | Johannesburg | Girls & Boys | 15–19 | Obs. | Qual | 40 |
| Mugisha and Zulu 2004 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–24 | Obs. | Mixed method | Not Stated |
| Ndugwa et al. 2011 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant | 1722 |
| Ngom, Magadi, and Owuor 2003 | Korogocho & Viwandani | Nairobi | Girls | 10–19 | Obs. | Quant | 788 |
| Okigbo et al. 2015 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant. | 1927 |
| Renzaho et al. 2017 | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
| Sidze et al. 2015 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–24 | Obs. | Quant | 689 |
| Ziraba et al. 2018 | Korogocho & Viwandani | Nairobi | Girls | 12–23 | Obs. | Quant. | 1390 |
| Zulu, Dodoo, & Ezeh 2002 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Quant. | 1645 |
Where: Obs. ➔Observational research; Interv➔ Intervention research, Qual➔ Qualitative; Quant➔ Quantitative, AAa-Addis Ababa BD b– Bahir Dar
The sexual risk behaviors examined include early age sexual debut [11, 15, 21] unprotected sexual intercourse [15, 22, 23], multiple sexual partnership [11, 15, 24], transactional sex [11, 15, 25] and age-disparate sex [25, 26].
Several studies examined factors that influence adolescent SRHR through the lens of an ecological framework outlining individual, familial/relational, societal and structural level factors. The slum environment in these studies was conceptualized as a mediating variable that intensifies the effect of these factors to cause adverse SRHR outcomes.
Study results showed that risky sexual behavior is strongly shaped by individual and socio-structural forces. The individual factors highlighted include: poor knowledge or access to protection (condoms) [23, 27]. The extent to which adolescents are knowledgeable about protection and have access to them was noted to be a factor determining their use of condoms to prevent against pregnancy, HIV/AIDS and other STIs. Other individual level factors notably associated with risky sexual behavior among adolescents were alcohol, drug and substance use [28–30].
Several studies also reported that young people living in urban slums engage in sexual intercourse much earlier and/or transactional and age disparate sex [11, 14, 15, 28, 31]. Adolescents living in slums were found to be more likely to have multiple sexual partners and to report that their most recent sexual intercourse was unprotected than their peers living in wealthier households.
Parental factors such as co-residence and parental control were also highlighted by some studies [15, 25, 32–34]. These studies show that adolescents living in informal settlements are more likely to be staying on their own or with friends and thus lack formal parental control, which may expose them to riskier behaviors.
Other social factors identified include peer and partner influences that operate in a gendered context and affect adolescent boys and girls differently [15, 23, 25, 28]. Studies suggest that adolescents’ relationship dynamics are characterized by unequal decision-making between male and female partners with females having less control over their sexual lives. There is also poor communication about sexual matters by male and female adolescent sexual partners and hence a lack of preparation for or anticipation of intercourse [35].
Adolescent pregnancy
The review identified 16 studies that investigated adolescent pregnancy. Majority (69%) of these studies were carried out in Nairobi. Two studies were conducted in Addis Ababa and one each in Kampala, Blantyre, and Johannesburg. The majority of these studies were observational and quantitative in type and design respectively. Only three studies were interventions or implementation research, and five were qualitative or mixed methods in nature.
Most of these studies examined the correlates of adolescent pregnancy in the slums (Table 3). Several studies looked at individual behavior correlates. These were: Low levels of knowledge on the menstruation cycle [15, 24, 32, 36]; low levels of knowledge on contraception or non-use of contraception [37, 38]; early sexual debut; multiple or frequent sexual partnership [11, 24, 36]; transactional and age-disparate sex [30, 32] and alcohol and drug use [28, 37, 39].
Table 3.
Studies on adolescent pregnancy
| Study | Slum Name | City | Population | Age group | Study Type | Design | Sample size |
|---|---|---|---|---|---|---|---|
| Abebe, 2006 | Teklehimanot | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant | 186 |
| Austrian et al., 2015 | Kibera | Nairobi | Girls | 18–25 | Interv | Qual | 128 |
| Austrian et al. 2015 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Austrian et al. .2018 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Beguy, Ndugwa, and Kabiru 2013 | Korogocho & Viwandani | Nairobi | Girls | 15–19 | Obs. | Quant | 897 |
| Beguy, et al. 2013 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–22 | Obs. | Mixed method | 4058 |
| Beguy et al. 2014 | Korogocho & Viwandani | Nairobi, Kenya | Girls | 10–24 | Obs. | Quant | 846 |
| Brahmbhatt et al. 2014 | Not specified | Johannesburg, Ibadan | Girls & Boys | 15–19 | Obs. | Quant | 1112 |
| Erulkar et al. 2004 | Merkato & Kazanchis | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant | 1076 |
| Jayaweera et al. 2018 | Not Specified | Nairobi | Girls | 15–35 | Obs. | Qual | 71 |
| Kabiru et al. 2010 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant | 2134 |
| Mphatso et al. 2015 | Mbayani and Mtopwa | Blantyre | Girls & Boys | 10–24 | Obs. | Qual | 60 |
| Mumah et al. 2014 | Korogocho & Viwandani | Nairobi | Girls | 15–19 | Obs. | Qual | 31 |
| Ngom, Magadi, and Owuor 2003 | Korogocho & Viwandani | Nairobi | Girls | 10–19 | Obs. | Quant | 788 |
| Renzaho et al. 2017 | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
| Zulu, Dodoo, and Ezeh 2002 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Quant | 1645 |
Where: Obs.➔ Observational research; Interv➔ Intervention research, Qual➔ Qualitative; Quant➔ Quantitative
Other studies looked at socio-ecological factors associated with pregnancy. These were poverty [11, 15, 28, 37]; peer pressure [15, 36, 37]; lack of parental control [15, 33, 39, 40] and the physical environment [11, 13, 39].
