Abstract
To date, SARS-CoV-2 (the virus that causes COVID-19) has spread to almost every region of the world, infecting millions and resulting in the deaths of hundreds of thousands of people. Although it was predicted that Africa would suffer a massive loss of life due to this pandemic, the number of COVID-19 cases has been relatively low across the continent. Researchers have speculated that several factors may be responsible for this outcome in Africa, including the extensive experience that countries have with infectious diseases and the young median age of their populations. However, it is still important for African countries to adopt aggressive and bold approaches against COVID-19, in case the nature of the pandemic changes. This short review will summarize the status of the outbreak in Africa and propose possible reasons for current trends, as well as discuss interventions aimed at preventing a rapid increase in the number of COVID-19 cases in the future.
Keywords: Africa, SARS-CoV-2 cases, COVID-19 susceptibility, Public health interventions, Pandemic
Introduction
The first cases of the novel coronavirus (2019-nCoV) were reported in late December 2019 in the city of Wuhan, Hubei province in the People’s Republic of China (Morawska and Milton, 2020). Phylogenetic analysis of whole genome sequence data also showed that 2019-nCoV falls within the genus Betacoronavirus, which includes the severe acute respiratory syndrome coronavirus (SARS-CoV), the Middle East respiratory syndrome coronavirus (MERS-CoV), and several bat-derived SARS-like coronaviruses (Chen et al., 2020, Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, 2020, Udugama et al., 2020, Xu et al., 2020). On February 12, 2020, the World Health Organization (WHO) officially named the novel coronavirus SARS-CoV-2, the pathogen causing COVID-19 (“coronavirus disease 2019”) (Srivastava et al., 2020). In March, COVID-19 was declared a global pandemic with more than 100,000 cases and 4000 deaths in over 100 countries. Currently, SARS-CoV-2 has spread to every part of the globe except Antarctica, infecting millions and killing hundreds of thousands of people. In Africa, the first confirmed case of COVID-19 was reported in Egypt on February 14 (Rosenthal et al., 2020), and by March COVID-19 cases were observed across most of the continent (Rosenthal et al., 2020).
SARS-CoV-2 is an enveloped virus containing a positive-sense, single-stranded RNA genome ∼30 kilobases in length with 5′-cap structure and 3′-poly-A tail (Chen et al., 2020). Moreover, SARS-CoV-2 shares ∼50% similarity with MERS-CoV, ∼96% with bat coronavirus RaTG13 and 80% sequence identity to SARS-CoV (Chen et al., 2020, Ge et al., 2013, Udugama et al., 2020, Zhou et al., 2020). Additionally, SARS-CoV-2 mainly infects the respiratory and gastrointestinal tracts of humans using the angiotensin-converting enzyme 2 (ACE2) receptors to gain entry into host cells (Pal et al., 2020). Although studies have reported that the highest transmissibility of SARS-CoV-2 occurs around the time of symptom onset (Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, 2020, Ghinai et al., 2020), recent analyses have shown that asymptomatic individuals can also contribute to the onward transmission of the virus (Al-Tawfiq, 2020, Chan et al., 2020, Moghadas et al., 2020, Rothe et al., 2020). Furthermore, studies have found that aerosols containing viral RNA—released during exhalation, talking, and coughing—are a major route of transmission in addition to respiratory droplets and contaminated surfaces (van Doremalen et al., 2020, Jayaweera et al., 2020, Li et al., 2020). RecentlyRec, a number of clinical trials were conducted to identify effective therapeutic vaccines against SARS-CoV-2 (Lurie et al., 2020, Thanh Le et al., 2020). Although several promising vaccines have been discovered, they are not yet widely available to the general public. Notably, prior to their development, several other therapeutic interventions had been proposed. For example, research in China suggested that nutritional interventions, immuno-enhancers, interferon, intravenous gamma-globulin and thymosin have an anti-viral effect against several coronaviruses including SARS-CoV-2 (Xie and Chen, 2020). Furthermore, an herbal tonic (“COVID-Organics”), derived from the sweet wormwood (Artemisia annua) plant, had been promoted as a potent treatment for COVID-19 in Madagascar (Dandara et al., 2020). Additionally, several studies have reported that hydroxychloroquine and the closely-related compound chloroquine can inhibit the transmission of coronaviruses in vitro (Hernandez et al., 2020, Vincent et al., 2005, Xie and Chen, 2020, Yao et al., 2020). However, the efficacy of these proposed treatments for COVID-19 has not been convincingly demonstrated to date, and in some cases these remedies are highly discouraged (Abena et al., 2020, Hernandez et al., 2020, Meyerowitz et al., 2020, Torti et al., 2020).
