Abstract
Introduction
Despite declines of cigarette use in the civilian population, military personnel report alarmingly high rates of cigarette use. Enlisted Air Force recruits are required to remain tobacco-free for the first 12 weeks of training, and the majority express confidence they will not use tobacco after the ban; however, most previous smokers return to smoking and many nonsmokers initiate. Understanding the factors associated with cigarette-smoking initiation among non-users and re-initiation among former users is critical for the development of successful tobacco control efforts.
Materials and Methods
The current study examines predictors of cigarette smoking among a sample of 2,188 USAF personnel after their first year of service. Logistic regression analyses examined associations between baseline predictors and initiation and re-initiation of cigarette smoking at a one-year follow-up.
Results
Compared to never smokers at both time points, the strongest predictor of smoking initiation over the past 12 months was having owned cigarette-branded merchandise (OR 3.81, 95% CI 1.67, 8.71). Compared to former smokers who remained abstinent, the strongest predictor of re-initiation was intention to use tobacco (OR 2.08, 95% CI 1.53, 2.83). Compared to individuals who initiate, the strongest predictors of re-initiation were prior use of other tobacco products and tobacco use intentions (ORs range 1.85 to 4.63).
Conclusions
Multiple risk factors are associated with tobacco use. Given that Airmen are tobacco-free for the first 12 weeks of training, tobacco interventions during this period might be more effective. Our findings can be used to tailor interventions to prevent tobacco use in the U.S. military.
Keywords: Smoking, Military Personnel, Tobacco Use, Prevention
INTRODUCTION
While national rates of cigarette use have declined in recent years,1 the prevalence remains high among active duty military personnel. Twenty-four percent of active duty military personnel report current cigarette smoking, compared to 18% among civilians.1,2 In comparison, it was nearly 20 years ago that rates of cigarette use were that high in the civilian sector.2 Given the Department of Defense spends an average of $1.6 billion treating tobacco-related morbidity among active-duty military personnel (e.g., medical care, hospitalizations, lost work days),3 it is critical that effective interventions are developed targeting military personnel.
Throughout the 8½ weeks of Basic Military Training (BMT), Air Force recruits are required to remain alcohol- and tobacco-free. Following successful completion of BMT, recruits become Airmen (so-called regardless of gender or rank) and advance to Technical Training to acquire skills for their designated U.S. Air Force (USAF) job (e.g., aircraft maintenance) for 2 weeks to 18 months, depending on the career field. For the first 4 weeks of Technical Training, Airmen remain alcohol- and tobacco-free. During this period, research indicates 63% of Airmen report they are “completely confident” they will remain tobacco-free.4 And yet, despite this intention and the established anti-tobacco regulations on all military bases,5 the majority of former smokers relapse during Technical Training when allowed to use tobacco. In a previous study, we found that 12.6% of individuals who never smoked initiated cigarette smoking during their first year of service, and 62.6% re-initiated cigarette smoking.6 Of particular relevance is that over half of this initiation and re-initiation is occurring shortly after the tobacco ban is lifted in Technical Training. Unfortunately, very little research exists examining reasons for smoking initiation among military personnel.
Green et al., found Airmen were more likely to initiate tobacco if they perceived smoking to be normative among peers, their roommate smoked, or their Military Training Leaders or instructors used tobacco.7 This cross-sectional study, however, did not assess which baseline characteristics predicted tobacco initiation and re-initiation by Airmen. Moreover, prior attempts to prevent tobacco initiation among Airmen have been unsuccessful.8,9 A greater understanding of factors associated with smoking following enlistment could guide development of effective interventions to decrease tobacco-use onset during Technical Training. Knowledge of predictive factors may provide a starting place to understand tobacco use initiation or re-initiation among active duty personnel in other branches of the military as well.
This study sought to fill this gap by examining factors associated with cigarette smoking and smoking abstinence among individuals 12 months after joining the USAF. We conducted our analyses in a cohort of 2,188 USAF enlistees as a first step in understanding how to reduce tobacco use during military training.
METHODS
Participants and Procedures
Participants were USAF Technical Trainees from Joint Base San Antonio – Lackland in training between March 2011 and July 2013 in San Antonio, TX. Airmen consented for this study during a standard, group-based brief alcohol intervention (BAI),9 given to all Technical Trainees during the first week of Technical Training, while they are still tobacco free. Both the 59th Medical Wing Institutional Review Board at Wilford Hall Ambulatory Surgical Center and the University of Tennessee Health Science Center Institutional Review Board approved the protocol.
Airmen were convened by squadron (i.e., a group of Airmen undergoing Technical Training together). After the BAI, 8,943 Airmen were presented with a study description. 76.9% of Airmen (N = 6,880) consented to participate and completed the baseline questionnaire. The 1-year follow-up was completed among active duty Airmen stationed at bases within the Continental United States and Hawaii. 1,349 non-active duty Airmen (i.e., National Guard [n = 655 or Reserve [n = 694]) were identified and excluded from the follow-up assessment. Of the remaining 5,531 Active Duty Airmen, 35% were assumed to be ineligible due to being overseas, separated, deployed, incarcerated, switched service branches or deceased. Therefore, Airmen were oversampled using a random sampling procedure to achieve a 35% follow-up rate.
