Background:
A suitable fundus camera for telemedicine screening can expand the scale of eye care service. The purpose of this study was to compare a handheld nonmydriatic digital fundus camera and a conventional mydriatic fundus camera according to the image quality of their photographs and usability of those photographs to accurately diagnose various retinal diseases.
Methods:
A handheld nonmydriatic fundus camera and conventional fundus camera were used to take fundus photographs of outpatients at an ophthalmic clinic before and after pupillary dilation. Image quality and diagnostic agreement of the photos were graded by two masked and experienced retinal specialists.
Results:
A total of 867 photographs of 393 eyes of 200 patients were collected. Approximately 80% of photos taken under nonmydriasis status using the handheld nonmydriatic fundus camera had good (55.7%) or excellent (22.7%) image quality. The overall agreement of diagnoses between the doctors was more than 90%. When the handheld nonmydriatic fundus camera was used after mydriasis, the proportion of images with good (45%) or excellent (49.7%) quality reached 94.7% and diagnostic agreement was 93.4%. Lens opacity was associated with the quality of images obtained using the handheld camera (p = 0.041), and diagnosis disagreement for handheld camera images was associated with preexisting diabetes diagnosis (p = 0.009). Approximately 40% of patients expressed preference for use of the handheld nonmydriatic camera.
Conclusion:
This study demonstrated the effectiveness of the handheld nonmydriatic fundus camera in clinical practice and its feasibility for telemedicine screening of retinal diseases.
Keywords: Handheld nonmydriatic fundus camera, Retinal diseases, Telemedicine
1. INTRODUCTION
Digital retinal photography has played a critical role in ophthalmic diagnostics over the past few years.1–3 Digital fundus photographs are easy to display, archive, and transmit and have thus simplified clinical work. In addition, digital communication has greatly enhanced the practice of teleophthalmology. Digital images collected in remote areas where medical resources are scarce can be transferred electronically to an image reading center where well-trained personnel can perform disease screening and identification. After image transfer and disease screening, patients suspected to have ocular disorders may be further referred to an ophthalmologist to receive diagnosis and treatment. Thus, ocular health care can be delivered to remote populations through a telemedicine system with the aid of digital communication.
Digital fundus cameras are efficient tools for screening for retinal diseases. However, the table-top configuration of the conventional fundus camera constrains its application in particular situations such as examination of patients with limited mobility, bedridden patients, or noncooperative pediatric patients. Moreover, the use of the table-top fundus camera in impoverished and remote areas remain rare due to the limited funding its system implementation and the camera’s poor maneuverability. Hence, portable devices specialized for primary fundus screening are comparatively practical in telemedicine.4 A suitable fundus camera for telemedicine screening could expand the scale of eye care services and thus reduce the incidence of advanced diseases and even blindness. In this study, we compared image quality, diagnostic accuracy, and patient preference between a handheld nonmydriatic digital fundus camera and a conventional mydriatic fundus camera.
2. METHODS
This study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of Taipei Veterans General Hospital (TVGH). Outpatients attending the ophthalmic clinic of TVGH were enrolled in the study and gave informed consent. From July 2012 to May 2013, 867 photographs of 393 eyes of 200 patients were collected.
Fundus photographs of the patients were taken using a handheld nonmydriatic fundus camera (Horus Eye-Fundus Camera; Medimaging Integrated Solution Inc., Hsinchu, Taiwan) before and/or after pupillary dilation (1% tropicamide, Alcon), and then taken using a conventional fundus camera (CX1 Retinal Camera; Canon Inc., Tokyo, Japan) with pupil dilatation. The handheld camera was manipulated with the patient sitting on the chair and looking into the fixation target light in the camera. The pictures were taken by stepping on a foot pedal, which is connected to the camera. The conventional camera was mounted on table as usual. The images obtained with the handheld fundus camera had a field of view (FOV) of 40° and a resolution of two megapixels. The images taken by the conventional fundus camera had 50° FOV and 18-megapixel resolution. Medical personnel and technicians who were well-trained in fundus photography captured the photographs. Images were required to cover the fundus regions of a patient’s macula and optic disc to be eligible for collection and analysis. Images of eyes with angle-closure glaucoma were excluded from the study. On-the-spot diagnostic results obtained by a senior ophthalmologist were recorded and used in subsequent camera comparisons. These diagnostic results may be confirmed by extra examinations such as fluorescein angiography or optical coherence tomography in addition to the fundus records. The patients’ preferences with regard to the camera type were also recorded.