State of affairs in Africa
As COVID-19 swept across the globe, resulting in the deaths of hundreds of thousands of people, this devastating loss of life has not been reported for much of Africa, despite the grim predictions of misery across the continent due to the pandemic (Berhan, 2020, Torti et al., 2020). As of November 25, there were 2.1 million confirmed cases of SARS-CoV-2 infection on the African continent (50,715 total deaths) in comparison to the ∼16.3 million cases in Europe (371,005 total deaths) and the ∼15.3 million cases in North America (398,846 total deaths) (Johns Hopkins, 2020, WorldoMeter, 2020). Furthermore, it has been reported that among the SARS-CoV-2 positive cases in Africa, the proportion of severe COVID-19 outcomes, including death, appears to be lower than expected (in fact, mortality attributed to the novel coronavirus in Africa is less than 1% of the global cases of death reported to date) (Chibwana et al., 2020, Torti et al., 2020, Uyoga et al., 2020, World Health Organization, 2020). The relatively low number of reported confirmed coronavirus positive cases, cases of severe COVID-19, and COVID-19-related deaths in Africa (Table 1 ) could be due to a number of factors, a few of which we discuss below:
Table 1.
Reported total number of positive cases, deaths and new cases of COVID-19 by major continental region on November 25, 2020. * % indicates the percentage of the world total for Total cases, Total deaths, and New cases, respectively. Data for Table 1 come from WorldoMeter (2020).
| Country | Total cases | (%)* | Total deaths | (%)* | New cases (single day) | (%)* |
|---|---|---|---|---|---|---|
| Europe | 16,252,809 | 26.8 | 371,005 | 26.0 | 212,384 | 38.6 |
| North America | 15,279,312 | 25.2 | 398,846 | 28.0 | 161,649 | 29.3 |
| Asia | 16,098,425 | 26.5 | 283,312 | 19.9 | 108,006 | 19.6 |
| South America | 10,851,433 | 17.9 | 320,035 | 22.5 | 54,856 | 10.0 |
| Africa | 2,119,193 | 3.5 | 50,715 | 3.6 | 13,672 | 2.4 |
| Oceania | 44,136 | 0.07 | 1,011 | 0.07 | 17 | 0.003 |
| World | 60,645,308 | 1,424,924 | 550,584 |
Host genetics
While the majority of SARS-CoV-2 studies have focused on the genomic and epidemiological characteristics of the virus, the role of host genetics in COVID-19 onset has been largely unexplored (Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, 2020). This gap in our knowledge motivated the launch of the Host Genetics Initiative, which aims to identify host genetic factors that influence the risk for COVID-19 (Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, 2020). To date, research groups affiliated and unaffiliated with the Host Genetics Initiative have reported strong associations between a number of genetic loci and COVID-19 susceptibility in European and South Asian populations (Ellinghaus et al., 2020, Zeberg and Pääbo, 2020). For example, a recent study identified a cluster of genes on chromosome 3 correlated with respiratory failure in hospitalized COVID-19 patients in southern Europe (Ellinghaus et al., 2020).
Indigenous Africans are characterized by higher levels of within– and between– population genetic diversity compared to non-Africans (Campbell et al., 2014). This genetic variation also has been shown to influence resistance to a number of infectious diseases (Gomez et al., 2014). For example, prior studies have indicated that some individuals who are highly exposed to the human immunodeficiency 1 virus (HIV-1) in Africa remain uninfected likely due to allelic differences in immune-related genes (Marmor et al., 2006, Songok et al., 2012, Tomescu et al., 2011, Yao et al., 2014). In another study, structural variation at the GYPA and GYPB genes are correlated with a 40% reduced risk for severe malaria (Leffler et al., 2017). Furthermore, a genetic analysis reported evidence for adaptive evolution at the GYPA and GYPB genes in African populations living in malaria-endemic environments (Ko et al., 2011). In addition, studies also have detected genetic signatures of adaptive change at other loci (such as APOL1, LARGE and IL-21) that are suggested to be protective against African trypanosomiasis and Lassa fever (Ko et al., 2013, Telenti and Goldstein, 2006, Vitti et al., 2013). Arguably, it is not inconceivable that genetic variation present in sub-Saharan Africa could confer resistance to COVID-19 in contemporary populations. However, more genetic and epidemiological studies, including case-control and fine mapping analyses, are needed to explore this hypothesis.
Experience with pandemics
Africa has extensive experience with a number of historical and emerging infectious diseases, including the plague, cholera, malaria, sleeping sickness, Ebola, HIV and TB (Egeru et al., 2020, El-Sadr and Justman, 2020, Mwisongo and Nabyonga-Orem, 2016, 0). Therefore, African countries already have a high capacity to combat pathogen outbreaks (El-Sadr and Justman, 2020, Mwisongo and Nabyonga-Orem, 2016, Quaglio et al., 2020). Notably, in response to the COVID-19 pandemic, African intergovernmental agencies worked quickly to minimize transmission of the novel coronavirus at a relatively early stage (Massinga Loembé et al., 2020). For example, an emergency meeting of African health ministers (hosted by the African Union Commission) was convened on February 22 and discussions resulted in the formation of the Africa Taskforce for Coronavirus Preparedness and Response. The African Union of Member States and the Africa CDC also launched the Africa COVID-19 Response Fund to raise money for transmission prevention, medical responses, and socioeconomic support (Quaglio et al., 2020). Furthermore, individual countries implemented public health interventions to reduce the spread of the COVID-19 virus. For instance, as early as the beginning of January, Ivory Coast conducted enhanced surveillance of passengers at airports, and Rwanda instituted a nationwide lockdown shortly after the first case of COVID-19 appeared in March (Kavanagh et al., 2020, Massinga Loembé et al., 2020). To date, Ivory Coast and Rwanda have a reported 21,168 cases (131 total deaths) and 5779 cases (47 total deaths), respectively (WorldoMeter, 2020). Other mitigating actions implemented by African countries included quarantines, curfews, school and border closures, the installation of hand-washing stations in public spaces, and restrictions on the number of attendees at social gatherings (Kavanagh et al., 2020, Lamarche, 2020, Mwisongo and Nabyonga-Orem, 2016).
