Abstract
WHO Member States adopted the Global Code of Practice on the International Recruitment of Health Personnel 10 years ago. This study assesses adherence with the Code’s principles and its continuing relevance in the WHO Europe region with regards to international recruitment of health workers. Data from the joint OECD/EUROSTAT/WHO-Europe questionnaire from 2010 to 2018 are analyzed to determine trends in intra- and inter-regional mobility of foreign-trained doctors and nurses working in case study destination countries in Europe. In 2018, foreign-trained doctors and nurses comprised over a quarter of the physician workforce and 5% of the nursing workforce in five of eight and four of five case study countries, respectively. Since 2010, the proportion of foreign-trained nurses and doctors has risen faster than domestically trained professionals, with increased mobility driven by rising East-West and South-North intra-European migration, especially within the European Union. The number of nurses trained in developing countries but practising in case study countries declined by 26%. Although the number of doctors increased by 27%, this was driven by arrivals from countries experiencing conflict and volatility, suggesting countries generally are increasingly adhering to the Code’s principles on ethical recruitment. To support ethical recruitment practices and sustainable workforce development in the region, data collection and monitoring on health worker mobility should be improved.
Introduction
It is now more than 10 years since World Health Organization (WHO) Member States adopted the landmark ‘WHO Global Code of Practice on the International Recruitment of Health Personnel’.1 The Code represents a significant global effort to tackle the challenge of international health worker mobility, a critical factor driving chronic workforce shortages in developing countries and undermining sustainable health workforce development in both source and destination countries alike.2,3 Through the Code, ‘voluntary principles and practices’ were established to ensure that international migration of health workers was ethical and of benefit to health systems in all WHO Member States.1,2 Significantly, the Code aimed to discourage the active recruitment of health workers from low- and middle-income countries (LMIC) deemed to be facing a critical shortage of health workers. To further support source countries and ‘sustain and promote health human resource development and training’, the Code encourages collaboration and skills exchange between source and destination countries, for example through bilateral agreements and by incentivizing return migration.1 The need to reduce recruitment of migrant health workers was placed within the wider context of creating a sustainable health workforce in all countries, underpinned by ‘effective health workforce planning, education and training and retention strategies’.1
An important aspect of the Code is its emphasis on improving data gathering and research on health worker migration and its impact on health systems. This data collection and research help to support achievement of the Code’s objectives and helps more widely to improve health workforce planning and the implementation of evidence-based workforce policies.1,2 Although results from the first and second round of monitoring on the Code’s implementation in 2013 and 2016 suggested that data collection and research capacity on international health workforce migration globally remained limited, greater progress and engagement with the Code was seen in Europe.3,4 A notable landmark in the region has been the extension of joint data collection on health worker mobility to all countries through the Joint OECD/EUROSTAT/WHO-Europe questionnaire on non-monetary healthcare statistics (JQNMHC), with the aim of improving the completeness and comparability of data on intra- and inter-European mobility of doctors and nurses.5
A limited number of studies have since used JQNMHC data to analyze trends in health worker mobility in Europe. Two of these studies, using data up until 2016, determined that health worker mobility in in the region had increased since 2010, although no data were provided on country or region of training of migrant health professionals.6,7 EU enlargement from 2004 to 2007 and the economic crisis in 2008–09 were shown to be significant events affecting the size and patterns of mobility trends.6,7 Away from the JQNMHC, studies mostly using non-nationally representative sample data have indicated that Finland, Germany, Ireland, Sweden, Switzerland and the UK have a high share of foreign-trained health professionals from LMIC, although trends over time were generally not explored.8,9
In this study, we aim to build on these prior studies by estimating how the share of foreign-trained doctors and nurses in major receiving countries in Europe have changed in the decade following the Code’s implementation, using the latest available data from the JQNMHC. Our analysis disaggregates data by country of training origin, allowing us to explore inter- and intra-European mobility of health workers from key individual source countries and according to World Bank income group. Our results inform an assessment of: (i) whether health worker migration from LMIC into major receiving European countries has declined since 2010; and (ii) whether the Code remains of value in the region, including within the European Union (EU) free-movement area.
Methods
Data source
Data were taken from the 2019 joint OECD/EUROSTAT/WHO-Europe questionnaire on non-monetary healthcare statistics.5 The JQNMHC was first administered to focal points in all European and OECD countries in 2010, with data now collected annually to provide internationally comparable statistics on non-monetary features of healthcare systems, including the health workforce.10 In 2015, a new part was added to the questionnaire to improve monitoring of health worker migration by capturing data on the total stock and annual inflow of foreign-trained doctors and nurses.5 The collection of this data aims to be relevant to both source and destination countries. In each round of data collection, respondents are asked to report data from the year 2000 to the latest full year, ending 31 December.
