Abstract
Hip displacement is a common orthopedic problem in children with cerebral palsy (CP) that can result in significant morbidity. Hip surveillance has been shown to reduce the incidence of hip dislocations in children with CP and to reduce the need for salvage hip surgeries. Guidelines for hip surveillance have been developed and can be adapted to meet local needs. Implementation of surveillance guidelines for a population of children is complex and highly dependent upon the region, province/state, or country’s system of care for children with CP. Recognizing that implementation of the evidence on hip surveillance was necessary in British Columbia, a Canadian province spanning 1 million square kilometers, a comprehensive, coordinated approach to hip surveillance was developed collaboratively by provincial stakeholders. Surveillance guidelines and a desired implementation plan were established based on the best available research evidence, current international practice, and service delivery in British Columbia. Staged implementation preceded full provincial roll out. Implementation was supported by detailed communication, knowledge translation, and evaluation plans. This province-wide hip surveillance program is the first of its kind in North America.
Keywords: cerebral palsy, hip, implementation, surveillance
Introduction
Hip displacement affects one in three children with cerebral palsy (CP) [1–4]. Treatment of hip displacement and dislocation is dependent upon when the problem is detected. Left untreated progressive hip displacement may cause pain, loss of mobility, difficulties with personal care, and decreased quality of life [5–8].
Preventive and reconstructive surgical interventions, prior to dislocation, are recommended to ensure the hip remains in joint, mobile, and pain free [9–11]. Preventive surgery, which involves lengthening of the hip adductors, and possible lengthening of the iliopsoas and obturator neurectomy, often fails in children who are nonambulatory but may delay the need for bony reconstruction [12–14]. Definitive treatment typically involves reconstructive surgery with a femoral varus derotation osteotomy and possibly a pelvic osteotomy. Reconstructive surgery has been shown to reduce pain frequency and intensity and improve health-related quality of life [11,15]. Salvage surgeries, which include arthrodesis, femoral-head resection with valgus osteotomy, proximal femoral resection with soft-tissue interposition, and replacement arthroplasty, may be required for painful, dislocated hips when the severity of the damage prevents reconstruction [16]. While such surgeries can have a positive result, they are associated with inconsistent pain relief, increased risk of complications, and high rates of surgical revisions making them a less desirable result [17,18].
Hip surveillance is the process of identifying and monitoring early indicators of progressive hip displacement to enable early assessment and management by an orthopedic surgeon [19]. Existing hip surveillance programs recommend clinical and radiological examinations at frequencies dictated by the child’s risk for displacement as indicated by their Gross Motor Function Classification System (GMFCS) level [19–21]. The clinical examination includes identifying the child’s GMFCS level and may include assessment of range of motion, tone, and pain. A supine anteroposterior (AP) pelvis radiograph taken in standardized positioning is required [19].
Research evidence supports the use of hip surveillance to decrease the incidence of hip dislocations and salvage procedures in children with CP [3,20–23]. A recent systematic review reported that implementation of formal hip surveillance programs is associated with a significant decrease in the incidence of hip dislocation, particularly when associated with responsive orthopedic surgical services [24]. In 2014, results from 20 years of hip surveillance in Sweden were reported and showed a drop in dislocation rate from 8% in a historical control to 0.5% in the surveillance group [20].
The British Columbia experience
Historically, monitoring of hip displacement in children with CP has been highly variable throughout the province of British Columbia, a large Canadian province with a population of more than 4.5 million people spanning over 1 million square kilometers. In some cases, only once a hip became painful would a child have been assessed by a pediatric orthopedic surgeon. In 2009, a chart audit showed that salvage procedures for painful, dislocated hips accounted for a greater than expected percentage of hip surgeries performed in an 18-month period. A comparison of the surgical practice at the province’s major treatment, teaching and research pediatric hospital, to one Australian state with an established hip surveillance strategy showed there was a dramatic difference in the proportion of children requiring salvage procedures in British Columbia.
It was identified that failure to implement a hip surveillance program would contribute to decreased mobility and quality of life for children with CP and may increase medical costs to the system. Consequently, a proposal highlighting the need for hip surveillance and summarizing the supporting literature was developed. With the support of parents of children with CP, the need for a change in practice was communicated to hospital administration, parent groups, and government. Parents of children with CP who had experienced salvage procedures or whose children were at risk of requiring salvage procedures advocated for change. Working with key stakeholders, Child Health BC organized a provincial process to identify evidence based strategies to prevent hip displacement and dislocation for children and youth with CP in British Columbia. Child Health BC (www.childhealthbc.ca) is a network of healthcare providers that aims to improve access to high quality clinical health services for all children in British Columbia.