Intriguingly, it also has been suggested that previous exposure to other less-lethal coronaviruses could provide individuals with some protection from COVID-19 (Nordling, 2020). Thus, researchers have hypothesized that regular exposure to these infectious agents among others in Africa could prepare the immune system to fight new pathogens, including SARS-CoV-2 (Nordling, 2020).
Lack of testing
The prevalence of SARS-CoV-2 infection and corresponding disease are underestimated in Africa due to the low capacity of many countries to test for the virus. Although the WHO recommends the use of nucleic acid amplification tests for diagnosing SARS-CoV-2 infection, these PCR-based tests are expensive and inaccessible for most African countries (Shey et al., 2020, Torti et al., 2020). Furthermore, only a small proportion of rapid immunoassay-based tests with high specificity and sensitivity are available globally. Thus, scaling up diagnostic testing for SARS-CoV-2 in Africa is currently very challenging (Duong et al., 2020, Kavanagh et al., 2020). Consequently, African scientists have shifted their focus to the development of cheaper immunoassay diagnostic kits (Torti et al., 2020, Wild, 2020). However, the efficacy of these tests remains unclear. Nonetheless, widespread testing is needed to monitor the rate of infection as well as determine the extent to which individuals advance to and/or die from severe COVID-19 across the continent. Additionally, it will be important to expand this testing into rural environments where infection status and disease prevalence are not well-known since some communities may not have regular access to primary health care (Musoke et al., 2014).
Misdiagnosis
Equally as important, misdiagnosis of COVID-19 could potentially inhibit countries’ ability to accurately determine disease prevalence. In the absence of testing, the identification of COVID-19 cases involves individuals presenting themselves to health professionals with complaints of symptoms (e.g. fever, cough, shortness of breath, fatigue, headache, gastro-intestinal problems among others) (Chanda-Kapata et al., 2020, Kusotera and Nhengu, 2020). Interestingly, however, malaria also shares common symptoms with COVID-19 (Chanda-Kapata et al., 2020). Therefore, it is possible that COVID-19 could be misclassified as malaria and vice versa, if symptoms alone are used to diagnose cases (Chanda-Kapata et al., 2020). Furthermore, patients could also have COVID-19 and malaria co-infection, and the diagnosis/treatment of one disease may lead to missing the presence of the other (Chanda-Kapata et al., 2020).
The young age of populations
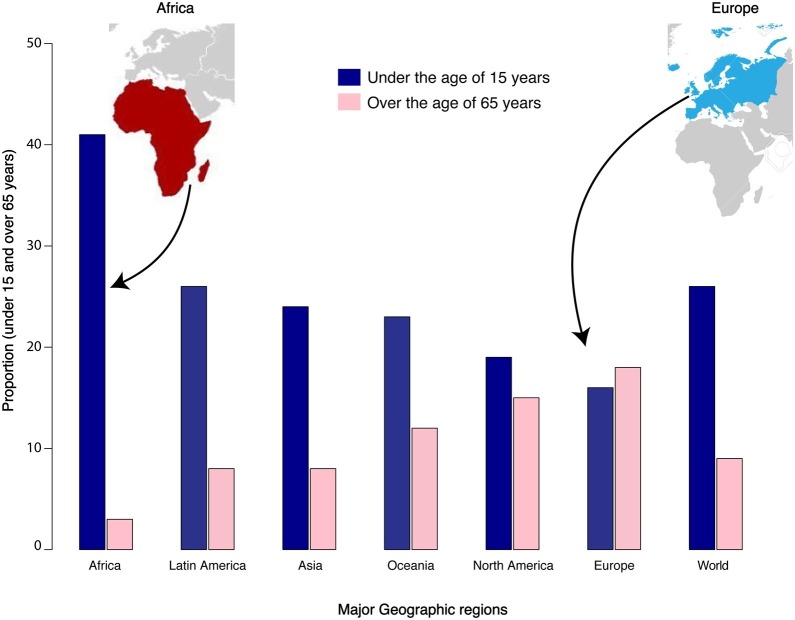
While people of all ages are susceptible to COVID-19, older individuals (>65 years of age) and those with pre-existing medical conditions—such as cardiovascular disease, obesity, chronic respiratory disease, and cancer—are at a higher risk for severe disease (Jordan et al., 2020, Petrakis et al., 2020, Williamson et al., 2020). Many countries in Africa have a relatively young population with the median age of 19.7 years and a small proportion of individuals over the age of 60 years (Diop et al., 2020). In fact, Africa has the largest proportion of young people in the world (Figure 1 ). Hence, in situations where there may be high infection rates within younger age groups, these individuals can be either asymptomatic or have a greater capacity to overcome the disease (Diop et al., 2020). It is important to note that in Italy—one of the countries hit hardest by SARS-CoV-2—23.1% of its population is age 65 and over (Faye et al., 2020, Kondō, 2010, Renzaho, 2020), giving some support to the notion that the age structure of African countries may reduce the risk for severe COVID-19.
