Abstract
Purpose
We evaluated whether the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) pandemic was associated with changes in the pattern of acute cardiovascular admissions across European centers.
Methods
We set-up a multicenter, multinational, pan-European observational registry in 15 centers from 12 countries. All consecutive acute admissions to emergency departments and cardiology departments throughout a 1-month period during the COVID-19 outbreak were compared with an equivalent 1-month period in 2019. The acute admissions to cardiology departments were classified into 5 major categories: acute coronary syndrome, acute heart failure, arrhythmia, pulmonary embolism, and other.
Results
Data from 54,331 patients were collected and analyzed. Nine centers provided data on acute admissions to emergency departments comprising 50,384 patients: 20,226 in 2020 compared with 30,158 in 2019 (incidence rate ratio [IRR] with 95% confidence interval [95%CI]: 0.66 [0.58-0.76]). The risk of death at the emergency departments was higher in 2020 compared to 2019 (odds ratio [OR] with 95% CI: 4.1 [3.0-5.8], P < 0.0001). All 15 centers provided data on acute cardiology departments admissions: 3007 patients in 2020 and 4452 in 2019; IRR (95% CI): 0.68 (0.64-0.71). In 2020, there were fewer admissions with IRR (95% CI): acute coronary syndrome: 0.68 (0.63-0.73); acute heart failure: 0.65 (0.58-0.74); arrhythmia: 0.66 (0.60-0.72); and other: 0.68(0.62-0.76). We found a relatively higher percentage of pulmonary embolism admissions in 2020: odds ratio (95% CI): 1.5 (1.1-2.1), P = 0.02. Among patients with acute coronary syndrome, there were fewer admissions with unstable angina: 0.79 (0.66-0.94); non-ST segment elevation myocardial infarction: 0.56 (0.50-0.64); and ST-segment elevation myocardial infarction: 0.78 (0.68-0.89).
Conclusion
In the European centers during the COVID-19 outbreak, there were fewer acute cardiovascular admissions. Also, fewer patients were admitted to the emergency departments with 4 times higher death risk at the emergency departments.
Keywords: Acute cardiovascular admissions, Acute coronary syndrome, COVID-19, Outbreak, SARS-CoV2
Clinical Significance.
-
•
In European centers during the COVID-19 outbreak fewer patients were admitted to the emergency departments.
-
•
Patients presented at emergency departments had higher risk of death in 2020 compared with the same period in 2019.
-
•
There was also a significant decrease in acute admissions to the cardiology departments during the COVID-19 outbreak.
-
•
Patients admitted to the cardiology departments were younger and had shorter length of in-hospital stay.
Alt-text: Unlabelled box
Introduction
Rapid outbreak of new coronavirus disease (COVID-19) has substantially changed the health care systems in all countries across the globe, which mainly have focused on pandemic as a state of emergency, according to the declaration of the World Health Organization (WHO) on January 30, 2020. Strict restrictions have been imposed, and millions of people remained at home to minimize severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) transmission. Planned hospital admissions and outpatient visits are either limited or canceled.1 In many countries, there has also been a significant decrease in acute admissions to cardiology departments.2, 3, 4, 5, 6 The limited access to public medical care, fear of infection of SARS-CoV-2, and reorganization of medical services may have an impact on the number and profile of patients admitted to cardiology departments but also those presenting to emergency departments with subsequent changes in the outcomes.7, 8, 9 The aim of this study was to present the pan-European data regarding the effects of the COVID-19 pandemic on the pattern of acute cardiovascular admissions across European centers in the countries affected by the disease.
Methods
Study Design
A multicenter, multinational (pan-European) observational registry was set up. All consecutive acute admissions to the emergency and cardiology departments throughout a 1-month period during the COVID-19 outbreak were retrospectively collected. This period differed across participating European countries depending on the “peak month” of SARS-CoV-2 infection at a particular center (decision which period to select was left at the discretion of the investigator) but was limited to a period between March 1 and April 30, 2020. The data was compared with the corresponding period of 1 month in the year 2019.