In the context of the questionnaire, ‘foreign-trained’ focuses on the place of training (rather than nationality) for the first medical (degree) or recognized nursing qualification. Respondents are asked to provide data from available national sources (with professional registries preferred) on practising physicians and nurses where possible, or otherwise professionally active physicians or nurses and/or those licenced to practise. An overview of key definitions and inclusion and exclusion criteria for data is provided in Supplementary table S1.
Data analysis
We analyze trends in international health worker migration and mobility in selected case study countries that are traditional receiving countries for foreign-trained doctors and nurses in Europe. Our analysis explores trends by source country of training and country of destination to determine how intra-European mobility has changed over time both within the EU and from outside, and how migration patterns have changed for health professionals trained in LMIC. To meet these aims, countries were only included as a case study country if the following criteria were met:
Data on foreign-trained doctors and/or foreign-trained nurses were available from 2010/11 or before, to 2017/18.
Data on the specific country of training for the first qualification are available for all years, with no >20% of countries of training classified as ‘other’.
The share of foreign-trained doctors in the physician workforce was 5% or above; or the share of foreign-trained nurses in the nurse workforce was 2% or above.
Eight countries met the criteria above and are included as case studies for our analysis of the foreign-trained physician workforce: Austria, Belgium, France, Germany, Ireland, Norway, Switzerland and the UK. Data were less comprehensive for the foreign-trained nurse workforce, leaving only five case study countries: Belgium, France, Norway, Switzerland and the UK. It should be noted that for Germany, the definition of foreign-trained physicians and nurses are based on nationality and not place of training; this reduces comparability with other countries, in particular when assessing trends for non-EU mobility as third-country nationals may be more likely to acquire German nationality. Additionally, data on the nursing workforce in Switzerland only capture nurses working in hospitals (∼51% of all nurses in 2016)11 and is therefore not representative of the entire nursing workforce. Data on doctors for the UK cover England and Scotland only and not Wales and Northern Ireland, although data for nurses are from all four nations.
To explore intra-European mobility both within the EU and outside, all European countries of training origin were organized into three groups (Supplementary table S2): (i) EU-15 Member States that joined prior to May 2004 (including the UK) plus four EFTA countries (Iceland, Liechtenstein, Norway and Switzerland); (ii) EU-13 Member States that joined after 1 May 2004; and (iii) 21 non-EU countries of the WHO European Region. Remaining countries of training origin were classified according to World Bank income groups: high-, upper middle- and low and lower middle-income economies. All analyses were undertaken in Excel.
Results
Large variations in the reliance on foreign-trained doctors and nurses exist across Europe
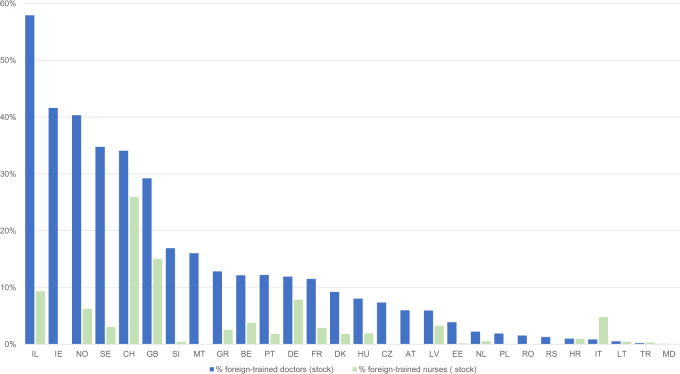
Figure 1 shows the proportion of foreign-trained doctors and nurses in WHO Europe Member States reporting at least 1 year of recent data to the JQNMHC. Although data were reported by 53% of countries, 22 reported no data (predominantly non-EU Member States in the East of the region), while Finland, Spain and Slovakia reported no data past 2012. Data completeness was higher for foreign-trained doctors (28 reporting countries) than nurses (23 reporting countries; figure 1).
Figure 1.
