Abstract
Objective
Although adverse events (AEs) following voluntary medical male circumcision (VMMC) are rare, their prompt ascertainment and management is a marker of quality care. The use of two-way text messaging (2wT) for client follow-up after VMMC reduces the need for clinic visits (standard of care (SoC)) without compromising safety. We compared the cost-effectiveness of 2wT to SoC for post-VMMC follow-up in two, high-volume, public VMMC sites in Zimbabwe.
Materials and methods
We developed a decision-analytic (decision tree) model of post-VMMC client follow-up at two high-volume sites. We parameterized the model using data from both a randomized controlled study of 2wT vs. SoC and from the routine VMMC program. The perspective of analysis was the Zimbabwe government (payer). The time horizon covered the time from VMMC to wound healing. Costs included text messaging; both in-person and outreach follow-up; and AE management. Costs were estimated in 2018 U.S. dollars. The outcome of analysis was AE yield relative to the globally accepted safety standard of a 2% AE rate. We estimated the incremental cost per percentage increase in AE ascertainment and the incremental cost per additional AE identified. We conducted univariate and probabilistic sensitivity analyses.
Results
2wT increased the costs due to text messaging by $4.42 but reduced clinic visit costs by $2.92 and outreach costs by $3.61 –a net savings of $2.10. 2wT also increased AE ascertainment by 50% (92% AE yield in 2wT compared to 42% AE yield in SoC). Therefore, 2wT dominated SoC in the incremental analysis: 2wT was less costly and more effective. Results were generally robust to univariate and probabilistic sensitivity analysis.
Conclusions
2wT is cost-effective for post-VMMC follow-up in Zimbabwe. Countries in which VMMC is a high-priority HIV prevention intervention should consider this mHealth intervention to reduce overall cost per VMMC, increasing the likelihood of current and future VMMC program sustainability.
Introduction
Voluntary medical male circumcision (VMMC) reduces the risk of female-to-male HIV-1 transmission by up to 60% [1–3]. As a result, nearly 19 million VMMCs were performed across 14 sub-Saharan African (SSA) countries from 2008 to 2017. VMMC is cost-effective for HIV prevention [4, 5] and is considered a priority for HIV prevention in SSA. In 2016, the UNAIDS set an annual target of 5 million VMMCs to reach 25 million men in SSA by 2021. However, many VMMC-priority countries face persistent healthcare resource constraints, characterized by low healthcare expenditures [6] personnel shortages [7] and an overdependence on donors for financing HIV prevention and treatment interventions [8]. These healthcare resource constraints threaten the quality and pace of VMMC scale-up [9, 10].
In VMMC programs, personnel shortages are a particularly difficult problem to address and assess as training and capacity building typically take a long time. Short-term monetary outlays, as are common with international donor-funded programs, don’t always include training beyond specific skillsets for singular program implementation, reducing long-term health personnel efficiency and impact. Program maintenance or sustainability is also threatened by continuous VMMC demand as successive cohorts of males come of age and traditional donor agencies plan to transfer VMMC programs to local Ministries and implementing partners. Resource shortages may also lead to cutting corners on program implementation, promoting program quantity over quality at scale [11].
Countries in which VMMC is of high priority have experienced a substantial increase in mobile health (mHealth) interventions. However, most mHealth interventions employ one-way (blast) messaging [12–14] which is less effective than bidirectional (two-way texting) communication that encourages interaction [15, 16]. In much of SSA, including Zimbabwe, mobile phone usage is widespread and presents an opportunity for mHealth innovation and deployment at scale. In the VMMC space, text message-based mHealth interventions have been applied with mixed success for demand creation [17], post-HIV testing demand creation [18], to deter early post-VMMC resumption of sexual activity [13, 19], and to encourage post-VMMC clinic visits [12].
In countries in which VMMC is of high priority, the intersection between increasing mHealth opportunities and healthcare resource constraints (human and financial) presents an opportunity for increased efficiency and cost reduction. While in-person follow-up after VMMC is critical for early detection of adverse events (AEs) [20], AEs are rare in routine program settings. Reported AE rates of large-scale VMMC programs are typically below the globally accepted AE rate of 2% [20–22]. Although the vast majority of VMMC recipients heal without complications [23], including those in Zimbabwe [24], in-person post-operative visits facilitate timely identification, management, and reporting of AEs. Recognizing both the importance of early AE ascertainment and the inefficiency of mandating in-clinic follow-up for the substantial majority of men who heal without complication, a randomized controlled trial (RCT) of post-VMMC follow-up using 2-way texting (2wT) was conducted in Zimbabwe [25]. In the RCT, VMMC clients were randomized to receive post-VMMC follow-up using 2wT or the standard of care (SoC). The 2wT arm required no in-person post-operative reviews while the SoC adhered to the national VMMC guidelines which required in-clinic follow-up visits on days 2, 7, and 42. Clinical outcomes from the RCT showed that 2wT-based follow-up was as safe as SoC: there was no significant difference in AE rates between groups [26]. However, 2wT ascertained and reported more AEs. As timely AE ascertainment is an indicator of VMMC program quality, 2wT-based follow-up appeared to improve patient care.