Fifteen centers from 12 countries participated in the registry. All 15 centers delivered data on the acute admissions to the cardiology departments, and 9 centers provided data on acute admissions to the emergency departments and, subsequently, to cardiology departments. The sample size was determined by the time window of the study. The following information was collected in patients presenting to the emergency departments: sex, age, result of reverse transcription-polymerase chain reaction tests from an upper airway swab for SARS-CoV-2 (if available), discharge status (categorized into admitted to the cardiology departments or discharged/transferred to noncardiac department or death at the emergency departments).
For those admitted to the cardiology departments, we collected additional information on major primary diagnosis, which was classified into major 5 categories: acute coronary syndrome, acute heart failure, arrhythmia, pulmonary embolism, and other. For several diagnoses in a patient, priority was given for pulmonary embolism > acute coronary syndrome > acute heart failure > arrhythmia. Other was chosen when none from prespecified diagnoses was indicated.
The information on length of hospital stay and on in-hospital deaths was also collected.
Patients admitted with a diagnosis of acute coronary syndrome were classified as those with unstable angina, non-ST segment elevation myocardial infarction (NSTEMI), or ST-segment elevation myocardial infarction (STEMI); types of arrhythmia admissions included atrial, ventricular, or heart blocks and bradycardia. Collecting information about the different categories of acute coronary syndrome and arrhythmia was optional.
Data were retrospectively obtained in individual centers from their own clinical databases using the data form provided by the coordinating center (Medical University, Wroclaw, Poland). The final database was double-checked for missing or potentially incorrect entries. In each center, the principal investigator took full responsibility for the accuracy and quality of the data. The study protocol was approved by the local ethics committee and was conducted in accordance with the Declaration of Helsinki.10
Acute coronary syndrome was defined in accordance with the Fourth Universal Definition of Myocardial Infarction,11 and heart failure was diagnosed based on the guidelines for the diagnosis and treatment of acute and chronic heart failure.12 Atrial arrhythmias included atrial fibrillation, atrial flutter, tachycardia with narrow QRS, and supraventricular tachycardia with wide QRS.13 Ventricular arrhythmias included ventricular fibrillation and ventricular tachycardia.14 Bradycardia was recognized when symptomatic, including heart blocks (second- and third-degree blocks). Pulmonary embolism was confirmed according to the guidelines of acute pulmonary embolism.15
Outcomes
The outcomes measures were:
-
a.
The number of acute admissions to the emergency and cardiology departments.
-
b.
For patients admitted to the emergency departments: death at the emergency departments, transfer to cardiology departments, or discharge or transfer to a noncardiac department.
-
c.
For patients admitted to the cardiology departments: in-hospital mortality and duration of hospital stay in patients discharged home.
Statistical Analysis
Normally distributed continuous variables were presented as means with or without standard deviations. The intergroup differences were tested using Student t-test and the Mann-Whitney U test. Variables with a skewed distribution were expressed as medians with lower and upper quartiles. The categorical variables were expressed as numbers with percentages. The intergroup differences were tested using the χ2 test. The associations between death and risk factors were tested using univariable and multivariable logistic regression models. To estimate odds ratios (ORs) with 95% confidence interval (95% CI), a logistic regression was applied with a “successes/failures” matrix to produce the correct binomial denominator. The independent variables were the year of the hospitalization (2019 year as a reference), age ≥ 65 years old, male gender, presence of SARS-CoV-2 infection, and death was a dependent variable. The multivariable model included variables that were statistically significant associated in univariable models and remained statistically significant also in a multivariable. To model incidence rate ratio (IRR) and 95% CI between the periods, the negative binomial regression was used. Additionally, to compare the estimated IRRs among the study centers, we performed a meta-analysis. Poisson process was involved to figure out the duration of hospitalization (waiting time) in cardiology departments and home discharge. Allowing for greater dispersion or variance of times, the negative binomial distribution was assumed for response data. The difference of duration of hospitalization between 2020 study period and 2019 intrayear control period was expressed by a rate ratio (RR). A value of P < 0.05 was considered as statistically significant. Statistical analysis was performed using the STATISTICA 13.3 data analysis software system (StatSoft, Inc.) and in R statistical platform (R Core Team. R: A language and environment for statistical computing [Version 3.6.3. R Foundation for Statistical Computing, Vienna, Austria. 2020]) and “metafor,” Meta-Analysis Package for R (Version 2.4-0. CRAN, Austria).