Figure 1.
Proportion of two age classes across major geographic regions. The figure shows the proportion of individuals under the age of 15 years (in blue) and the proportion of individuals over the age of 65 years (in pink) for major continents (Desjardins, 2020). The figure also includes maps of Africa and Europe, two continents that are compared in the manuscript.
No time to be complacent
While there have been examples of success in the fight against COVID-19, mitigating actions are still needed to contain the spread of SARS-CoV-2 in Africa. Indeed, without sustained public health interventions, there is the potential for an increase in the number of COVID-19 cases, as countries eventually begin to ease lockdowns (The Lancet Editorial, 2020). As another complicating factor, studies have found several novel recurrent mutations in the SARS-CoV-2 genome, leading to the emergence of multiple strains of the virus (Eaaswarkhanth et al., 2020, Pachetti et al., 2020). However, the contribution of this genetic variability to the evolution of drug resistance in SARS-CoV-2 or to its infectivity remains unclear. Given these events, it is important to remain vigilant in order in order to minimize the risk for SARS-CoV-2 infection in Africa. Below, we discuss several public health considerations that can potentially reduce the transmission of this virus in the future:
Community-directed intervention
To encourage adherence to public policies, community involvement in health initiatives needs to be a priority (Massinga Loembé et al., 2020). In particular, outreach activities by local leaders can help to inform other community members about COVID-19 transmission and health-promoting behavior (Massinga Loembé et al., 2020). This strategy is particularly useful in remote regions of African countries where people face barriers to COVID-19 care services (Massinga Loembé et al., 2020). For example, in Chad traditional storytellers (known as “troubadours”) and town criers—trained in COVID-19 prevention awareness—are deployed in rural communities to provide health information and to dispel myths about the coronavirus (International Organization for Migration, 2020). However, the extent to which individual countries engage in this type of community-based intervention is not fully known.
Enhanced hygiene
It is estimated that 47% of individuals in Africa do not have access to clean water, representing a monumental barrier to combatting the spread of COVID-19 and water-borne diseases (Armah et al., 2018). Moreover, data have indicated that SARS-CoV-2 particles can be found in human feces, raising the possibility of fecal-oral transmission of the virus (Heller et al., 2020). Consequently, regular hand-washing with soap is a critical step in decreasing the transmission of SARS-CoV-2 (Singh, 2020). As a stop-gap measure, the WHO has provided guidelines for manufacturing hand sanitizers, which can be implemented in African countries (Pickering et al., 2010). Nevertheless, the need for improved sanitation and access to clean water across Africa cannot be underestimated, particularly among socioeconomically disadvantaged communities (Armah et al., 2018).
Increased testing
Given the current limits of COVID-19 testing, African scientists have devised local solutions, such as the development of immunoassay diagnostic kits, to enhance testing capacity (Torti et al., 2020, Yeung, 2020). The African Union also announced plans to distribute one million COVID-19 test kits across the continent (Rosenthal et al., 2020). In addition, the further development of existing rapid kits—for example, saliva-based tests recently approved by the Federal Drug Administration in the United States (Vogels et al., 2020, Wyllie et al., 2020)—could yield non-invasive and low-cost alternatives to current methods. Indeed, large-scale testing will be beneficial for detecting infected individuals (including asymptomatic people who contribute to the transmission of SARS-CoV-2) and for guiding prevention efforts (Moghadas et al., 2020). In addition, unlike nucleic acid tests, highly sensitive and specific rapid kits for widespread testing can enable clinicians to detect the presence of SARS-CoV-2 in patients, including asymptomatic individuals, providing a fast and accurate estimate of infection status (Udugama et al., 2020). However, with more than 70 countries restricting export of needed medical supplies, the import of diagnostic kits for widespread use in Africa is an ongoing challenge (Nkengasong, 2020). As a possible solution to this problem, it has been suggested that African countries band together to purchase medical supplies as a single customer, wherever export markets are open, and then distribute these supplies amongst themselves (Nkengasong, 2020).
Enhanced isolation and contact tracing
Besides testing, the WHO recommends other mitigation measures, such as the immediate isolation of cases and rigorous tracking of contacts among other public health strategies. Indeed, recent data have shown that a combination of isolation and contact tracing can effectively prevent onward transmission (Moghadas et al., 2020, Senghore et al., 2020). To track the primary and secondary contacts of confirmed COVID-19 cases, one targeted approach that has been proposed is the use of mobile positioning data technology. Currently, researchers at the University of Cape Town in South Africa are developing a smartphone app that will enable the Department of Health to find and alert the contacts of infected individuals (Nachega et al., 2020, Rose et al., 2020). Given the high transmission rate of SAR-CoV-2, a combination of isolation and contact tracing practices will be needed to minimize the risk of resurgence, particularly as countries begin the process of lifting restrictions.
