Abstract
Background
The acute nature of COVID-19 and its effects on society in terms of social distancing and quarantine regulations affect the provision of palliative care for people with dementia who live in long-term care facilities. The current COVID-19 pandemic poses a challenge to nursing staff, who are in a key position to provide high-quality palliative care for people with dementia and their families.
Objective
To formulate practice recommendations for nursing staff with regard to providing palliative dementia care in times of COVID-19.
Design and method
A rapid scoping review following guidelines from the Joanna Briggs Institute. Eligible papers focused on COVID-19 in combination with palliative care for older people or people with dementia and informed practical nursing recommendations for long-term care facilities. After data extraction, we formulated recommendations covering essential domains in palliative care adapted from the National Consensus Project's Clinical Practice Guidelines for Quality Palliative Care.
Data sources
We searched the bibliographic databases of PubMed, CINAHL and PsycINFO for academic publications. We searched for grey literature using the search engine Google. Moreover, we included relevant letters and editorials, guidelines, web articles and policy papers published by knowledge and professional institutes or associations in dementia and palliative care.
Results
In total, 23 documents (7 (special) articles in peer-reviewed journals, 6 guides, 4 letters to editors, 2 web articles (blogs), 2 reports, a correspondence paper and a position paper) were included. The highest number of papers informed recommendations under the domains ‘advance care planning’ and ‘psychological aspects of care’. The lowest number of papers informed the domains ‘ethical care’, ‘care of the dying’, ‘spiritual care’ and ‘bereavement care’. We found no papers that informed the ‘cultural aspects of care’ domain.
Conclusion
Literature that focuses specifically on palliative care for people with dementia in long-term care facilities during the COVID-19 pandemic is still largely lacking. Particular challenges that need addressing involve care of the dying and the bereaved, and ethical, cultural and spiritual aspects of care. Moreover, we must acknowledge grief and moral distress among nursing staff. Nursing leadership is needed to safeguard the quality of care and nursing staff should work together within an interprofessional care team to initiate advance care planning conversations in a timely manner, to review and document advance care plans, and to adapt goals of care as they may change due to the COVID-19 situation.
Tweetable abstract: The current COVID-19 pandemic affects people living with dementia, their families and their professional caregivers. This rapid scoping review searched for academic and grey literature to formulate practical recommendations for nursing staff working in long-term care facilities on how to provide palliative care for people with dementia in times of COVID-19. There is a particular need for grief and bereavement support and we must acknowledge grief and moral distress among nursing staff. This review exposes practice and knowledge gaps in the response to COVID-19 that reflect the longstanding neglect and weaknesses of palliative care in the long-term care sector. Nursing leadership is needed to safeguard the quality of palliative care, interprofessional collaboration and peer support among nursing staff.
Keywords: COVID-19, Dementia, Long-term care facilities, Nursing, Palliative care, Recommendations
What is already known about the topic?
-
•
Palliative care for people with dementia is complex and involves responding to physical, psychological, social and spiritual needs, discussing wishes and care preferences, and supporting families before and after bereavement.
-
•
Nursing staff working in long-term care facilities have a key role in providing person-centered and compassionate palliative care.
-
•
Ideally, palliative care should be in place in times of humanitarian crises or pandemics to meet end-of-life care needs and to facilitate a peaceful death.
What this paper adds
-
•
The global response to the COVID-19 pandemic regarding palliative care for people with dementia reflects the longstanding neglect and weaknesses of palliative care in the long-term care sector. This paper formulates practical nursing recommendations based on 23 documents to inform palliative dementia care during this crisis.
-
•
The unprecedented COVID-19 situation raises a particular need for grief and bereavement care to mitigate adverse outcomes such as complicated grief and trauma. Moreover, we need to acknowledge grief experiences and moral distress in nursing staff.
-
•
The pandemic emphasizes the need for nursing leadership to safeguard the quality of palliative care, to establish effective interprofessional collaboration and to maintain a peer support system among nursing staff members.
1. Introduction
In recognition of the global outbreak of COVID-19, the World Health Organization (WHO) declared a COVID-19 pandemic on March 11, 2020 (World Health Organization, 2020). The world population is at risk due to the rapid spread of the virus. As of July 15th, over 580,000 deaths have been reported from 215 countries (Worldometers, 2020). The case fatality rate is highest among frail older adults (Onder et al., 2020; Shams et al., 2020). Current estimates of the case fatality rate from COVID-19 are below 0.2% for people aged under 60, and up to 9.3% among people aged over 80 years (Ferguson et al., 2020). Older people with dementia are generally frail and they are more likely to have comorbid conditions such as cardiovascular disease, diabetes and pneumonia compared to older individuals without dementia (Bauer et al., 2014). Hence, they constitute a particularly vulnerable group that is at risk for negative health outcomes of COVID-19 (Clarfield et al., 2020). The population of people living with dementia is expected to show more severe illness and higher mortality as a result of COVID-19, due to their comorbidities and other characteristics of dementia (Brown et al., 2020). Even as an independent risk factor, Atkins and colleagues found that pre-existing dementia was the strongest risk diagnosis for developing severe symptoms of COVID-19 in community-dwelling adults aged over 65 (Atkins et al., 2020). Although this may be different for older people living in facilities, once a virus enters a facility, it is difficult to control and likely to spread rapidly (Gardner et al., 2020). Residents with dementia may be more at risk of contracting and transmitting COVID-19 resulting from difficulties to understand and remember infection prevention regulations such as isolation, social distancing and general hygiene regulations such as hand sanitizing (Brown et al., 2020; Livingston et al., 2020).
In most western countries, the majority of people living in long-term care facilities have some form of dementia (Doupe et al., 2011; Froggatt et al., 2016; Seitz et al., 2010). The institutional nature of long-term care facilities facilitates the spread of the virus and adds to the risk of COVID-19 among residents (Clarfield et al., 2020). The double challenge of dementia combined with the COVID-19 pandemic raises concerns for residents living with dementia, their families and their caregivers (Brown et al., 2020; Wang et al., 2020a). In addition to the increased risk of COVID-19, societal regulations and the organization of healthcare in response to COVID-19 affect the usual provision of care for all people with dementia living in long-term care facilities. Social distancing regulations and visiting restrictions compromise their social contacts and engagement with other residents, physical exercise and meaningful or joint activities undertaken within facilities. These changes may elicit anxiety, agitation and depression in residents with dementia, as well as loneliness, distress and confusion (Velayudhan et al., 2020). Loneliness and social isolation are linked to poorer mental and physical health outcomes and a higher mortality risk (Leigh-Hunt et al., 2017; Sutin et al., 2018). In addition, reduced sensory stimulation due to social isolation and physical distancing from others may lead to boredom, sedentary behavior or behavioral disturbances such as agitation or apathy in people with dementia (Brown et al., 2020; Kolanowski et al., 2017). Nonpharmacological treatments of neuropsychiatric behaviors such as distraction, engagement in activities or going out for a walk are more difficult to apply due to contagion prevention regulations (Canevelli et al., 2020). This may increase the risk of use of physical restraints and inadequate psychotropic medications in long-term care facilities to manage isolation and distancing regulations, particularly in the case of wandering behaviors (Canevelli et al., 2020; Velayudhan et al., 2020; Zuidema et al., 2010).
Maintaining quality of life and optimizing comfort are important goals of care for people with moderate to severe dementia (van der Steen et al., 2014). In many western countries, the most common place of death of people with dementia is a long-term care facility (Reyniers et al., 2015), which highlights the need for palliative and end-of-life care for people with dementia who live in these facilities. Palliative care aims to improve the quality of life by responding to physical, psychosocial and spiritual needs. Early end-of-life conversations and advance care planning are cornerstones of high-quality palliative care, as are the management of pain and other burdensome symptoms, the pursuit of a comfortable death, and support for families before and after bereavement (van der Steen et al., 2014). There is increasing recognition of the need for the integration of palliative care with care for people with dementia. Nonetheless, palliative care for people with dementia is challenging even in more stable circumstances. For instance, people with dementia are more likely to have unmet needs, to receive poor treatment of pain and other symptoms, to face inappropriate aggressive medical treatments and to be transferred to acute care at the end of life (Birch and Draper, 2008). Professional caregivers such as nurses and physicians report difficulties in palliative dementia care related to lacking or fragmented palliative care services, pain management, psychosocial needs and challenging behaviors, and end-of-life communication and (shared) decision-making (Bolt et al., 2019; Davies et al., 2014; Ryan et al., 2012).