Foreign-trained doctors and nurses as a share of total stock of doctors and nurses, 2018 (or latest available year*). IL, Israel; IE, Ireland; NO, Norway; SE, Sweden; CH, Switzerland; GB, United Kingdom; SI, Slovenia; MT, Malta; GR, Greece; BE, Belgium; PT, Portugal; DE, Germany; FR, France; DK, Denmark; HU, Hungary; CZ, Czech Republic; AT, Austria; LV, Latvia; EE, Estonia; NL, Netherlands; PL, Poland; RO, Romania; RS, Serbia; HR, Croatia; IT, Italy; LT, Lithuania; TR, Turkey; MD, Moldova. Note: *Latest available year for foreign-trained doctors if no data for 2018: Turkey, 2015; Croatia, Denmark, Netherlands, Sweden, 2016; Germany, Greece, Hungary, Latvia, Lithuania, Malta, Moldova, Poland, Portugal, Romania, Switzerland, 2017. Latest available year for foreign-trained nurses if no data for 2018: Portugal, 2014; Greece, Turkey, 2015; Denmark, Netherlands, Sweden, 2016; Croatia, Germany, Hungary, Latvia, Moldova, Poland, Romania, Slovenia, Switzerland, 2017. Countries reporting data on foreign-trained physicians but not nurses: Austria, Bulgaria, Czech Republic, Ireland, Malta, Serbia, Slovakia. Source: Data reported to Ref. [5]
In 2018, foreign-trained doctors comprised over a quarter of the physician workforce in Israel, Ireland, Norway, Sweden, Switzerland and the UK. In many countries in the East and South of the region (Croatia, Italy, Latvia, Moldova, Poland, Romania, Serbia and Turkey) this proportion was <2% (figure 1). It should be noted that 40.6% and 54.0% of foreign-trained doctors in Israel and Norway, respectively were native-born individuals who studied abroad before returning. While Israel has the highest share of foreign-trained doctors (57.9%), the UK and Germany are the main countries of destination in terms of absolute numbers. Foreign-trained nurses make up a smaller proportion of the workforce (but a higher number of professionals overall), with only Germany, Israel, Norway, Switzerland and the UK reporting that more than 5% of the nursing stock were foreign-trained. Switzerland has the highest share of foreign-trained nurses (25.9%), with the UK the main country of destination for foreign-trained nurses in absolute terms.
In the subsequent analysis, we narrow our focus to explore health worker mobility in case study countries.
Doctors trained in LMIC are a small share of the foreign-trained workforce in case study countries, with some exceptions
Table 1 provides an overview of the country of training of doctors in eight case study countries in 2018. Although the share of foreign-trained doctors trained in a LMIC was generally small (below 3%), it was over 50% in Ireland and the UK and over 15% in Germany and France (table 1). In Austria, Belgium and Switzerland, the majority of foreign-trained doctors were trained in an EU-15/EFTA country, with a smaller but sizeable share trained in an EU-13 Member State. Doctors trained in EU-13 Member States comprised the largest share of foreign-trained doctors in Germany and Norway. In France, source countries for foreign-trained doctors were more evenly split between LMIC, upper middle-income countries and EU-15/EFTA and EU-13 Member States. It should be noted that Belgium and France have a relatively high proportion of training country of origin classified as ‘other’ (10.6% and 17.5%, respectively), making it likely that the totals for some groups of origin are underestimated.
Table 1.