HIV/AIDS and other STIs
The review identified 23 studies that investigated HIV/AIDS in the slums of SSA cities. Some of these studies examined the prevalence and/or incidence of HIV/AIDS in the slums in comparison with other settlements. From these studies (Table 4), the prevalence of HIV was significantly higher in slums than other urban areas and other settlements. For example, in Nairobi the HIV prevalence among young people aged 15–19 years in informal urban settlements (15.2%) was relatively higher than in formal settlements (11.4%) [13]. Similarly, across 20 countries in SSA, it was reported that the urban poor have on average 19% higher odds of being HIV positive than their non-poor urban counterparts of similar background characteristics (age, gender, educational attainment, gender of household head and religion [41].
Table 4.
Studies on HIV/AIDS
| Study | Name of Slum | City | Population | Age group | Study Type | Design | Sample size |
|---|---|---|---|---|---|---|---|
| Abebe, 2006 | Teklehimanot | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant | 186 |
| Adebola et al., 2007 | NS | Ibadan | Girls & Boys | 15–24 | Obs. | Quant | 1042 |
| Adedimeji et al. 2008 | Ita-Ege, Esu-Awele, Isale-Ijebu | Ibadan | Girls & Boys | 15–24 | Obs. | Quant | 886 |
| Austrian, et al., 2015 | Kibera | Nairobi | Girls | 18–25 | Interv | Qual | 128 |
| Beguy, et al. 2013 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–22 | Obs. | Mixed | 4058 |
| Dodoo et.al, 2007 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Mixed Method | 15,315 |
| Dunbar et al. 2010 | NS | Harare | Girls | 15–19 | Interv | Quant | 315 |
| Erulkar et al. 2004 | Merkato & Kazanchis | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant | 1076 |
| Erulkar et al. 2013 | NS | Addis Ababa | Girls | 10–19 | Interv | Quant | 1172 |
| Gibbs et al. 2017 | eThekwini | Durban | Girls & Boys | 18–30 | Interv | Mixed method | 232 |
| Greif et al., 2010 | NS | Dara, Kama, Accra, Harare | Girls | 15–49 | Obs. | Quant | Not stated |
| Hall et al., 2006 | Kibera | Nairobi | Girls | 16–22 | Interv | Quant | 255 |
| Henwood et al. 2016 | Khayelitsha | Cape Town | Girls & Boys | 12–25 | Interv | Mixed method | 60 |
| Kamndaya et al. 2014 | NS | South Africa | Girls & Boys | 10–24 | Obs. | Quant | 530 |
| Kabiru et al. 2010 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–19 | Obs. | Quant | 2134 |
| Kabiru et al. 2011 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–22 | Obs. | Quant | 4028 |
| Khoza et al. 2018 | NS | Johannesburg | Girls & Boys | 16–18 | Interv | Qual | 120 |
| Madise et al. 2012 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Quant | 5048 |
| Mphatso Kamndaya et al. 2015 | Mbayani and Mtopwa | Blantyre, Malawi | Girls & Boys | 10–24 | Obs. | Qual | 60 |
| Mugisha and Zulu 2004 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–24 | Obs. | Mixed method | Not stated |
| Renzaho et al. 2017a | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
| Ziraba et al. 2018 | Korogocho & Viwandani | Nairobi | Girls | 12–23 | Obs. | Quant | 1390 |
| Zulu, Dodoo, and Ezeh 2002 | Korogocho & Viwandani | Nairobi | Girls & Boys | 15–49 | Obs. | Mixed method | 1645 |
aAddressed HIV/AIDS and other STI;
Where: Obs.➔ Observational research; Interv➔ Intervention research, Qual➔ Qualitative; Quant➔ Quantitative; Dar ➔ Dares Salaam; Kam➔ Kampala; Har ➔ Harare; NS – not specified
HIV/AIDS is often transmitted through heterosexual intercourse and most studies in the slum settlements examined sexual behavior patterns that predispose adolescents to HIV infection [11, 13–15, 26, 36, 42]. It is important to note that due to the criminalization of same sex relations in SSA, an accurate estimate of the modes of HIV transmission is difficult. Several studies examined how poverty and related economic hardships contribute to risky sexual practices and may increase risk of infection [11, 14, 15, 28, 31, 43].
Contraception and abortion
About a fifth of the studies examined contraceptive use: three of which investigated patterns of a full range of contraceptives [22, 42, 44], while six studies examined condoms use patterns for dual protection against pregnancies and HIV/AIDS [23, 28, 45–47]. These studies show that adolescents face many barriers in the use of contraceptive methods including lack of access, fear/embarrassment, cost and lack of knowledge. Consequently, the use of contraception among adolescents remains low leading to high levels of unintended pregnancies, unplanned births and unsafe abortion (Table 5).
