Abstract
Introduction
Infected pancreatic necrosis (IPN) and its related septic complications are the major causes of death in patients with acute necrotising pancreatitis (ANP). Therefore, the prevention of IPN is of great clinical value, and immunomodulatory therapy with thymosin alpha 1 may be beneficial. This study was designed to test the hypothesis that the administration of thymosin alpha 1 during the acute phase of ANP will result in a reduced incidence of IPN.
Methods and analysis
This is a randomised, multicentre, double-blind, placebo-controlled study. 520 eligible patients with ANP will be randomised in a 1:1 ratio to receive either the thymosin alpha 1 or the placebo using the same mode of administration. The primary endpoint is the incidence of IPN during the index admission. Most of the secondary endpoints will be registered within the index admission including in-hospital mortality, the incidence of new-onset organ failure and new-onset persistent organ failure (respiration, cardiovascular and renal), receipt of new organ support therapy, requirement for drainage or necrosectomy, bleeding requiring intervention, human leucocyte antigens-DR(HLA-DR) on day 0, day 7, day 14, and so on and adverse events. Considering the possibility of readmission, an additional follow-up will be arranged 90 days after enrolment, and IPN and death at day 90 will also be served as secondary outcomes.
Ethics and dissemination
This study was approved by the ethics committee of Jinling Hospital, Nanjing University (Number 2015NZKY-004-02). The thymosin alpha 1 in the prevention of infected pancreatic necrosis following acute necrotising pancreatitis(TRACE) trial was designed to test the effect of a new therapy focusing on the immune system in preventing secondary infection following ANP. The results of this trial will be disseminated in peer-reviewed journals and at scientific conferences.
Trial registration number
ClinicalTrials.gov Registry (NCT02473406).
Keywords: pancreatic disease, immunology, infectious diseases
Strengths and limitations of this study.
This is a randomised, multicentre, double-blind, placebo-controlled trial providing top-class evidence concerning the efficacy and safety of thymosin alpha 1 for patients with acute necrotising pancreatitis.
The data will be handled by an independent data safety monitoring board to ensure the safety of the participants.
Thymosin alpha 1 is a well-studied drug with a favourable safety profile in previous trials.
A sample size of 520 is required to detect the efficacy of thymosin alpha 1 in preventing infected pancreatic necrosis, which will take years before the conclusion could be drawn.
Continuous immune function assessment is not applied in this study.
Background
Infected pancreatic necrosis (IPN) and its related septic complications contribute substantially to deaths in patients with acute necrotising pancreatitis(ANP).1 Compared with patients with sterile necrosis, those with IPN suffered a significant increase in mortality ranging from 14% to 69%, despite advances in critical care, surgical and endoscopic interventions and antibiotics.2 Therefore, the prevention of IPN is of great clinical value in the treatment of ANP. Over the past years, numerous attempts had been made to prevent or delay the development of IPN, including antibiotic prophylaxis, early enteral nutritional, selective gut decontamination and probiotics. Still, none of them had been proved to improve patient-centred outcomes with high-quality evidence.3–6 More promising treatment aiming at reducing infectious complications of ANP is in need.
Immunosuppression and disorders characterised by decreased human leucocyte antigens-DR(HLA-DR) expression and unbalanced CD3/CD4+/CD8+T cells of peripheral blood mononuclear cell are reported to be associated with IPN,7 8 especially in those with a more severe type of disease, whose suppressed immune function occurs early and strongly.8 9 Our previous observational study found that early enteral nutrition could moderate the excessive immune response during the acute phase of severe acute pancreatitis (AP) without leading to subsequent immunosuppression and ultimately reduce the incidence of infection and intensive care unit (ICU) stay.10 Thus, immunomodulatory treatment could potentially intervene in the development of IPN, resulting in better outcomes. Efforts had been made in this field using drugs like lexipafant and octreotide. Still, the hitherto existing evidence failed to show robust clinical benefits of immunomodulation with regards to key clinical outcomes.11
Thymosin alpha 1 had been shown to have immunomodulatory properties and was reported to be clinically beneficial in patients with sepsis,12 13 majorly through the involvement of distinct toll-like receptors acting on different dendritic cell subsets and involving the MyD88-dependent signalling pathway. However, for AP, the only randomised controlled study was the pilot one conducted by our group years ago, suggesting that the use of thymosin alpha 1 was associated with improved cellular immunity and reduced infection rate in a group of 24 patients.14 Due to the single-centre set and small sample size, the clinical implication and generalisability of this study are thought to be limited. Therefore, we designed this multicentre trial, the thymosin alpha 1 in the prevention of IPN following ACN (Thymosin alpha 1 in the prevention of infected pancreatic necrosis following acute necrotising pancreatitis(TRACE)), with sufficient power to test the hypothesis that the administration of thymosin alpha 1 during the acute phase of ANP will result in a reduced incidence of IPN.