During the COVID-19 pandemic, providing palliative care for long-term care residents with dementia (with or without COVID-19) is even more complex. The pandemic particularly challenges nursing staff working in long-term care, who have an important role in providing palliative care for people with dementia and their families. While they need to deliver medical and physical care to the current standard, they also need to preserve human contact, dignity and comfort for people with dementia with or without COVID-19. Physical touch and social interactions are important to enhance the wellbeing of people with severe dementia, particularly if other forms of communication become difficult (Nicholls et al., 2013). Social distancing regulations and personal protective equipment deprive people with dementia at the end of life from intimacy and being touched gently by their family members or caregivers (Lapid et al., 2020). Moreover, personal protective equipment may be frightening and confusing for people with dementia (Lapid et al., 2020; Velayudhan et al., 2020). It is particularly challenging to respond to psychological symptoms such as anxiety and depression, and to deal with challenging behaviors, as people with dementia are likely to have difficulties understanding their current situation (Velayudhan et al., 2020). Palliative care for people with dementia also involves compassionate advance care planning conversations. However, as COVID-19 unfolds rapidly and visiting of families is restricted, there may be insufficient time and occasions for elaborate and personal conversations with persons with dementia and their families (British Geriatrics Society, 2020). Families as proxy decision-makers may face difficult and ethically challenging decisions, for instance, concerning the desirability of hospitalization (Livingston et al., 2020; Moore et al., 2020a, 2020b). Overall, families must be involved in end-of-life care for people with dementia, which is hindered due to the widespread lockdown regulations in long-term care facilities (Gordon et al., 2020). Caring for a person with dementia who is dying of COVID-19 or its complications may raise additional challenges for families and nursing staff. Rapid deterioration of health and a lack of personal protective equipment in long-term care facilities may compromise family involvement in the last phase. These situations may be stressful for families and for nursing staff (Brown et al., 2020; Moore et al., 2020a, 2020b), who have often cared for a person with dementia and their family for a long period.
The current COVID-19 crisis poses multiple challenges for nursing staff, who are key professionals providing high-quality palliative care for people with dementia residing in long-term care facilities. This paper describes a rapid scoping review to inform practice recommendations for nursing staff with regard to providing palliative dementia care in long-term care facilities in times of COVID-19.
2. Methods
This rapid scoping review is part of the overarching research project ‘DEDICATED: Desired Dementia Care Towards End of Life’. The goal of DEDICATED is to improve palliative care for people with dementia and their families. To structure this review, we used the framework proposed by the Joanna Briggs Institute (Peters et al., 2015). The framework builds upon the original framework for scoping reviews by Arksey and O'Malley (2005), taking into account earlier enhancements by Levac et al. (2010). Thereby, the Joanna Briggs Institute's framework provides a detailed and explicit description for conducting systematic and rigorous scoping reviews. It is a leading source for guiding the conduct of scoping reviews (Lockwood et al., 2019) and it informed the development of the PRISMA Extension for Scoping Reviews checklist (Tricco et al., 2018).
2.1. Search strategy
We performed weekly literature searches between April and May 2020, with a last search on May 18th. The search strategy included four steps, following the Joanna Briggs Institute manual (Peters et al., 2015). In step one, we searched the databases of PubMed, CINAHL, PsycINFO and the search engine Google (Scholar) to identify relevant keywords related to the subjects (Table 1 , view details of the search in Supplementary material 1). In step two, we used these keywords to build elaborated search strings for searching the databases of PubMed, CINAHL and PsycINFO. We used various combinations of search terms to either broaden or narrow down the search, depending on the results in a specific database. The search string focused on keywords in titles and abstracts. We searched for papers written in English or Dutch and published from December 2019 onwards, as this review focusses on the COVID-19 period. In step three, we hand-searched the reference lists of articles that we considered eligible. Finally, in step four we searched for grey literature using the search engine Google. Furthermore, we searched for relevant letters and editorials, guides, web articles and policy papers published by knowledge and professional institutes or associations in dementia and palliative care. These included: The European Association for Palliative Care, Alzheimer's Disease International, The Gerontological Society of America, International Psychogeriatric Association, The Society for Post-Acute and Long-Term Care Medicine, International Long-Term Care Policy Network, Marie Curie, Dutch professional nurses organization, Palliaweb (Dutch online platform), Dutch Palliative Care Cooperation, Dutch Association of Elderly Care Physicians Verenso.
Table 1.
Key subjects and their search terms.
| Subject | Search terms |
|---|---|
| People with dementia | Dementia; Alzheimer's disease; Alzheimer; cognitive impairment; cognitively impaired |
| Palliative care | Palliative care; terminal care; end-of-life care; comfort care; nursing home; aged care; long-term care; bereavement; grief |
| COVID-19 | Covid-19; Corona; Coronavirus; 2019-nCoV; SARS-CoV-2 |
2.2. Study selection process
Table 2 displays the inclusion criteria for selecting articles and grey literature. Initially, we screened titles and abstracts or summaries and we excluded articles and papers that were irrelevant or beyond the scope of this review. After screening titles and abstracts or summaries, we obtained articles and papers that we deemed eligible as full texts and further scanned them for eligibility. Authors JM and SB contributed to the study selection process by both performing title–abstract and summary screening and full-text screening independently on all potential titles. Afterwards, the authors discussed any discrepancies and reached full agreement on which articles and papers to include in the review.
Table 2.
In- and exclusion criteria for selecting articles.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
2.3. Data synthesis and analysis
Three authors (JM, SB and IM) extracted data from the included papers. First, IM and SB extracted descriptive information from the articles to fill in a data extraction form. Extracted descriptive information included authors, date of publication, country, source or organization, type of article, setting and focus relevant to the review. Further, JM and SB read the included papers thoroughly to become acquainted with the content. Thereafter, JM listed initial relevant findings related to the research question that could inform recommendations for nursing staff working in long-term care facilities. The two authors (JM and SB) discussed the findings and SB formulated practical recommendations using the extracted information from included sources, adapted to our specific goal.
The recommendations were initially categorized according to the domains of palliative care as proposed by the National Consensus Project Clinical Practice Guidelines for Quality Palliative Care (Ferrell et al., 2018). These domains include physical aspects of care, psychological aspects of care, social aspects of care, spiritual aspects of care, cultural aspects of care, care for the dying, ethical aspects of care, and structure and processes of care. We discussed the recommendations that followed from this process iteratively throughout the analysis. We placed them under what we considered the most appropriate domain. Based on inductive findings from the included articles, we included recommendations on advance care planning and bereavement care. After JM and SB set up a complete list of recommendations, these were discussed with all authors integrating each team member's expertise for further interpretation, practical application and fine-tuning. The team's areas of expertise cover palliative care (for people with dementia and/or frailty), advance care planning, elderly care medicine, transmural nursing home care, and long-term care and (community) nursing. This process resulted in a final overview of recommendations for nursing staff on how to provide palliative care for people with dementia during the COVID-19 crisis.