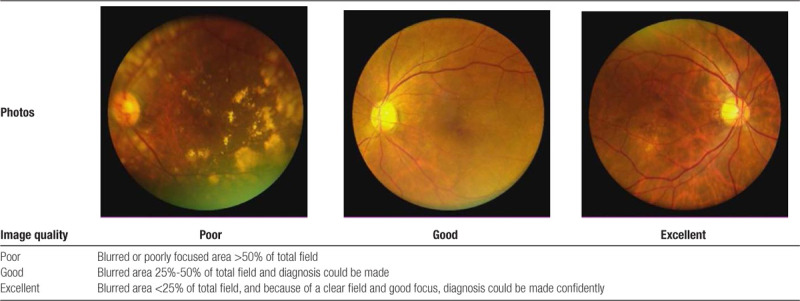
All photographs were randomized and presented on computer screens to two masked and experienced ophthalmologists. The ophthalmologists separately evaluated their image quality and made diagnoses without information about the patients or the cameras used. Diagnostic results were compared between the two ophthalmologists, as well as to the on-the-spot diagnostic results, for each of the three imaging situations (undilated handheld nonmydriatic camera photos, dilated handheld nonmydriatic camera photos, and conventional camera photos). Image quality was evaluated as excellent if blurred areas comprised of less than 25% of the fundus field and clear and in-focus areas contributed to a valid diagnosis; good if blurred areas accounted for 25%-50% of the fundus field and a diagnosis could be made; and poor if blurred or poorly focused areas comprised of more than half of the total field (Table 1).
Table 1.
Definition of image quality
Statistical analysis was performed using IBM SPSS (version 20.0; IBM Corp., Somers, NY, USA). Distribution patterns of image quality and diagnosis consistency were compiled using Pearson’s chi-square test and Fisher’s exact test. Differences with p < 0.05 were considered statistically significant.
3. RESULTS
Among the patients, 111 were men and 89 were women. Their average age was 61.61 years. Gender distribution did not vary according to age. The handheld nonmydriatic digital fundus camera was used to photograph the fundus regions of 44 patients before and after pupil dilation. In seven cases, photographs were only taken before pupil dilation, and in 149 cases, photographs were only taken after pupil dilation.
A total of 31 diagnoses were made including: age-related macular degeneration, epiretinal membrane, proliferative diabetic retinopathy (DR), myopic maculopathy, choroidal neovascularization, retinal detachment, and others (Fig. 1). The sensitivity of the handheld mydriatic and the mydriatic conventional camera were 93.8% and 96.3%, respectively. The compared sensitivity (the handheld mydriatic/the mydriatic conventional camera) was 97.4%. The specificity of the handheld mydriatic and the mydriatic conventional camera were 89.2% and 85.7%, respectively. The compared specificity (the handheld mydriatic/the mydriatic conventional camera) was 104.1%.
Fig. 1.
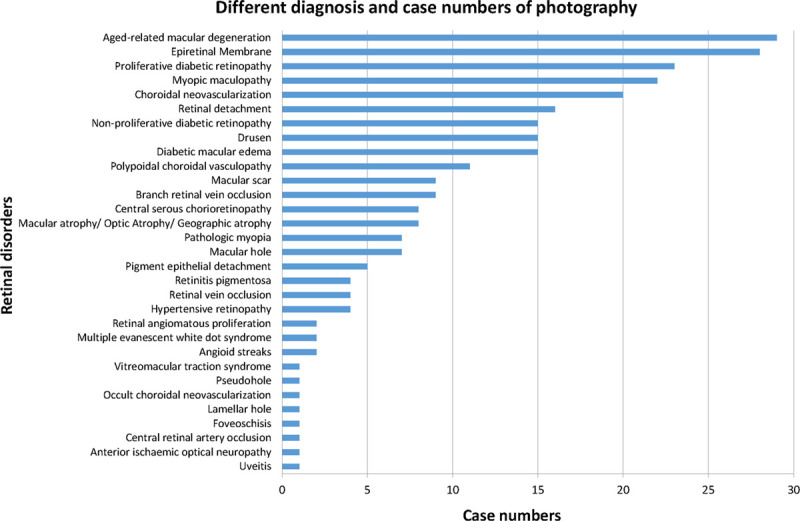
Diagnoses and case numbers of patients photographed.