Study objectives
The primary objective of the TRACE trial is to determine whether thymosin alpha 1 is superior to placebo in reducing the incidence of IPN in patients with ANP. Secondary objectives are to determine the safety and the impact on the immune function of thymosin alpha 1 among patients with ANP.
Study design
The present study is an investigator-initiated, multicentre, individually randomised, double-blind, placebo-controlled, parallel-group study. This trial was registered on 16 June 2015 and was approved by the ethics committee of Jinling Hospital, Nanjing University. Local ethics approval was also obtained before enrolment in each participating centre. The TRACE trial was designed and coordinated by the Center of Severe Acute Pancreatitis at Nanjing University and the coordinating and data management centre of the Chinese Acute Pancreatitis Clinical Trials Group (CAPCTG). The trial steering committee was formed to oversee the implementation of the study, and a data safety monitoring board (DSMB) will regularly (every 6 months) review the safety report prepared by the trial statistician from the accumulating data of this trial.
Study population
This trial is performed in 16 hospitals from China. All adult patients with AP admitted to the participating centres will be assessed for eligibility after admission. The inclusion and exclusion criteria are as follows:
Inclusion criteria
Symptoms and signs of AP based on abdominal pain suggestive of AP, serum amylase at least three times the upper limit of normal and/or characteristic findings of AP on CT or less commonly MRI or transabdominal ultrasonography according to the Revised Atlanta Criteria.15
Less than 1 week from the onset of abdominal pain.
Age between 18 and 70 years.
Acute Physiology and Chronic Health Evaluation (APACHE II) score ≥8 during the last 24 hours before enrolment.
Balthazar CT score ≥5 (presence of pancreatic necrosis).16
Written informed consent obtained.
Exclusion criteria
Pregnant pancreatitis.
History of chronic pancreatitis.
Malignancy-related AP.
Receiving early intervention or surgery due to abdominal compartment syndrome or other reasons before admission.
Patients with a known history of severe cardiovascular, respiratory, renal or hepatic diseases defined as (1) greater than New York Heart Association Class II heart failure (Class II not included), (2) active myocardial ischaemia or (3) cardiovascular intervention within previous 60 days, (4) history of cirrhosis or (5) chronic kidney disease with creatinine clearance <40 mL/min or (6) chronic obstructive pulmonary disease with the requirement for home oxygen.
Patients with preexisting immune disorders such as AIDS.