Stock of foreign-trained doctors and nurses in case study countries by European origin or income group, 2018
| Country | Domestic- trained, % of total stock (n) | Foreign- trained, % of total stock (n) | EU15 + EEA + CH, % of foreign- trained (n) | EU-13, % of foreign- trained (n) | WHO Europe Region (non-EU), % of foreign- trained (n) | Low and lower middle incomea, % of foreign- trained (n) | Upper middle incomea, % of foreign- trained (n) | High incomea, % of foreign- trained (n) | Other (not classified), % of foreign- trained (n) |
|---|---|---|---|---|---|---|---|---|---|
| Foreign-trained doctors in case study countries | |||||||||
| Austria (2018) | 94.0% (35 970) | 6.0% (2282) | 72.0% (1643) | 27.8% (635) | 0.1% (2) | 0% (0) | 0% (0) | 0.1% (2) | 0% (0) |
| Belgium (2018) | 87.9% (58 499) | 12.1% (8062) | 62.1% (5003) | 21.4% (1724) | 0.9% (76) | 1.4% (110) | 3.3% (263) | 0.37% (30) | 10.6% (856) |
| France (2018) | 88.5% (200 811) | 11.5% (26 048) | 21.8% (5689) | 22.3% (5816) | 2.6% (672) | 17.1% (4452) | 18.4% (4795) | 0.29% (75) | 17.5% (4549) |
| Germany (2017) | 88.1% (310 935) | 11.9% (41 934) | 20.4% (8555) | 28.2% (11 840) | 21.2% (8884) | 16.0% (6662) | 10.1% (4223) | 2.4% (989) | 1.86% (781) |
| Ireland (2018) | 58.4% (13 429) | 41.6% (9583) | 13.1% (1253) | 18.9% (1813) | 1.52% (146) | 50.1% (4796) | 13.2% (1268) | 3.19% (306) | 0.01% (1) |
| Norway (2018)b | 58.3% (14 816) | 40.3% (10 248) | 41.7% (4270) | 44.5% (4558) | 6.3% (642) | 2.47% (253) | 2.81% (288) | 1.06% (109) | 4.80% (128) |
| Switzerland (2017) | 65.9% (24 330) | 34.1% (12 570) | 81.8% (10 280) | 8.26% (1038) | 2.94% (369) | 1.58% (199) | 3.34% (420) | 0.95% (120) | 1.15% (144) |
| UK (2018)b | 66.1% (115 508) | 29.2% (51 115) | 14.1% (7219) | 8.9% (4550) | 2.6% (1322) | 59.9% (30 601) | 10.9% (5587) | 2.17% (1109) | 1.42% (727) |
| Foreign-trained nurses in case study countries | |||||||||
| Belgium (2018) | 96.3% (202 617) | 3.8% (7889) | 58.3% (4598) | 26.4% (2084) | 0.25% (20) | 4.5% (353) | 1.45% (114) | 0.16% (13) | 9.0% (707) |
| France (2018)c | 97.0% (700 743) | 2.9% (20 757) | 80.7% (16 746) | 1.89% (393) | 0.09% (18) | 0% (0) | 0% (0) | 0% (0) | 17.3% (3600) |
| Norway (2018)c | 88.8% (86 296) | 6.2% (6065) | 51.8% (3140) | 16.4% (996) | 4.47% (271) | 16.6% (1006) | 2.23% (135) | 6.81% (413) | 1.71% (104) |
| Switzerland (2017)c | 60.5% (42 974) | 25.9% (18 403) | 76.7% (14 118) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 23.3% (4285) |
| UK (2018) | 85.0% (589 253) | 15.1% (104 365) | 18.1% (18 924) | 12.5% (13 037) | 0.07% (76) | 35.6% (37 155) | 2.77% (2886) | 1.37% (1426) | 29.3% (30 621) |
Notes: The dark shaded column is the domestically-trained workforce. The light shaded columns are foreign-trained doctors or nurses from Europe.
Excludes European countries.
Does not equal 100% as 1.4% of doctors in Norway and 4.7% of doctors in the UK have an unknown place of training.
Does not equal 100% as 0.15% of nurses in France, 5.0% in Norway and 13.6% in Switzerland have an unknown place of training.
The foreign-trained doctor workforce has grown faster than the domestic workforce
The number of foreign-trained doctors increased by over 46% between 2010 and 2018 in the eight case study countries, more than three times the growth rate of 13% in the overall number of doctors (Supplementary table S3). Although the number of foreign-trained doctors more than doubled in Germany, it increased by only 10% in the UK.
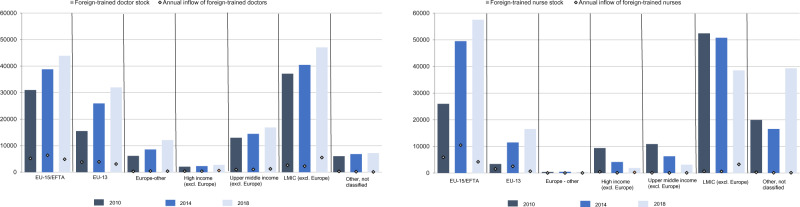
Figure 2 shows that the stock of doctors trained in other EU-15/EFTA countries, EU-13 countries and elsewhere in Europe but practising in the eight sample countries increased between 2010 and 2018. The largest proportionate increase of 107% was seen for doctors trained in an EU-13 Member State, with the number of doctors trained in Europe but outside of the EU rising by 97%. The number of doctors trained in (non-European) high-income, upper-middle income and LMIC increased over the same period by approximately 30% for each group, more than double the increase in the total stock of doctors.
Figure 2.