The image quality of photographs obtained using the handheld nonmydriatic camera was good (55.7%) and excellent (22.7%) for approximately 80% of photos taken under nonmydriasis and for 94.7% (45% good and 49.7% excellent) of photos taken under mydriasis. The conventional camera photograph image quality was good and excellent in 24% and 73.5% of cases, respectively (97.5% of all the images were satisfactory). The overall prevalence of agreement of the diagnoses made by the two doctors on the basis of the handheld nonmydriatic photos taken under nonmydriasis exceeded 90% (Table 2).
Table 2.
Comparison of image quality and diagnostic agreement
| Image quality and diagnostic agreement | Nonmydriasis | Mydriasis | p | |
|---|---|---|---|---|
| Handheld nonmydriatic fundus camera, n (%) | Handheld nonmydriatic fundus camera, n (%) | Conventional fundus camera, n (%) | ||
| Poor | 21 (21.6) | 20 (5.3) | 10 (2.5) | <0.05* |
| Good | 54 (55.7) | 170 (45.0) | 94 (24.0) | |
| Excellent | 22 (22.7) | 188 (49.7) | 288 (73.5) | |
| Diagnosis Agreement | 88 (90.7) | 353 (93.4) | 373 (95.2) | |
p < 0.05.
Of the nonmydriatic photos taken using the handheld nonmydriatic camera, 21.6% (21/97) were ungradable. Univariate analysis showed that lens opacity was significantly associated with poor image quality (p = 0.041) (Table 3), whereas age, gender, pupil size, and a diagnosis of diabetes were not. Diagnosis of diabetes was significantly associated with diagnostic disagreement between doctors (p = 0.009) (Table 4), whereas age, gender, pupil size, and lens opacity were not.
Table 3.
Univariate analysis of image quality
| Handheld nonmydriatic fundus camera | ||
|---|---|---|
| Nonmydriasis | ||
| n (%) | p | |
| Age | ||
| <65 y/≥65 y | 13 (21.3)/8 (22.2) | 0.916 |
| Gender | ||
| Male/female | 11 (23.9)/10 (19.6) | 0.607 |
| Pupil diameter | ||
| ≤4 mm/>4 mm | 14 (20.9)/0 (0.0) | 0.578 |
| Lens condition | ||
| Cataract/clear lens or pseudophakia | 4 (57.1)/13 (18.8) | 0.041* |
| Diabetes | ||
| Yes/no | 5 (45.5)/16 (18.6) | 0.056 |
p < 0.05.
Table 4.
Univariate analysis for diagnostic disagreement
| Handheld nonmydriatic fundus camera | ||
|---|---|---|
| Nonmydriasis | ||
| n (%) | p | |
| Age | ||
| <65 y/≥65 y | 5 (8.2)/4 (11.1) | 0.723 |
| Gender | ||
| Male/female | 6 (13.0)/3 (5.9) | 0.301 |
| Pupil diameter | ||
| ≤4 mm/>4 mm | 5 (7.5)/1 (25.0) | 0.303 |
| Lens condition | ||
| Cataract/clear lens or pseudophakia | 1 (14.3)/4 (5.8) | 0.392 |
| Diabetes | ||
| Yes/no | 4 (36.4)/5 (5.8) | 0.009* |
p < 0.05.
All patients who completed the three stages of photography completed a questionnaire. The factors used to assess patient preferences between the handheld nonmydriatic camera and conventional camera were level of camera flash before and after dilation, exposure discomfort, and shooting-prolonged discomfort (Table 5). Among the 51 patients who had photos taken before dilation, 41 preferred the handheld nonmydriatic fundus camera (80.39%); nine specified no preference between the two cameras (17.65%); and only one patient considered the handheld nonmydriatic fundus camera worse than the conventional camera (1.96%). Among the 149 patients who had photos taken after dilation, 35 preferred the handheld nonmydriatic fundus camera (23.49%); 104 specified no preference (60.80%); and 10 patients considered the handheld nonmydriatic fundus camera worse than the conventional camera (6.71%).