Consensus building
In 2011, Child Health BC hosted a meeting that spanned 1.5 days and was attended by parents, pediatric orthopedic surgeons, developmental pediatricians, pediatricians, general physicians, a radiologist, physiotherapists, occupational therapists, therapy services managers, nurses, and policy makers. Selected guests were invited based on their knowledge of the problem and their role in service delivery to children with CP in the province. Stakeholders from all regions of the province, including both urban and rural settings, were invited. A content expert from outside the province also attended. The objective of this interdisciplinary workshop was to facilitate consultation aimed at identifying a standardized, comprehensive, and coordinated approach to hip management and to improve provincial surveillance practices with the ultimate aim of reducing the incidence of hip displacement and the need for complex surgical procedures. Additionally, the meeting aimed to identify barriers and supports for implementation of a provincial guideline for hip surveillance and consider the necessary evaluation of any proposed system of service.
Creation of British Columbia specific guidelines
To encourage participants to consider hip surveillance within the province’s framework of existing service providers and vast geography, a description of the population of children with CP in the province and the provision of regional and provincial specialized and subspecialized services for these children was provided. The opportunity to strengthen community capacity by optimizing healthcare resources closer to home was emphasized. The current status of orthopedic care was described which demonstrated the need for improved management of hip displacement. Best practices for early detection and intervention for hip dislocation in children with CP and the published evidence on hip surveillance was presented. Surveillance practices and outcomes from both Australia and Sweden were reviewed and compared [1–3,19,21]. Finally, the need to consider meaningful outcomes, such as quality of life, was highlighted.
Following these presentations and open discussion, there was unanimous agreement that standardized hip surveillance was needed in British Columbia. Utilizing the Australian Standards of Care as a starting point for discussion, the group considered and discussed the purpose of hip surveillance, delineation of roles and responsibilities for executing surveillance, and the level of evidence available to support the guidelines used internationally. Consensus was subsequently reached on key foundational points using a voting system. There was agreement that: the guidelines should be based on GMFCS levels, a clinical examination and radiograph must be included, skeletal maturity be defined as closure of the triradiate cartilage, migration percentage of 30% be considered at-risk, and the guidelines not include intervention. Relevant definitions, including those for CP, surveillance, displacement, and dislocation, were agreed upon. Pediatric orthopedic surgeons in attendance agreed that only a single AP pelvis radiograph is necessary for hip surveillance.
In determining the components of the clinical examination, the lack of evidence to support clinical measures being used to detect hip displacement was discussed. Participants questioned how the results would be utilized as indicators for a referral to a pediatric orthopedic surgeon. In addition, the need to standardize assessments across multiple assessors and the high degree of measurement error between assessors was noted. A list of musculoskeletal measurements was produced following this discussion, but it was proposed that further review of the evidence for use of these measures was indicated.
Specific guidelines for each of the GMFCS levels were then developed. International surveillance practices and evidence were reviewed throughout this discussion. Provision of services for children with CP in British Columbia was considered, along with the need to provide uniform services for children throughout the entire province. Overuse of resources, radiation exposure, and undersurveillance were considered. In order to promote the optimal balance for these issues, the group agreed to create guidelines in four subgroups: (1) GMFCS levels I and II, (2) GMFCS level III, (3) GMFCS levels IV and V, and (4) Winters, Gage, & Hicks Group IV hemiplegic gait pattern. Discussion initially focused on children at the highest risk, those at GMFCS levels IV and V. Consensus was reached on the commencement, and frequency for surveillance. The recommendations established for this high-risk group were then used as a basis for children at lower GMFCS levels. It was agreed that discharge from surveillance occur at age 5 years for children at GMFCS levels I and II and skeletal maturity for those at GMFCS levels III–V or with a group IV hemiplegic gait pattern when migration percentage is less than 30%, and there are no clinical concerns. This established the British Columbia Consensus on Hip Surveillance for Children with Cerebral Palsy (Fig. 1).
Fig. 1.