Stock and annual inflow of foreign-trained doctors and nurses by region of training origin (World Bank income or European group), 2010*, 2014 and 2018* in case study countries. Note: *Or nearest year. For foreign-trained doctors: France and Ireland—2011 and 2018, Germany and Switzerland—2010 and 2017; for foreign-trained nurses: UK—2006 and 2018, Switzerland—2010 and 2017. Source: Data reported to Ref. [5]
The rate of growth in the number of foreign-trained doctors practising in case study countries from Europe (including EU Member States) and other high and upper middle-income countries was fastest between 2010 and 2014, but has subsequently slowed. However, the increase in the stock of doctors trained in LMIC between 2014 and 2018 (average annual growth rate of 3.1%) was almost two times higher compared with 2010–14 (average annual growth rate of 1.7%). The increase in the stock of foreign-trained doctors from LMIC was higher between 2014 and 18 compared with 2010–14 in Belgium, France, Germany, Ireland, Norway and the UK. Overall, the largest increase between 2010 and 2018 in both percentage and absolute terms in the number of foreign-trained doctors from LMIC was seen in Germany.
From 2014 to 2018 a 2-fold increase in the annual inflow of doctors trained in LMIC was seen (figure 2 and Supplementary figure S4). At the same time, the annual inflow of doctors trained in EU Member states and elsewhere in Europe has fallen, leading to a rise in the share of foreign-trained doctors from LMIC.
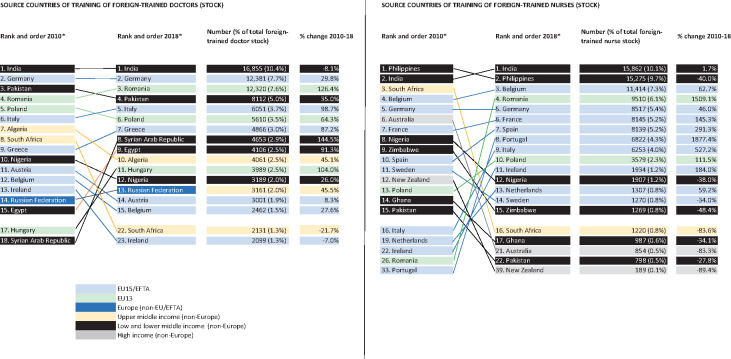
LMIC and EU member states are leading source countries for foreign-trained doctors
Pooled data from case study countries show that India, Germany, Romania, Pakistan and Italy were the top five countries of training for foreign-trained doctors in 2018 (figure 3). Declines in the stock of foreign-trained doctors from India and South Africa were seen between 2010 and 2018 (figure 3), driven by a fall in numbers practising in Ireland and the UK. A rise of over 80% was conversely seen for doctors trained in a number of countries, including: Egypt, Hungary, Romania, Syrian Arab Republic, Greece and Italy.
Figure 3.
Top 15 source countries of training origin by rank: foreign-trained doctors and nurses (stock) 2010 and 2018*. Note: *Or nearest available year. Data from eight case study countries for foreign-trained doctors (Austria, Belgium, France, Germany, Ireland, Norway, Switzerland and UK); data from five case study countries for foreign-trained nurses (Belgium, France, Norway, Switzerland and UK). Source: Data reported to Ref [5]
The countries of destination for foreign-trained doctors from the top 15 most common countries of training origin in 2018 is shown in Supplementary figure S5. Of those who trained in Algeria and Belgium and now practise in a case study country, the majority do so in France. Of those trained in Egypt, India, Nigeria and Pakistan and now practising in a case study country, most are likely to work in the UK, whereas doctors trained in Austria, Greece, Russian Federation and Syrian Arab Republic are most commonly found in Germany. Like Belgium, Germany is both a top receiving and sending country for foreign-trained doctors; the majority of doctors trained in Germany and now practising in a case study country are in Switzerland. In the majority of case study countries, the largest group of foreign-trained doctors in 2018 were most frequently trained in a neighbouring EU-15/EEA or EU-13 Member States, in particular where languages spoken are the same (e.g. France/Belgium or Austria/Germany/Switzerland; Supplementary table S6). Exceptions include the UK, where the most frequent countries of training were countries with historical colonial ties including India, Pakistan and Ireland, where the most common countries of training origin were Sudan and Pakistan.