Strengthen the supply chain
Indeed, increased availability of medical and laboratory supplies, including personal protective equipment, is important for protecting healthcare workers and patients from infection (Quaglio et al., 2020, Rosenthal et al., 2020). However, regular supply of these critical materials is complicated in Africa given the continent’s limited manufacturing capacity (Rosenthal et al., 2020). To mitigate this situation, a possible short-term solution is investment in the manufacture of low-tech supplies, such reusable face masks produced by local seamsters (Rosenthal et al., 2020). Additionally, humanitarian aid and other financial resources can serve as a stop-gap to ensure the provisioning of essential supplies until longer-term solutions are found. Other beneficial measures include the suspension of tariffs on health-care products and the easing of restrictions on food exports, as recommended by the United Nations.
Enhanced patient care
Although prevention is the strongest defense against COVID-19, it is also important for African countries to provide a high level of care, including respiratory support, for people who become ill. However, there are currently fewer than 5000 available intensive care unit (ICU) beds in 43 Africa countries, equaling five beds per one million individuals (in comparison, Europe has 4000 beds per million individuals) (Quaglio et al., 2020). Furthermore, there is a critical shortage of ventilators and healthcare professionals who are trained in intensive care in most African countries (Quaglio et al., 2020). Overall, innovative solutions that lead to enhanced patient care are badly needed in Africa.
Conclusion
Although the novel coronavirus has presented unique challenges in Africa, many countries have implemented measures designed to slow the rate of infection and resulting disease. However, it is still important to strengthen efforts to build resilient healthcare systems to combat COVID-19 and future pandemics. As humans continue to transform their environments, emerging infectious diseases and their global spread will be one of the grand challenges that countries will face over the coming decades. To counter these rising problems, countries around the world will need to consider serious investment in science and healthcare infrastructure, improved testing capacity, and therapeutic solutions including manufacturing (Faye et al., 2020). Equally as important, building social welfare and protection (e.g. governmental financial support) for vulnerable people in communities characterized by poverty cannot be ignored (Ebuenyi, 2020). This social investment will help to minimize the adverse effects of lower income on health (Ebuenyi, 2020). By enhancing public health and social interventions, African countries can still effectively fight against COVID-19 and other infectious diseases (e.g. malaria), even in the absence of effective vaccinations (Torti et al., 2020).
Ethical approval
Ethical approval was not required for this research.
Declaration of competing interests
The authors declare no conflicts of interest.
Acknowledgments
This work was supported by Darfur College (Nyala, Sudan) as well as by funds provided by the National Science Foundation (HRD-EHR #2011933) and the Office of the Provost at Howard University to M.C.C.
References
- Abena P.M., Decloedt E.H., Bottieau E., Suleman F., Adejumo P., Sam-Agudu N.A. Chloroquine and hydroxychloroquine for the prevention or treatment of COVID-19 in Africa: caution for inappropriate off-label use in healthcare settings. Am J Trop Med Hyg. 2020;102(6):1184–1188. doi: 10.4269/ajtmh.20-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Tawfiq J.A. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19) Travel Med Infect Dis. 2020;35:101608. doi: 10.1016/j.tmaid.2020.101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitiri A.R., Nyieku F.E. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon. 2018;4(11):e00931. doi: 10.1016/j.heliyon.2018.e00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berhan Y. Will Africa be devastated by Covid-19 as many predicted? Perspective and prospective. Ethiop J Health Dev. 2020;30(3):459. doi: 10.4314/ejhs.v30i3.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell M.C., Hirbo J.B., Townsend J.P., Tishkoff S.A. The peopling of the African continent and the diaspora into the new world. Curr Opin Genet Dev. 2014;29:120–132. doi: 10.1016/j.gde.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanda-Kapata P., Kapata N., Zumla A. COVID-19 and malaria: a symptom screening challenge for malaria endemic countries. Int J Infect Dis. 2020;94:151–153. doi: 10.1016/j.ijid.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibwana M.G., Jere K.C., Kamng'ona R., Mandolo J., Katunga-Phiri V., Tembo D. High SARS-CoV-2 seroprevalence in Health Care Workers but relatively low numbers of deaths in urban Malawi. medRxiv. 2020 2020.07.30.20164970. [Google Scholar]
- Coronaviridae Study Group of the International Committee on Taxonomy of V The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandara C., Dzobo K., Chirikure S. COVID-19 Pandemic and Africa: from the situation in Zimbabwe to a case for precision herbal medicine. Omics. 2020 doi: 10.1089/omi.2020.0099. [DOI] [PubMed] [Google Scholar]