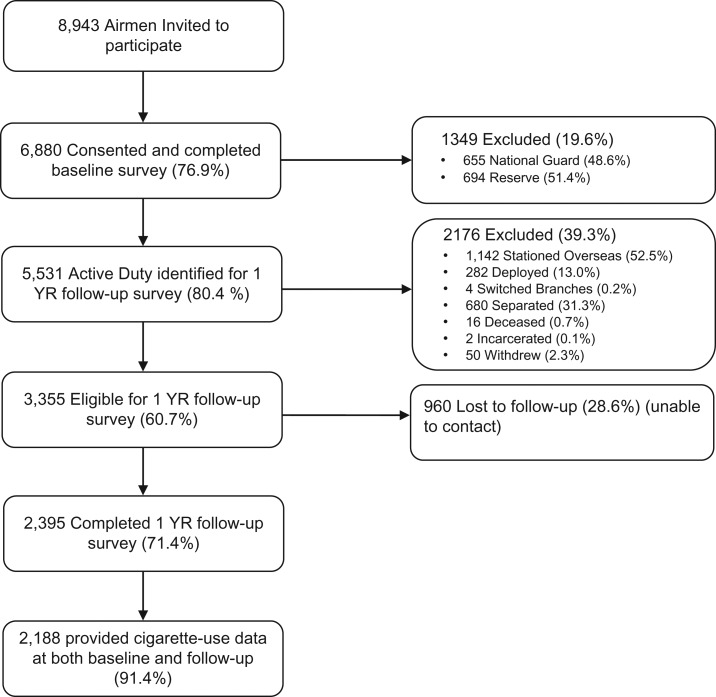
One month prior to the projected follow-up date, a list of participants was sent to the Defense Manpower Data Center (DMDC). DMDC returned current contact information for participants, who were invited to complete the follow-up. Airmen were ineligible for follow-up due to being stationed overseas (n = 1,142), deployed (n = 282), switched to a different military branch (n = 4), separated from the USAF (n = 680), deceased (n = 16), or incarcerated (n = 2). An additional 2.3% (N = 50) Airmen withdrew from the study. The one-year assessment was completed by 2,395 (71.4%) eligible Airmen, with 97% of participants responding by phone (N = 2,323) and 3% by email (N = 72). Our final analytic sample only included the 2,188 Airmen who provided cigarette-use data at both baseline and follow-up (see Figure 1).
FIGURE 1.
Flowchart of participants in cohort.
Baseline Questionnaire
The baseline questionnaire assessed four domains: demographics, tobacco-use prevalence (e.g., cigarettes, smokeless tobacco, cigars), intrapersonal factors (e.g., perceived harm), and interpersonal factors (e.g., peer use).
Demographic variables included age (<21 or ≥21 years old, dividing the sample at the mean age), BMI (weight/height2), gender (female, male), marital status (not married, married), ethnicity (non-Hispanic, Hispanic), race (white, black, Asian, other, multiple), education (high school graduate/GED/vocational training post-high school, at least some college), and residence prior to BMT (South, Northeast, Midwest, West).
Tobacco-use prevalence was assessed by asking history of using cigarettes, smokeless tobacco, or cigars prior to BMT (since all Airmen were tobacco-free when surveyed). Response options ranged from “I smoked/used (tobacco product) every day and I smoked/used (tobacco product) (amount) per day/per week”, “I didn’t use (tobacco product) every day, but I used at least once a week”, “I didn’t use (tobacco product) every week but I used at least once a month”, “I used (tobacco product) less than once a month”, “I didn’t use (tobacco product)”, “I used (tobacco product) but quit prior to BMT.” Pre-BMT history of cigars and smokeless tobacco were recoded into dichotomous variables (did not use, any use [including quit prior to BMT]). Dual use was defined as a history of using two tobacco products before BMT (No/Yes). Never use at baseline was defined as no use of a tobacco product before BMT.
To assess intrapersonal factors, Airmen were asked about intentions to use tobacco, perceived harm of tobacco, and beliefs regarding tobacco. Intentions were assessed through three items: intentions to use tobacco after Technical Training (plan to remain tobacco free, thinking about using tobacco, definitely will use tobacco), and would use product that claims to be safer than cigarettes (No/Yes) and will use tobacco to help me meet weight standards in the military (No/Yes). Beliefs were assessed by asking Airmen if they agree Tobacco restrictions in BMT/Technical Training are a great way to keep people tobacco free (Strongly disagree = 1 to Strongly agree = 5). Lastly, Airmen were asked if they owned at least one item (e.g., t-shirt, hat) with cigarette advertising on it (No/Yes).
Interpersonal factors were assessed by asking about peer, BMT Military Training Instructors (MTIs), and family/roommate use. Peer use assessed how many of their closest friends smoked cigarettes (None = 0 to Almost all, 80% or more = 4); 7.13% (N = 156) reported almost all, 80% or more. BMT MTI use variable was created by taking a mean of three items asking Airmen the number of BMT MTIs who used each tobacco product (cigarettes, smokeless tobacco or both) (I don’t know = 0 to Almost all, 80% or more = 6 [3 items; α = 0.78]). Family/Roommate use was assessed by asking Airmen if they lived with someone who regularly used (cigarettes, smokeless tobacco or both) prior to BMT (No/Yes).