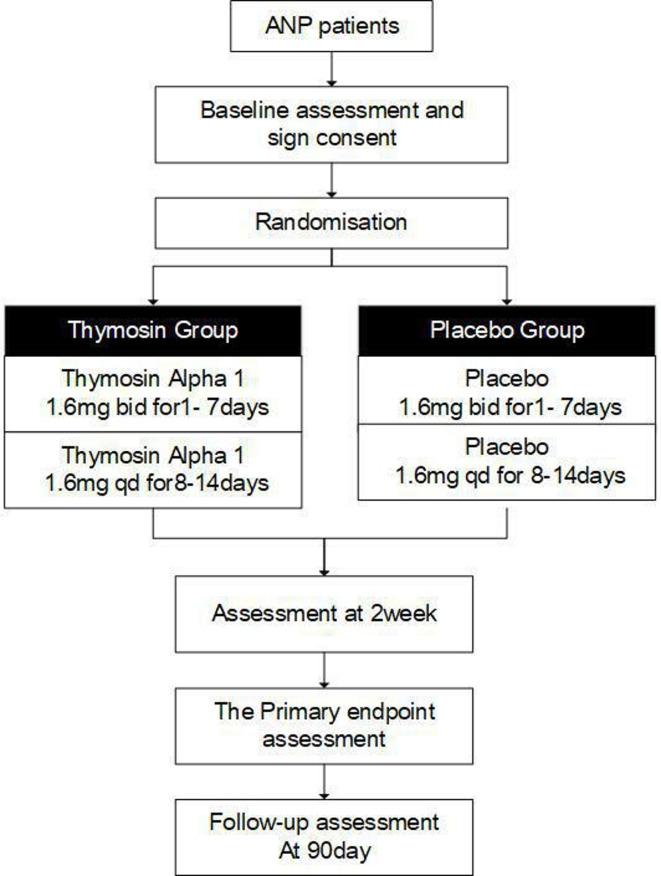
A patient will be considered eligible if he/she meets the inclusion criteria and does not meet any of the exclusion criteria. Allocation will be performed after signed consent is obtained. The study protocol flow of participants is outlined in figure 1.
Figure 1.
Trial flowchart. ANP, acute necrotising pancreatitis.
Randomisation and blinding methods
After the completion of screening measurements and the acquisition of written informed consent, eligible participants will be randomised in a 1:1 ratio to either the treatment group or the placebo group. The randomisation code was computer generated with a block size of 4, and the randomisation was stratified by sites.
Participants, clinical investigators and investigators assessing outcome data will be blinded to the treatment allocation to minimise potential sources of bias. The trial statistician will also be blinded regarding the treatment code when developing the statistical programmes, which will be validated and completed using dummy randomisation codes. The actual allocation will only be provided to the study team after locking of the database and approval of the statistical analysis plan.
Trial drugs
After randomisation, the participant will receive:
Thymosin alpha 1, 1.6 mg injectio hypodermic (I.H), every 12 hours for the first 7 days and 1.6 mg I.H, four times a day for the following 7 days. The administration will be terminated any day during the treatment when the patient is deemed as qualified for hospital discharge or dead.
Matching placebo (normal saline) using the same mode of administration as the above mentioned.
As shown in, the recruited patients will start to receive randomised drugs subcutaneously from the day after the allocation day. Thymosin alpha will be provided by SciClone Pharmaceuticals and the matching placebo by Chengdu Tongde Pharmaceuticals. All study drugs will be stored in a secure area with access limited to the investigators and authorised study site personnel, and under appropriate storage conditions.
General treatment regimen
All patients will receive standard treatment including fluid therapy, early enteral nutrition, routine medical treatment like proton pump inhibitor as indicated, mechanical ventilation if needed and continuous renal replacement therapy if needed in the light of recently published guidelines.17 All participating centres are able to offer appropriate intensive care in case the patients require organ support or continuous monitoring. The necrotic collection will be intervened when infection is suspected or confirmed, preferably after 4 weeks from the onset of the disease when the patient could tolerate the symptoms as suggested by the guidelines.17
When pancreatic infection occurs, either a surgical or endoscopic step-up approach considering the location of the necrotic collection and the technical availability in each participating centre will be applied. Principally, either percutaneous catheter drainage or endoscopic transluminal placement of double pig-tail stents, rather than debridement, are the primary choices of treatment.
Endpoints
Primary outcome measure
The incidence of IPN during the index admission will be served as the primary outcome measure of the TRACE trial. The diagnosis of IPN will be based on the international guidelines when one or more of the following were present: gas bubbles within (peri) pancreatic necrosis on CT; a positive culture of (peri) pancreatic necrosis obtained by image-guided fine-needle aspiration; a positive culture of (peri) pancreatic necrosis obtained during the first drainage and/or necrosectomy.15
Secondary outcome measures
Part I:secondary outcomes during the index admission
The occurrence of new-onset organ failure and new-onset persistent organ failure (Sequential Organ Failure Assessment (SOFA) score for respiration, cardiovascular or renal system ≥2). New-onset is defined as events that occur after randomisation and not present 24 hours before randomisation.