In this study, we assessed the cost-effectiveness of 2wT in Zimbabwe’s VMMC program. We hypothesized that 2wT would achieve gains in efficiency by reducing in-clinic post-VMMC follow-up visits. If 2wT proved more efficient in addition to being safe, swift replication of the intervention could better support VMMC sustainability. Due to the importance of safety and efficiency at scale, we sought to assess the tradeoff between identification of AEs (for quality VMMC management) and the costs of post-VMMC follow-up.
Materials and methods
This study was approved by the Medical Research Council of Zimbabwe (MRCZ) and the University of Washington Institutional Review Board. All subjects received comprehensive information regarding their voluntary participation in the study and signed the written informed consent form prior to enrollment in the study. The trial was registered on ClinicalTrials.gov, trial NCT03119337, and activated on April 18, 2017. https://clinicaltrials.gov/ct2/show/NCT03119337.
We conducted a model-based cost-effectiveness analysis using primary data collected in the RCT of 2-way texting (2wT) for post-operative follow-up in Zimbabwe’s VMMC program [25]. The RCT was conducted in two high-volume VMMC clinics operated by the ZAZIC consortium, an implementing partner of the Zimbabwe Ministry of Health and Child Care’s (MoHCC) VMMC program. The ZAZIC VMMC approach adheres to MoHCC guidelines and was described previously [27]. The base case population was adult men (over 18 years) who underwent VMMC by dorsal slit. The study was conducted from the payer perspective, the Zimbabwe MoHCC. In the analysis, we considered only costs that would be incurred by the MoHCC. Costs to VMMC patients, such as transportation and time off work, were excluded. The study was conducted from a short-term time horizon corresponding to the time from VMMC to healing and as such, no discounting was necessary.
Comparators
The comparators in the study were:
Standard of care (SoC)—post-VMMC wound care counseling; required in-person follow-up visits on post-surgery days 2, 7, and 42; instructions to seek care outside of scheduled visits on suspicion of AEs; and tracing with up to three phone calls followed by a home visit if clients did not return for the day 2 follow-up clinic visit.
Two-way texting (2wT)—enhanced post-VMMC counseling on use of 2wT, bandage removal, wound care, and AE recognition; automated daily texts from day 1–13 with requested responses; triaging of possible AEs via 2wT between patients and providers; and, return to clinic for suspicion and/or confirmation of AEs.
Decision-analytic model
We developed a decision-analytic model (decision tree) to simulate the post-VMMC experience of members of the base case population. Fig 1 is a schematic of the model. After the VMMC procedure, clients in the SoC arm returned or did not return for follow-up on day two. Those who did not return on day two were followed up by phone calls and home visits. Clients returned or failed to return for follow-up on days 7 and 42. Those who did not return on days 7 and 42 were not followed further. In the 2wT arm, clients returned or failed to return on days 2, 7 and 42; 2wT clients who did not return were not followed up except through 2wT. Clients in both arms developed (or survived) VMMC-related AEs.
Fig 1. Decision analytic model (decision tree) of post-VMMC follow-up of men in Zimbabwe.
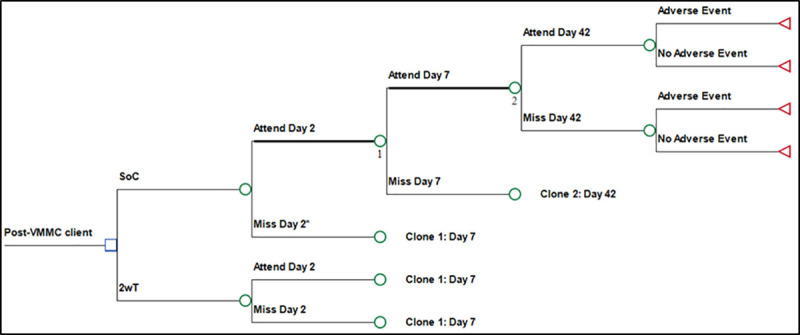
*Leads to outreach. **Note the use of clones to complete the decision tree diagram after day 2 in the SOC and 2wT arms.