Follow-up Questionnaire
Cigarette use prevalence was assessed by asking Airmen about their cigarette use over the year since joining the USAF. Responses options were the same as the baseline responses.
Statistical Analysis
Descriptive statistics of demographic and tobacco variables at baseline were computed separately by cigarette-use status at one-year follow-up. In order to determine whether factors that predict cigarette use among one group was common across all, which aids in selecting behavioral targets for interventions, we created four cigarette-use status categories (N = 2,188): (1) individuals who never used (no cigarette use prior to BMT and no cigarette use in the previous 12 months at follow-up; N = 1,422, 65%); (2) individuals who initiated (no cigarette use prior to BMT and at least some (i.e., less than monthly to daily) cigarette use in the previous 12 months at follow-up; N = 204, 9.3%); (3) individuals who formerly used and remained abstinent from cigarettes (lifetime use prior to BMT and no cigarette use in the previous 12 months at follow-up; N = 210, 9.6%); and (4) individuals who re-initiate (lifetime use prior to BMT and at least some cigarette use in the previous 12 months at follow-up; N = 352, 16.1%). Differences in proportions of demographic variables across user groups were calculated using Nonparametric Kruskal–Wallis test for continuous variables and Fisher’s exact test for categorical variables.
Our primary analytical approach is to employ three separated multivariable logistic regression models to assess associations between pre-specified predictors at baseline and cigarette smoking at one year follow up: (Model 1) individuals who initiated vs. individuals who never used; (Model 2) individuals who re-initiate vs individuals who formerly used and remained abstinent from cigarettes; and (Model 3) individuals who re-initiate vs. individuals who initiated. To determine which pre-specified predictors will be included in our final models, we first examined all predictors within each of the four domains in predicting cigarette smoking at the follow up separately, including (a) 8 demographic predictors, (b) 3 tobacco use history predictors, (c) 5 intrapersonal predictors, and (d) 3 interpersonal predictors. Next, if any of the predictors among the four domains reached a statistical significant threshold of p < 0.10, they were included in the final models. Associations were considered significant in the final logistic regression models at the alpha level of 0.05. The area under the receiver operative characteristic (ROC) curve was utilized as a measure of overall predictive discrimination of each of the final models. Data were analyzed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Comparisons between baseline characteristics across the four user categories are presented in Table I. Individuals who initiated tended to be younger, male, non-white, and have less education compared to the other user categories (all ps < 0.05). Individuals who had never smoked reported less use of other tobacco products prior to joining the Air Force compared to other categories (p < 0.0001). These individuals had lower intentions to use tobacco, were less likely to own cigarette-branded merchandise, and were less likely to have reported peer use, MTI use, and history of living with a tobacco user compared to other categories (all ps < 0.05). Additionally, never smokers were more likely to have believed tobacco restrictions during training promoted abstinence (p < 0.0001). There were no differences across user categories in terms of BMI (all ps > 0.05).
Table I.
Baseline Characteristics by Cigarette User Groups at One Year Follow-up (N = 2,188)a
| Individuals who never used (N = 1,422) | Individuals who initiate (N = 204) | Individuals who formerly used (N = 210) | Individuals who re-initiate (N = 352) | p-value | |
|---|---|---|---|---|---|
| Demographic Factors | |||||
| Over 21 yr old | 40.30% | 27.94% | 47.14% | 37.22% | 0.0004 |
| Male | 72.36% | 81.37% | 77.62% | 79.55% | 0.0025 |
| BMIb | 24.16(2.52) | 24.08(2.46) | 24.44(2.55) | 24.02(2.15) | 0.4908 |
| Married | 12.17% | 6.90% | 15.71% | 12.22% | 0.0507 |
| Hispanic | 13.84% | 18.81% | 14.83% | 10.54% | 0.0560 |
| Race | <.0001 | ||||
| White | 66.83% | 65.84% | 78.85% | 77.27% | |
| Black | 17.22% | 12.87% | 5.77% | 5.68% | |
| Asian | 3.67% | 2.97% | 1.92% | 3.13% | |
| Other | 5.43% | 7.92% | 7.21% | 5.11% | |
| More than one race | 6.85% | 10.40% | 6.25% | 8.81% | |
| Some college | 52.19% | 38.73% | 49.52% | 43.18% | 0.0002 |
| State of residence prior to BMT | 0.3997 | ||||
| South | 40.18% | 38.42% | 39.61% | 36.23% | |
| Northeast | 13.21% | 15.76% | 12.08% | 16.23% | |
| Midwest | 20.83% | 23.65% | 27.54% | 25.22% | |
| West | 25.28% | 21.67% | 20.29% | 21.74% | |
| Tobacco Use History | |||||
| Pre-BMT smokeless tobacco use | 7.52% | 11.27% | 38.10% | 36.08% | <.0001 |
| Pre-BMT cigar use | 13.79% | 29.41% | 52.86% | 51.85% | <.0001 |
| Dual use (2 products) | 6.47% | 12.75% | 36.67% | 40.63% | <.0001 |
| Intrapersonal Factors | |||||
| Intentions to Use Tobacco After Technical Trainingb,c | 0.10(0.37) | 0.29(0.55) | 0.40(0.66) | 0.80(0.71) | <.0001 |
| Will use product that claims to be safer than cigarettes | 2.75% | 11.82% | 26.67% | 42.74% | <.0001 |
| Will use tobacco to help me meet weight standards in the military | 1.48% | 9.31% | 12.44% | 28.69% | <.0001 |
| Tobacco restrictions in training promote abstinenceb,d | 3.91(1.11) | 3.49(1.22) | 3.45(1.22) | 2.91(1.27) | <.0001 |
| Own cigarette branded merchandise | 1.55% | 5.39% | 4.76% | 8.24% | <.0001 |
| Interpersonal Factors | |||||
| Peer Useb,e | 1.26(1.02) | 1.65(1.08) | 2.30(1.11) | 2.50(1.04) | <.0001 |
| Military Training Instructor Tobacco Useb,f | 0.60(0.81) | 0.60(0.89) | 0.88(1.11) | 0.70(0.93) | 0.0189 |
| Lived with Tobacco User Prior to BMT | 43.88% | 48.04% | 55.71% | 62.22% | <.0001 |
aAll figures are percentages, unless otherwise noted.