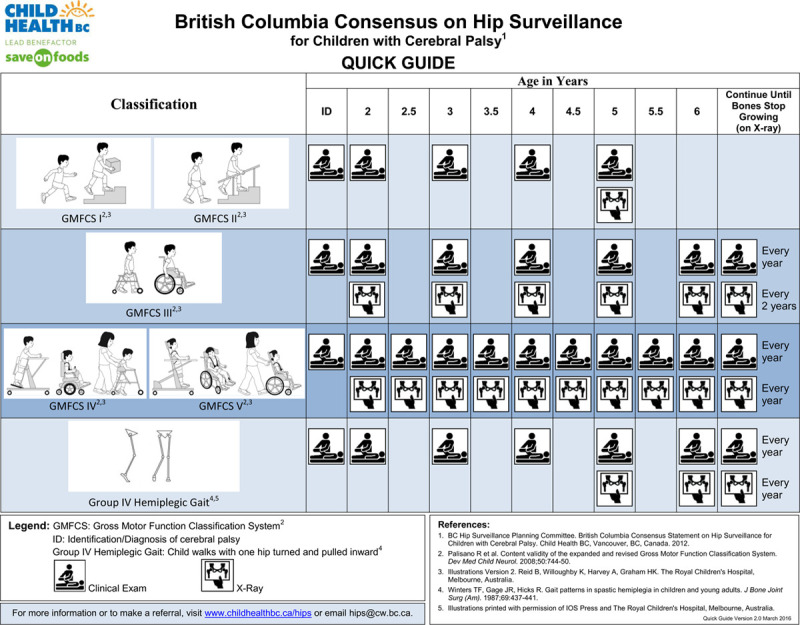
British Columbia Consensus Statement on Hip Surveillance for Children with Cerebral Palsy – 2012 Quick Guide. Reproduced with permission of Child Health BC, Vancouver, Canada (www.childhealthbc.ca/hips).
Barriers to implementation
Participants subsequently divided into groups, based on geographic region, to discuss potential barriers to implementation. Areas of discussion included engaging healthcare providers, delineation of roles, data management, access to care, physical resources and supplies, and knowledge translation. Suggested solutions to the identified barriers, from a regional perspective, were then discussed. Results of these discussions were used to form the framework of a subsequent meeting that focused on implementation.
Implementation planning
In 2012, Child Health BC convened a second meeting with the goal of gaining agreement on a model for province-wide implementation. A parent of a child with CP opened the meeting to highlight the need to consider the child and family when developing an implementation plan. Prior to implementation planning, outstanding issues from the first meeting were further discussed. Evidence supporting the role of clinical examination measures in hip surveillance was reviewed by meeting organizers prior to the meeting. It was confirmed that there is no evidence to support the use of clinical measures in identifying hip displacement and that the reliability of goniometric and tone measures is questionable. Pediatric orthopedic surgeons in the province were surveyed to determine which clinical measures and values were important to their decision making regarding hip displacement and should warrant a referral to orthopedics. The surgeons came to consensus on the clinical exam elements (Table 1) and referral criteria specific to hip surveillance (Table 2) which were presented and subsequently approved by the meeting attendees.
Table 1.
Summary of 2012 consensus on hip surveillance clinical examination measures
| Clinical examination components | |
|---|---|
| Classify | GMFCS level |
| If hemiplegia, identify if Type IV hemiplegic gait | |
| Measure | Hip abduction range of motion with hips at 0° flexion (slow speed) |
| Angle of hip abduction at which a muscle reaction is elicited on passive movement at a fast speed (Tardieu scale) | |
| Thomas test for hip flexion contracture | |
| Ask | Does your child experience pain related to the hip? This may be noticed when changing your child’s position, when you move your child’s leg, or during daily activities such as diaper changing? |
| Do you have more difficulty caring for your child during activities such as perineal care, dressing, bathing or other similar activities requiring hip movement? | |
| Has there been deterioration in your child’s function, such as a change in their ability to walk or a decreased ability or tolerance of sitting or standing, which is related to the hip? | |
| Who is your family physician/pediatrician? | |
The child’s physical therapist typically completes the classification and measurement components of the clinical examination and asks the child and or the child’s caregiver the questions listed. (Tardieu Scale [25]).
GMFCS, Gross Motor Function Classification System.
Table 2.