Table 5.
Studies on Contraception and Abortion
| Study | Slum Name | City | Population | Age group | Study Type | Design | Sample size |
|---|---|---|---|---|---|---|---|
| Contraception/Family planning | |||||||
| Abebe 2006 | Teklehaimanot | Addis Ababa | Girls & Boys | 10–19 | Obs. | Quant | 186 |
| Adebola et.al 2007 | Not specified | Ibadan | Girls & Boys | 15–24 | Obs. | Quant | 1042 |
| Adedimeji et al. 2008 | Ita-Ege, Esu-Awele, Isale-Ijebu | Ibadan | Girls & Boys | 15–24 | Obs. | Quant | 886 |
| Austrian et al. 2015 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Austrian et al. 2018 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Beguy, et al. 2013 | Korogocho & Viwandani | Nairobi | Girls & Boys | 12–22 | Obs. | Mixed method | 4058 |
| Ochako et al. 2016 | Korogocho & Viwandani | Nairobi | Girls | 15–49 | Obs. | Quant | 1873 |
| Renzaho et al. 2017 | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
| Sidze et al. 2015 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–24 | Obs. | Quant | 689 |
| Ziraba et al. 2018 | Korogocho & Viwandani | Nairobi | Girls | 12–23 | Obs. | Quant | 1390 |
| Abortion | |||||||
| Jayaweera et al. 2018 | Not Specified | Nairobi | Girls | 15–35 | Obs. | Qual | 71 |
| Kenya Human Rights Commission 2010 | Korogocho | Nairobi | Girls | 15–27 | Obs. | Mixed method | 65 |
| Renzaho et al. 2017 | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
Where: Obs.➔ Observational research; Interv➔ Intervention research, Qual➔ Qualitative; Quant➔ Quantitative
Only three studies focused on abortion among adolescent girls [38, 42, 48]. These studies underscore unsafe abortion resulting from unintended pregnancies among adolescent girls as a maternal health issue of great concern in most SSA settings where abortion laws are restrictive and safe abortion is largely inaccessible. Therefore, many adolescents in need of pregnancy termination resort to unsafe abortion, which is associated with significant mortality and morbidity risks.
Gender-based violence
This review identified nine (17%) studies that investigated GBV among adolescent (Table 6), most of which examined intimate partner physical and sexual violence [27, 29, 42, 49–51]. Very few studies focused on child marriage and female genital mutilation [52].
Table 6.
Studies on Gender-Based Violence
| Study | Slum name | City | Population | Age group | Study Type | Design | Sample size |
|---|---|---|---|---|---|---|---|
| General Gender-Based Violence | |||||||
| Abuya et al. 2012 | Not Specified | Nairobi | Girls | 15–19 | Obs. | Qual | 10 |
| Austrian et al. 2015 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Austrian et al. 2018 | Kibera | Nairobi | Girls | 11–14 | Interv | Quant | 6000 |
| Erulkar et al. 2013 | Not Specified | Addis Ababa | Girls | 10–19 | Interv | Quant | 1172 |
| Gibbs et al. 2017 | eThekwini | Durban | Girls & Boys | 18–30 | Interv | Mixed method | 232 |
| Mugisha and Zulu 2004 | Korogocho & Viwandani | Nairobi | Girls & Boys | 10–24 | Obs. | Mixed method | Not stated |
| Renzaho et al. 2017 | Makindye and Nakawa | Kampala | Girls & Boys | 10–24 | Obs. | Quant | 663 |
| Swart E. 2012 | Kibera | Nairobi | Girls | 18–30 | Obs. | Quant | 200 |
| Female Genital Mutilation | |||||||
| Mudege et al. 2012 | Korogocho&Viwandani | Nairobi | Girls | 12–24 | Obs. | Quant | 527 |
Where: Obs.➔ Observational research; Interv➔ Intervention research, Qual➔ Qualitative; Quant➔ Quantitative
The studies that examined the prevalence, causes and consequences of GBV suggest that it is common among adolescents in slum settlements with adolescent girls more likely to be affected than boys [29, 50–52]. Accordingly, the main driver of GBV may be traditional norms and cultural beliefs that men are more powerful than women and therefore should dominate or control women and their sexuality including sexual intercourse [50–52]. Other correlates include alcohol and drug use [29] and commercial and/or transactional sex [50]. The consequences of GBV highlighted include injury, pain, psychological distress and other mental health illnesses, STIs, including HIV/AIDS, and unintended pregnancy [47, 50, 51].
Programs and interventions
The review identified nine interventions targeting adolescent SRHR outcomes in slums in SSA. The interventions encompassed a variety of designs including pre-post quasi- experimental designs, interventions with matched comparison groups, community interventions without comparison or control groups and randomized controlled trials (Table 7). Most of these interventions were conducted in slum areas in East Africa with limited work in Southern Africa and West Africa. Since they targeted adolescents in slum settlement most addressed the socio-economic correlates of poor adolescent SRHR outcomes by building adolescents’ economic and social assets [27, 31, 47, 53–55]. The interventions for economic empowerment of girls included provision of microfinance, financial literacy, cash transfers, and savings programs aimed at reducing adolescents’ vulnerability to adverse SRHR outcomes. Some interventions also included the creation of safe spaces where girls could meet and receive training on various issues.