In-hospital mortality.
Bleeding requiring intervention.
Gastrointestinal perforation or fistula requiring intervention.
Incidence of pancreatic fistula.
New receipt of mechanical ventilation (not applied 24 hours before randomisation).
New receipt of renal replacement therapy (not applied 24 hours before randomisation).
New receipt of vasoactive agents (not applied 24 hours before randomisation).
The requirement for catheter drainage (either percutaneous or endoscopic).
Number of drainage procedures required.
The requirement for minimally invasive debridement.
Number of minimally invasive necrosectomy required.
The requirement for open surgery.
Number of open operations required.
Length of ICU stay.
Length of hospital stay.
SOFA score on day 0, day 7 and day 14.
C reactive protein level on day 0, day 7 and day 14.
HLA-DR level on day 0, day 7 and day 14.
Lymphocyte count on day 0, day 7 and day 14.
In-hospital cost.
Part II:secondary outcomes within 90 days after enrolment
Incidence of infection within 90 days after enrolment.
Mortality within 90 days after enrolment.
Sample size estimation
The incidence of IPN during the index admission was reported to be around 25% in ANP episodes combined with an APACHE II score ≥8 in our previous studies.18 19 To reduce the incidence of IPN from 25% to 15% on the basis of our pilot study,14 we projected a sample size of 500 participants with 80% power at a two-sided alpha level of 0.05 using the PASS software (PASS V.11, NCSS software, Kaysville, USA). In our study, we planned to randomise 520 patients after considering 4% of lost follow-up.
Statistical analysis
Primary analyses will be based on the intention-to-treat (ITT) population, and secondary supportive analyses will be done on the Per-protocol (PP) population. The safety analysis will be performed on the safety population. Missing data will be handled by multiple imputations to evaluate the robustness of the primary endpoint analyses.20 The populations are defined as follows:
ITT population: This population consists of all randomised subjects, regardless of whether they are ineligible, prematurely discontinue treatment or are otherwise protocol violators/deviators.
PP population: This population is a subset of the ITT population. Subjects with major protocol deviations will be excluded from the PP population. Major protocol deviations will be defined in the statistical analysis plan.
Safety population: this population will be the same as the ITT population, which consists of all randomised subjects, who receive at least one dose of study drug.
The normality of continuous variables was examined using skewness and kurtosis. Categorical data were expressed as number and percentage. A generalised linear model will be employed to compare group differences in the primary outcome. No interim analysis was planned in our study. The detailed analysis strategies for secondary outcomes and subgroup analyses by the severity of AP (severe and non- severe), age (dichotomised at 60 years old), aetiologies of AP (biliary and non-biliary) and extent of pancreatic necrosis (>50% and ≤50%) will be included in the statistical analysis plan. Statistical tests will be two-sided, and p values <0.05 will be deemed as significant.
Adverse events
Adverse events (AEs) are defined in accordance with the National Cancer Institute-Common Terminology Criteria for Adverse Events as any untoward medical occurrence in a patient or clinical investigation subject administered an investigational intervention and which does not necessarily have to have a causal relationship with this treatment.
It is recognised that the study patient population (ANP with relatively high APACHE II score) will experience a number of common aberrations in laboratory values, signs and symptoms due to the severity of the underlying disease and the impact of standard therapies. These will not necessarily constitute an AE unless they require significant intervention or are considered to be of concern in the investigator’s clinical judgement. Thymosin alpha 1 is a well-studied drug with a favourable safety profile in previous trials.21 The DSMB will review the safety report every 6 months.
Recruiting process
The trial was registered on 16 June 2015. The first patient was randomised on 22 March 2017. So far, 426 patients had been randomised, and the enrolment keeps to the schedule.