Outcomes
Effectiveness of post-operative follow-up
The outcome was VMMC AE yield relative to the expected (maximum) rate of VMMC AEs in this population. The expected maximum rate of VMMC AEs in this population was assumed to be 2%, the commonly accepted safety standard [20–22]. Consequently, an AE yield less than 2% would be considered an underestimate of AEs while an AE yield of over 2% would be considered an overestimate of AEs. The percentage change in AE yield was calculated relative to 2% (i.e., percentage yield in SoC and 2wT divided by 2%) and expressed as a percentage. Data for effectiveness were obtained from the RCT, with reported AE rates as the base case estimates, and 95% confidence intervals were used in sensitivity analysis [25] Parameters for the outcome estimation are shown in Table 1.
Table 1. Outcome estimation parameters.
| Baseline | Range | Source | |
|---|---|---|---|
| Probabilities | |||
| Attend day 2 visit | |||
| SOC | 0.91 | 0.88–0.94 | RCT* |
| 2wT | 0.05 | 0.03–0.08 | RCT* |
| Attend day 7 visit | |||
| SOC | 0.52 | 0.47–0.57 | RCT* |
| 2wT | 0.05 | 0.04–0.09 | RCT* |
| Attend day 42 visit | |||
| SOC | 0.04 | 0.03–0.07 | RCT* |
| 2wT | 0.03 | 0.02–0.06 | RCT* |
| Adverse events | |||
| SOC | 0.0084 | 0.0028–0.0243 | RCT* |
| 2wT | 0.0188 | 0.0086–0.0403 | RCT* |
| Cost parameters | |||
| Text messaging (2wT arm only) | |||
| Commercial cost (per 250 texts) | $1.00 | $0.50—$2.00 | Econet [28] |
| Nurse wage (per month) | $907.00 | $883.00—$931.00 | MoH pay structure |
| FTEs dedicated to 2wT | 0.17 | 0.08–0.25 | Nurse time log |
| RCT study logs | |||
| Mean number of texts per client | 21.25 | 17.00–25.50 | 2wT call log |
| Duration of 2wT program (months)** | 9 | — | RCT study logs |
| Number of 2wT clients** | 362 | — | RCT study logs |
| Follow-up phone calls | |||
| Commercial cost per call | $0.09 | $0.05—$0.14 | Econet [28] |
| RCT study logs | |||
| FTEs dedicated to calls | 0.022 | 0.018–0.026 | Call logs |
| RCT study logs | |||
| Mean number of calls per client | 0.083 | 0.066–0.099 | Call logs |
| RCT study logs | |||
| In-clinic follow-up | |||
| Clinic clerk wage (per month) | $700.00 | $350.00—$1050.50 | MoH pay structure |
| RCT study logs | |||
| Clerk time (hours) | 0.024 | 0.017–0.067 | Time-motion |
| RCT study logs | |||
| Nurse review time (hours) | 0.083 | 0.017–2.033 | Time-motion study |
| RCT study logs | |||
| Hours worked per month | 160 | 128–192 | RCT study logs |
| Gloves | $0.20 | $0.10—$0.30 | MoHCC |
| Antiseptic | $0.50 | $0.25—$0.75 | |
| Gauze swabs | $0.20 | $0.10—$0.30 | |
| Bed liner | $0.20 | $0.10—$0.30 | |
| Distilled water | $0.10 | $0.05—$0.15 | |
| Alcohol rub | $0.30 | $0.15—$0.45 | |
| Outreach follow-up | |||
| Mean distance to client home (km) | 42.5 | 34.0–44.8 | ZAZIC program logs |
| Liters of diesel (per km) | 0.1 | 0.08–1.2 | RCT study logs |
| Price of diesel (per liter) | $1.37 | $0.69—$2.06 | |
| Driver wage (per month) | $905.05 | $452.53—$1,357 | |
| Outreach time (hours) | 1.125 | 0.900–1.350 | |
| Phone-call during outreach | $0.09 | $0.05—$0.14 | |
| Lunch allowance | $10 | $5—$15 | |
| Adverse events | |||
| Probability of bleeding | 0.0097 | 0.0078–0.0117 | RCT* |
| Probability of infection | 0.0069 | 0.0055–0.0083 | |
| Probability of swelling | 0.0083 | 0.0067–0.0100 | |
| Cost of surgery | $53.24 | $26.62—$79.86 | Assumption*** |
| Cost of antibiotic | $5.00 | $2.50—$10.00 | Assumption |
| Cost of pain killer/ anti-inflammatory | $2.00 | $1.00—$4.00 | Assumption |
Resource use and cost
We used a micro-costing approach for cost estimation. The parameter estimates, ranges used for sensitivity analysis, and data sources are presented in Table 1. We divided costs into the following categories: text messaging (2wT arm only), follow-up phone calls (as follow-up to 2wT), in-clinic post-VMMC follow-up, outreach post-VMMC follow-up (for missed day 2 appointments in SoC, including phone calls), and management of AEs.