Table 5.
Questionnaire regarding patients’ camera preferences
| Questionnaire | Standard score |
|---|---|
| Pre-phobia | Discomfort experienced anticipating the flash of the newly developed camera before dilation. Level of discomfort scored from 1 to 10; a higher score indicates greater discomfort |
| Pre-time | Anticipating the flash of the newly developed camera before pupillary dilation. Level of discomfort scored from 1 to 10; a higher score indicates greater discomfort |
| Post-phobia | Discomfort level of accepting the flash of the newly developed camera after dilation. Level of discomfort scored from 1 to 10; a higher score indicates greater discomfort |
| Post-time | The process of accepting the flash of the newly developed camera after pupillary dilation. Level of discomfort scored from 1 to 10; a higher score indicates greater discomfort |
| Compare | Compare comfort between being photographed using the newly developed and conventional cameras: |
| (1) New camera is better | |
| (2) Both provide a comfortable experience | |
| (3) New camera is worse | |
| Overall | Which camera would you choose for an eye exam: |
| (1) Newly developed camera, nonmydriasis | |
| (2) Conventional camera, mydriasis | |
| (3) Newly developed camera, mydriasis | |
| (4) No preference among the three options |
Approximately 40% of the patients (76/200) indicated preference for the handheld nonmydriatic camera. Preference for the handheld nonmydriatic fundus camera without mydriasis was 19% (38/51 patients) and with mydriasis was 18% (36/149 patients). Fifty percent of patients felt that there was no difference between the two devices (Fig. 2).
Fig. 2.
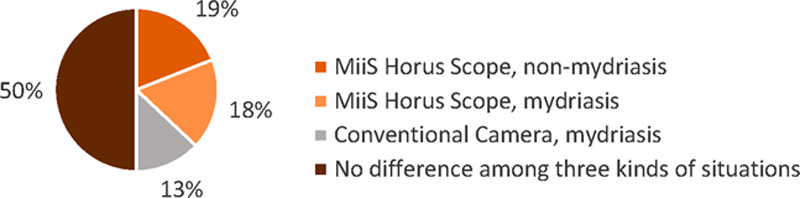
Camera type and photography condition preferences of 200 patients.
4. DISCUSSION
In previous teleophthalmology studies, researchers have used either mydriatic or nonmydriatic fundus photography and fixed in-clinic conventional fundus cameras, digital nonmydriatic retinal cameras, or RetCams (RetCam II [Clarity Medical Systems, Pleasanton, CA]/The Retcam 120 wide-angle fundus camera [Novartis Pharma AG, Basel, Switzerland]). These cameras have been proven effective as diagnostic tools for eye diseases including DR, retinopathy of prematurity, age-related macular degeneration, and others.1–3,5–10 Our study demonstrated the effectiveness and practicability of the handheld nonmydriatic fundus camera for examining retinal diseases (Fig. 3).
Fig. 3.
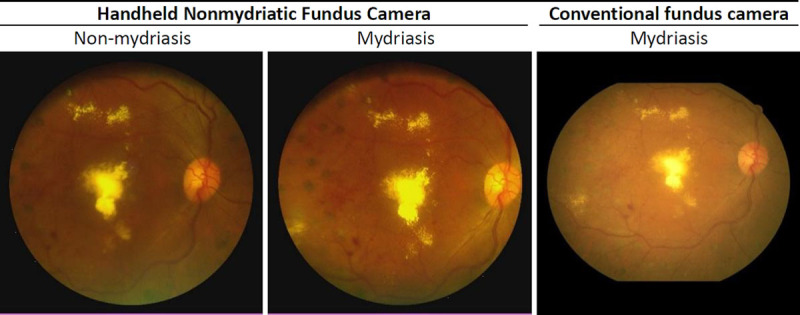
Photos of a same patient with diabetic retinopathy taken by both cameras with or without mydriasis.
Although nonmydriatic cameras provide lower image quality and a smaller FOV than conventional cameras, they present other advantages for screening and for use in emergency circumstances.11–14 Our results showed that, of images taken under nonmydriasis, 80% were satisfactory and could be used to determine diagnoses; their quality was comparable to that of the conventional camera images. When mydriasis was used, 94.7% of images were good quality and diagnostic agreement was 93.4%. The most common causes of low photograph quality have been reported to be media opacity and poor pupil dilation.3,15 Our results agreed with these findings and showed that lens condition was the critical factor in image quality.