3. Results
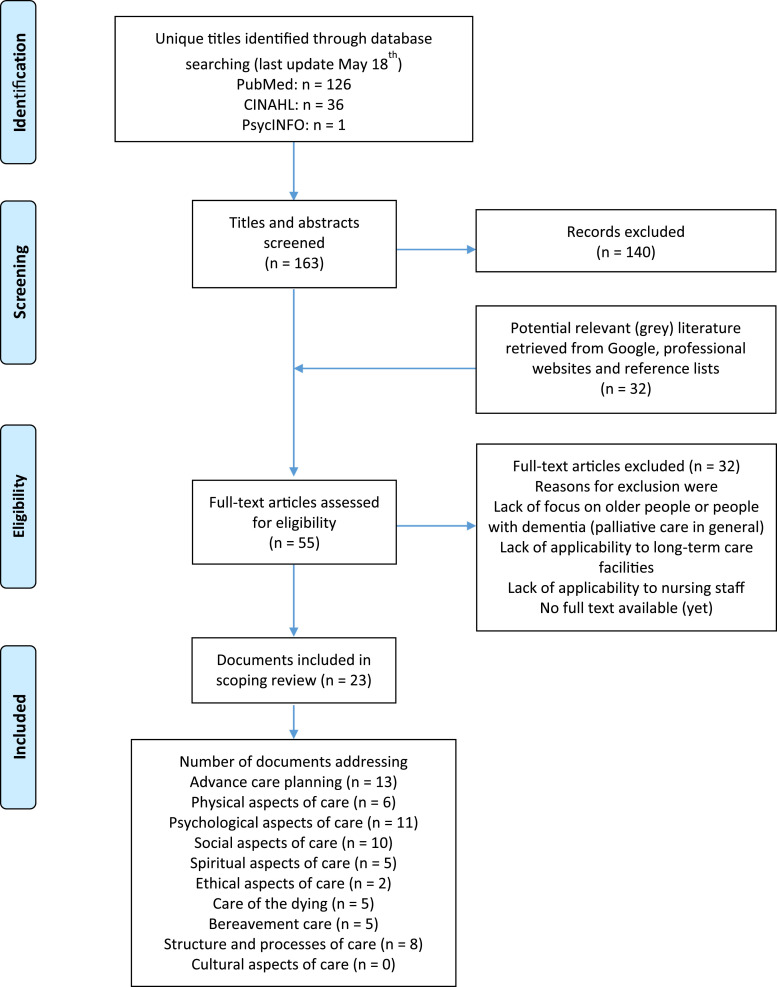
Searching CINAHL, PsycINFO and PubMed databases and searching (non-scientific) websites for eligible grey literature yielded 163 unique titles (Fig. 1 ). Eventually, we obtained full texts from 55 documents based on title/abstract screening, by hand searching eligible articles and by searching for grey literature. Of these full texts, 23 were eligible.
Fig. 1.
Flowchart of the search and selection process.
Table 3 shows the included articles and other documents, and their focus relevant to this review. Among the included documents, there were 7 (special) articles published in peer-reviewed journals (Borasio et al., 2020; Brown et al., 2020; D'Adamo et al., 2020; Kunz and Minder, 2020; Lapid et al., 2020; Moore et al., 2020a, 2020b; Wallace et al., 2020), 6 guides (British Geriatrics Society, 2020; Dementia Australia, 2020; Kaserer and Hofland, 2020; The Irish Hospice Foundation, 2020; The Scottish Government, 2020; Victoria State Government, 2020), 4 letters to editors (Eghtesadi, 2020; Husebo and Berge, 2020; Padala et al., 2020; Wang et al., 2020b), 2 web articles (blogs) (Bauer, 2020; Russell, 2020), 2 reports (Bauer et al., 2020; European Academy of Neurology, 2020), one correspondence paper (Wang et al., 2020a), and one position paper (Livingston et al., 2020). The documents (first authors) were from the UK and Ireland (n = 7), Europe (n = 6), the USA (n = 3), Australia (n = 2), Canada (n = 2), and Asia (n = 2). One was an international paper.
Table 3.
Descriptive information of the included articles and other documents.
| No. | Author(s) | Publication date, Country | Source or organisation | Type of article | Setting | Focus of the article relevant to the review |
|---|---|---|---|---|---|---|
| 1 | Victoria State Government | 18 March 2020, Australia | Victoria State Government | Guide | Long-term care facilities | Guidance for residential aged care staff regarding recognizing and responding to residents at the end of life |
| 2 | Borasio et al. | 24 March 2020, Switserland | Swiss Medical Weekly (peer-reviewed journal) | Special article | Various settings | Palliative care for vulnerable groups receiving palliative or long-term care |
| 3 | Kunz & Minder | 24 March 2020, Switserland | Swiss Medical Weekly (peer-reviewed journal) | Special article | Home and long-term care facilities | Palliative care for frail older people in long-term care facilities |
| 4 | D'Adamo, Yoshikawa & Ouslander | 25 March 2020, USA | Journal of the American Geriatrics Society (peer-reviewed journal) | Special article | Long-term care facilities | Care for frail older people living in long-term care facilities |
| 5 | Kaserer & Hofland | 25 March 2020, The Netherlands | Curinamae | Guide | Various settings | Advice on how to arrange rituals at the end of life and enable families to say goodbye (from a distance) |
| 6 | Russell | 26 March 2020, UK | British Geriatrics Society | Web article (blog) | Long-term care facilities | Advice on how to deal with challenges due to lockdowns in long-term care facilities |
| 7 | British Geriatrics Society | 30 March 2020, UK | British Geriatrics Society | Guide | Long-term care facilities | Decision-making and palliative care for residents in long-term care facilities |
| 8 | Wang et al. | 30 March 2020, China | The Lancet (peer-reviewed journal) | Correspondence (letter) | Long-term care facilities | Challenges and requirements in care and support for people living with dementia |
| 9 | Bauer | 31 March 2020 Switserland | International Long-Term Care Policy Network | Web article (blog) | Various settings | Palliative care for vulnerable groups with pre-existing conditions and those receiving long-term care |
| 10 | The Irish Hospice Foundation | April 2020 Ireland | The Irish Hospice Foundation | Guide | Various settings | Advice for family members on how to deal with a loss due to COVID-19 |
| 11 | European Academy of Neurology | 3 April 2020, European countries | European Academy of Neurology | Report | Various settings | Advice for care providers on how to support people with dementia in times of social isolation and lockdown |
| 12 | Livingston & Weidner | 9 April 2020, UK | Alzheimer's Disease International | Position paper | Various settings | Difficult palliative care decisions for people with dementia and their families |
| 13 | Eghtesadi | 11 April 2020, Canada | Journal of the American Geriatrics Society (peer-reviewed journal) | Letter to editor | Long-term care facilities | Tips for using modern technology in long-term care facilities to avoid acute care services |
| 14 | Wallace et al. | 13 April 2020, USA | Journal of Pain and Symptom Management (peer-reviewed journal) | Clinical practice article | Hospital and long-term care facilities | Dealing with (complicated) grief, considerations for palliative care providers |
| 15 | Brown et al. | 18 April 2020, Canada | The American Journal of Geriatric Psychiatry (peer-reviewed journal) | Special article | Various settings | Challenges in the care for people with dementia due to the impact of the COVID-19 pandemic in different (long-term) care settings |
| 16 | Wang et al. | 20 April 2020, Singapore | Journal of Palliative Medicine (peer-reviewed journal) | Letter to editor | Various settings | Advice for care providers to support older COVID-19 patients at the end of life and their families in grief and bereavement |
| 17 | Husebo & Berge | 22 April 2020, Norway | American Journal of Geriatric Psychiatry (peer-reviewed journal) | Letter to editor | Long-term care facilities | The challenge of restricted visits in long-term care facilities and the importance of advance care planning |
| 18 | Padala, Jendro & Orr | 23 April 2020, USA | Psychiatry Research (peer-reviewed journal) | Letter to editor | Long-term care facilities | An example of managing behavioral disturbances in a resident with dementia |
| 19 | Moore et al. | 30 April 2020, UK | International Psychogeriatrics (peer-reviewed journal) | Journal article | Various settings | Support needs of family caregivers of older people with dementia at the end of life and after bereavement |
| 20 | Dementia Australia | April 2020, Australia | Dementia Australia | Guide | Long-term care facilities | Guidance for long-term care staff caring for people with dementia |
| 21 | Bauer, Dixon & Comas-Herrera | 1 May 2020, UK | International Long-Term Care Policy Network | Report | Long-term care facilities | Provision of palliative care for older people residing in long-term care facilities |
| 22 | Lapid et al. | 11 May 2020, International | International Psychogeriatrics | Special article | Various settings | Providing end-of-life care for older people (with dementia) |
| 23 | The Scottish Government | 15 May 2020 (update), Scotland | The Scottish Government | Guide | Long-term care facilities | Practical advice for long-term care staff providing palliative care for residents |
From the included information sources, we extracted original content that informed a list of specific recommendations for nursing staff regarding the provision of palliative care for people with dementia living in long-term care facilities during the COVID-19 pandemic (Table 4 ). We categorized recommendations under a number of key domains in palliative care adapted from the National Consensus Project Clinical Practice Guidelines for Quality Palliative Care (Ferrell et al., 2018). Some would fit under multiple domains, though we chose what we considered the most appropriate domain. The domains with the highest number of articles that informed recommendations are ‘advance care planning’ and ‘psychological aspects of care’ (Fig. 1). The domains with the lowest number of articles that informed recommendations are ‘ethical care’, ‘care of the dying’, ‘spiritual care’ and ‘bereavement care’. We did not find information on ‘cultural aspects of care’.