Table 7.
Programs and interventions targeting adolescent SRHR
| Name of the Intervention | City | Target | Study Design | Brief Description |
|---|---|---|---|---|
| Adolescent Girls Initiative-Kenya (AGI-K) (Austrian et al. 2015; Austrian et al.; 2018) | Nairobi | 11–14 years girls | Randomized trial | Building adolescent girls assets (education, health, and wealth creation); cash transfer, savings, financial education, SRHR education and violence prevention |
| Binti Pamoja Centre (Daughters United Centre) (Carolina for Kibera 2007) | Nairobi | 11–18 year girls | Community Intervention | Gender empowerment and creation of safe spaces for young people in order to 1) reduce violence, female genital mutilation, sexual abuse, rape, prostitution, and poverty; and 2) increase reproductive health knowledge, financial education, leadership and personal skills |
| BiruhTefta-Bright Future (Erulkar et al. 2013) | Addis Ababa | 10–19 years girls | Quasi-experimental | Addresses social isolation by building social capital, literacy, providing information on HIV, reproductive health and GBV |
| CHANGE (Khoza et al. 2018) | Johannesburg | 16–18 girls and boys | Randomized controlled trial | Examines the effects of unconditional versus conditional cash transfers on clinic and school attendance for HIV prevention |
| TRY-Tap and Reposition Youth (Hall, Dondo, and Sebstad 2006) | Nairobi | 16–22 years young women | Intervention study with matched comparison | Improve livelihoods through microfinance, life skills, financial literacy in order to reduce vulnerability to adverse SRHR outcomes |
| Stepping Stones (Gibbs et al. 2017) | Durban | 18-30 years (youth) | Cluster Randomized Control Trial | Comprehensive sexuality and behavior change communication (sexual health knowledge, communication skills, critical reflection and reduce sexual health risk) |
| Tupange (URHI-Urban Reproductive Health Initiative (Speizer et al. 2013) | Nairobi | 10-24 years (young people) | Community Intervention study | Building capacity of service providers, contraceptive commodity security, demand-promotion and advocacy (dispel myth and misconception about contraceptives) |
| Virtual support group (Khaya HIV Positive) (Henwood et al. 2016) | Cape Town | 12-25 years (young people) | Mhealth (social media) intervention study | Virtual support group. The chat-room used the MXit social networking platform to provide information on a youth-friendly HIV services (testing, treatment and care) and contraception |
Some interventions focused on comprehensive sexuality education and behavior change communication strategies. These included information provision through mass media, social media, virtual space, social mobilization, advocacy, and through participatory activities [54, 56] . Others combined sexuality education with microcredit and community mobilization or gender empowerment training combined with life skills and financial literacy [27, 47]. The reported outcomes of these interventions included increased knowledge of HIV/AIDS and condom use [27, 57], reduction in the number of sexual partners [31, 55] reduced GBV [53, 55, 57] and transactional sexual relationships and improved gender attitudes [47, 57].
Discussion
This scoping review mapped existing evidence on adolescent SRHR in slums in SSA and identified 54 studies published between January 2000 and May 2019. The review showed that adolescents and young people growing up in slums face tremendous challenges in relation to their SRHR needs resulting in poor outcomes such as early pregnancy, STIs, and sexual violence. Of the 54 studies identified, majority were conducted in slum areas in Nairobi, Kenya with very few in other slums areas across SSA.
The scope of the studies is also limited. The literature was skewed towards sexual behavior and HIV/AIDS with very few studies examining other aspects of SRHR such as contraception, abortion, GBV and STIs. The surge in the interest on adolescent sexual behavior is mainly related to the HIV/AIDS prevention programs [58]. This partly explains the narrow focus of these studies on “risky” sexual behavior to the exclusion of other facets of sexuality such as sexual satisfaction, sexual pleasure, eroticism and sexual identity. There is need for studies to explore the whole purview of sexuality such as sexual pleasure and satisfaction, sexual identity, orientation, sexual practices in addition to risky sexual behavior. Unexpectedly, there is minimal research on the utilization of maternal health services by adolescents overall despite the high risk of adolescent mothers to maternal morbidity and mortality due to their unique biological, sociological and economic status [59].
Since most studies were observational, cross-sectional quantitative studies, causal inferences cannot be made. Further, the relative dearth of qualitative studies that interrogate and give deeper insights to the experiences and needs of individuals mean that most studies provide limited data and/or information. As sexuality and other SRHR outcomes are partly driven by cultural norms and beliefs, qualitative studies exploring the roles/influence of contextual characteristics are needed [32, 60]. There is also need for studies to go beyond the conventional cross-sectional designs with a view to exploring how sexual behavior, identity, orientation, sexual practices and other SRHR behavior evolve especially in adolescence and younger ages. Studies interrogating puberty, romantic relationships and the effect of gender norms on romantic relationships are also needed. Mixed method designs that incorporate qualitative techniques can be undertaken to provide deeper understanding about these aspects of adolescent SRHR.