Studies focused on DR screening demonstrated that nonmydriatic color photos were at least as sensitive as mydriatic ophthalmoscopy, and a single nonmydriatic monochromatic wide-field digital photograph of a disk and macula was found to be even better.5,16 However, microaneurysms, which may be difficult to visualize, may limit their usability.8 Seven-field mydriatic color images of a relatively large fundus area have the advantage of stereopsis and are considered the gold standard for determining DR severity; by comparison, nonmydriatic digital images are not as detailed. This inferiority reasonably explains the significant association of diabetes with diagnostic disagreement that was found in this study.
A high proportion of patients in this study expressed preference for the handheld nonmydriatic fundus camera over the conventional fundus camera. Only 13% (26/200) of the patients preferred that the conventional camera be used to photograph them, whereas approximately 40% (37/200) preferred that the handheld nonmydriatic fundus camera be used. Lamirel et al11 reported factors that increased the quality of nonmydriatic photographs taken in an emergency department. The ideal time range in which to take photographs was found to be 30-90 seconds, most likely because this range does not provide adequate time for pupillary redilation after the first flash. A waiting time longer than this window was associated with poorer photograph quality.11 In our study, the low flash intensity of the nonmydriatic digital camera-enabled photography of two or more fields within a relatively short time. It also shortened the imaging time and decreased flash-related discomfort before pupillary dilation, resulting in the relative preferability of the camera among patients.
The major purposes of current teleophthalmology services are patient screening and appropriate referral to experts.17,18 Numerous studies have shown that increasing numbers of patients are satisfied with telemedicine because it increases health care accessibility and reduces traveling cost and time.19 Examinations through teleophthalmology were shown to be less expensive than conventional in-person examinations.20 A study showed that screening for DR in a community health center was 35% less costly when telemedicine was used rather than direct observation.21 Use of telemedicine screening for DR among populations in underdeveloped rural areas showed cost efficiency, but the expense of maintaining remote imaging facilities in such circumstances may render annual testing economically impractical. The handheld nonmydriatic fundus camera used in our study not only provides satisfactory image quality but also presents the advantages of portability, data storage capacity, and wireless communication of digital images. Thus, the camera may greatly enhance the practice of telemedicine. In telehealth programs, nonmydriatic digital cameras may also be used for detecting retinopathy and may increase the screening rate. Taylor et al22 reported that showing patients their eye condition at the site of screening significantly increased reattendance.
In conclusion, this study demonstrated the feasibility of using a handheld nonmydriatic digital fundus camera to diagnose various retinal disorders. The results showed that the camera could produce photographs with satisfying image quality that contribute to high diagnostic accuracy. Thus, this device is suitable for use in teleophthalmology.
ACKNOWLEDGMENTS
This study was an Industry-Government-Academic Cooperation Project supported by the Small Business Innovation Research program (No. 1Z1000040) of the Ministry of Economic Affairs, Taiwan. The project was formally approved by Taipei Veterans General Hospital (Institutional Review Board No. 2012-06-022B).