Results
Fifteen cardiac centers from 12 countries participated in the registry, and data from 54,331 consecutive patients (mean age 59 ± 20 years, 51% male) were collected and analyzed.
Patients Admitted to the Emergency Departments
Characteristics, Including SARS-CoV-2 Status in Study Group
Nine centers provided data on acute emergency departments admissions, comprising 50,384 patients. In total, there were 20,226 patients admitted to the emergency departments in 2020 versus 30,158 in 2019. The IRR (95% CI) was 0.66 (0.58-0.76). Among patients presented at the emergency departments in 2020 (vs 2019), there were more men: 10,748 (53%) versus 14,593 (48%) and fewer patients older than 65 years: 8022 (40%) versus 12,994 (43%), all P < 0.0001. There was no difference in out of hospital cardiac arrest as cause of admission: 40 (0.24%) versus 46 (0.18%), P = 0.23.
During the study period, 7476 (37%) of all patients were evaluated for the presence of SARS-CoV-2 infection and in 4168 (21%) COVID-19 was confirmed. Those patients were older (65 ± 15 vs 56 ± 20 years), older than 65 years old: 2132 (51%) versus 5890 (37%), and were more often males: 2604 (62%) 8144 (51%) (all P < 0.0001), when compared with patients without suspicion and with negative test for SARS-CoV-2. Moreover, patients with confirmed COVID-19 had lower mortality at emergency departments: 11 (0.26%) versus 119 (0.74%), OR (95% CI) 2.8 (1.5-5.2), P < 0.001, and almost all were transferred to noncardiac departments or discharged: 4111 (99%) versus 14557 (91%), P < 0.0001 in comparison to the group without suspicion and with negative test for SARS-CoV-2.
Outcomes
The rate of death at the emergency departments was significantly higher in 2020 compared with 2019 with 130 (0.64 %) deaths in 2020 versus 48 (0.16%) deaths in 2019 (IRR [95% CI]: 2.7 [1.94-3.77], P < 0.0001). In the logistic multivariable regression model for all patients hospitalized at the emergency departments, the year of the hospitalization 2020, age ≥ 65 years old, and male gender were associated with an increased risk of all-cause death (OR [95% CI]: 4.1 [3.0-5.8], P < 0.0001, 7.1 [4.8-10.5], P < 0.0001 and 1.8 [1.3-2.4], P = 0.0001, respectively).
The percentage of patients transferred from the emergency departments to the cardiology departments was similar: 1427 (7.1%) versus 2085 (6.9%) (2020 vs 2019, respectively), P = 0.54, and IRR (95% CI): 0.68 (0.64-0.73).
Patients Admitted to the Cardiology Departments
Characteristics and Pattern of Clinical Diagnoses
All 15 centers provided data on acute admissions to cardiology departments. There were 3007 patients admitted to cardiology departments in 2020 versus 4452 in 2019, respectively (IRR [95% CI]: 0.68 [0.64-0.71]).
