LETTER
The COVID-19 pandemic is an unprecedented situation with physicians awaiting information on therapeutic advances to an extent hardly ever seen in medical history. In the context of this medical crisis, we here exemplify the rapidity by which dissemination of scientific data impacts real-life medical prescriptions.
In Strasbourg University Hospital, France, which was severely affected by the SARS-CoV-2 epidemic at the beginning of March 2020, we analyzed the consumption of antiviral agents according to the emergence of relevant scientific data. At this time, no medically evaluated standard treatment was available, and so, the need for information was vital. The treatment strategies in our center, outside clinical trials, included standard of care alone or in combination with lopinavir-ritonavir or hydroxychloroquine (HCQ) in off-label utilization and without grading of the recommendations. This strategy was in accordance with the French recommendations.
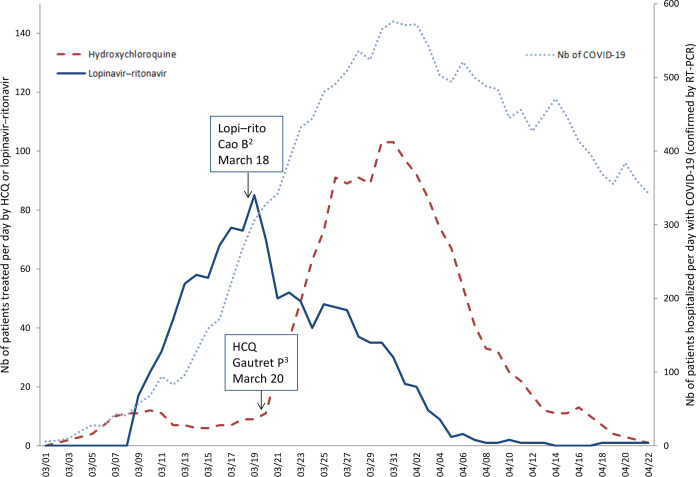
The first patients were treated with standard care alone or in combination with lopinavir-ritonavir (Fig. 1). This treatment had shown some efficacy in nonrandomized trials on SARS-CoV and Middle East respiratory syndrome (1). Moreover, the drug was available, and side effects were known. Data on the first randomized clinical trial appeared online on 18 March and showed no benefit of lopinavir–ritonavir (2). This information triggered a quick decrease in our prescriptions, despite the increase of COVID-19 cases.
FIG 1.
Consumption of lopinavir-ritonavir and hydroxychloroquine from 1 March 2020 to 22 April 2020 at Strasbourg University Hospital. The x axis represents the date (month/day, 2020). The left y axis represents the number of patients treated per day by hydroxychloroquine or lopinavir-ritonavir. The right y axis shows the number of patients hospitalized per day with COVID-19. Six patients had been treated by remdesivir (compassionate use). Since 25 March, 102 patients have been included in randomized clinical trials (data not shown). HCQ, hydroxychloroquine; Lopi–rito, lopinavir-ritonavir; Nb, number.
On 20 March, a nonrandomized open-label study on 26 patients treated with hydroxychloroquine (6 patients also received azithromycin) showed some efficacy in decreasing viral load compared with controls (3). This study was widely shared in the French media. On the same day, the president of the United States, Donald Trump, declared that he had a good feeling about this drug. Despite the major limitations of this study—including no outcome data on clinical efficacy or safety, the small number of patients enrolled, and the absence of randomization—we experienced a dramatic increase in our HCQ prescriptions following this publication (Fig. 1). The use of azithromycin had the same trend (data not shown).
In April, HCQ prescriptions decreased for several reasons, including the publication of “negative” studies, the increase in serious adverse events reported, inclusion of some of our patients in clinical trials, and a decrease of new COVID-19 cases (4, 5). Following the publication of a large observational study on 22 May showing no beneficial effect of HCQ, this treatment regimen is not authorized anymore in France outside clinical trials (6). Two weeks later, this article was retracted.
During the emergence of this life-threatening pandemic, developing treatment strategies for COVID-19 is challenging with so little relevant scientifically supported data at hand. Remarkably, we observed that all relevant scientific publications, even if they had important limitations, had rapid and major impacts on the prescription of antivirals. Information flowed quickly, especially when amplified by traditional media, which seems to greatly influence medical prescriptions. Decisively, the results of ongoing randomized clinical trials are urgently needed to define standard treatment as well as novel approaches (7).
ACKNOWLEDGMENTS
F.D. declares personal fees from Gilead outside the submitted work. Y.H. declares personal fees from Gilead and Sanofi outside the submitted work. Y.R., M.F., C.K., N.L., J.M., and T.N. have nothing to declare.
F.D. designed the study and had full access to all of the data. All authors have collected and interpreted the data. F.D. wrote the first draft of the manuscript, and all authors have critically revised the manuscript.
We received no financial support.
REFERENCES
- 1.Chu CM, Cheng VCC, Hung IFN, Wong MML, Chan KH, Chan KS, Kao RYT, Poon LLM, Wong CLP, Guan Y, Peiris JSM, Yuen KY, HKU/UCH SARS Study Group . 2004. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax 59:252–256. doi: 10.1136/thorax.2003.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, Ruan L, Song B, Cai Y, Wei M, Li X, Xia J, Chen N, Xiang J, Yu T, Bai T, Xie X, Zhang L, Li C, Yuan Y, Chen H, Li H, Huang H, Tu S, Gong F, Liu Y, Wei Y, Dong C, Zhou F, Gu X, Xu J, Liu Z, Zhang Y, Li H, Shang L, Wang K, Li K, Zhou X, Dong X, Qu Z, Lu S, Hu X, Ruan S, Luo S, Wu J, Peng L, Cheng F, Pan L, Zou J, Jia C, Wang J, Liu X, Wang S, Wu X, Ge Q, He J, Zhan H, Qiu F, Guo L, Huang C, Jaki T, Hayden FG, Horby PW, Zhang D, Wang C. 2020. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med 382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gautret P, Lagier J-C, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S, Colson P, Chabrière E, La Scola B, Rolain J-M, Brouqui P, Raoult D. 2020. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Molina JM, Delaugerre C, Le Goff J, Mela-Lima B, Ponscarme D, Goldwirt L, de Castro N. 2020. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Med Mal Infect 50:384. doi: 10.1016/j.medmal.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borba MGS, Val FFA, Sampaio VS, Alexandre MAA, Melo GC, Brito M, Mourão MPG, Brito-Sousa JD, Baía-da-Silva D, Guerra MVF, Hajjar LA, Pinto RC, Balieiro AAS, Pacheco AGF, Santos JDO, Naveca FG, Xavier MS, Siqueira AM, Schwarzbold A, Croda J, Nogueira ML, Romero GAS, Bassat Q, Fontes CJ, Albuquerque BC, Daniel-Ribeiro C-T, Monteiro WM, Lacerda M, CloroCovid-19 Team . 2020. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Netw Open 3:e208857. doi: 10.1001/jamanetworkopen.2020.8857. [DOI] [PubMed] [Google Scholar]
- 6.Mehra MR, Desai SS, Ruschitzka F, Patel AN. 2020. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet doi: 10.1016/S0140-6736(20)31180-6 [Retraction, .] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Li H, Zhou Y, Zhang M, Wang H, Zhao Q, Liu J. 2020. Updated approaches against SARS-CoV-2. Antimicrob Agents Chemother 64:e00483-20. doi: 10.1128/AAC.00483-20. [DOI] [PMC free article] [PubMed] [Google Scholar]