bMean (standard deviation).
cResponses range from 0 to 2.
dResponses range from 1 to 5.
eResponses range from 0 to 4.
fResponses range from 0 to 5.
p-values calculated with Nonparametric Kruskal–Wallis test for continuous variables and Fisher’s exact test for categorical variables.
Table II presents the results from the logistic regression models examining the four domains of predictors of cigarette initiation and re-initiation at the one-year follow-up separately, and these results were also used to build up our final models based on significant threshold at p < 0.10. Compared to never smokers, individuals who initiated were more likely to be under 21, male, identified with more than one race, smoked cigars prior to BMT, intended to use tobacco after Technical Training, intended to use a product that claims to be safer than cigarettes, less likely to have agreed tobacco restrictions in training promoted abstinence, believed tobacco will help them meet military weight standards, own cigarette-branded merchandise, and reported peer tobacco use.
TABLE II.
Logistic Regression Analyses Using Baseline Characteristics to Predict Cigarette Smoking Status at the One Year Follow-up
| Model 1 (Individuals Who Initiated vs. Never Users) | Model 2 (Individuals Who Re-Initiated vs. Former Users) | Model 3 (Individuals who Re-Initiated vs. Individuals who Initiated) | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| A. Demographic predictors | |||
| Over 21 years old | 0.70(0.47,1.04) | 0.64(0.42,0.98) | 1.30(0.82,2.07) |
| Male | 1.87(1.26,2.76) | 1.18(0.76,1.83) | 0.79(0.49,1.26) |
| BMI | 0.99(0.93,1.05) | 0.92(0.85,1.00) | 1.00(0.92,1.08) |
| Married | 0.60(0.33,1.11) | 1.00(0.58,1.72) | 1.94(0.97,3.89) |
| Hispanic | 1.28(0.82,2.01) | 0.65(0.35,1.21) | 0.48(0.27,0.84) |
| Race | |||
| White | 1.00 (ref) | 1.0 (ref) | 1.00 (ref) |
| Black | 0.83(0.53,1.32) | 1.02(0.46,2.27) | 0.33(0.17,0.64) |
| Asian | 0.95(0.39,2.29) | 3.64(0.78,17.01) | 0.79(0.27,2.27) |
| Other | 1.47(0.78,2.78) | 1.04(0.45,2.36) | 0.70(0.32,1.55) |
| More than one race | 1.65(0.95,2.85) | 1.54(0.73,3.25) | 0.87(0.45,1.66) |
| Some college | 0.76(0.53,1.09) | 0.95(0.63,1.42) | 0.96(0.63,1.46) |
| State of residence prior to BMT | |||
| South | 1.00 (ref) | 1.0 (ref) | 1.00 (ref) |
| Northeast | 1.23(0.78,1.95) | 1.39(0.79,2.44) | 0.98(0.57,1.68) |
| Midwest | 1.25(0.84,1.86) | 0.97(0.61,1.53) | 0.92(0.57,1.48) |
| West | 0.82(0.55,1.24) | 1.10(0.67,1.80) | 1.06(0.64,1.75) |
| B. Tobacco use predictors | |||
| Pre-BMT smokeless use | 1.26(0.75,2.10) | 0.96(0.66,1.39) | 4.59(2.71,7.77) |
| Pre-BMT cigar use | 2.62(1.75,3.91) | 1.04(0.73,1.49) | 1.58(1.04,2.41) |
| Dual use (2 products) | 0.95(0.53,1.68) | 1.17(0.81,1.70) | 4.94(3.04,8.05) |
| C. Intrapersonal predictors | |||
| Intentions to use tobacco after technical training | 1.42(0.99, 2.01) | 1.73(1.23, 2.43) | 2.04(1.38, 3.01) |
| Will use product that claims to be safer than cigarettes | 1.98(1.06,3.72) | 1.16(0.75,1.79) | 2.90(1.71,4.93) |
| Will use tobacco to help me meet weight standards in the military | 2.79(1.33,5.87) | 1.40(0.81,2.44) | 1.34(0.71,2.52) |
| Tobacco restrictions in training promote abstinence | 0.82(0.72,0.94) | 0.81(0.69,0.95) | 0.86(0.73,1.01) |
| Own cigarette branded merchandise | 2.98(1.35,6.56) | 1.36(0.62,2.99) | 1.17(0.53,2.59) |
| D. Interpersonal predictors | |||
| Peer use | 1.41(1.23, 1.62) | 1.23(1.04, 1.45) | 2.05(1.70, 2.46) |
| Military training instructor tobacco use | 0.97(0.81,1.16) | 0.81(0.68,0.96) | 1.02(0.83,1.26) |
| Lived with tobacco user prior to BMT | 1.01(0.75,1.37) | 1.26(0.89,1.80) | 1.37(0.94, 2.00) |
Note: Odds Ratios p < 0.10 are highlighted in bold.