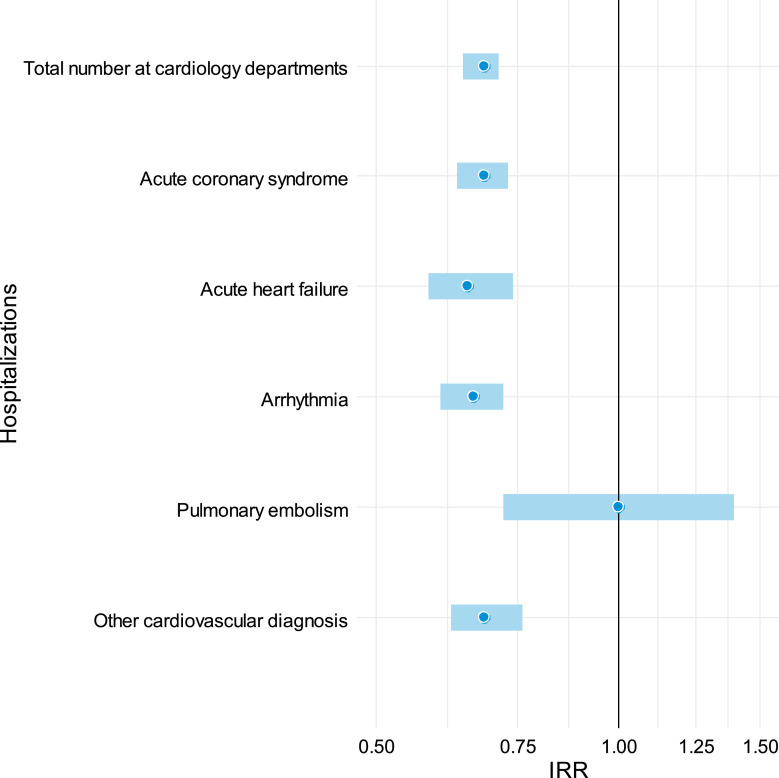
Patients admitted in 2020 were younger: ≥65 years 1842 (61%) versus 2871 (64 %) in 2020 compared to 2019, respectively, P < 0.001. There was no difference in gender: males 1928 (64%) versus 2370 (64%), P = 0.63. There were fewer admissions across the following 4 categories with IRR (95% CI): acute coronary syndrome: 0.68 (0.63-0.73); acute heart failure: 0.65 (0.58-0.74); arrhythmia: 0.66 (0.60-0.72); other: 0.68 (0.62-0.76), and all P<0.0001. There was no difference only for pulmonary embolism, IRR (95% CI): 1.00 (0.72-1.39) (Table 1 , Figure 1 ), which resulted in a relatively higher percentage of patients admitted with pulmonary embolism in 2020: 71 (2.4%) in 2020 versus 71 (1.6%) in 2019 (OR [95%CI]: 1.49 (1.07-2.08), P = 0.02) (Table 2 ).
Table 1.
Comparison of Patients Numbers and Primary Cause of Admission at Cardiology Departments Between the Study Period (2020) and the Control Period (2019)
| All, n | Study Period, 2020 | Control Period, 2019 | |
|---|---|---|---|
| Acute coronary syndrome, n IRR (95% CI) |
2803 | 1132 | 1671 |
| 0.68 (0.63-0.73) | |||
| Acute heart failure, n IRR (95% CI) |
1137 | 450 | 687 |
| 0.65 (0.58-0.74) | |||
| Arrhythmia, n IRR (95% CI) |
1992 | 790 | 1202 |
| 0.66 (0.60-0.72) | |||
| Pulmonary embolism, n IRR (95% CI) |
142 | 71 | 71 |
| 1.00 (0.72-1.39) | |||
| Other, n IRR (95% CI) |
1379 | 564 | 821 |
| 0.68 (0.62-0.76) | |||
IRR = incident rate ratio; 95% CI = 95% confidence interval.
Figure 1.
Forest plots showing the incidence rate ratios of the primary causes of hospitalization between the study period (2020) and the control period (2019).
Table 2.
Comparison of Patient Profiles at Cardiology Departments Between the Study Period (2020) and the Control Period (2019)
| All | Study Period, 2020 | Control Period, 2019 | OR (95% CI) | P | |
|---|---|---|---|---|---|
| Demography | |||||
| Gender, male, n (%) | 4774 (64) | 1928 (64) | 2846 (64) | 1.01 (0.97-1.04) | 0.63 |
| Age ≥65 years, n (%) | 4714 (63) | 1842 (61) | 2871 (64) | 0.87 (0.79-0.96) | <0.01 |
| Cause of Admission | |||||
| Acute coronary syndrome, n (%) | 2803 (37) | 1132 (38) | 1671 (38) | 1.00 (0.95-1.05) | 0.88 |
| Acute heart failure, n (%) | 1137 (15) | 450 (15) | 687 (15) | 0.96 (0.86-1.08) | 0.52 |
| Arrhythmia, n (%) | 1992 (27) | 790 (26) | 1202 (27) | 0.96 (0.87-1.07) | 0.47 |
| Pulmonary embolism, n (%) | 142 (1.9) | 71 (2.3) | 71 (1.6) | 1.49 (1.07-2.08) | 0.02 |
| Other, n (%) | 1379 (19) | 564 (19) | 821 (18) | 1.02 (0.90-1.15) | 0.74 |
IRR = incident rate ratio; 95% CI = 95% confidence interval; OR = odds ratio.