Our review highlighted age-overlaps in many of the studies identified. Although adolescent is normally defined as the period between 10 and 19 years [61], many studies identified did not strictly adhere to this definition. Barely half of the studies focused exclusively on adolescents (10–19), while the remaining combined adolescents with other groups namely; young people (10–24 years); youths 15–24 and reproductive age women and men (15–49 years). There is need for more studies on SRHR that focus exclusively on adolescent girls and boys in slums in SSA. Even very critical is the limited number of studies on very young adolescents (10–14), a group with what is called a ‘window of opportunity’ to address SRHR problems [62] .Early adolescence is a critical time to lay the foundation for healthy and fulfilling sexual and reproductive lives of adolescents. There is need for studies that categorize the adolescent period into early (10–14) and late (15–19) to allow for the comparison of SRHR outcomes and drivers between early versus late adolescence.
The results suggest a general paucity of intervention research that is focused on adolescent SRHR in the slum areas in the SSA. Specifically, intervention studies that allow for the comparison of impacts between early versus late adolescence are lacking. Intervention studies that address differential vulnerability in early and late adolescence among adolescent girls and boys in urban slums also are needed. Understanding what works to improve SRHR in early adolescence will likely lead to healthy trajectories across their life course [46, 63]. Although the identified interventions aimed at addressing the economic and social drivers of adolescent risk to poor SRHR outcomes, not all socio-structural factors highlighted in the review such as parenting were addressed by interventions. There are no interventions that focused on parenting as a key mechanism of socialization of adolescents, yet this was one of the factors that affect their healthy transition into adulthood [33, 34]. There is therefore need for interventions with and explicit focus on improving parent-child relationships (communication and other dimensions of parenting) in the slums. Finally, comparative studies across sites and SRHR components are lacking. There is a dearth of multi-country or multi-site and multi-theme studies on adolescent SRHR in slums settlement in SSA that can provide generalizable evidence.
Understanding the unique challenges of urban poverty is critical in understanding the drivers of adolescent SRHR outcomes in the slum settings. Rapid urbanization is taking place in SSA in the context of poor economic performance, which presents challenges for adolescents in cities [8, 64]. There are wide disparities in health and socio-economic outcomes between the wealthy and poor urban adolescents: more adolescents in poor urban settings engage in riskier sexual behaviors, have higher HIV infection, experience higher mortality and are more likely to experience violence and drug abuse than their wealthier counterparts [16, 65, 66]. The review focused on several key SRHR issues (sexual behavior, adolescent pregnancy, HIV/AIDS, and GBV among others) but yet has not included studies around puberty, romantic relationships and the effect of gender norms on romantic relationships.
To our knowledge, this is the first scoping review examining adolescent SRHR in urban slums in SSA. Although we used rigorous and transparent methods to ensure a comprehensive search of the literature, it is possible that we did not retrieve all studies in peer-reviewed journals or grey literature. Further, our review only included articles published in English. Nonetheless, the review has yielded important findings on several key SRHR issues that affect adolescents living in resource-limited urban slums in SSA, a region with a high burden of poor SRHR outcomes including early and unintended pregnancy, HIV/AIDS, and GBV.
Conclusion
The results of this review point to several potential target areas for programming and research aimed at improving adolescents’ SRHR. To improve and promote adolescent SRHR, development and well-being, it is important to understand the broader socio-ecological context of slum residence as a risky environment with poor, unhealthy and unsafe living conditions, rather than focusing solely on individual SRHR-related behaviour. Understanding and addressing adolescents’ SRHR requires a comprehensive understanding of the contexts that increase their vulnerability to poor outcomes. Interventions that address this risky environment will help adolescents transition into adulthood as a healthy workforce that can help countries in SSA achieve a demographic dividend.
Acknowledgments
The authors gratefully acknowledge the support of Eliud Wekesa in appraising the papers, and Isabella Aboderin in the conceptualization of the project.
Abbreviations
- AIDS
Acquired immunodeficiency syndrome
- GBV
Gender-based violence
- HIV
Human immunodeficiency virus
- LMICs
Low- and Middle-Income Countries
- SRHR
Sexual and Reproductive Health and Rights
- SSA
Sub-Saharan Africa
- STI
Sexually transmitted infection
- UNFPA
United Nations Population Fund
- WHO
World Health Organization
Authors’ contributions
YD and MB conceptualized the study, supervised the review process, drafted the manuscript and participated in the interpretation of findings. CK participated in interpretation of findings and in drafting and revising the manuscript. GF contributed to study methodology, interpretation of findings and revising the manuscript. The authors participated in giving final approval of the version to be published.
Funding
The scoping review was supported by a grant to the African Population and Health Research Center (APHRC) from the David and Lucile Packard Foundation (grant #2016–6250). Writing time and article processing fees (partial) were supported by a grant from the African Regional Office of the Swedish International Development Cooperation Agency, Sida Contribution No. 12103 for APHRC’s challenging the Politics of Social Exclusion project.
Availability of data and materials
The list of publications used for the scoping review are available in the manuscript and can also be made available upon request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yohannes Dibaba Wado, Email: ywado@aphrc.org.
Martin Bangha, Email: mbangha@aphrc.org.