The results of the analyses comparing individuals who re-initiate cigarettes and former smokers showed individuals who re-initiate were more likely to be under 21, had a lower BMI, had higher intentions to use tobacco, were less likely to have believed training tobacco restrictions promote abstinence, reported peer tobacco use and reported MTI use compared to former users.
Compared to individuals who initiate, individuals who re-initiate were more likely to be married, non-Hispanic, less likely to be black, previously used smokeless tobacco, smoked cigars, reported dual-tobacco use, intended to use tobacco after Technical Training, used a product that claims to be safer than cigarettes, and reported peer tobacco use, and less likely to have believed tobacco restrictions in training promoted abstinence.
Table III presents the results of the final multivariable models, including those predictors from the four domains reached significant threshold at p < 0.10. In the final model comparing individuals who initiate with never users, individuals who initiated were more likely to be male, identify as other race or more than one race, have smoked cigars prior to BMT, used a product claiming to be safer than cigarettes, used tobacco to meet military weight standards, less likely to have agreed tobacco restrictions in training promote abstinence compared to never users, owned cigarette-branded merchandise and reported peer use of tobacco (all ps < 0.05; ROC = 0.72). Results comparing individuals who re-initiate and former users showed individuals who re-initiate were more likely to have had a lower BMI, be less likely to intend to use tobacco after Technical Training, less likely to agree tobacco restrictions in training promoted abstinence and less likely to report MTI use (all ps < 0.05; ROC = 0.72). Comparing individuals who initiated to individuals who re-initiated, individuals who re-initiated were more likely to be female, had used smokeless tobacco prior to BMT, reported dual tobacco use, intended to use tobacco after Technical Training, intended to use a product that claimed to be safer than cigarettes and reported peer use of tobacco (all ps < 0.05; ROC = 0.85).
TABLE III.
Final Multivariable Models: Demographics, Intrapersonal and Interpersonal Variables Predicting Cigarette Smoking at One Year Follow up (significant at p < 0.05)
| Model 1 (Individuals Who Initiated vs. Never Users) | Model 2 (Individuals Who Re-Initiated vs. Former Users) | Model 3 (Individuals who Re-Initiated vs. Individuals who Initiated) | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Over 21 | 0.74(0.49,1.12) | 0.79(0.51,1.24) | 1.57(0.90,2.74) |
| Male | 1.68(1.11,2.54) | 0.98(0.61,1.56) | 0.46(0.26,0.81) |
| BMI | 0.95(0.89,1.02) | 0.89(0.82,0.97) | 0.96(0.87,1.06) |
| Married | 0.56(0.29,1.08) | 1.01(0.57,1.80) | 2.07(0.86,4.99) |
| Hispanic | 1.41(0.88,2.27) | 0.73(0.38,1.41) | 0.62(0.31,1.25) |
| Race | |||
| White | 1.00 (ref) | 1.0 (ref) | 1.00 (ref) |
| Black | 1.02(0.62,1.65) | 1.50(0.65,3.49) | 0.54(0.24,1.24) |
| Asian | 1.38(0.56,3.39) | 4.57(0.92,22.76) | 1.59(0.45,5.57) |
| Other | 1.98(1.03,3.80) | 1.04(0.43,2.51) | 1.10(0.43,2.79) |
| More than one race | 1.91(1.08,3.39) | 1.47(0.67,3.20) | 0.64(0.29,1.4) |
| Some college | 0.81(0.55,1.18) | 1.05(0.69,1.61) | 1.23(0.74,2.04) |
| State of residence prior to BMT | |||
| South | 1.00 (ref) | 1.0 (ref) | 1.00 (ref) |
| Northeast | 1.22(0.75,1.98) | 1.54(0.84,2.82) | 0.90(0.46,1.76) |
| Midwest | 1.16(0.76,1.77) | 1.03(0.63,1.68) | 0.84(0.46,1.51) |
| West | 0.83(0.54,1.27) | 1.14(0.68,1.92) | 1.38(0.73,2.59) |
| Pre-BMT smokeless use | -- | -- | 2.27(1.22,4.20) |
| Pre-BMT cigar use | 1.83(1.21,2.76) | -- | 1.39(0.83,2.31) |
| Dual use (2 products) | -- | -- | 4.36(2.54,7.49) |
| Intentions to Use Tobacco After Technical Training | 1.19(0.81,1.76) | 2.02(1.48,2.75) | 1.83(1.18,2.83) |
| Will use product that claims to be safer than cigarettes | 2.02(1.07,3.83) | -- | 2.41(1.32,4.40) |
| Will use tobacco to help me meet weight standards in the military | 3.09(1.43,6.67) | -- | -- |
| Tobacco restrictions in training promote abstinence | 0.85(0.74,0.97) | 0.79(0.68,0.93) | 0.95(0.78,1.15) |
| Own cigarette branded merchandise | 3.69(1.61,8.46) | -- | -- |
| Peer Use | 1.30(1.12,1.51) | 1.18(0.98,1.41) | 1.92(1.55,2.37) |
| Military Training Instructor Tobacco Use | -- | 0.77(0.64,0.94) | -- |
Note: Predictors from Table II that were p < 0.10 were included in the final multivariable models. Odds Ratios significant at p < 0.05 are highlighted in bold.