Data collection and management
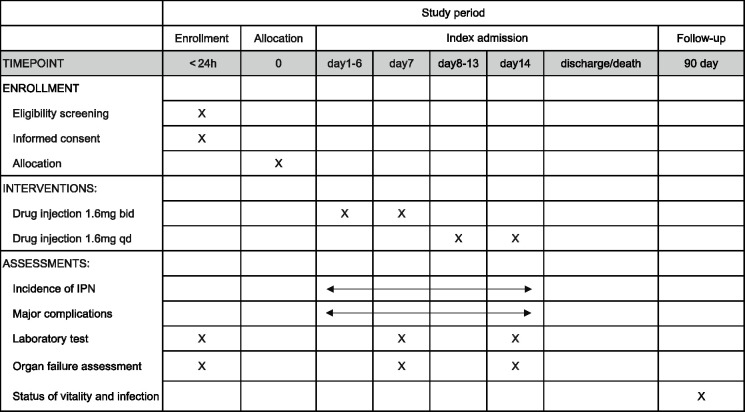
A web-based electrical database (access through the website of the CAPCTG, https://capctg.medbit.cn/) will be used for data collection and storage. All data will be input by the primary investigator or nominated investigators (less than two for each participating centre) approved by the primary investigator, and a double check will be done by the research coordinator. Training for data entry will be performed by the provider of the electrical database (Unimed Scientific, Wuxi, China) and the coordinating and data management centre of the CAPCTG. According to the schedule shown in figure 2, the investigator will collect data during the index admission and on day 90 after enrolment. If a study subject wishes to discontinue the study drug or the treating physician believes a study subject should discontinue the study drug due to medical considerations, the investigator will communicate with the study subject and the treating physician to obtain the reasons. Further evaluation and follow-up will still be performed unless the study subject withdraws consent for disclosure of information. The study blinding will only be broken in a medical emergency when the treating physician believes that the administration of the study drug is associated with the emergency.
Figure 2.
Schedule for participants enrolment, drug administration and data collection. IPN, infectedpancreatic necrosis.
Ethics approval and dissemination
This study was approved by the ethics committee of Jinling Hospital. The ethical approval document ID is 2015NZKY-004-02. Even when central ethical approval has been confirmed, we will not begin recruiting at other participating centres in the trial until the local ethics committee approved the study. Site ethical approvals were obtained from ethics committees of First Affiliated Hospital of Nanchang University, The Affiliated Hospital of Qingdao University, Affiliated Hospital of Zunyi Medical College, Nanhua Hospital, Second Affiliated Hospital of Nantong University, Yijishan Hospital of Wannan Medical College, 908th Hospital of Chinese People’s Liberation Army, Jiangsu Province Hospital on Integration of Chinese and Western Medicine, Zhejiang Provincial People’s Hospital, Luoyang Central Hospital, The Affiliated Hospital of Henan University of Science and Technology, Northern Jiangsu People’s Hospital, First People’s Hospital of Shangqiu, Qilu Hospital of Shandong University and First Affiliated Hospital of Anhui Medical University. The results of this trial will be reported in peer-reviewed journals and presented at scientific conferences.
Consent to participate
The consents for this study are obtained from each patient or his/her next of kin with full information regarding the possible adverse effects of the experimental drug and potential consequences. The translated patient consent form is attached as a online supplemental file.
bmjopen-2020-037231supp001.pdf (129.6KB, pdf)
Discussion
The TRACE trial was designed to test the efficacy of a new therapy targeting the immune system in preventing IPN following ANP, which is a potentially lethal complication causing substantial morbidity and mortality. We also aimed to investigate the efficacy of immunomodulatory treatment with thymosin alpha 1 in patients with different clinical characteristics using predefined subgroup analysis. The results of the TRACE trial would potentially provide a novel therapeutic option in the management of ANP and identify the patient population who may benefit most from the administration of thymosin alpha 1.