Table 4.
Recommendations for nursing staff on providing palliative care for people with dementia in long-term care facilities in times of COVID-19.
| Advance care planning |
|---|
|
| Physical aspects of care |
|---|
|
| Psychological aspects of care |
|---|
|
| Social aspects of care |
|---|
|
| Spiritual aspects of care |
|---|
|
Additional recommendations for people with dementia who have COVID-19
|
| Care of the dying |
|---|
|
| Bereavement care |
|---|
|
| Ethical aspects of care |
|---|
|
| Structure and processes of care |
|---|
|
*Referencing numbers correspond with the overview of included documents in Table 3.
4. Discussion
This paper describes a rapid scoping review to formulate practice recommendations for nursing staff with regard to providing palliative dementia care in long-term care facilities in times of COVID-19. The recommendations that followed from the review touch upon most of the key elements of palliative care for people with dementia. Initially, we found papers that mainly addressed advance care planning and physical or medical care of COVID-19 patients. At the time of our first searches, articles on psychological, social and spiritual care and on nursing care were scarce. However, over time, more papers appeared that described these other domains and the impact of the COVID-19 pandemic on (caring for) people living with dementia. Although we found an increasing number of papers to inform palliative care given to people with dementia in times of COVID-19, papers that explicitly discussed palliative care in dementia specifically in relation to COVID-19 were limited. This illustrates that, although over the past two decades there has been increasing attention for palliative care in dementia (Hashimie et al., 2020; van der Steen, 2010), it is not a top priority when a crisis strikes. The current literature emphasizes specific challenges in times of COVID-19 related to advance care planning, family involvement and management of psychosocial needs that may aggravate due to social isolation and residents’ limited understanding of the situation. To a lesser extent, the literature addressed the spiritual aspects of care and grief and bereavement. So far, ethical and cultural aspects of palliative dementia care in times of COVID-19 remain under-reported. The available literature on the current pandemic reflects the need for holistic palliative care for people with dementia in long-term care facilities as well as for their families before and after bereavement. Besides improved experiences of people with dementia and their families, a palliative approach to care may contribute to better use of healthcare resources. For instance, advance care planning and setting palliative care goals may reduce hospitalizations and futile medical treatments, and education of healthcare staff may reduce medication administration and costs (Senderovich and Retnasothie, 2019). Adequate allocation of healthcare resources is imperative in times of COVID-19 (Barclay, 2020).
Although previous papers emphasize the important role of palliative care in times of humanitarian crises and pandemics (Downar and Seccareccia, 2010; Powell et al., 2017; Rosoff, 2006), the global response to COVID-19 exposes a lack of efficient pandemic palliative care plans and gaps in palliative care training and literature (Etkind et al., 2020). In long-term care facilities, which are generally understaffed and under-resourced with regard to providing palliative care, the current pandemic poses particular challenges by further increasing the workload and potential distress of staff (Arya et al., 2020). At this early point, it is difficult to map the adequacy of palliative care in long-term care facilities in the context of COVID-19. However, Bauer and colleagues wrote that many people at the end of life may have unmet palliative care needs in times of COVID-19, particularly the frail population residing in long-term care facilities (Bauer et al., 2020). The COVID-19 pandemic raises concerns as it induces a strain on health providers who are under-resourced to provide safe and effective palliative care (The Lancet, 2020). As the number of infected individuals has increased, the potential seriousness and mortality of the infection is becoming more clear, for vulnerable groups and for people with dementia in particular (Atkins et al., 2020). Moreover, social isolation regulations may have a detrimental effect on the psychosocial and physical wellbeing of residents with dementia in long-term care facilities (Velayudhan et al., 2020). These challenges highlight the necessity of adequate palliative care to relieve suffering of people with dementia on the physical, psychological, social and spiritual domain (The Lancet, 2020). Expectations are that COVID-19 will continue to be a long-lasting global health problem, which underlines the need to provide simultaneous COVID-sensitive and dementia-sensitive care as we transition back from emergency care to regular care (Canevelli et al., 2020). The current scoping review adds to the knowledge base by providing an overview of relevant literature and practical recommendations.
Over the past few months, the initial response to the pandemic crisis was focused on curing those infected, containing extensive outspread and preventing intensive care facilities from being overwhelmed by demand. This also reflects the more general, longstanding neglect of the long-term care sector (Lapid et al., 2020) and weaknesses in its palliative care capacities (Bauer et al., 2020). Although the initial response focused on the hospital setting and less on long-term care setting, initiatives that address the psychosocial and spiritual consequences of the pandemic for older people with dementia are on the rise. Long-term care organizations are thinking of innovative ways to deal with social isolation and quarantine regulations to avoid loneliness and social exclusion of older people and persons with dementia (Dementia Australia, 2020). Nursing staff working in long-term care facilities have a key role in providing psychosocial and spiritual care, especially when face-to-face meetings between families and their relatives with dementia are prohibited.
Literature that addresses domains of palliative dementia care other than the physical domain is increasing. However, a gap remains on some important aspects. The included documents in our review most often addressed advance care planning and psychological care, whereas practical information on spiritual care, care of the dying and the bereaved, and ethical aspects of care was sparse. The recommendations that we formulated related to these aspects are underpinned by a smaller body of literature, which suggests that (practical) knowledge on these aspects needs to be expanded. Currently, the most prominent literature gap is in cultural aspects of care, despite the global impact of COVID-19. Another recent review of worldwide guidance documents on palliative care in long-term care facilities also shows that several key aspects, such as holistic symptom management, decision-making and end-of-life and bereavement care remain under-reported (Gilissen et al., 2020). Although the recommendations that we formulated provide an initial basis for palliative care provision for people with dementia in times of COVID-19, they are limited to the currently available literature. Ideally, the recommendations should be updated regularly to provide ongoing support and information for nursing staff in long-term care facilities. This should inform contemporary COVID-sensitive and dementia-sensitive practice in long-term care facilities and add to the knowledge base for anticipating possible future crises.