DISCUSSION
Previous research has documented as much as 15% of active-duty personnel initiate cigarette smoking after enlistment.10 The majority of this initiation may occur during advanced training as is the case with Airmen during their Technical Training;6 however, little is known about the factors that encourage tobacco use in the training environment. The present study investigated predictors of cigarette smoking among a sample of Airmen during their first year of service.
Males were more likely to be individuals who initiated while females were more likely to be individuals who re-initiated. This is in contrast to previous findings that women were more likely to initiate at age 20 or older compared to men.11,12 We found no geographical differences between user categories in contrast to previous research which indicates greater rates of smoking in the Midwest.13 Interestingly, having a lower BMI was predictive of cigarette-smoking re-initiation, perhaps indicating concern about post-cessation weight gain; however there were no differences between user categories in terms of BMI at baseline. It is possible that because this is a young population, age-related weight gain has yet to accumulate among smokers and non-smokers. Cigarette smokers commonly report smoking to control body weight.14 Smoking reduces aging-related weight gain, resulting in larger differences in body weight between smokers and non-smokers.15 Previous focus groups with military populations reported smoking was viewed as an effective method to avoid weight gain.16 Similarly, in the current study, believing tobacco would assist in meeting the military’s weight standards was predictive of smoking initiation compared to never users. Military personnel are required to pass a fitness test as part of their yearly performance evaluation. Failure results in probation and possible discharge from the military. Unfortunately, cigarette use impairs military-readiness through diminished physical performance and endurance long-term;17 thus, it is important that efforts to reduce tobacco use also address weight concerns. Adding a weight management component to Technical Training (including correcting misperceptions regarding smoking, fitness, and body weight, as well as helping develop healthy nutrition habits) could improve smoking rates and the overall health of the USAF.
Willingness to use a tobacco product that claims to be safer than cigarettes and lifetime use of other tobacco products were associated with both initiation and re-initiation. Previous research found a high prevalence of dual- and poly-tobacco use among USAF recruits.18 Over half of tobacco users reported using more than one tobacco product; the most common combination of three products was cigarettes, cigarillos, and hookah.18 Unfortunately, very little is known about treating dual- and poly-tobacco-use dependence, and even less is known about these behaviors in the military.
Owning cigarette-branded merchandise prior to joining the USAF was the strongest predictor of cigarette initiation. Previous research consistently observed owning cigarette-branded merchandise is a strong predictor of smoking initiation among adolescents.19–22 Most Airmen in Technical Training are emerging adults, in a transitional phase with a strong desire to establish personal identity.23 Owning cigarette-branded merchandise may influence and solidify one’s identity with smoking as a central component, potentially reinforced through peer and role-model identification.24 In future interventions, it will be important to intervene using behavior-change techniques related to this factor, including highlighting the discrepancy between the identity of being a smoker and other aspirational identities, and identifying positive, non-smoking role models.25 However, given manufacturers are now prohibited from producing tobacco-branded merchandise,26 it is likely this predictor will become less important.
In the limited research examining tobacco initiation and re-initiation in Technical Training, researchers observed peer and role model (i.e., MTIs) perceived norms were associated with initiation and re-initiation.7 This study found not knowing whether one’s MTI used tobacco had a protective effect. According to USAF Education and Training Command (AETC) Instruction 36-2909, MTIs are not allowed to use tobacco in the presence of trainees; however, a quarter of Airmen reported knowing their MTI used cigarettes (24%) or smokeless tobacco (25.9%). While it is unclear how respondents knew about MTI use from the study measures, the findings support AETC Instruction 36-2909 and demonstrate the policy’s effectiveness to prevent initiation. Other military branches have similar policies to prevent tobacco use during their Technical Training.