The cost of text messaging for 2wT was calculated by summing the program costs of the text message service and the personnel cost of sending and responding to text messages. The cost of the text message service was calculated by multiplying the unit cost of a single text message by the mean number of texts sent per client in the trial. Because text messages are sold in bundles of 250, the cost of a single text message was estimated as a fraction of the bundle cost. The cost of 2wT-specific personnel was calculated using research logs to estimate the full time equivalents (FTE) spent by the nurse responsible for managing the 2wT system (including sending and responding to texts), and multiplying the FTE estimate by wage. Reports from research staff showed that the FTE required by the nurse to manage the texting was estimated at five to 15 minutes per hour, assuming an 8-hour work day and five working days a week, over the nine-month time period of the trial. The cost of follow-up phone calls made to 2wT clients was calculated by summing the costs of the phone service and the personnel costs of making calls. The cost of the phone service was calculated by multiplying the unit cost of a call by the mean number of calls per client in the trial as shown in call logs.
The cost of in-clinic follow-up was calculated by summing the personnel cost of follow-up and the costs of clinical supplies provided by the MoHCC VMMC program. The personnel cost of in-clinic follow-up was estimated by multiplying the time spent per client (by one clinic clerk and one VMMC nurse) by their wages. The use of one clinical clerk and one VMMC nurse reflects the pattern of routine post-VMMC follow-up in the MoHCC VMMC program. The cost of supplies included the components of a MoHCC wound dressing bundle of gloves, antiseptic, alcohol rub, gauze, bed liner, and distilled water.
The cost of follow-up for missed day two visits in SoC was calculated by summing the personnel costs of outreach, transportation costs, costs of phone calls (made during attempts to reach client’s homes), and costs of clinical supplies obtained from both RCT records and VMMC program logs. The costs of personnel were calculated based on the common practice of using one driver and one nurse for home visits and multiplying their wages by the time spent in this outreach activity. The nurse and driver also received a lunch allowance per outreach which was also included. The costs of phone calls during outreach assumed an average of one phone call per client home visit. The cost of clinical supplies included the components of a wound dressing bundle as described above. The costs of outreach transportation were calculated by multiplying the cost of fuel per unit distance by the mean distance of follow-up, both obtained from program data.
The costs of AE management were calculated by multiplying the probability of occurrence of the AE type from the trial (bleeding, infection, and swelling) [25] by the costs of managing the different AE types (minor surgery, antibiotics, and analgesics/antipyretics). The cost of minor surgery was assumed to equal to the cost of dorsal slit VMMC minus the cost of circumcision kits. All costs were estimated in 2018 US dollars ($US).
Analysis
The base case analysis compared: 1) the mean cost and adverse event yield of 2wT to SoC; and 2) the incremental cost-effectiveness ratio (ICER)—the cost per percentage increase in AE yield; and 3) cost per additional AE identified (relative to the expected number)—comparing 2wT to SoC. We conducted univariate sensitivity analyses to assess the most influential parameters. All parameters were varied across plausible ranges: we used 95% confidence intervals (CIs) of empirical estimates and, where 95% CIs were unavailable, we employed ranges of +/- 20% for probabilities and +/- 50% for costs [29–31]. We also conducted probabilistic sensitivity analyses using Monte Carlo simulation to assess overall model parameter uncertainty and to further test the robustness of the results. We used the baseline values as means and estimated standard errors assuming ranges were equivalent to 95% CIs (four times the standard error). We assumed beta distributions for probabilities, gamma distributions for costs, and normal distributions for other variables.
Results
Base-case analysis
The base case results are shown in Table 2. 2wT-specific activities increased the mean costs of post-VMMC follow-up by $4.42 overall: $0.09 in text service costs, $3.83 in text-related personnel costs, $0.01 in phone call costs and $0.50 in call-related personnel costs. However, the 2wT intervention also reduced costs: clinic visits decreased by $2.92, outreach visits by $3.61, and AE management by $0.002. Therefore, the net impact was that 2wT reduced the mean costs of VMMC follow-up by $2.10. The 2wT intervention also increased AE ascertainment (as compared to the expected AE yield of 2%) by 50% (92% AE yield in 2wT compared to 42% AE yield in SoC). Therefore, 2wT dominated SoC in the incremental analysis: 2wT was less costly and more effective.