4.1. Ethical issues in decision-making
An important, yet under-reported issue is how to deal with people for whom life-sustaining measures may be inappropriate in the context of COVID-19. In a paper responding to a previous influenza pandemic, Downar and colleagues describe ethical issues related to scarce healthcare resources and medical decision-making (Downar and Seccareccia, 2010). Triage systems and decision-making in times of scarcity may deprive seriously ill people from potentially life-sustaining treatments and cause physical and emotional suffering for patients, their families and care staff. Advance care planning is a process between healthcare professionals, an individual patient and his or her loved ones. Advance care planning and shared decision-making are core processes in establishing care goals for the end of life of persons with dementia (van der Steen et al., 2014) and may prevent unwanted life-sustaining treatments, which is paramount during this pandemic. Advance care planning conversations are particularly important in times of COVID-19 so that individual wishes for end-of-life care can be discussed in a timely manner and to inform people with dementia and their families about potential risks of hospitalization with the infection (Livingston et al., 2020). Families may feel more confident and less guilty about making end-of-life care decisions on behalf of their loved one with dementia if they know the person's wishes (Sellars et al., 2019). Particularly in times of COVID-19, it may be difficult and emotive for families of people with dementia who have not previously discussed their wishes to make such decisions (Moore et al., 2020a, 2020b). Although discussing care preferences may help to reduce chances of potentially futile and burdensome treatments and hospitalization, discussions concerning triage for intensive-care treatment under resource scarcity should not be included in the advance care planning process. However, during this pandemic, the autonomy to opt for life-prolonging treatments or a preferred place of death is possibly challenged because of public health directives and scarce resource accessibility (Brown et al., 2020).
Lack of a palliative care plan in times of a pandemic raises concerns about the provision of care that is in line with individual wishes of people facing life-limiting conditions and their families. A pandemic palliative care plan should facilitate palliative care services and health organizations to respond quickly and flexibly in times of scarce resources (Etkind et al., 2020). As Downar and colleagues described: we need “stuff” (for instance, stockpile medications), staff (education, expertise), space (special wards and units) and systems (triage systems, updated care plans) to provide comprehensive palliative care during a crisis (Downar and Seccareccia, 2010). In times of COVID-19 specifically, older and vulnerable people with cognitive impairment may not receive mechanical ventilation due to their prognosis, even if they wish to (Parsons and Johal, 2020). Residents with COVID-19 may be confined to a room or a special COVID-19 ward that is not of their choosing and regulations of social isolation and quarantine may hamper involvement of family members in the last phase of life of people with dementia (Radbruch et al., 2020). Even if people with dementia may not qualify for life-sustaining measures or acute care admission, it is a human right that they are not denied palliative care and adequate relief of suffering, regardless of whether they have COVID-19 (Brennan, 2007; Clarfield et al., 2020; Downar and Seccareccia, 2010). Stigma increases the risk of certain groups being denied access to health and social services (Brown et al., 2020). In dementia, stigmatization is a pervasive and widespread problem and there have been reports on stigmatization of older people who are at risk for contracting COVID-19 (Fraser et al., 2020). Hence, people with dementia may face double stigmatization (Brown et al., 2020). Nursing staff have an important role in advocating for people with dementia to shelter them from the negative consequences of stigmatization. During this pandemic, it is a global, public health urgency to apply palliative care knowledge to its best to provide equitable, compassionate and dignified care, to alleviate suffering and to mitigate the impact on caregiver grief and distress (Radbruch et al., 2020). In this review, we added advance care planning as a key domain for nursing recommendations. Nursing staff are essential stakeholders advocating for the provision of dignified palliative care for people with dementia. To achieve high-quality palliative care in times of this pandemic, it is crucial to review care plans within the interprofessional care team and to update goals of care through advance care planning conversations with people with dementia and their families (Borasio et al., 2020; British Geriatrics Society, 2020; Kunz and Minder, 2020).
Nursing staff should collaborate diligently with families, and with physicians and other healthcare professionals to provide timely and adequate care that is tailored to individual wishes. Vice versa, healthcare professionals from other disciplines must acknowledge and support nursing staff to facilitate their role. The current pandemic emphasizes the need for nursing leadership in long-term care settings. Especially registered nurses should have a recognized leading role in the delegation and oversight of care tasks, initiation and evaluation of care plans and assessment of their effectiveness (McGilton et al., 2016). They should also function as mentors and supervisors for other care personnel. In the context of COVID-19, decision-making and care provision may be challenging due to strained resources, which can induce moral distress. Moral distress arises when constraints prevent us from doing what we think is morally right, and it may induce unresolved grief and burnout in families and nursing staff (Wallace et al., 2020). It is important that nursing staff engage in open communication with their (interprofessional) colleagues and with families about the experience of distress. Nursing staff and family members often place the wellbeing of the person with dementia above their own feelings. Nonetheless, we need to stimulate self-care and increase self-awareness of families and nursing staff about (negative) emotions and thoughts during care provision in times of the COVID-19 pandemic. Again, this requires leadership skills among nurses to provide peer support and facilitate self-reflection and peer-to-peer coaching.
4.2. Grief and bereavement
In the context of the COVID-19 pandemic, experiences of grief and anticipatory grief are subject to change, which stimulates the need for adapting usual approaches to grief support (Wallace et al., 2020). Anticipatory grief is an emotional reaction to imminent losses and occurs before the actual death of oneself or a relative (Wallace et al., 2020). Anticipatory grief in relation to dementia is prevalent and complex (Moore et al., 2020a, 2020b), given the uncertain and sometimes lengthy illness trajectory, which is accompanied by serial losses on different domains (cognition, autonomy, social relationships) (Chan et al., 2013). Severe symptoms of anticipatory grief and low preparedness for the death of a relative are part of a complex network of risk factors for adverse bereavement outcomes, such as complicated grief (Nielsen et al., 2016; Stroebe et al., 2006; Wallace et al., 2020).
In this review's recommendations, we included bereavement care as a separate domain, given the unusual circumstances under which people are currently facing the loss of a relative. Given the sudden and rapid decline that a COVID-19 infection may cause, families and nursing staff may feel unprepared for the loss of a person (Moore et al., 2020a, 2020b; Wallace et al., 2020). Along with the possible inability of families to see or have physical contact with their relative at the end of life, this may increase the risk of complicated grief (Moore et al., 2020a, 2020b). It is important to note that nursing staff may equally suffer from grief or moral distress following the deaths of their residents (Bauer et al., 2020; Lapid et al., 2020). They may have to communicate distressing news to loved ones, which may be particularly disturbing for care staff who often consider residents (whom they have cared for over an extended period) as a part of their own family. Not being able to say goodbye properly relates to post-bereavement depression and complicated grief (Moore et al., 2020a, 2020b; Otani et al., 2017). Moreover, the world population is facing multiple potential or actual losses in several other areas due to the COVID-19 pandemic, including the loss of jobs and financial income security, of social, physical and spiritual connections, of physical or mental health, and of autonomy and freedom. A lack of social support relates to increased pre-death grief among family caregivers of people with dementia (Moore et al., 2020a, 2020b). Moreover, social distancing regulations force those who are bereaved in times of COVID-19 to suspend funerals or to arrange an online service instead, with no physical attendance of family members and friends. Thus, bereaved individuals may lack support in terms of physical touch from and closeness to others (‘a shoulder to cry on’, literally) (Moore et al., 2020a, 2020b). All these factors may increase the risk of trauma, posttraumatic stress disorder, feelings of abandonment or loneliness and a lack of social support to enable coping with the loss of a relative.
The complexity of grief and bereavement in times of COVID-19 emphasizes the role of nursing staff in adequately recognizing and addressing anticipatory grief, in preparing families for bereavement, and in helping families come to terms with their loss as a part of palliative care (Shore et al., 2016; Wallace et al., 2020). We need to optimize the quality of palliative care to reduce potential risk of adverse outcomes for those bereaved of a relative or friend with dementia during the COVID-19 pandemic. To achieve this, it is important that nurses pay attention to possible unmet psychosocial needs of people with dementia and their families, spiritual needs, rituals and family involvement towards the end of life, and signs of anticipatory or complicated grief. Moreover, grief and moral distress among nursing staff in times of COVID-19 should be acknowledged (Moore et al., 2020a, 2020b) and long-term care organizations should facilitate (peer) support structures.