Summary of criteria for referral to a pediatric orthopedic surgeon from hip surveillance
| Parameter | Referral criteria (any one or more) |
|---|---|
| Migration percentage | >30% |
| Hip abduction end range | ≤30˚ |
| Hip abduction or Thomas test | Deterioration or asymmetry |
| Clinical examination questions | Positive answer to any one of the three |
| Other | Any other clinical concern that is felt to be related to the hip |
Implementation considerations and models
Prior to the meeting, five key questions were identified to assist meeting delegates in developing an implementation model (Table 3). Three potential models for implementation were presented to the group that offered different options to these key questions. The models featured (1) coordination by a provincial and/or regional coordinator and utilization of an electronic management system; (2) coordination without a data management system; and (3) recommendations for practice with no coordination. These models differed in the resources required and method of service delivery. Following the presentation of these models, participants were divided, based on geographic region, and asked to consider which model was most suitable to service provision in their region and to provide suggestions for improvements while considering the key questions that were introduced.
Table 3.
Questions identified as being significant when developing an implementation plan for system wide hip surveillance
| Key questions to consider for implementation |
|---|
| 1. Who will identify the child? |
| a. Who will ensure the child meets program criteria and complete enrollment? |
| b. Who will complete the clinical examination? |
| 2. Who will manage surveillance? |
| 3. Is a database required? |
| 4. Who will request a radiograph? |
| 5. Who will measure migration percentage? |
There was consensus amongst all regions that the preferred model includes a provincial coordinator and a data management system (Fig. 2). In this model, surveillance occurs in the child’s home community with the child’s local healthcare team working collaboratively with a provincial coordinator, a physiotherapist, and medical lead, a pediatric orthopedic surgeon, who are based at the provincial tertiary care pediatric hospital. Physiotherapists in child development centers and schools throughout the province were identified as key in identifying, enrolling, and completing the required clinical exam due to their existing relationships with children with CP and their families and their skills in completing the clinical examination. Imaging, when recommended, occurs locally but is ordered and reviewed by the coordinator and medical lead with the coordinator measuring migration percentage. If a child meets one of the preidentified criteria (Table 2), they are referred to a pediatric orthopedic surgeon at the province’s children’s hospital or one of four pediatric orthopedic surgeons throughout the province. No regions identified that coordination should be done at a regional level, but did identify the use of regional content experts as a possible strategy to improve knowledge translation.
Fig. 2.
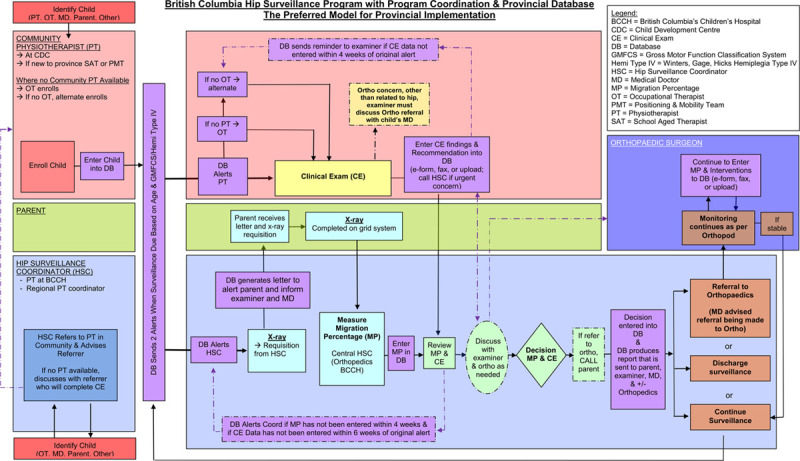
Preferred implementation model. Reproduced with permission of Child Health BC, Vancouver, Canada (www.childhealthbc.ca/hips).
When discussing implementation, concern was raised that children at GMFCS levels I and II may be at risk of missing the clinical examination and radiograph that was originally recommended at age 6 in the established British Columbia Consensus. In British Columbia, children typically transition from early intervention services to school services at age 5. While children at GMFCS levels I and II are likely to receive early intervention services, they rarely qualify for school based services and, therefore, may not have access to a physiotherapist to complete the clinical examination at age 6. The original choice of 6 years for children at GMFCS I and II was based on the Swedish model and provided continuity with the guidelines for those at levels III, IV, and V. After a prolonged discussion, consensus was reached that children that are classified at GMFCS level I and II or that have a Type IV hemiplegic gait pattern would be better served if the clinical examination and radiograph were moved to age 5.