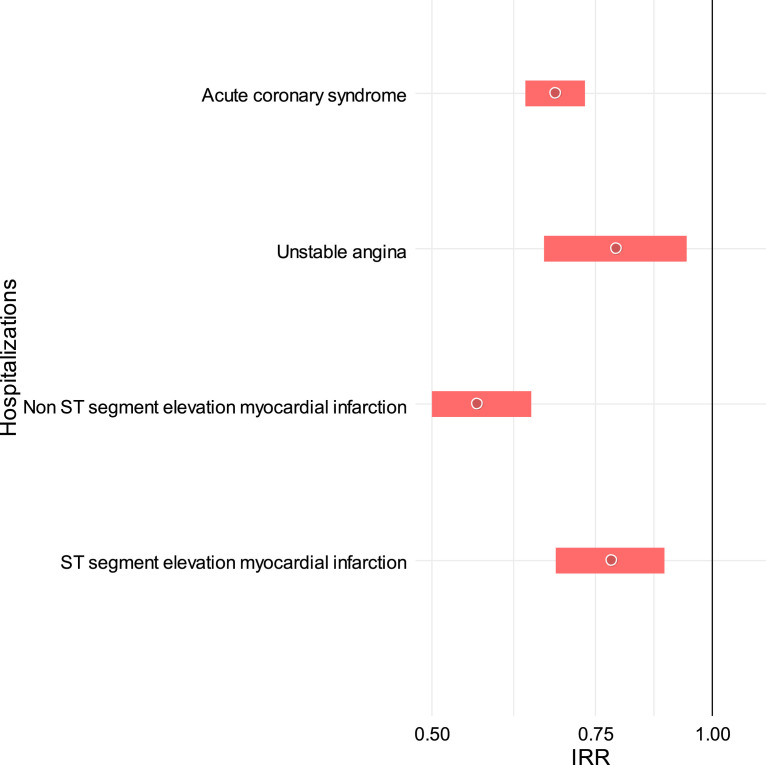
There were fewer admissions in all 3 categories of acute coronary syndrome with IRR (95% CI) for unstable angina: 0.79 (0.66-0.94), P < 0.01; for NSTEMI: 0.56 (0.50-0.64), P < 0.0001; and STEMI: 0.78 (0.68-0.89), P < 0.001, respectively. However if analyzed as percentage of all acute coronary syndrome admissions in 2020, unstable angina constituted for 21%, NSTEMI for 41%, and STEMI for 37%, whereas in 2019 unstable angina constituted for 18%, NSTEMI for 49%, and STEMI for 32%, resulting in a relatively lower percentage of NSTEMI and higher percentage of STEMI in 2020 (Table 3 , Figure 2 ).
Table 3.
Comparison of Acute Coronary Syndrome Categories Between the Study Period (2020) and the Control Period (2019)
| All, n (%) | Study Period, 2020 | Control Period, 2019 | OR (95% CI) | P | |
|---|---|---|---|---|---|
| Acute Coronary Syndrome | |||||
| Unstable angina, n (%) IRR (95% CI) |
479 (19) | 211 (21) | 268 (18) | 1.21 (0.99-1.48) | 0.06 |
| 0.79 (0.66-0.94) | |||||
| NSTEMI, n (%) IRR (95% CI) |
1126 (46) | 406 (41) | 720 (49) | 0.72 (0.61-0.85) | <0.0001 |
| 0.56 (0.50-0.64) | |||||
| STEMI, n (%) IRR (95% CI) |
841 (34) | 368 (37) | 473 (32) | 1.24 (1.05-1.48) | 0.01 |
| 0.78 (0.68-0.89) | |||||
IRR = incident rate ratio; 95%CI = 95% confidence interval; NSTEMI = non-ST segment elevation myocardial infarction; STEMI = ST elevation myocardial infarction.
Figure 2.
Forest plots showing the incidence rate ratios of acute coronary syndrome categories between the study period (2020) and the control period (2019).