Ultimately, humane and empathetic provision of palliative care including grief and bereavement support should prevail, even in times of the COVID-19 pandemic. As Dame Cecily Saunders once said, ‘‘how people die remains in the memory of those who live on.’’ Despite the tragedy of the COVID-19 pandemic, its worldwide impact may raise public death literacy and awareness with regard to the need to prioritize integration of palliative care into global health to ensure relief of suffering both before and after death (Lapid et al., 2020; Radbruch et al., 2020).
4.3. Limitations
This rapid scoping review has a few limitations. The goal of this review was to gather relevant information from various resources regarding palliative care and dementia care during the COVID-19 pandemic at short notice. The conduct of the searches was not fully systematic. Relevant documents may have been omitted due to oversight of relevant search terms and due to the rapid increase of both academic and grey literature focusing on COVID-19. Moreover, this review only included documents that were written in English or Dutch. The recommendations were not ranked on their importance. We did not perform a structured quality assessment of the included documents. However, this is in line with the conduct of scoping reviews (Peters et al., 2015).
5. Conclusion
In times of COVID-19, a pressing need arises for high-quality palliative care for people with dementia living in long-term care facilities and their families. Literature that informs how we should address this need increased over the last months. Nonetheless, an explicit focus on palliative dementia care is still largely lacking in the current academic and grey literature. Although medical and physical care are crucial in times of this pandemic, we need to address spiritual care, and culturally sensitive and ethical care. The COVID-19 outbreak and its ensuing societal impact emphasizes a particular need for care of the dying and the bereaved. We must acknowledge grief and moral distress that may arise among staff caring for residents in long-term care facilities. Currently, literature on the spiritual, cultural and ethical aspects and on care of the dying and the bereaved is scarce. The current pandemic raises the need for nursing leadership. Nursing staff should collaborate with their interprofessional teams to establish and document suitable goals of care, tailored to the wishes of patients and their families as these may change in times of COVID-19. Nursing staff are essential to providing palliative care across all domains of care for people with dementia and their families to safeguard a peaceful death and a worthy farewell in these unsettling times.
Conflict of Interest
None to declare.
Acknowledgments
Acknowledgments
Our very special thanks and our thoughts go out to all the nursing staff and other care professionals working hard to provide the best possible care in times of COVID-19. We thank all (regional and national) partners in the DEDICATED (Desired Dementia Care Towards End of Life) project. We thank our DEDICATED-nurses for their continuing efforts to improve palliative care for people with dementia.
Funding sources
This review was conducted as a part of the DEDICATED project, which is funded by ZonMw, the Netherlands Organisation for Health Research and Development (Palliantie; grant number 844001405).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnurstu.2020.103781.
Appendix. Supplementary materials
References
- Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Arya A., Buchman S., Gagnon B., Downar J. Pandemic palliative care: beyond ventilators and saving lives. Can. Med. Assoc. J. 2020;192(15):E400. doi: 10.1503/cmaj.200465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins, J.L., Masoli, J.A.H., Delgado, J., Pilling, L.C., Kuo, C.-L.C., Kuchel, G., Melzer, D., 2020. Preexisting Comorbidities Predicing Severe Covid-19 in Older Adults in the UK Biobank Community Cohort. medRxiv, 2020.2005.2006.20092700. DOI: 10.1101/2020.05.06.20092700
- Barclay, L., 2020. Age, Dementia and the Allocation of Health Resources During and Beyond COVID-19. Retreived from: https://www.alz.co.uk/sites/default/files/pdfs/Age-dementia-and-the-allocation-of-health-resources-during-and-beyond-COVID-19.pdf (accessed 6 July 2020).
- Bauer, A., 2020. COVID19: Providing Palliative Care for the Many. Article in Article in LTCcovis.org. International Long-Term Care Policy Network, CPEC-LSE. Retreived from: https://ltccovid.org/2020/03/31/covid19-proving-palliative-care-for-the-many/ (accessed 17 April 2020)
- Bauer, A., Dixon, J., Comas-Herrera, A., 2020. End-of-life Support for People in Care Homes in the Context of COVID-19: International Report. International Long-Term Care Policy Network, CPEC-LSE. Retreived from: https://ltccovid.org/wp-content/uploads/2020/05/Palliative-care-in-care-homes-and-COVID-1-May-2020.pdf (accessed 19 May 2020).
- Bauer K., Schwarzkopf L., Graessel E., Holle R. A claims data-based comparison of comorbidity in individuals with and without dementia. BMC Geriatr. 2014;14(1):10. doi: 10.1186/1471-2318-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch D., Draper J. A critical literature review exploring the challenges of delivering effective palliative care to older people with dementia. J. Clin. Nurs. 2008;17(9):1144–1163. doi: 10.1111/j.1365-2702.2007.02220.x. [DOI] [PubMed] [Google Scholar]
- Bolt S.R., van der Steen J.T., Schols J.M.G.A., Zwakhalen S.M.G., Pieters S., Meijers J.M.M. Nursing staff needs in providing palliative care for people with dementia at home or in long-term care facilities: a scoping review. Int. J. Nurs. Stud. 2019;96:143–152. doi: 10.1016/j.ijnurstu.2018.12.011. [DOI] [PubMed] [Google Scholar]
- Borasio G.D., Gamondi C., Obrist M., Jox R., For, The Covid-Task Force Of Palliative, Ch COVID-19: decision making and palliative care. Swiss Med. Wkly. 2020;150:w20233. doi: 10.4414/smw.2020.20233. [DOI] [PubMed] [Google Scholar]
- Brennan F. Palliative care as an International Human Right. J. Pain Symptom Manag. 2007;33(5):494–499. doi: 10.1016/j.jpainsymman.2007.02.022. [DOI] [PubMed] [Google Scholar]
- British Geriatrics Society, 2020. COVID-19: Managing the COVID-19 Pandemic in Care Homes for Older People. Retreived from: https://www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes (accessed 27 March 2020)
- Brown E.E., Kumar S., Rajji T.K., Pollock B.G., Mulsant B.H. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer's disease and related dementias. Am. J. Geriatr. Psychiatry. 2020 doi: 10.1016/j.jagp.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canevelli M., Bruno G., Cesari M. Providing simultaneous COVID-19-sensitive and dementia-sensitive care as we transition from crisis care to ongoing care. Journal of the American Medical Directors Association. 2020 doi: 10.1016/j.jamda.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan D., Livingston G., Jones L., Sampson E.L. Grief reactions in dementia carers: a systematic review. Int. J. Geriatr. Psychiatry. 2013;28(1):1–17. doi: 10.1002/gps.3795. [DOI] [PubMed] [Google Scholar]
- Clarfield A.M., Dwolatzky T., Brill S., Press Y., Glick S., Shvartzman P., Doron I. Israel ad hoc COVID 19 committee. Guidelines for care of older persons during a pandemic. J. Am. Geriatr. Soc. 2020 doi: 10.1111/jgs.16554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Adamo H., Yoshikawa T., Ouslander J.G. Coronavirus disease 2019 in geriatrics and long-term care: the ABCDs of COVID-19. J. Am. Geriatr. Soc. 2020 doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- Davies N., Maio L., Vedavanam K., Manthorpe J., Vernooij-Dassen M., Iliffe S. Barriers to the provision of high-quality palliative care for people with dementia in England: a qualitative study of professionals' experiences. Health Soc. Care Community. 2014;22(4):386–394. doi: 10.1111/hsc.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dementia Australia, 2020. Coronavirus (COVID-19) Tips for Residential Aged Care Providers. Retreived from: https://www.dementia.org.au/files/helpsheets/DA_COVID19_Helpsheet_02_residential_care_providers_FA-v4.pdf (accessed 27 March 2020).