This study found peer use significantly predicted initiation and re-initiation. Peer use is an established predictor of adolescent tobacco use.19 Peer use was assessed at the beginning of Technical Training before friend groups were established in this new environment (Airmen have only been in Technical Training for a day or two). Therefore, it may be likely Airmen are reporting cigarette-use behaviors of their closest friends prior to enlistment. Researchers have hypothesized homophily (i.e., similarity) of a behavior (e.g., smoking) in peer groups can be attributed to peer influence (i.e., peer pressure) and peer selection.20 It is unclear to what extent these factors interact to influence tobacco use in the current study; however, one could speculate among Airmen, in new environments where they must establish new peer relationships, peer selection may be an influence on smoking initiation/re-initiation. Future studies should directly measure the extent peer selection and influence play in smoking behaviors among military personnel.
While previous interventions have been effective in reducing re-initiation,8,9 they have been unable to impact the significant amount of tobacco initiation that occurs in the military. Results from the current study provide clear behavioral targets for future intervention efforts for individuals who initiate. Compared to individuals who re-initiate, individuals who initiate had lower intentions to both use tobacco after Technical Training and use a product that claims to be safer than cigarettes. Previous research found intentions to use tobacco are a reliable indicator of future use;21,22,27,28 however, among this initiator sample, there is a disconnect between intentions (76% planned to remain tobacco-free) and behavior. Future research is needed to understand what in the Technical Training environment alters these Airmen’s intentions, given the majority of initiation occurs during Technical Training. Interventions early in advanced training could focus on strengthening Airmen’s resolve to remain tobacco-free. One possible way to do this is through brief, group-based interventions, focusing on benefits associated with being tobacco-free and avoiding costs of tobacco use – a behavioral economics approach.29 For instance, one could begin by eliciting Airmen’s short and long-term goals, followed with a discussion about how tobacco use aligns with their goals. This approach has shown promise in reducing perceived harm and intentions-to-use tobacco in the short-term.30
This study is the first to analyze predictors of tobacco initiation and re-initiation following the tobacco ban in military training. Although the current sample is representative of USAF Technical Trainees, and the USAF is the 2nd largest service branch in the US with over 300,000 active duty Airmen, study findings may not generalize to other military branches. The study is also limited by the focus on cigarette use. With the growing prevalence of other tobacco products4,31 and dual- and poly-tobacco use18 among this population, the scope of future studies should include the full range of tobacco products used by Airmen in order to develop effective interventions. Reducing cigarette use without accounting for other tobacco products is not sufficient; prevention and cessation efforts must address contemporary use patterns.18 Only 76% of Airmen consented to participate in the current study. Although that represents 76% of all Airmen undergoing Technical Training at Joint Base San Antonio – Lackland during that time, it is still important to consider how those that did not agree to participate may have differed both in terms of demographics, but also tobacco use status. Unfortunately, in the current study we were unable to collect any information on non-consenting participants. Our rates of gender, ethnicity and race are in line with the demographics of the United States Air Force.32 Additionally, Airmen stationed overseas were excluded from the current study. Given that many foreign countries have higher rates of cigarette use than the U.S., with more social acceptability, it is possible that Airmen stationed overseas would report higher rates of cigarette use than Airmen stationed within the continental U.S. Future studies should consider exploring how socio-cultural influences from other countries could influence Airmen to smoke. Finally, given that this is a vulnerable population, the study staff was forthcoming regarding the nature of the study which could have led to information bias by subjects selectively revealing information about smoking. In our previous studies,4,6 we have found higher rates of reported tobacco use in our surveys of active duty military populations than the Department of Defense (DoD) Health Related Behaviors Survey,33 perhaps because we emphasize that we are researchers and not part of the DoD and thus participants feel free to report their actual intentions and behavior. However, it is still possible that some individuals fail to accurately disclose their intentions or behaviors.
The DoD is the nation’s largest employer with 1.4 million active-duty personnel,3 and each year more than 250,000 individuals leave the military,4 continuing their tobacco dependence into civilian life. Advancing our understanding of the factors impacting cigarette use among active-duty military personnel following initial enlistment will lead to improvements in the health and readiness of both the US military force and veteran population.
Opinions expressed in this document are solely those of the authors and do not represent an endorsement by or the views of the USAF, Department of Defense, or US Government.
References
- 1. Agaku IT, King BA, Dube SR: Current cigarette smoking among adults – United States, 2005–2012. MMWR 2014; 63(2): 29–34. [PMC free article] [PubMed] [Google Scholar]
- 2. Epidemiology Br : Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Cigarette Smoking among Adults – United States, 1999. MMWR 2001; 50(40): 869–781. [PubMed] [Google Scholar]
- 3. Department of Defense Department of Defense Anti-Tobacco Campaign Invades Military Markets. 2008.
- 4. Little MA, Derefinko KJ, Bursac Z, et al. : Prevalence and correlates of tobacco and nicotine containing product use in a sample of United States Air Force trainees. Nicotine Tobacco Res 2015; 18(4): 416–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoffman KM, Poston WS, Jitnarin N, et al. : A content analysis of tobacco control policy in the U.S. Department of Defense. J Public Health Policy 2011; 32(3): 334–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Little MA, Ebbert JO, Krukowski RA, et al. : Predicting cigarette initiation and re-initiation among active duty Air Force recruits. Substance Abuse 2019; 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Green KJ, Hunter CM, Bray RM, Pemberton M, Williams J: Peer and role model influences for cigarette smoking in a young adult military population. Nicotine Tobacco Res 2008; 10(10): 1533–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klesges RC, DeBon M, Vander Weg MW, et al. : Efficacy of a tailored tobacco control program on long-term use in a population of U.S. military troops. J Consult Clin Psychol 2006; 74(2): 295–306. [DOI] [PubMed] [Google Scholar]
- 9. Klesges RC, Haddock CK, Lando H, Talcott GW: Efficacy of forced smoking cessation and an adjunctive behavioral treatment on long-term smoking rates. J Consult Clin Psychol 1999; 67(6): 952–958. [DOI] [PubMed] [Google Scholar]
- 10. Bray RM, Pemberton MR, Hourani LL, et al. Department of Defense survey of health related behaviors among active duty military personnel. DTIC Document;2009.