Most foreign-trained nurses in case study countries were trained in another EU-15/EFTA country, with the UK as an exception
Table 1 shows that in four of the five case study countries (Belgium, France, Norway and Switzerland), the majority of foreign-trained nurses were trained in another EU-15/EFTA country. However, in the UK, just over one-third of foreign-trained nurses (37 155 of 104 125 foreign-trained nurses) were trained in a LMIC. The number of foreign-trained nurses grew by 29% between 2010 and 2018 in the five case study countries, above the 17% overall growth in the overall stock of nurses (Supplementary table S7). Although Belgium saw a 3-fold rise in the number of foreign-trained nurses, numbers declined by just over 5% in Norway.
From 2010 to 2018, the number of foreign-trained nurses from EU-15/EFTA and EU-13 Member States in case study countries more than doubled, with the majority of this growth occurring between 2010 and 2014, The number of nurses trained in non-European higher, upper and lower middle-income countries conversely declined from 2010 to 2018 (figure 2). Much of the fall in the number of nurses trained in upper and lower middle-income countries appears to be related to a reduction of almost 22 000 in nurses from these areas residing in the UK. However, interpreting trends in the region overall is challenging due to a doubling in the number of countries of training classified as ‘other’ across all case study countries.
It should be noted that since 2016 a steady increase in the annual inflow of nurses from LMIC into case study countries has been seen, while the number from EU Member States has declined, which may see the above trends reversed in the future (Supplementary figure S8). Changes in the annual inflow of nurses have been driven by an increase in nurses from LMIC (in particular from India and the Philippines, two countries with which the UK has bilateral agreements in place regarding nurse recruitment) and a fall in nurses trained in the EU arriving in the UK since 2016.
LMIC and EU member states are leading source countries for foreign-trained nurses
India, Philippines, Belgium, Germany and Romania were the top five countries of training for foreign-trained nurses in case study countries in 2018 (figure 3). Nurses trained in Australia, Ghana, Nigeria, Philippines, South Africa and Zimbabwe decreased from 2010 to 2018, primarily due to a decline in these individuals residing in the UK. A substantial rise in the mobility of nurses trained in France, Ireland, Italy, Portugal, Romania and Spain was, however, seen in particular from 2010 to 2014, with growth subsequently slowing considerably from 2014 to 2018, and in some cases (Ireland and Spain) even declining.
Nurses trained in the most common LMIC of training origin were most likely to reside in the UK, whereas those trained in Europe were most likely to reside in a neighbouring country (Supplementary figure S9). As is the case with foreign-trained doctors, the largest group of foreign-trained nurses in each case study country was trained in a neighbouring EU-15/EEA or EU-13 country (Supplementary table S10). The UK again provides an exception, with the largest groups of foreign-trained nurses trained in India, Philippines and Romania.
Discussion
This article updates information on the stock and inflow of foreign-trained doctors and nurses in Europe and provides one of the most detailed analyses of trends in health worker migration and mobility in the region. We show that in case study countries in Western Europe, the number of foreign-trained doctors and nurses has risen faster than the total stock of these health professionals since 2010, indicating that many countries remain reliant on a foreign-trained workforce. Furthermore, some countries (e.g. Belgium, Germany and Ireland) are both major source and destination countries, whereas others, predominantly EU Member States in the South and East of the region, face a substantial outflow of health workers. It is clear that mobility of health professionals remains an important issue affecting all countries in Europe in some form, ensuring that the principles and objectives of the Global Code of Practice remain highly pertinent in the region.
It is important to emphasize, however, that the countries studied generally appear to adhere to the Code’s core principle of reducing unethical international recruitment from LMIC.1 Although the number of doctors from LMIC has increased by almost 30% since 2010, much of this growth has been driven by arrivals from the Syrian Arab Republic and Egypt, likely as a result of conflict and volatility in these regions contributing to an outflow of health professionals.12,13 Drawing clear conclusions on migration of nurses is complicated by a substantial increase in the number of places of training classified as other, but trends indicate the number of nurses from LMIC has declined. It is also worth noting that some major destination countries (e.g. the UK) have bilateral agreements regarding recruitment practices in place with India and the Philippines, the leading source LMIC for nurses.1,2,14,15
Of course, while these findings overall indicate that European countries have reduced reliance on unethical international recruitment from LMIC, the extent to which this is attributable to implementation of the voluntary Code is difficult to assess given that health worker migration is highly complex and shaped by many different factors and policies. It should also be noted that a considerable increase in the annual inflow of nurses and doctors since 2016 is concerning and should be closely monitored in the coming years.