- Doupe M., Brownell M., St. John P., Strang D.G., Chateau D., Dik N. Nursing home adverse events: further insight into highest risk periods. J. Am. Med. Dir. Assoc. 2011;12(6):467–474. doi: 10.1016/j.jamda.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Downar J., Seccareccia D. Palliating a pandemic: "all patients must be cared for. J. Pain Symptom Manag. 2010;39(2):291–295. doi: 10.1016/j.jpainsymman.2009.11.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eghtesadi M. Breaking social isolation amidst COVID-19: a viewpoint on improving access to technology in long-term care facilities. J. Am. Geriatr. Soc. 2020 doi: 10.1111/jgs.16478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etkind S.N., Bone A.E., Lovell N., Cripps R.L., Harding R., Higginson I.J., Sleeman K.E. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J. Pain Symptom Manag. 2020;60(1):e31–e40. doi: 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Academy of Neurology, 2020. Dementia Scientific Panel Report – COVID-19. Retreived from: https://www.eanpages.org/2020/04/03/dementia-scientific-panel-report-covid-19/ (accessed 30 April 2020).
- Ferguson, N., Laydon, D., Nedjati Gilani, G., Imai, N., Ainslie, K., Baguelin, M., Bhatia, S., Boonyasiri, A., Cucunuba Perez, Z., Cuomo-Dannenburg, G., 2020. Report 9: Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. Retreived from: https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2020-03-16-COVID19-Report-9.pdf (accessed 6 July 2020).
- Ferrell B.R., Twaddle M.L., Melnick A., Meier D.E. National consensus project clinical practice guidelines for quality palliative care guidelines. J. Palliat. Med. 2018;21(12):1684–1689. doi: 10.1089/jpm.2018.0431. [DOI] [PubMed] [Google Scholar]
- Fraser S., Lagace M., Bongue B., Ndeye N., Guyot J., Bechard L., Garcia L., Taler V., Adam S., Beaulieu M., Bergeron C.D., Boudjemadi V., Desmette D., Donizzetti A.R., Ethier S., Garon S., Gillis M., Levasseur M., Lortie-Lussier M., Marier P., Robitaille A., Sawchuk K., Lafontaine C., Tougas F. Ageism and COVID-19: What does our society's response say about us? Age Ageing. 2020 doi: 10.1093/ageing/afaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froggatt, K., Edwards, M., Morbey, H., Payne, S., 2016. Mapping Palliative Care Systems in Long Term Care Facilities in Europe. PACE work package 1. Retreived from: https://www.eapcnet.eu/Portals/0/adam/Content/xwkGGSw2ykCLpHNMPZRxkA/Text/WP1_EAPC%20report%20Feb_25_2016.pdf (accessed 6 July 2020)
- Gardner W., States D., Bagley N. The coronavirus and the risks to the elderly in long-term care. J. Aging Soc. Policy. 2020;32(4-5):310–315. doi: 10.1080/08959420.2020.1750543. [DOI] [PubMed] [Google Scholar]
- Gilissen J., Pivodic L., Unroe K.T., van den Block L. International COVID-19 palliative care guidance for nursing homes leaves key themes unaddressed. J. Pain Symptom Manag. 2020 doi: 10.1016/j.jpainsymman.2020.04.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon, A.L., Goodman, C., Achterberg, W., Barker, R.O., Burns, E., Hanratty, B., Martin, F.C., Meyer, J., O'Neill, D., Schols, J., Spilsbury, K., 2020. Commentary: COVID in Care Homes-Challenges and Dilemmas in Healthcare Delivery. Age and ageing, afaa113. doi: 10.1093/ageing/afaa113. [DOI] [PMC free article] [PubMed]
- Hashimie J., Schultz S.K., Stewart J.T. Palliative care for dementia: 2020 update. Clin. Geriatr. Med. 2020;36(2):329–339. doi: 10.1016/j.cger.2019.11.011. [DOI] [PubMed] [Google Scholar]
- Husebo B.S., Berge L.I. Intensive medicine and nursing home care in times of SARS CoV-2: a Norwegian perspective. Am. J. Geriatr. Psychiatry. 2020 doi: 10.1016/j.jagp.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaserer, L., Hofland, B., 2020. Handleiding Voor Afscheidsrituelen in de Buitengewone Situatie van de Coronavirus-crisis. Retreived from: https://zingevingopdekaart.nl/_files/200000154-7a4de7a4e1/RK%20afscheidsrituelen-7.pdf (accessed 27 March 2020).
- Kolanowski A., Boltz M., Galik E., Gitlin L.N., Kales H.C., Resnick B., Van Haitsma K.S., Knehans A., Sutterlin J.E., Sefcik J.S., Liu W., Petrovsky D.V., Massimo L., Gilmore-Bykovskyi A., MacAndrew M., Brewster G., Nalls V., Jao Y.L., Duffort N., Scerpella D. Determinants of behavioral and psychological symptoms of dementia: a scoping review of the evidence. Nurs. Outlook. 2017;65(5):515–529. doi: 10.1016/j.outlook.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunz R., Minder M. COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Med. Wkly. 2020;150:w20235. doi: 10.4414/smw.2020.20235. [DOI] [PubMed] [Google Scholar]
- Lapid M.I., Koopmans R., Sampson E.L., Van den Block L., Peisah C. Providing quality end of life care to older people in the era of COVID-19: Perspectives from five countries. Int. Psychogeriatr. 2020:1–18. doi: 10.1017/s1041610220000836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement. Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston, G., Weidner, W., Alzheimer's Disease International, 2020. COVID-19 and Dementia: Difficult Decisions About Hospital Admission and Triage. Retreived from: https://www.alz.co.uk/news/adi-releases-position-paper-on-covid-19-and-dementia (accessed 15 April 2020).
- Lockwood C., dos Santos K.B., Pap R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs. Res. 2019;13(5):287–294. doi: 10.1016/j.anr.2019.11.002. [DOI] [PubMed] [Google Scholar]
- McGilton K.S., Bowers B.J., Heath H., Shannon K., Dellefield M.E., Prentice D., Siegel E.O., Meyer J., Chu C.H., Ploeg J., Boscart V.M., Corazzini K.N., Anderson R.A., Mueller C.A. Recommendations from the international consortium on professional nursing practice in long-term care homes. J. Am. Med. Dir. Assoc. 2016;17(2):99–103. doi: 10.1016/j.jamda.2015.11.001. [DOI] [PubMed] [Google Scholar]
- Moore K.J., Crawley S., Vickerstaff V., Cooper C., King M., Sampson E.L. Is preparation for end of life associated with pre-death grief in caregivers of people with dementia? Int. Psychogeriatr. 2020:1–11. doi: 10.1017/s1041610220000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K.J., Sampson E.L., Kupeli N., Davies N. Supporting families in end-of-life care and bereavement in the COVID-19 Era. Int. Psychogeriatr. 2020:1–10. doi: 10.1017/S1041610220000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls D., Chang E., Johnson A., Edenborough M. Touch, the essence of caring for people with end-stage dementia: a mental health perspective in Namaste Care. Aging Ment. Health. 2013;17(5):571–578. doi: 10.1080/13607863.2012.751581. [DOI] [PubMed] [Google Scholar]
- Nielsen M.K., Neergaard M.A., Jensen A.B., Bro F., Guldin M.-B. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin. Psychol. Rev. 2016;44:75–93. doi: 10.1016/j.cpr.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Otani H., Yoshida S., Morita T., Aoyama M., Kizawa Y., Shima Y., Tsuneto S., Miyashita M. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J. Pain Symptom Manag. 2017;54(3):273–279. doi: 10.1016/j.jpainsymman.2017.07.010. [DOI] [PubMed] [Google Scholar]
- Padala S.P., Jendro A.M., Orr L.C. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer's dementia during COVID-19. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons J.A., Johal H.K. Best interests versus resource allocation: could COVID-19 cloud decision-making for the cognitively impaired? J. Med. Ethics. 2020 doi: 10.1136/medethics-2020-106323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M.D., Godfrey C.M., McInerney P., Soares C.B., Khalil H., Parker D., The Joanna Briggs Institute . Methodology for JBI Scoping Reviews. The Joanna Briggs Institute; Adelaide, Australia: 2015. The Joanna Briggs Institute reviewers' manual 2015. [Google Scholar]
- Powell R.A., Schwartz L., Nouvet E., Sutton B., Petrova M., Marston J., Munday D., Radbruch L. Palliative care in humanitarian crises: always something to offer. Lancet. 2017;389(10078):1498–1499. doi: 10.1016/s0140-6736(17)30978-9. [DOI] [PubMed] [Google Scholar]
- Radbruch L., Knaul F.M., de Lima L., de Joncheere C., Bhadelia A. The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020;395(10235):1467–1469. doi: 10.1016/S0140-6736(20)30964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyniers T., Deliens L., Pasman H.R., Morin L., Addington-Hall J., Frova L., Cardenas-Turanzas M., Onwuteaka-Philipsen B., Naylor W., Ruiz-Ramos M., Wilson D.M., Loucka M., Csikos A., Rhee Y.J., Teno J., Cohen J., Houttekier D. International variation in place of death of older people who died from dementia in 14 European and non-European countries. J. Am. Med. Dir. Assoc. 2015;16(2):165–171. doi: 10.1016/j.jamda.2014.11.003. [DOI] [PubMed] [Google Scholar]
- Rosoff P.M. A central role for palliative care in an influenza pandemic. J. Palliat. Med. 2006;9(5):1051–1053. doi: 10.1089/jpm.2006.9.1051. [DOI] [PubMed] [Google Scholar]
- Russell, S., 2020. COVID-19: Supporting and Caring from Afar. British Geriatrics Society. Retreived from: https://www.bgs.org.uk/blog/covid-19-supporting-and-caring-from-afar (accessed 17 April 2020).