- Desjardins J. Mapped: the median age of the population on every continent. Visual Capitalist. 2020 https://www.visualcapitalist.com/mapped-the-median-age-of-every-continent/ [Google Scholar]
- Diop B.Z., Ngom M., Pougué Biyong C., Pougué Biyong J.N. The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: a modelling study. BMJ Global Health. 2020;5(5):e002699. doi: 10.1136/bmjgh-2020-002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong Y.T., Wright C.G., Justman J. Antibody testing for coronavirus disease 2019: not ready for prime time. BMJ. 2020;370:m2655. doi: 10.1136/bmj.m2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaaswarkhanth M., Al Madhoun A., Al-Mulla F. Could the D614G substitution in the SARS- CoV-2 spike (S) protein be associated with higher COVID-19 mortality? Int J Infect Dis. 2020;96:459–460. doi: 10.1016/j.ijid.2020.05.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebuenyi I.D. COVID-19: an opportunity for African governments to rethink social welfare benefits and protection. Pan Afr Med J. 2020;35(2):64. doi: 10.11604/pamj.supp.2020.35.2.23875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeru A., Dejene S.W., Siya A. Short report on implications of Covid-19 and emerging zoonotic infectious diseases for pastoralists and Africa. Pastoralism. 2020;10(1):12. doi: 10.1186/s13570-020-00173-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sadr W.M., Justman J. Africa in the path of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2008193. [DOI] [PubMed] [Google Scholar]
- Ellinghaus D., Degenhardt F., Bujanda L., Buti M., Albillos A., Invernizzi P. Genomewide association study of severe Covid-19 with respiratory failure. N Engl J Med. 2020;383(16):1522–1534. doi: 10.1056/NEJMoa2020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faye C., Wade C.T., Dione I.D. A dissymmetry in the figures related to the covid-19 pandemic in the world: what factors explain the difference between Africa and the rest of the world? medRxiv. 2020 [Google Scholar]
- Ge X.Y., Li J.L., Yang X.L., Chmura A.A., Zhu G., Epstein J.H. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 2013;503(7477):535–538. doi: 10.1038/nature12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghinai I., McPherson T.D., Hunter J.C., Kirking H.L., Christiansen D., Joshi K. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020;395(10230):1137–1144. doi: 10.1016/S0140-6736(20)30607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez F., Hirbo J., Tishkoff S.A. Genetic variation and adaptation in Africa: implications for human evolution and disease. Cold Spring Harb Perspect Biol. 2014;6(7):a008524. doi: 10.1101/cshperspect.a008524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller L., Mota C.R., Greco D.B. COVID-19 faecal-oral transmission: are we asking the right questions? Sci Total Environ. 2020;729:138919. doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez A.V., Roman Y.M., Pasupuleti V., Barboza J.J., White C.M. Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review. Ann Intern Med. 2020 doi: 10.7326/M20-2496. [DOI] [PubMed] [Google Scholar]
- International Organization for Migration IOM steps up risk communication and community engagement in response to COVID-19 in West and Central Africa. Afr Renewal. 2020 https://www.un.org/africarenewal/news/coronavirus/iom-steps-risk-communication-and-community-engagement-response-covid-19-west-and-central-africa [Google Scholar]
- Jayaweera M., Perera H., Gunawardana B., Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res. 2020;188:109819. doi: 10.1016/j.envres.2020.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins . 2020. Center for Systems Science and Engineering (CSSE) Coronavirus COVID-19 Global Cases (dashboard)https://coronavirus.jhu.edu/map.html [Google Scholar]
- Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- Kavanagh M.M., Erondu N.A., Tomori O., Dzau V.J., Okiro E.A., Maleche A. Access to lifesaving medical resources for African countries: COVID- 19 testing and response, ethics, and politics. Lancet. 2020;395(10238):1735–1738. doi: 10.1016/S0140-6736(20)31093-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko W.Y., Kaercher K.A., Giombini E., Marcatili P., Froment A., Ibrahim M. Effects of natural selection and gene conversion on the evolution of human glycophorins coding for MNS blood polymorphisms in malaria-endemic African populations. Am J Hum Genet. 2011;88(6):741–754. doi: 10.1016/j.ajhg.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko W.Y., Rajan P., Gomez F., Scheinfeldt L., An P., Winkler C.A. Identifying Darwinian selection acting on different human APOL1 variants among diverse African populations. Am J Hum Genet. 2013;93(1):54–66. doi: 10.1016/j.ajhg.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondō K. Trans Pacific Press; Australia: 2010. Health Inequalities in Japan: an empirical study of older people. [Google Scholar]
- Kusotera T., Nhengu T.G. Coronavirus-19 and malaria: the great mimics. Afr J Prim Health Care Fam Med. 2020;12(1):e1–e3. doi: 10.4102/phcfm.v12i1.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche A. Refugees International; 2020. Mounting hunger in the Sahel: the unintended impact of COVID-19 prevention.https://www.refugeesinternational.org/reports/2020/6/8/mounting-hunger-in-the-sahel-the-unintended-impact-of-covid-19-prevention [Google Scholar]