Caroline W. Kabiru, Email: ckabiru@aphrc.org
Garumma T. Feyissa, Email: garummatolu@yahoo.com
References
- 1.UN . World population prospects 2019:the 2019 Revisision. New York: UN Population Division, Department of Economic and Social Affairs; 2019. [Google Scholar]
- 2.Bearinger LH, Sieving R, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2007;369(9568):1220–1231. doi: 10.1016/S0140-6736(07)60367-5. [DOI] [PubMed] [Google Scholar]
- 3.WHO . WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. Geneva: World Health Organization; 2011. [PubMed] [Google Scholar]
- 4.UNFPA . Adolescent pregnancy: a review of the evidence. New York: United Nations Population Fund; 2013. [Google Scholar]
- 5.UNFPA . State of the world population 2013. New York: United Nations Popualtion Fund; 2013. Motherhood in childhood: facing the challenge of adolescent pregnancy. [Google Scholar]
- 6.Woog V, Kågesten A. The sexual and reproductive health needs of very young adolescents aged 10–14 in developing countries: what does the evidence show? New York: Guttmacher Institute; 2017. [Google Scholar]
- 7.UNFPA . Adolescent sexual and reproductive health. New York: United Nations Population Fund; 2014. [Google Scholar]
- 8.UN-HABITAT. World cities report 2016: urbanization and development - emerging futures. In: The state of world cities: UN habitat; 2016. https://unhabitat.org/world-cities-report.
- 9.Mberu B, Mumah J, Kabiru C, Brinton J. Bringing sexual and reproductive health in the urban contexts to the forefront of the development agenda: the case for prioritizing the urban poor. Matern Child Health J. 2014;18(7):1572–1577. doi: 10.1007/s10995-013-1414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO, UNHSP . Hidden cities: unmasking and overcoming health inequities in urban settings. Geneva: World Health Organization and United nations Human Settlement Program; 2010. [Google Scholar]
- 11.Zulu EM, Dodoo FN, Chika-Ezee A. Sexual risk-taking in the slums of Nairobi, Kenya, 1993-8. Popul Stud. 2002;56(3):311–323. doi: 10.1080/00324720215933. [DOI] [PubMed] [Google Scholar]
- 12.Sverdlik L. Ill-health and poverty: a literature review on health in informal settlements. Environ Urban. 2011;23(1):123–155. doi: 10.1177/0956247811398604. [DOI] [Google Scholar]
- 13.Madise NJ, Ziraba AK, Inungu J, Khamadi SA, Ezeh A, Zulu EM, et al. Are slum dwellers at heightened risk of HIV infection than other urban residents? Evidence from population-based HIV prevalence surveys in Kenya. Health & place. 2012;18(5):1144–1152. doi: 10.1016/j.healthplace.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dodoo FN, Zulu EM, Ezeh AC. Urban-rural differences in the socioeconomic deprivation--sexual behavior link in Kenya. Soc Sci Med. 2007;64(5):1019–1031. doi: 10.1016/j.socscimed.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabiru C, Beguy D, Undie CC, Zulu EM, Ezeh CA. Transition into first sex among adolescents in slum and non-slum communities in Nairobi, Kenya. J Youth Stud. 2010;13(4):453–471. doi: 10.1080/13676261003801754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anastasi E, Ekanem E, Hill O, Adebayo Oluwakemi A, Abayomi O, Bernasconi A. Unmasking inequalities: sub-national maternal and child mortality data from two urban slums in Lagos, Nigeria tells the story. PLoS One. 2017;12(5):e0177190. doi: 10.1371/journal.pone.0177190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arksey H, L OM. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 18.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evidence-Based Healthcare. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 21.Amuyunzu-Nyamongo MK, Magadi MA. Sexual privacy and early sexual debut in Nairobi informal settlements. Community Work Fam. 2006;9(2):143–158. doi: 10.1080/13668800600586936. [DOI] [Google Scholar]
- 22.Beguy D, Mumah J, Wawire S, Muindi K, Gottschalk L, Kabiru C. STEP UP technical working paper. Nairobi: African Population and Health Research Center; 2013. Status report on the sexual and reproductive health of adolescents living in urban slums in Kenya. [Google Scholar]
- 23.Adedimeji AA, Omololu FO, Odutolu O. HIV risk perception and constraints to protective behaviour among young slum dwellers in Ibadan, Nigeria. J Health Popul Nutr. 2007;25(2):146–157. [PMC free article] [PubMed] [Google Scholar]
- 24.Erulkar A, Tekle-Ab M, Negussie S, G. T. Adolescent life in low income and slum areas of Addis Ababa, Ethiopia. 2004. [Google Scholar]
- 25.Ziraba A, Orindi B, Muuo S, Floyd S, Birdthistle IS, J ea M. Understanding HIV risks among adolescent girls and young women in informal settlements of Nairobi, Kenya: lessons for DREAMS. PLoS One. 2018;13(5):e0197479. doi: 10.1371/journal.pone.0197479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Renzaho A, Kamara JK, Georgeou N, G K. Sexual, reproductive health needs, and rights of young people in slum areas of Kampala, Uganda: a cross sectional study. PLoS One. 2017;12(1):e0169721. doi: 10.1371/journal.pone.0169721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erulkar A, Ferede A, Girma W, Ambelu W. Evaluation of ‘Biruh Tesfa’ (bright future) program for vulnerable girls in Ethiopia, 8 (2): 182–92. Vulnerable Children and Youth Studies. 2013;8(2):182–192. doi: 10.1080/17450128.2012.736645. [DOI] [Google Scholar]