Immunomodulation is of significant clinical value in critically ill settings and the treatment of sepsis.12 While AP, which has a lot in common with sepsis like overwhelmed inflammation and infection-related complications, might be another suitable target for immunomodulatory therapy. In general, previously studied drugs such as lexipafant and octreotide were aimed to control cytokines, which are thought to be the pivotal part in the early inflammatory response of AP, rather than preventing the development of IPN.11 However, like what we learnt in sepsis, immunosuppression quickly following the initial inflammatory cascades should be the target of treatment during the course of ANP, as well, especially in those with organ failure.8 22 A pilot study published by our group several years ago indicated that the administration of thymosin alpha 1 could improve compromised monocyte HLA-DR expression and reduce infection rate in a small group of patients (n=24) with severe AP defined by the original Atlanta Classification. The result of this study is encouraging, which drive us to conduct this large multicentre randomized controlled trial (RCT) to obtain more reliable clinical evidences.14
The TRACE trial was sponsored by the Center of Severe Acute Pancreatitis(CSAP) at Jinling Hospital, Nanjing University, which is the national referral centre for AP admitting more than 600 cases of AP annually and coordinated by the CAPCTG coordinating and data management centre, which could cover the whole country. The trial is performed in 16 centres across China and aims to recruit 520 patients. Due to the limitation of the budget and technical availability, we can not conduct a continuous immune assessment with multiple markers and more time points. Alternatively, we choose monocyte HLA-DR, which is a representative parameter of the immune system, majorly reflecting the antigen presentation capacity to assess the immunomodulatory effect of thymosin alpha 1. HLA-DR was widely used in previous studies regarding immune function in different diseases like sepsis.12 23
In conclusion, the TRACE trial aims to assess the efficacy of thymosin alpha 1 administered early during the ANP on the incidence of IPN and other major clinical outcomes and thereby potentially offer a novel therapeutic option in the treatment of patients with ANP.
Supplementary Material
Footnotes
JZ and WM contributed equally.
Contributors: All authors were involved in the study design, and read and approved the final manuscript. During the study, JZ, WM and YL are responsible for randomising the patients and ensuring the blinding. JZ, WH, XP, MC, CH, WG, JW, JS, HN, JT, JS, GZ, WC, BX, XZ, MS are responsible for carrying out recruitment, managing the treatment of the patients and collecting data. WL, ZT, LK, JZ, TM and WH, XP, MC, CH, WG, JW, JS, HN, JT, JS, GZ, WC, BX, XZ, MS are members of the Trial Steering Committee. JZ, LK, ZT and TC drafted the manuscript.
Funding: This study is funded by SBE2016750187 of Science and technology project, Jiangsu Province, China, partly by SciClone Pharmaceuticals Holding Limited.
Competing interests: This study is supported by SBE2016750187 of Science and technology project, Jiangsu Province, China. SciClone Pharmaceuticals provides the study drug for this investigator-initiated study.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Dellinger EP, Forsmark CE, Layer P, et al. . Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg 2012;256:875–80. 10.1097/SLA.0b013e318256f778 [DOI] [PubMed] [Google Scholar]
- 2.Tenner S, Baillie J, DeWitt J, et al. . American College of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 2013;108:1400–15. 10.1038/ajg.2013.218 [DOI] [PubMed] [Google Scholar]
- 3.Wittau M, Mayer B, Scheele J, et al. . Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol 2011;46:261–70. 10.3109/00365521.2010.531486 [DOI] [PubMed] [Google Scholar]
- 4.Luiten EJ, Hop WC, Lange JF, et al. . Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Ann Surg 1995;222:57–65. 10.1097/00000658-199507000-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Besselink MG, van Santvoort HC, Buskens E, et al. . Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet 2008;371:651–9. 10.1016/S0140-6736(08)60207-X [DOI] [PubMed] [Google Scholar]