Although the continuing relevance and importance of the Code to Europe is clear, its application within the EU remains challenging. The fundamental rights of free-movement and mutual recognition of professional qualifications ensure that mobility of health workers within the area maintains primacy over the principles of the Code.16–19 This leaves migration flows heavily influenced by individual preferences, but also by market-based principles and responsive to external shocks.8,20 This was clearly demonstrated in the past by a surge in East–West and South–North mobility following EU enlargement in 2004 and 2007 and the economic crisis in 2008–09, respectively.8,9 Although we find a slight slowdown in the rate of increase in East–West and South–North EU mobility since 2016, potentially linked among other factors to the UK vote to leave the EU (‘Brexit’) and an economic recovery in many countries following the economic crisis, these mobility patterns have largely continued.
These persistent disparities between Member States raise important questions over the equity and efficiency of health systems in the EU as noted in previous studies,16,17 and challenges Member States to consider the broader requirements of the Code in order for it to function within the EU regulatory environment. For instance, growing and strengthening the domestic health workforce, as emphasized by the Code and the WHO’s recent Global workforce strategy 2030,21 will help address many of the push and pull factors of health worker migration. Providing financial and technical support and coordinating training and education through bilateral agreements and joint action at the EU-level can also ensure that health worker migration benefits both source and destination countries, while respecting the right to individual mobility and professional development.16,17
Strengthening research and data gathering on health worker mobility also remains critical for developing appropriate policy responses. While significant progress has been made in recent years, 22 primarily non-EU countries in the East of the region did not report data in the 2019 wave of joint data collection. Where data were reported, it was often not complete across years or specific indicators (particularly country of training). Going forward, continuing efforts are needed to improve the completeness and quality of data reporting within the Joint Questionnaire cycle by, for instance, capturing data on mobility of professions other than doctors and nurses. Data and research on health worker mobility should also strive to capture individual experiences and preferences; understanding the motivations and future migration intentions of individual healthcare workers will be important to determine the drivers of migration and to inform evidence-based policy actions and workforce planning.22
Limitations
Many of the limitations of this article stem from limitations in data reported to the Joint Questionnaire. As already noted, the proportion of training country of origin classified as ‘other’ has increased, in particular for nurses, making it difficult to accurately gauge trends over time. Additionally, data for Germany is based on nationality and not country of training, while Switzerland only reported data for hospital-based nurses. Taken together, these limitations are likely to lead to an underestimation of foreign-trained health workers, in particular for those trained outside of Europe. It is also important to note that while this article assesses trends over time in health worker mobility since the adoption of the Code in 2010, it does not determine causality between the Code’s implementation and subsequent trends in health worker migration from LMIC. Migration of health workers is a highly complex issue shaped by domestic and international policies, unexpected shocks (e.g. the economic crisis, conflict in other regions etc), personal motivations and other factors beyond the Code.
Conclusion
The principles of the WHO Code remain relevant within Europe, with countries either reliant on a foreign-trained workforce or facing a large outflow of health professionals. Adherence within the EU regulatory environment is challenging, but can be achieved by Member States considering the Code’s broader principles to strengthen the domestic health workforce through evidence-based policy and planning, underpinned by comprehensive human resources for health information systems. This will ultimately support development of a sustainable workforce that can deliver equitable, high-quality healthcare and advance progress towards universal health coverage throughout the region.
Supplementary Material
Acknowledgements
The data used in this article are collected through the Joint OECD/EUROSTAT/WHO-EUROPE data collection on non-monetary healthcare statistics. We would like to express our gratitude to the data providers in countries and colleagues at Eurostat and OECD for this collaborative effort.
Disclaimer
The authors are staff members of the World Health Organization. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Conflicts of interest: None declared.
Key points
The WHO Code of Practice remains pertinent in Europe, with many countries facing a substantial outflow or relying on foreign-trained health professionals.
Countries generally adhere to the Code’s core principle of reducing unethical international recruitment from low- and middle-income countries, but the extent to which a reduction is directly attributable to the Code’s implementation is difficult to assess.
Adherence within the European Union regulatory environment can be achieved by Member States considering the Code’s wider principles.
Data reporting on health worker mobility should be strengthened to support evidence-based health workforce policies.