Knowledge translation and evaluation
The group identified knowledge translation as being an essential component to successful implementation. Knowledge translation considerations, methods, and content were reviewed and the group recognized that regional and individual differences in knowledge translation needs and preferences may exist. The most effective knowledge translation methods were identified based on the available evidence. Again, in regional subgroups, participants identified what information needed to be communicated and to whom.
The importance of outcome evaluations and proposed topics for evaluation were presented. Four areas for evaluation were identified and included: (1) effectiveness of knowledge translation strategies; (2) adherence to the consensus statement; (3) patient and family outcomes; and (4) the consensus statement.
Program implementation and launch
Using the established consensus statement and the provincial implementation plan, Child Health BC established a business plan for the launch of the program. With hospital administration and government support, the Child Health BC Hip Surveillance Program for Children with Cerebral Palsy was launched in 2014.
Initially focusing on program development, detailed communication and knowledge translation plans were created that identified target audiences, key messaging, and individualized knowledge translation strategies. To support province wide implementation, work was completed to identify early intervention (0–5 years) and school aged (5–18 years) physiotherapy and occupational therapy services in the province. Possible gaps in these services were identified. An initial needs survey of therapists in the province was completed to identify therapists’ knowledge about hip surveillance and determine their learning and support needs. A quality assurance and evaluation plan was developed to assess program outcomes. These initiatives were developed with input from a multidisciplinary, provincial Advisory Committee. This committee, which includes parents and has representation from all regions of the province, was established to provide leadership and guidance during the program development.
Enrollment of children in the program began in 2015 at province’s tertiary care pediatric hospital. Two trial sites, with differing implementation challenges, were identified and subsequently began enrolling children in February 2016. Staged implementation allowed for trialing of knowledge translation materials, enrollment forms, and processes for communication. After successfully enrolling over 250 children at these sites, province wide implementation was initiated in 2016. Implementation was based on the previously developed model as previously described and illustrated in Fig. 2. The provincial coordinator and medical lead are responsible for overseeing the implementation and management of the surveillance program while supporting community physiotherapists and physicians in communities throughout the province.
Conclusion
Hip surveillance allows for early detection of hip displacement in children with CP. Systematically performed clinical and radiological exams are required. Guidelines for hip surveillance in British Columbia were established collaboratively by a multidisciplinary group of stakeholders representing all regions of the province. Being mindful of provincial resources and service delivery throughout a geographically vast area, a preferred model of implementation with provincial coordination and electronic data management was developed and subsequently executed using a staged, coordinated approach.
Development and implementation of hip surveillance guidelines must meet the requirements of the local healthcare system. Our implementation strategy was based on the strengths of the service delivery model in our province and may not be appropriate for all jurisdictions. Variables within the local context, including case finding, care coordination, review of radiographs, and data management, must be considered when developing an implementation strategy.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. 2006; 88:121–129 [DOI] [PubMed] [Google Scholar]
- 2.Hägglund G, Lauge-Pedersen H, Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord. 2007; 8:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connelly A, Flett P, Graham HK, Oates J. Hip surveillance in tasmanian children with cerebral palsy. J Paediatr Child Health. 2009; 45:437–443 [DOI] [PubMed] [Google Scholar]