- 6.Bakker OJ, van Brunschot S, van Santvoort HC, et al. . Early versus on-demand nasoenteric tube feeding in acute pancreatitis. N Engl J Med 2014;371:1983–93. 10.1056/NEJMoa1404393 [DOI] [PubMed] [Google Scholar]
- 7.Uehara S, Gothoh K, Handa H, et al. . Immune function in patients with acute pancreatitis. J Gastroenterol Hepatol 2003;18:363–70. 10.1046/j.1440-1746.2003.02979.x [DOI] [PubMed] [Google Scholar]
- 8.Yu W-K, Li W-Q, Li N, et al. . Mononuclear histocompatibility leukocyte antigen-DR expression in the early phase of acute pancreatitis. Pancreatology 2004;4:233–43. 10.1159/000078748 [DOI] [PubMed] [Google Scholar]
- 9.Minkov GA, Yovtchev YP, Halacheva KS. Increased circulating CD4+CD25+CD127low/neg regulatory T-cells as a prognostic biomarker in acute pancreatitis. Pancreas 2017;46:1003–10. 10.1097/MPA.0000000000000894 [DOI] [PubMed] [Google Scholar]
- 10.Sun J-K, Mu X-W, Li W-Q, et al. . Effects of early enteral nutrition on immune function of severe acute pancreatitis patients. World J Gastroenterol 2013;19:917–22. 10.3748/wjg.v19.i6.917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang N, Ke L, Tong Z, et al. . The effect of thymosin α1 for prevention of infection in patients with severe acute pancreatitis. Expert Opin Biol Ther 2018;18:53–60. 10.1080/14712598.2018.1481207 [DOI] [PubMed] [Google Scholar]
- 12.Wu J, Zhou L, Liu J, et al. . The efficacy of thymosin alpha 1 for severe sepsis (ETASS): a multicenter, single-blind, randomized and controlled trial. Crit Care 2013;17:R8. 10.1186/cc11932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin-Loeches I, Muriel-Bombín A, Ferrer R, et al. . The protective association of endogenous immunoglobulins against sepsis mortality is restricted to patients with moderate organ failure. Ann Intensive Care 2017;7:44. 10.1186/s13613-017-0268-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X, Li W, Niu C, et al. . Thymosin alpha 1 is associated with improved cellular immunity and reduced infection rate in severe acute pancreatitis patients in a double-blind randomized control study. Inflammation 2011;34:198–202. 10.1007/s10753-010-9224-1 [DOI] [PubMed] [Google Scholar]
- 15.Banks PA, Bollen TL, Dervenis C, et al. . Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–11. 10.1136/gutjnl-2012-302779 [DOI] [PubMed] [Google Scholar]
- 16.Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology 2002;223:603–13. 10.1148/radiol.2233010680 [DOI] [PubMed] [Google Scholar]
- 17.Working Group IAP/APA Acute Pancreatitis Guidelines IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013;13:e1–15. 10.1016/j.pan.2013.07.063 [DOI] [PubMed] [Google Scholar]
- 18.Sun J-K, Li W-Q, Ni H-B, et al. . Modified gastrointestinal failure score for patients with severe acute pancreatitis. Surg Today 2013;43:506–13. 10.1007/s00595-013-0496-6 [DOI] [PubMed] [Google Scholar]
- 19.Ke L, Ni H-B, Tong Z-H, et al. . D-dimer as a marker of severity in patients with severe acute pancreatitis. J Hepatobiliary Pancreat Sci 2012;19:259–65. 10.1007/s00534-011-0414-5 [DOI] [PubMed] [Google Scholar]
- 20.Zhang Z. Multiple imputation with multivariate imputation by chained equation (mice) package. Ann Transl Med 2016;4:30. 10.3978/j.issn.2305-5839.2015.12.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schulof RS. Thymic peptide hormones: basic properties and clinical applications in cancer. Crit Rev Oncol Hematol 1985;3:309–76. 10.1016/S1040-8428(85)80035-4 [DOI] [PubMed] [Google Scholar]
- 22.Kylänpää-Bäck ML, Takala A, Kemppainen E, et al. . Cellular markers of systemic inflammation and immune suppression in patients with organ failure due to severe acute pancreatitis. Scand J Gastroenterol 2001;36:1100–7. 10.1080/003655201750422738 [DOI] [PubMed] [Google Scholar]
- 23.Zorio V, Venet F, Delwarde B, et al. . Assessment of sepsis-induced immunosuppression at ICU discharge and 6 months after ICU discharge. Ann Intensive Care 2017;7:80. 10.1186/s13613-017-0304-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037231supp001.pdf (129.6KB, pdf)