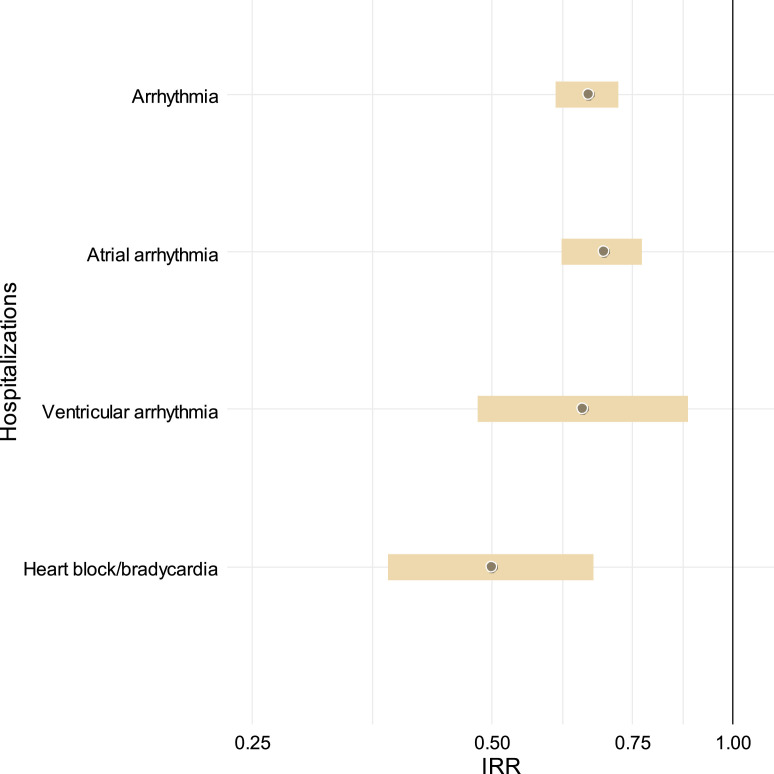
There was a reduction in admissions of all 3 groups admitted with a primary diagnosis of arrhythmia: IRR (95%CI) for atrial arrhythmias: 0.69 (0.6-0.77), P < 0.0001; for ventricular arrhythmias: 0.65 (0.48-0.88), P < 0.01; and for bradycardia/heart atrioventricular blocks: 0.50 (0.37-0.67), P < 0.0001, respectively. There was a relative decrease in the percentage of bradycardia/heart atrioventricular blocks: 11% in 2020 versus 14% in 2019, OR (95% CI): 0.73 (0.53-1.00), P < 0.05. (Table 4 , Figure 3 ).
Table 4.
Comparison of Arrhythmias Categories Between the Study Period (2020) and the Control Period (2019)
| All, n (%) | Study Period, 2020 | Control Period, 2019 | OR (95% CI) | P | |
|---|---|---|---|---|---|
| Categories of arrhythmia | |||||
| Atrial arrhythmia, n (%) IRR (95% CI) |
1193 (76) | 487 (78) | 706 (74) | 1.21 (0.96-1.54) | 0.11 |
| 0.69 (0.6-0.77) | |||||
| Ventricular arrhythmia, n (%) IRR (95% CI) |
177 (11) | 70 (11) | 107 (11) | 0.99 (0.76-1.30) | 0.96 |
| 0.65 (0.48-0.88) | |||||
| Bradycardia, AV blocks, n (%) IRR (95% CI) |
204 (13) | 68 (11) | 136 (14) | 0.73 (0.53-1.00) | <0.05 |
| 0.50 (0.37-0.67) | |||||
AV = atrioventricular; IRR = incident rate ratio; 95% CI = 95% confidence interval.
Figure 3.
Forest plots showing the incidence rate ratios of arrhythmia categories between the study period (2020) and the control period (2019).
Outcomes
There was no statistically significant difference in death rates between studied periods: 107 (3.6%) in 2020 versus 175 (3.9%) deaths in 2019: OR (95% CI) 0.92 (0.72-1.18), P = 0.57. The mean length of stay was significantly shorter in 2020 in comparison to 2019 (4.9 ± 5.0 versus 5.9 ± 7.2, P < 0.0001).
Discussion
In this pan-European study, we have shown a marked reduction in patients presenting to the emergency departments. In comparison to the last year (2019), these patients were younger and more frequently male, but the most striking finding was the much higher mortality with a 4 times higher death risk at the emergency departments during the COVID-19 outbreak, which was not related to COVID-19 directly. These findings were consistent across all countries and centers, including the 2 centers from the countries that were most severely hit by the pandemic (Madrid/Spain and Bergamo/Italy).