- Leffler E.M., Band G., Busby G.B.J., Kivinen K., Le Q.S., Clarke G.M. Resistance to malaria through structural variation of red blood cell invasion receptors. Science. 2017 doi: 10.1126/science.aam6393. eaam6393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Liu S.M., Yu X.H., Tang S.L., Tang C.K. Coronavirus disease 2019 (COVID-19): current status and future perspectives. Int J Antimicrob Agents. 2020;55(5):105951. doi: 10.1016/j.ijantimicag.2020.105951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N., Saville M., Hatchett R., Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. 2020;382(21):1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- Marmor M., Hertzmark K., Thomas S.M., Halkitis P.N., Vogler M. Resistance to HIV infection. J Urban Health. 2006;83(1):5–17. doi: 10.1007/s11524-005-9003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massinga Loembé M., Tshangela A., Salyer S.J., Varma J.K., Ouma A.E.O., Nkengasong J.N. COVID-19 in Africa: the spread and response. Nat Med. 2020;26(7):999–1003. doi: 10.1038/s41591-020-0961-x. [DOI] [PubMed] [Google Scholar]
- Meyerowitz E.A., Vannier A.G.L., Friesen M.G.N., Schoenfeld S., Gelfand J.A., Callahan M.V. Rethinking the role of hydroxychloroquine in the treatment of COVID-19. FASEB J. 2020;34(5):6027–6037. doi: 10.1096/fj.202000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghadas S.M., Fitzpatrick M.C., Sah P., Pandey A., Shoukat A., Singer B.H. The implications of silent transmission for the control of COVID-19 outbreaks. Proc Natl Acad Sci. 2020;117(30):17513–17515. doi: 10.1073/pnas.2008373117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Milton D.K. It is time to address airborne transmission of COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musoke D., Boynton P., Butler C., Musoke M.B. Health seeking behaviour and challenges in utilising health facilities in Wakiso district, Uganda. Afr Health Sci. 2014;14(4):1046–1055. doi: 10.4314/ahs.v14i4.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwisongo A., Nabyonga-Orem J. Global health initiatives in Africa – governance, priorities, harmonisation and alignment. BMC Health Serv Res. 2016;16(Suppl 4):212. doi: 10.1186/s12913-016-1448-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachega J.B., Leisegang R., Kallay O., Mills E.J., Zumla A., Lester R.T. Mobile health technology for enhancing the COVID-19 response in Africa: a potential game changer? Am J Trop Med Hyg. 2020;103(1):3–5. doi: 10.4269/ajtmh.20-0506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkengasong J. Let Africa into the market for COVID-19 diagnostics. Nature. 2020;580:565. doi: 10.1038/d41586-020-01265-0. [DOI] [PubMed] [Google Scholar]
- Nordling L. Africa’s pandemic puzzle: why so few cases and deaths? Science. 2020;369(6505):756. doi: 10.1126/science.369.6505.756. [DOI] [PubMed] [Google Scholar]
- Pachetti M., Marini B., Benedetti F., Giudici F., Mauro E., Storici P. Emerging SARS-CoV-2 mutation hot spots include a novel RNA-dependent-RNA polymerase variant. J Transl Med. 2020;18(1):179. doi: 10.1186/s12967-020-02344-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal M., Berhanu G., Desalegn C., Kandi V. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): an update. Cureus. 2020;12(3):e7423. doi: 10.7759/cureus.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrakis D., Margina D., Tsarouhas K., Tekos F., Stan M., Nikitovic D. Obesity a risk factor for increased COVID19 prevalence, severity and lethality (Review) Mol Med Rep. 2020;22(1):9–19. doi: 10.3892/mmr.2020.11127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering A.J., Boehm A.B., Mwanjali M., Davis J. Efficacy of waterless hand hygiene compared with handwashing with soap: a field study in Dar es Salaam, Tanzania. Am J Trop Med Hyg. 2010;82(2):270–278. doi: 10.4269/ajtmh.2010.09-0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quaglio G.L., Preiser W., Putoto G. COVID-19 in Africa. Public Health. 2020;185:60. doi: 10.1016/j.puhe.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renzaho A.M.N. The need for the right socio-economic and cultural fit in the COVID-19 response in Sub-Saharan Africa: examining demographic, economic political, health, and socio-cultural differentials in COVID-19 morbidity and mortality. Int J Environ Res Public Health. 2020;17(10):3445. doi: 10.3390/ijerph17103445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose S., Suri J., Brooks M., Ryan P.G. COVID-19 and citizen science: lessons learned from southern Africa. Ostrich. 2020;91(2):188–191. [Google Scholar]