- Ryan T., Gardiner C., Bellamy G., Gott M., Ingleton C. Barriers and facilitators to the receipt of palliative care for people with dementia: the views of medical and nursing staff. Palliat. Med. 2012;26(7):879–886. doi: 10.1177/0269216311423443. [DOI] [PubMed] [Google Scholar]
- Seitz D., Purandare N., Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int. Psychogeriatr. 2010;22(7):1025–1039. doi: 10.1017/S1041610210000608. [DOI] [PubMed] [Google Scholar]
- Sellars M., Chung O., Nolte L., Tong A., Pond D., Fetherstonhaugh D., McInerney F., Sinclair C., Detering K.M. Perspectives of people with dementia and carers on advance care planning and end-of-life care: a systematic review and thematic synthesis of qualitative studies. Palliat. Med. 2019;33(3):274–290. doi: 10.1177/0269216318809571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senderovich H., Retnasothie S. A systematic review of the integration of palliative care in dementia management. Palliat. Support Care. 2019:1–12. doi: 10.1017/s1478951519000968. [DOI] [PubMed] [Google Scholar]
- Shams S.A., Haleem A., Javaid M. Analyzing COVID-19 pandemic for unequal distribution of tests, identified cases, deaths, and fatality rates in the top 18 countries. Diabetes Metab. Syndr.: Clin. Res. Rev. 2020;14(5):953–961. doi: 10.1016/j.dsx.2020.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore J.C., Gelber M.W., Koch L.M., Sower E. Anticipatory grief: an evidence-based approach. J. Hosp. Palliat. Nurs. 2016;18(1) doi: 10.1097/NJH.0000000000000208. [DOI] [Google Scholar]
- Stroebe M.S., Folkman S., Hansson R.O., Schut H. The prediction of bereavement outcome: development of an integrative risk factor framework. Soc. Sci. Med. 2006;63(9):2440–2451. doi: 10.1016/j.socscimed.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Sutin A.R., Stephan Y., Luchetti M., Terracciano A. Loneliness and risk of dementia. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018 doi: 10.1093/geronb/gby112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Irish Hospice Foundation, 2020. Ackowledging and Coping with Grief from a Covid-19 Death. Retreived from: https://hospicefoundation.ie/bereavement-2-2/covid19-care-and-inform/acknowledging-and-coping-with-grief-from-a-covid-19-death/ (accessed 30 April 2020).
- The Lancet Palliative care and the COVID-19 pandemic. Lancet. 2020;395(10231):1168. doi: 10.1016/s0140-6736(20)30822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Scottish Government, 2020. National Clinical and Practice Guidance for Adult Care Homes in Scotland during the COVID-19 Pandemic. Retreived from: https://www.gov.scot/binaries/content/documents/govscot/publications/advice-and-guidance/2020/03/coronavirus-covid-19-clinical-and-practice-guidance-for-adult-care-homes/documents/clinical-guidance-for-nursing-home-and-residential-care-residents/clinical-guidance-for-nursing-home-and-residential-care-residents/govscot%3Adocument/National%2BClinical%2BGuidance%2Bfor%2BCare%2BHomes%2BCOVID-19%2BPandemic-%2BMASTER%2BCOPY%2B-%2BFINAL%2B-%2B15%2BMay%2B2020.pdf (accessed 18 May 2020).
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., Hempel S., Akl E.A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M.G., Garritty C., Lewin S., Godfrey C.M., Macdonald M.T., Langlois E.V., Soares-Weiser K., Moriarty J., Clifford T., Tunçalp Ö., Straus S.E. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169(7):467–473. doi: 10.7326/m18-0850. [DOI] [PubMed] [Google Scholar]
- van der Steen J.T. Dying with dementia: what we know after more than a decade of research. J. Alzheimers Dis. 2010;22(1):37–55. doi: 10.3233/jad-2010-100744. [DOI] [PubMed] [Google Scholar]
- van der Steen J.T., Radbruch L., Hertogh C.M., de Boer M.E., Hughes J.C., Larkin P., Francke A.L., Junger S., Gove D., Firth P., Koopmans R.T., Volicer L. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat. Med. 2014;28(3):197–209. doi: 10.1177/0269216313493685. [DOI] [PubMed] [Google Scholar]
- Velayudhan L., Aarsland D., Ballard C. Mental health of people living with dementia in care homes during COVID-19 pandemic. Int. Psychogeriatr. 2020:1–2. doi: 10.1017/S1041610220001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victoria State Government, 2020. Coronavirus Disease 2019 (COVID-19): Recognising and Responding to a Person at the End of Life. Retreived from: https://www.dhhs.vic.gov.au/recognising-and-responding-at-the-end-of-life-COVID-19 (accessed 18 May 2020).
- Wallace C.L., Wladkowski S.P., Gibson A., White P. Grief during the COVID-19 pandemic: considerations for palliative care providers. J. Pain Symptom Manag. 2020 doi: 10.1016/j.jpainsymman.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Li T., Barbarino P., Gauthier S., Brodaty H., Molinuevo J.L., Xie H., Sun Y., Yu E., Tang Y., Weidner W., Yu X. Dementia care during COVID-19. Lancet. 2020;395(10231):1190–1191. doi: 10.1016/s0140-6736(20)30755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S.S.Y., Teo W.Z.Y., Yee C.W., Chai Y.W. Pursuing a good death in the time of COVID-19. J. Palliat. Med. 2020 doi: 10.1089/jpm.2020.0198. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020. Rolling Updates on Coronavirus Disease (COVID-19). Retreived from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 8 May 2020).
- Worldometers, 2020. COVID-19 Coronavirus Pandemic. Retreived from: https://www.worldometers.info/coronavirus/ (accessed 15 July 2020).
- Zuidema S.U., de Jonghe J.F., Verhey F.R., Koopmans R.T. Environmental correlates of neuropsychiatric symptoms in nursing home patients with dementia. Int. J. Geriatr. Psychiatry. 2010;25(1):14–22. doi: 10.1002/gps.2292. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.