- 28.Goshu A. A study on contributing factors to adolescents, reproductive behavior in slum areas of Addis Ababa: the case of Teklehaimanot area. Addis Ababa: Addis Ababa University; 2006. [Google Scholar]
- 29.Mugisha F, EM Z. The influence of alcohol, drugs and substance abuse on sexual relationships and perception of risk to HIV infection among adolescents in the informal settlements of Nairobi. J Youth Stud. 2004;7(3):279–293. doi: 10.1080/1367626042000268926. [DOI] [Google Scholar]
- 30.Ndugwa R, Kabiru C, Cleland J, Beguy D, Egondi T, et al. Adolescent problem behavior in Nairobi’s informal settlements: applying problem behavior theory in sub-Saharan Africa. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2011;77(2):S298–S317. doi: 10.1007/s11524-010-9462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khoza N, Stadler J, MacPhail C, Chikandiwa A, Brahmbhatt H, Delany-Moretlwe S. Cash transfer interventions for sexual health: meanings and experiences of adolescent males and females in inner-city Johannesburg. BMC Public Health. 2018;18(1):120. doi: 10.1186/s12889-018-5027-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marston M, Beguy B, Kabiru C, Cleland J. Predictors of sexual debut among young adolescents in Nairobi’s informal settlements. Int Perspect Sex Reprod Health. 2013;39(1):22–31. doi: 10.1363/3902213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ngom P, Magadi MA, Owuor T. Parental presence and adolescent reproductive health among the Nairobi urban poor. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2003;33(5):369–377. doi: 10.1016/S1054-139X(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 34.Okigbo CC, Kabiru CW, Mumah JN, Mojola SA, Beguy D. Influence of parental factors on adolescents' transition to first sexual intercourse in Nairobi, Kenya: a longitudinal study. Reprod Health. 2015;12:73. doi: 10.1186/s12978-015-0069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Varga CA. How gender roles influence sexual and reproductive health among south African adolescents. Stud Fam Plan. 2004;34(3):160–172. doi: 10.1111/j.1728-4465.2003.00160.x. [DOI] [PubMed] [Google Scholar]
- 36.Beguy D, Ndugwa R, C. K. Entry into motherhood among adolescent girls in two informal settlements in Nairobi, Kenya. J Biosoc Sci. 2013;45(6):721–742. doi: 10.1017/S0021932013000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mumah J, Kabiru C, Cea M. African population and Health Research Center. 2014. Unintended pregnancies in Kenya: a country profile. [Google Scholar]
- 38.Jayaweera R, Ngui FM, Hall KS, C. G. Women’s experiences with unplanned pregnancy and abortion in Kenya: a qualitative study. PLoS One. 13(1):e0191412. [DOI] [PMC free article] [PubMed]
- 39.Brahmbhatt H, Kagesten A, Emerson M, Decker MR, Olumide AO, Ojengbede O, et al. Prevalence and determinants of adolescent pregnancy in urban disadvantaged settings across five cities. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2014;55(6 Suppl):S48–S57. doi: 10.1016/j.jadohealth.2014.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beguy D, Mumah J, L. G. Unintended pregnancies among young women living in urban slums: evidence from a prospective study in Nairobi City, Kenya. PLoS One. 2014;9(7):e101034. doi: 10.1371/journal.pone.0101034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magadi M. The disproportionate high risk of HIV infection among the urban poor in sub-Saharan Africa. AIDS Behav. 2013;17(5):1645–1654. doi: 10.1007/s10461-012-0217-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Renzaho AM, Kamara JK, Georgeou N, Kamanga G. Sexual, reproductive health needs, and rights of young people in slum areas of Kampala, Uganda: a cross sectional study. PLoS One. 2017;12(1):e0169721. doi: 10.1371/journal.pone.0169721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kamndaya M, Vearey J, Thomas L, Kabiru CW, Kazembe LN. The role of material deprivation and consumerism in the decisions to engage in transactional sex among young people in the urban slums of Blantyre, Malawi. Global public health. 2016;11(3):295–308. doi: 10.1080/17441692.2015.1014393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ochako R, Mbondo M, Aloo S, Kaimenyi S, Thompson R, Temmerman M, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC Public Health. 2015;15(1):118. doi: 10.1186/s12889-015-1483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sidze E, Elungata’a P, Maina B, Mutua M. Does the quality of parent–child connectedness matter for adolescents’ sexual behaviors in Nairobi informal settlements? Arch Sex Behav. 2015;44(3):631–638. doi: 10.1007/s10508-014-0402-3. [DOI] [PubMed] [Google Scholar]
- 46.Austrian K, Althea D. Barriers and facilitators to health behaviour change and economic activity among slum-dwelling adolescent girls and young women in Nairobi, Kenya: the role of social, health and economic assets. Sex Education. 2015;15(1):64–77. doi: 10.1080/14681811.2014.947364. [DOI] [Google Scholar]
- 47.Austrian K, Soler-Hampejsek E, Mumah J, Kangwana B, Wado YD, Abuya B, et al. Adolescent girls initiative-Kenya: midline results report. Nairobi: Population Council; 2018. [Google Scholar]