- Rosenthal P.J., Breman J.G., Djimde A.A., John C.C., Kamya M.R., Leke R.G.F. COVID-19: shining the light on Africa. Am J Trop Med Hyg. 2020;102(6):1145–1148. doi: 10.4269/ajtmh.20-0380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senghore M., Savi M.K., Gnangnon B., Hanage W.P., Okeke I.N. Leveraging Africa’s preparedness towards the next phase of the COVID-19 pandemic. Lancet Global Health. 2020;8(7):e884–e885. doi: 10.1016/S2214-109X(20)30234-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shey M., Okeibunor J.C., Yahaya A.A., Herring B.L., Tomori O., Coulibaly S.O. Genome sequencing and the diagnosis of novel coronavirus (SARS-COV-2) in Africa: how far are we? Pan Afr Med J. 2020;36:80. doi: 10.11604/pamj.2020.36.80.23723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh P.K. World Health Organzation; 2020. Promote hand hygiene to save lives and combat COVID-19.https://www.who.int/southeastasia/news/detail/04-05-2020-promote-hand-hygiene-to-save-lives-and-combat-covid-19 [Google Scholar]
- Songok E.M., Luo M., Liang B., McLaren P., Kaefer N., Apidi W. Microarray analysis of HIV resistant female sex workers reveal a gene expression signature pattern reminiscent of a lowered immune activation state. PLoS One. 2012;7(1):e30048. doi: 10.1371/journal.pone.0030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava N., Baxi P., Ratho R.K., Saxena S.K. Coronavirus Disease 2019 (COVID-19) 2020. Global Trends in Epidemiology of Coronavirus Disease 2019 (COVID-19) pp. 9–21. [Google Scholar]
- Telenti A., Goldstein D.B. Genomics meets HIV-1. Nat Rev Microbiol. 2006;4(11):865–873. doi: 10.1038/nrmicro1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanh Le T., Andreadakis Z., Kumar A., Gomez Roman R., Tollefsen S., Saville M. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(5):305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- The Lancet Editorial COVID-19 in Africa: no room for complacency. Lancet. 2020;395:1669. doi: 10.1016/S0140-6736(20)31237-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomescu C., Abdulhaqq S., Montaner L.J. Evidence for the innate immune response as a correlate of protection in human immunodeficiency virus (HIV)-1 highly exposed seronegative subjects (HESN) Clin Exp Immunol. 2011;164(2):158–169. doi: 10.1111/j.1365-2249.2011.04379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torti C., Mazzitelli M., Trecarichi E.M., Darius O. Potential implications of SARS-CoV-2 epidemic in Africa: where are we going from now? BMC Infect Dis. 2020;20(1):412. doi: 10.1186/s12879-020-05147-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y.C. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020;14(4):3822–3835. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- Uyoga S., Adetifa I.M.O., Karanja H.K., Nyagwange J., Tuju J., Wanjiku P. Seroprevalence of anti?SARS-CoV -2 IgG antibodies in Kenyan blood donors. Science. 2020 doi: 10.1126/science.abe1916. eabe1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent M.J., Bergeron E., Benjannet S., Erickson B.R., Rollin P.E., Ksiazek T.G. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2005;2:69. doi: 10.1186/1743-422X-2-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitti J.J., Grossman S.R., Sabeti P.C. Detecting natural selection in genomic data. Annu Rev Genet. 2013;47:97–120. doi: 10.1146/annurev-genet-111212-133526. [DOI] [PubMed] [Google Scholar]
- Vogels C.B.F., Brackney D., Wang J., Kalinich C.C., Ott I., Kudo E. SalivaDirect: Simple and sensitive molecular diagnostic test for SARS-CoV -2 surveillance. medRxiv. 2020 [Google Scholar]
- Wild S. African countries scramble to ramp up testing for African countries scramble to ramp up testing for COVID-19. Sci Am. 2020 https://www.scientificamerican.com/article/african-countries-scramble-to-ramp-up-testing-for-covid-19/ [Google Scholar]
- Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Coronavirus disease 2019 (COVID-19) situation report—29. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200218-sitrep-29-covid-19.pdf?sfvrsn=6262de9e_2, 2020.
- WorldoMeter . 2020. COVID-19 Coronovirus pandemic.https://www.worldometers.info/coronavirus/ [Google Scholar]
- Wyllie A.L., Fournier J., Casanovas-Massana A., Campbell M., Tokuyama M., Vijayakumar P. Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N Engl J Med. 2020;383(13):1283–1286. doi: 10.1056/NEJMc2016359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie M., Chen Q. Insight into 2019 novel coronavirus — an updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis. 2020;94:119–124. doi: 10.1016/j.ijid.2020.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Chen P., Wang J., Feng J., Zhou H., Li X. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao T.T., Qian J.D., Zhu W.Y., Wang Y., Wang G.Q. A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus-A possible reference for coronavirus disease-19 treatment option. J Med Virol. 2020;92(6):556–563. doi: 10.1002/jmv.25729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao X.D., Omange R.W., Henrick B.M., Lester R.T., Kimani J., Ball T.B. Acting locally: innate mucosal immunity in resistance to HIV-1 infection in Kenyan commercial sex workers. Mucosal Immunol. 2014;7(2):268–279. doi: 10.1038/mi.2013.44. [DOI] [PubMed] [Google Scholar]
- Yeung P. Senegal to trial $1 speedy test for covid-19. New Sci. 2020;246(3282):13. doi: 10.1016/S0262-4079(20)30914-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeberg H., Pääbo S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature. 2020;587(7835):610–612. doi: 10.1038/s41586-020-2818-3. [DOI] [PubMed] [Google Scholar]
- Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]