- 4.Terjesen T. The natural history of hip development in cerebral palsy. Dev Med Child Neurol. 2012; 54:951–957 [DOI] [PubMed] [Google Scholar]
- 5.Bagg MR, Farber J, Miller F. Long-term follow-up of hip subluxation in cerebral palsy patients. J Pediatr Orthop. 1993; 13:32–36 [DOI] [PubMed] [Google Scholar]
- 6.Samilson RL, Tsou P, Aamoth G, Green WM. Dislocation and subluxation of the hip in cerebral palsy. Pathogenesis, natural history and management. J Bone Joint Surg Am. 1972; 54:863–873 [PubMed] [Google Scholar]
- 7.Penner M, Xie WY, Binepal N, Switzer L, Fehlings D. Characteristics of pain in children and youth with cerebral palsy. Pediatrics. 2013; 132:e407–e413 [DOI] [PubMed] [Google Scholar]
- 8.Jung NH, Pereira B, Nehring I, Brix O, Bernius P, Schroeder SA, et al. Does hip displacement influence health-related quality of life in children with cerebral palsy? Dev Neurorehabil. 2014; 17:420–425 [DOI] [PubMed] [Google Scholar]
- 9.Presedo A, Oh CW, Dabney KW, Miller F. Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J Bone Joint Surg Am. 2005; 87:832–841 [DOI] [PubMed] [Google Scholar]
- 10.El-Sobky TA, Fayyad TA, Kotb AM, Kaldas B. Bony reconstruction of hip in cerebral palsy children gross motor function classification system levels III to V: a systematic review. J Pediatr Orthop B. 2018; 27:221–230 [DOI] [PubMed] [Google Scholar]
- 11.Rutz E, Vavken P, Camathias C, Haase C, Jünemann S, Brunner R. Long-term results and outcome predictors in one-stage hip reconstruction in children with cerebral palsy. J Bone Joint Surg Am. 2015; 97:500–506 [DOI] [PubMed] [Google Scholar]
- 12.Miller F, Dabney KW, Rang M. Epps CH, Jr, Bowen JR. Complications in cerebral palsy treatment. Complications in Pediatric Orthopaedic Surgery. 1995, Philadelphia: Lippincott Company; 477–544 [Google Scholar]
- 13.Shore BJ, Yu X, Desai S, Selber P, Wolfe R, Graham HK. Adductor surgery to prevent hip displacement in children with cerebral palsy: the predictive role of the gross motor function classification system. J Bone Joint Surg Am. 2012; 94:326–334 [DOI] [PubMed] [Google Scholar]
- 14.Kiapekos N, Broström E, Hägglund G, Åstrand P. Primary surgery to prevent hip dislocation in children with cerebral palsy in Sweden: a minimum 5-year follow-up by the national surveillance program (CPUP). Acta Orthop. 2019; 18:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiFazio R, Shore B, Vessey JA, Miller PE, Snyder BD. Effect of hip reconstructive surgery on health-related quality of life of non-ambulatory children with cerebral palsy. J Bone Joint Surg Am. 2016; 98:1190–1198 [DOI] [PubMed] [Google Scholar]
- 16.Shore BJ, Graham HK. Management of moderate to severe hip displacement in nonambulatory children with cerebral palsy. JBJS Rev. 2017; 5:e4. [DOI] [PubMed] [Google Scholar]
- 17.Kolman SE, Ruzbarsky JJ, Spiegel DA, Baldwin KD. Salvage options in the cerebral palsy hip: a systematic review. J Pediatr Orthop. 2016; 36:645–650 [DOI] [PubMed] [Google Scholar]
- 18.Boldingh EJ, Bouwhuis CB, van der Heijden-Maessen HC, Bos CF, Lankhorst GJ. Palliative hip surgery in severe cerebral palsy: a systematic review. J Pediatr Orthop B. 2014; 23:86–92 [DOI] [PubMed] [Google Scholar]
- 19.Wynter M, Gibson N, Kentish M, Love S, Thomason P, Kerr Graham H. The consensus statement on hip surveillance for children with cerebral palsy: australian standards of care. J Pediatr Rehabil Med. 2011; 4:183–195 [DOI] [PubMed] [Google Scholar]
- 20.Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J. 2014; 96-B:1546–1552 [DOI] [PubMed] [Google Scholar]
- 21.Hägglund G, Andersson S, Düppe H, Lauge-Pedersen H, Nordmark E, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy. The first ten years of a population-based prevention programme. J Bone Joint Surg Br. 2005; 87:95–101 [PubMed] [Google Scholar]
- 22.Kentish M, Wynter M, Snape N, Boyd R. Five-year outcome of state-wide hip surveillance of children and adolescents with cerebral palsy. J Pediatr Rehabil Med. 2011; 4:205–217 [DOI] [PubMed] [Google Scholar]
- 23.Dobson F, Boyd RN, Parrott J, Nattrass GR, Graham HK. Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br. 2002; 84:720–726 [DOI] [PubMed] [Google Scholar]
- 24.Wynter M, Gibson N, Willoughby KL, Love S, Kentish M, Thomason P, Graham HK; National Hip Surveillance Working Group. Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. 2015; 57:808–820 [DOI] [PubMed] [Google Scholar]
- 25.Haugh AB, Pandyan AD, Johnson GR. A systematic review of the Tardieu scale for the measurement of spasticity. Disabil Rehabil. 2006; 28:899–907 [DOI] [PubMed] [Google Scholar]