- 48.KHRC . Teenage pregnancy and unsafe abortion: the case of Korogocho slums. Nairobi: The Kenya Human Rights Commission (KHRC); 2010. [Google Scholar]
- 49.Gibbs A, Washington L, Willan S, Ntini N, Khumalo T, Mbatha N, et al. The stepping stones and creating futures intervention to prevent intimate partner violence and HIV-risk behaviours in Durban, South Africa: study protocol for a cluster randomized control trial, and baseline characteristics. BMC Public Health. 2017;17(1):336. doi: 10.1186/s12889-017-4223-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abuya B, Onsomu E, Moore D, J. S. A phenomenological study of sexual harassment and violence among girls attending high schools in urban slums, Nairobi, Kenya. J Sch Violence. 2012;11(4):323–344. doi: 10.1080/15388220.2012.706874. [DOI] [Google Scholar]
- 51.Swart E. Gender-based violence in a Kenyan slum: creating local, woman-centered interventions. J Soc Serv Res. 2012;38(4):427–438. doi: 10.1080/01488376.2012.676022. [DOI] [Google Scholar]
- 52.Mudege N, Egondi T, Beguy D, EM Z. The determinants of female circumcision among adolescents from communities that practice female circumcision in two Nairobi informal settlements. Health Sociol Rev. 2012;21(2):242–250. doi: 10.5172/hesr.2012.21.2.242. [DOI] [Google Scholar]
- 53.Kibera Cf: uuangane Tuangaze (Let’s Unite and Shed Light) 2006 annual report in: Annual report. Chapel Hill: Carolina for Kibera; 2007. [Google Scholar]
- 54.Dunbar MS, Maternowska MC, Kang MS, Laver SM, Mudekunye-Mahaka I, Padian NS. Findings from SHAZ!: a feasibility study of a microcredit and life-skills HIV prevention intervention to reduce risk among adolescent female orphans in Zimbabwe. Journal of prevention & intervention in the community. 2010;38(2):147–161. doi: 10.1080/10852351003640849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hall J, Dondo A, Sebstad J. Tap and reposition youth (TRY) program: providing social support, savings and microcredit opportunities to adolescent girls at risk for HIV/AIDS in Kenya. New York: Population Council; 2006. [Google Scholar]
- 56.Henwood R, Gabriela P, Barnett W, Hwang B, Metcalf C, Hacking D, et al. Acceptability and use of a virtual support group for HIV-positive youth in Khayelitsha, Cape Town using the MXit social networking platform. AIDS Care. 2016;28(7):898–903. doi: 10.1080/09540121.2016.1173638. [DOI] [PubMed] [Google Scholar]
- 57.Jewkes R, Gibbs A, Jama-Shai N, Willan S, Misselhorn A, Mushinga M, et al. Stepping stones and creating futures intervention: shortened interrupted time series evaluation of a behavioural and structural health promotion and violence prevention intervention for young people in informal settlements in Durban, South Africa. BMC Public Health. 2014;14:1325. doi: 10.1186/1471-2458-14-1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pettifor A, Bekker LG, Hosek S, DiClemente R, Rosenberg M, et al. Preventing HIV among young people: research priorities for thefuture. J Acquir Immune Defic Syndr. 2013;63(2):S155–S160. doi: 10.1097/QAI.0b013e31829871fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Banke-Thomas OE, Banke-Thomas AO, Ameh CA. Factors influencing utilisation of maternal health services by adolescent mothers in low-and middle-income countries: a systematic review. BMC pregnancy and childbirth. 2017;17(1):65. doi: 10.1186/s12884-017-1246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Motsomi K, Makanjee C, Basera T, P. N. Factors affecting effective communication about sexual and reproductive health issues between parents and adolescents in Zandspruit informal settlement, Johannesburg, South Africa. The Pan African Medical Journal. 2016;25(October):120. doi: 10.11604/pamj.2016.25.120.9208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.WHO . Health for the world's adolescents. Geneva: World Health Organization; 2014. [Google Scholar]
- 62.Woog V, K. A. The sexual and reproductive health needs of very young adolescents aged 10–14 in developing countries: what does the evidence show? New York: Guttmacher Institute; 2017. [Google Scholar]
- 63.Hindin MJ, Kalamar M, Thompson T, UD U. Interventions to prevent unintended and repeat pregnancy among young people in low- and middle-income countries: a systematic review of the published and gray literature. J Adolesc Health. 2016;59(3):s8–15. doi: 10.1016/j.jadohealth.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 64.Montgomery MR, Hewett PC. Urban poverty and health in developing countries: household and neighborhood effects. Demography. 2005;42(3):397–425. doi: 10.1353/dem.2005.0020. [DOI] [PubMed] [Google Scholar]
- 65.Speizer IS, Fotso CJ, Davis J, Saad A, Otai J. Timing and circumstances of first sex among female and male youth from select urban areas of Nigeria, Kenya, and Senegal. J Adolesc Health. 2013;53(5):609–616. doi: 10.1016/j.jadohealth.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thomas L, Vearey J, Mahlangu P. Making a difference to health in slums: an HIV and African perspective. Lancet. 2011;377(9777):1571–1572. doi: 10.1016/S0140-6736(11)60642-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The list of publications used for the scoping review are available in the manuscript and can also be made available upon request.