- 11. Jha P, Ramasundarahettige C, Landsman V, et al. : 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med 2013; 368(4): 341–350. [DOI] [PubMed] [Google Scholar]
- 12. Thompson AB, Tebes JK, McKee SA: Gender differences in age of smoking initiation and its association with health. Addict Res Theory 2015; 23(5): 413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L: Current cigarette smoking among adults – United States, 2005–2013. MMWR 2014; 63(47): 1108–1112. [PMC free article] [PubMed] [Google Scholar]
- 14. Cavallo DA, Duhig AM, McKee S, Krishnan-Sarin S: Gender and weight concerns in adolescent smokers. Addict Behav 2006; 31(11): 2140–2146. [DOI] [PubMed] [Google Scholar]
- 15. Audrain-McGovern J, Benowitz NL: Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther 2011; 90(1): 164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haddock CK, Taylor JE, Hoffman KM, et al. : Factors which influence tobacco use among junior enlisted personnel in the United States Army and Air Force: a formative research study. Am J Health Promot 2009; 23(4): 241–246. [DOI] [PubMed] [Google Scholar]
- 17. Committee on Smoking Cessation in Military and Veteran Populations, Board on Population Health and Public Health Practice : Combating Tobacco Use in Military and Veteran Populations. Washington, DC, Institute of Medicine of the National Academies, 2009. [Google Scholar]
- 18. Little MA, Bursac Z, Derefinko KJ, et al. : Types of dual and poly-tobacco users in the US Military. Am J Epidemiol 2016; 184(3): 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tyas SL, Pederson LL: Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control 1998; 7(4): 409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoffman B, Monge P, Chou C-P, Valente T: Perceived peer influence and peer selection on adolescent smoking. Addict Behav 2007; 32: 1546–1554. [DOI] [PubMed] [Google Scholar]
- 21. Cengelli S, O’Loughlin J, Lauzon B, Cornuz J: A systematic review of longitudinal population-based studies on the predictors of smoking cessation in adolescent and young adult smokers. Tob Control 2012; 21(3): 355–362. [DOI] [PubMed] [Google Scholar]
- 22. Eckhardt L, Woodruff SI, Elder JP: A longitudinal analysis of adolescent smoking and its correlates. J Sch Health 1994; 64(2): 67–72. [DOI] [PubMed] [Google Scholar]
- 23. Schwartz SJ, Zamboanga BL, Luyckx K, Meca A, Ritchie RA: Identity in emerging adulthood: reviewing the field and looking forward. Emerg Adulthood 2013; 1(2): 96–113. [Google Scholar]
- 24. Sargent JD, Dalton M, Beach M, Bernhardt A, Heatherton T, Stevens M: Effect of cigarette promotions on smoking uptake among adolescents. Prev Med 2000; 30(4): 320–327. [DOI] [PubMed] [Google Scholar]
- 25. Tombor I, Shahab L, Herbec A, Neale J, Michie S, West R: Smoker identity and its potential role in young adults’ smoking behavior: a meta-ethnography. Health Psychol 2015; 34(10): 992–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Administration USFD 21 U.S.C. 301 et seq., Sec. 102, Pub. L. 111-31, 123 Stat. 1776. In: Administration USFD, ed. Title 21--Food and Drugs https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=11402010.
- 27. Hoving C, Reubsaet A, de Vries H: Predictors of smoking stage transitions for adolescent boys and girls. Prev Med 2007; 44(6): 485–489. [DOI] [PubMed] [Google Scholar]
- 28. Klosky JL, Tyc VL, Hum A, et al. : Establishing the predictive validity of intentions to smoke among preadolescents and adolescents surviving cancer. Journal of Clinical Oncology 2010; 28(3): 431–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Murphy JG, Dennhardt AA, Skidmore JR, et al. : A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. J Consult Clin Psychol 2012; 80(5): 876–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Little MA, Talcott GW, Bursac Z, et al. : Efficacy of a brief tobacco intervention for tobacco and nicotine containing product use in the US Air Force. Nicotine & Tobacco Research. 2016; 18(5): 1142–1149. [DOI] [PubMed] [Google Scholar]
- 31. Little MA, Derefinko KJ, Colvin L, et al. : The prevalence of E-cigarette use in a sample of U.S. Air Force recruits. Am J Prev Med 2015; 49(3): 402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. United States Air Force Military Demographics. 2018; https://www.afpc.af.mil/About/Air-Force-Demographics/. Accessed January 17, 2019.