Numerous factors may explain the main finding (“significantly fewer presentations of patients to the emergency departments cardiology departments”). One can assume that fear of being easily infected in the hospital precluded many patients to seek medical care. Reorganization of the health service and focus on fighting the pandemic resulted in difficulties to get access to medical care. Based on the data presented, one can speculate that patients with more advanced or severe cardiovascular disease were admitted to the emergency departments, which resulted in higher risk of death. Another possible cause may be the allocation of resources, manpower, and equipment for younger patients with higher chance of survival. This illustrates a potentially worrying situation once capacities of the health care system are being challenged.
Additionally, we noted a significant decrease in acute admissions to the cardiology departments across all European countries during the COVID-19 pandemic, with a marked reduction in acute cardiovascular admissions resulting from acute coronary syndrome, acute heart failure, and arrhythmias. Of note, only pulmonary embolism was more often present during the COVID-19 outbreak. We showed that the admitted patients were younger, in-hospital stay was shorter, and in-hospital mortality was similar compared to the control period (2019). The interesting aspect is shortening of length of stay because of the possible modification of therapeutic aims at minimizing the hospitalization time. Moreover, the total number of acute coronary syndrome admissions was reduced by more than 30% (homogenous across all centers), with a reduction in NSTEMI (or unstable angina) but an increase in STEMI. Patients presenting with STEMI are more symptomatic and tend to seek for medical care faster as compared to NSTEMI and unstable angina, which possibly explains these differences. In addition, less physical activity may have masked symptoms. However, less activity may increase the risk of thromboembolism, potentially responsible for the higher percentage of pulmonary embolism, together with COVID-19, incidence. This is an important implication for the health care system and signal for early modification of the prophylactic and therapeutic aims in the pandemic period.
Conclusion
This pan-European study shows that during the COVID-19 outbreak, there was a significant decrease in acute admissions to the cardiology departments. Patients admitted were younger and had shorter stays in the hospital; there was similar in-hospital mortality compared with 2019. Additionally, fewer patients were admitted to the emergency departments, with 4 times higher death rates.
Footnotes
Funding: None.
Conflicts of Interest: None.
Authorship: All authors had access to the data and a role in writing this manuscript.
References
- 1.European Centre for Disease Prevention and Control . European Centre for Disease Prevention and Control; Stockholm, Sweden: 2020. Guidance for health system contingency planning during widespread transmission of SARS-CoV-2 with high impact on healthcare services. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-guidance-health-systems-contingency-planning.pdf. Accessed July 25, 2020. [Google Scholar]
- 2.Rosa S De, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huet F, Prieur C, Schurtz G, et al. One train may hide another: acute cardiovascular diseases could be neglected because of the COVID-19 pandemic. Arch Cardiovasc Dis. 2020;113:303–307. doi: 10.1016/j.acvd.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol. 2020;2:82–89. doi: 10.24875/RECICE.M20000123. [DOI] [Google Scholar]
- 7.Baldi E, Sechi GM, Mare C, et al. Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sokolski M, Sokolska JM, Zymlinski R, et al. Cardiac emergencies during the COVID-19 pandemic in the light of the current evidence. Kardiol Pol. 2020;78:818–824. doi: 10.33963/KP.15516. [DOI] [PubMed] [Google Scholar]
- 10.Rickham PP. Human experimentation. Code of ethics of the world medical association. Declaration of Helsinki. Br Med J. 1964;2:177. doi: 10.1136/bmj.2.5402.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018) J Am Coll Cardiol. 2018;72:2231–2264. doi: 10.1016/j.gheart.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 13.Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC guidelines for the management of patients with supraventricular tachycardia: the task force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC) Eur Heart J. 2020;41:655–720. doi: 10.1093/eurheartj/ehz467. [DOI] [PubMed] [Google Scholar]
- 14.Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC) Eur Heart J. 2015;36:2793–2867. doi: 10.1093/eurheartj/ehv316. [DOI] [PubMed] [Google Scholar]
- 15.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur Respir J. 2019;54 doi: 10.1093/eurheartj/ehz405. [DOI] [PubMed] [Google Scholar]