References
- 1.World Health Organization. WHO Global Code of Practice on the International Recruitment of Health Personnel. Geneva: World Health Organization, 2010. [Google Scholar]
- 2.World Health Organization. User’s Guide to the WHO Global Code of Practice on the International Recruitment of Health Personnel. Geneva: World Health Organization, 2011. [Google Scholar]
- 3. Siyam A, Zurn P, Rø OC, et al. Monitoring the implementation of the WHO Global Code of Practice on the International Recruitment of Health Personnel. Bull World Health Organ 2013;91:816–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO Global Code of Practice on the International Recruitment of Health Personnel: second round of national reporting. Report by the Secretariat, Sixty-Ninth World Health Assembly A69/37. 2016. Available a: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_37-en.pdf?ua=1 (31 May 2020, date last accessed)
- 5.OECD/Eurostat/World Health Organization Europe Office. Guidelines for completing the OECD/EUROSTAT/WHO-Europe Questionnaire 2020. Joint Data Collection on Non-monetary health care statistics, 2019. Available at: https://www.oecd.org/statistics/data-collection/Health%20Data%20-%20Guidelines%202.pdf (31 May 2020, date last accessed)
- 6. Lafortune G, Socha-Dietrich K, Vickstrom E. Recent trends in international mobility of doctors and nurses In: OECD, editor. Recent Trends in International Migration of Doctors, Nurses and Medical Students. Paris: OECD, 2019. [Google Scholar]
- 7.OECD. Changing patterns in the international migration of doctors and nurses to OECD countries In: International Migration Outlook 2015. Paris: OECD, 2015. [Google Scholar]
- 8. Buchan J, Wismar M, Glinos I, Bremner J. Health Professional Mobility in a Changing Europe. Copenhagen: World Health Organization, (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies), 2014. [Google Scholar]
- 9. Wismar M, Maier C, Glinos I, et al. Health Professional Mobility and Health Systems. Evidence from 17 European Countries. Copenhagen: World Health Organization, (on behalf of the European Observatory on Health Systems and Policies) , 2011. [Google Scholar]
- 10.European Commission. Healthcare non-expenditure statistics – methodology 2015. Available at: https://ec.europa.eu/eurostat/statistics-explained/index.php/Healthcare_non-expenditure_statistics_-_methodology#Main_features (15 May 2020, date last accessed).
- 11. Schwendimann R, Ausserhofer D, Schubert M, et al. Switzerland In: Rafferty AM, Busse RB, Zander-Jentsch B, et al. editors. Strengthening Health Systems through Nursing: Evidence from 14 European Countries. Health Policy Series, No. 52. Copenhagen: World Health Organization, (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies), 2019. [PubMed] [Google Scholar]
- 12. Abbara A, Rayes D, Omar M, et al. Overcoming obstacles along the pathway to integration for Syrian healthcare professionals in Germany. BMJ Glob Health 2019;4:e001534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bou-Karrou L, Daou K, Nomier M, et al. Health care workers in the setting of the ‘Arab Spring’: a scoping review for the Lancet-AUB Commission on Syria. J Glob Health 2019;9:010402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Koff SZ. Nursing in the European Union Anatomy of a Profession, Vol. 1 New Brunswick: Transaction Publishers, 2016. [Google Scholar]
- 15. Dhillon I, Clark M, Kapp R. Innovations in Cooperation: A Guidebook on Bilateral Agreements to Address Health Worker Migration. Washington DC: Aspen Institute, 2010. [Google Scholar]
- 16. Glinos I. Health professional mobility in the European Union: exploring the equity and efficiency of free movement. Health Policy 2015;119:1529–36. [DOI] [PubMed] [Google Scholar]
- 17. Glinos I, Wismar M, Buchan J, Rakovac I. How can countries address the efficiency and equity implications of health professional mobility in Europe? In: Adapting Policies in the Context of the WHO Code of Practice and EU Freedom of Movement. Copenhagen: World Health Organization, (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies), 2015. [PubMed] [Google Scholar]
- 18.Directive 2005/36/EC of the European Parliament and of the Council of 7 September 2005 on the recognition of professional qualifications (Text with EEA relevance), European Parliament, Council of the European Union, 2005.
- 19.Directive 2013/55/EU of the European Parliament and of the Council of 20 November 2013 amending Directive 2005/36/EC on the recognition of professional qualifications and Regulation (EU) No 1024/2012 on administrative cooperation through the Internal Market Information System (the IMI Regulation). Text with EEA relevance, European Parliament, Council of the European Union, 2013.
- 20. Leone C, Bruyneel L, Anderson JE, et al. Work environment issues and intention to leave in Portuguese nurses: a cross-sectional study. Health Policy 2015;119:1584–92. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva: World Health Organization, 2016. [Google Scholar]
- 22. Kuhlmann E, Batenburg R, Wismar M, et al. A call for action to establish a research agenda for building a future health workforce in Europe. Health Res Policy Syst 2018;16:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.