Footnotes
Conflicts of interest: Dr S.-J. Chen was a consultant at Medimaging Integrated Solution Inc. from December 2016 to December 2017. The other authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.Williams GA, Scott IU, Haller JA, Maguire AM, Marcus D, McDonald HR. Single-field fundus photography for diabetic retinopathy screening: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1055–62. [DOI] [PubMed] [Google Scholar]
- 2.Taylor CR, Merin LM, Salunga AM, Hepworth JT, Crutcher TD, O’Day DM, et al. Improving diabetic retinopathy screening ratios using telemedicine-based digital retinal imaging technology: the Vine Hill study. Diabetes Care. 2007;30:574–8. [DOI] [PubMed] [Google Scholar]
- 3.Szabó D, Fiedler O, Somogyi A, Somfai GM, Bíró Z, Ölvedy V, et al. Telemedical diabetic retinopathy screening in Hungary: a pilot programme. J Telemed Telecare. 2015;21:167–73. [DOI] [PubMed] [Google Scholar]
- 4.Ting DS, Tay-Kearney ML, Kanagasingam Y. Light and portable novel device for diabetic retinopathy screening. Clin Exp Ophthalmol. 2012;40:e40–6. [DOI] [PubMed] [Google Scholar]
- 5.Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol. 2002;134:204–13. [DOI] [PubMed] [Google Scholar]
- 6.Thomas SM, Jeyaraman MM, Jeyaraman M, Hodge WG, Hutnik C, Costella J, et al. The effectiveness of teleglaucoma versus in-patient examination for glaucoma screening: a systematic review and meta-analysis. PLoS One. 2014;9:e113779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang SK, Callaway NF, Wallenstein MB, Henderson MT, Leng T, Moshfeghi DM. SUNDROP: six years of screening for retinopathy of prematurity with telemedicine. Can J Ophthalmol. 2015;50:101–6. [DOI] [PubMed] [Google Scholar]
- 8.Newton MJ. The promise of telemedicine. Surv Ophthalmol. 2014;59:559–67. [DOI] [PubMed] [Google Scholar]
- 9.Jirawison C, Yen M, Leenasirimakul P, Chen J, Guadanant S, Kunavisarut P, et al. Telemedicine screening for cytomegalovirus retinitis at the point of care for human immunodeficiency virus infection. JAMA Ophthalmol. 2015;133:198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wedekind L, Sainani K, Pershing S. Supply and perceived demand for teleophthalmology in triage and consultations in California emergency departments. JAMA Ophthalmol. 2016;134:537–43. [DOI] [PubMed] [Google Scholar]
- 11.Lamirel C, Bruce BB, Wright DW, Delaney KP, Newman NJ, Biousse V. Quality of nonmydriatic digital fundus photography obtained by nurse practitioners in the emergency department: the FOTO-ED study. Ophthalmology. 2012;119:617–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouyang Y, Heussen FM, Keane PA, Sadda SR, Walsh AC. The retinal disease screening study: retrospective comparison of nonmydriatic fundus photography and three-dimensional optical coherence tomography for detection of retinal irregularities. Invest Ophthalmol Vis Sci. 2013;54:5694–700. [DOI] [PubMed] [Google Scholar]
- 13.Chin EK, Ventura BV, See KY, Seibles J, Park SS. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed J E Health. 2014;20:102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mackay DD, Bruce BB. Non-mydriatic fundus photography: a practical review for the neurologist. Pract Neurol. 2016;16:343–51. [DOI] [PubMed] [Google Scholar]
- 15.Toy BC, Myung DJ, He L, Pan CK, Chang RT, Polkinhorne A, et al. Smartphone-based dilated fundus photography and near visual acuity testing as inexpensive screening tools to detect referral warranted diabetic eye disease. Retina. 2016;36:1000–8. [DOI] [PubMed] [Google Scholar]
- 16.Cavallerano AA, Cavallerano JD, Katalinic P, Tolson AM, Aiello LP, Aiello LM; Joslin Vision Network Clinical Team Use of Joslin Vision Network digital-video nonmydriatic retinal imaging to assess diabetic retinopathy in a clinical program. Retina. 2003;23:215–23. [DOI] [PubMed] [Google Scholar]
- 17.Sreelatha OK, Ramesh SV. Teleophthalmology: improving patient outcomes? Clin Ophthalmol. 2016;10:285–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caffery LJ, Taylor M, Gole G, Smith AC. Models of care in tele-ophthalmology: A scoping review. J Telemed Telecare. 2019;25:106–22. [DOI] [PubMed] [Google Scholar]
- 19.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320:1517–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lamminen J, Forsvik H, Vopio V, Ruohonen K. Teleconsultation: changes in technology and costs over a 12-year period. J Telemed Telecare. 2011;17:412–6. [DOI] [PubMed] [Google Scholar]
- 21.Li HK. Telemedicine and ophthalmology. Surv Ophthalmol. 1999;44:61–72. [DOI] [PubMed] [Google Scholar]
- 22.Taylor DJ, Fisher J, Jacob J, Tooke JE. The use of digital cameras in a mobile retinal screening environment. Diabet Med. 1999;16:680–6. [DOI] [PubMed] [Google Scholar]