Table 2. Base case results.
| SoC | 2wT | 2wT vs. SoC | |
|---|---|---|---|
| Costs (of follow-up) per client | |||
| 2wT | |||
| Text (service) | — | $0.085 | $0.085 |
| Text (personnel) | — | $3.833 | $3.833 |
| Call back (service) | — | $0.007 | $0.007 |
| Call back (personnel) | — | $0.496 | $0.496 |
| Total costs of 2wT | $0.00 | $4.42 | $4.42 |
| Clinic visits | $3.20 | $0.28 | – $2.92 |
| Outreach visits | $3.61 | — | – $3.61 |
| Adverse event management | $0.003 | $0.001 | – $0.002 |
| Total costs | $6.82 | $4.72 | – $2.10 |
| Outcomes | |||
| AE yield (vs. expected AE rate)* | 42.00% | 92.00% | 50.00% |
| Analysis | |||
| Cost per % increase in AE yield (vs. expected rate) | — | — | 2wT dominant** |
| Cost per additional AE identified (vs. expected #) | — | — | 2wT dominant** |
*Calculated as AE rate divided by expected rate (2%) for both SoC and 2wT, separately, and expressed as a percentage.
**Less costly and more effective.
Sensitivity analysis
In univariate sensitivity analysis (Fig 2), the reduction in mean cost of post-VMMC follow-up in 2wT as compared to SoC was most sensitive to the FTE of nurses providing the 2wT service, the probability of attending (or missing) the day two visit in the SoC, and the lunch allowance provided to outreach personnel. This result was generally robust to univariate sensitivity analysis as the highest estimate of 2wT-related FTE was associated with a reduction of $0.25 compared to SoC.
Fig 2. One-way sensitivity analysis on incremental cost comparing 2wT to SoC.
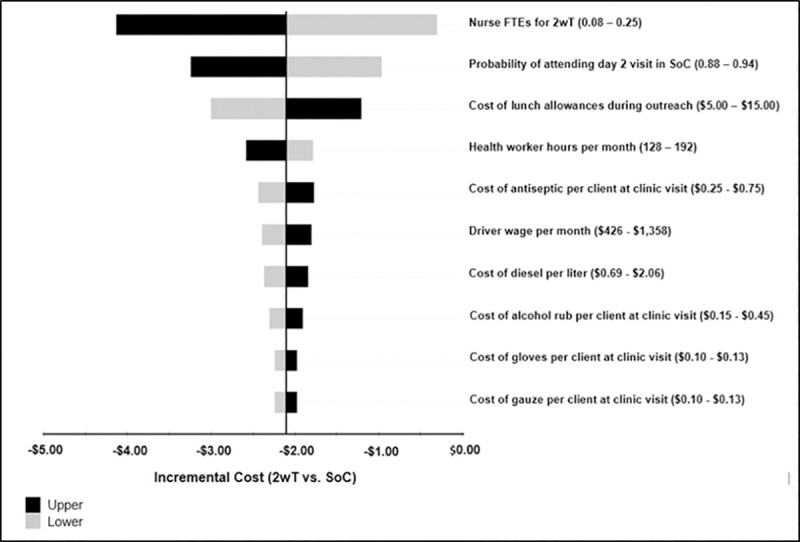
The top ten influential variables are shown. FTE–full time equivalent. 2wT–two-way texting. SoC—standard of care.
The results of the probabilistic sensitivity analysis are shown in an incremental cost-effectiveness (ICE) scatterplot (Fig 3). Of the 1,000 Monte Carlo simulations, 53% of the cost-effectiveness pairs were in the “south-east” quadrant (increased effectiveness and reduced cost) of the cost-effectiveness plane, which is also the quadrant of the base case results. Of the 1,000 Monte Carlo simulations, 39% of the cost-effectiveness pairs were in the “north-east” quadrant (increased effectiveness and increased cost) of the cost-effectiveness plane. Much smaller proportions of the cost-effectiveness pairs from the 1,000 Monte Carlo simulations were in the “north-west” quadrant (3%) and the south-west quadrant (5%) of the cost-effectiveness plane.
Fig 3. Incremental cost-effectiveness scatterplot of comparison of 2wT vs. SoC.
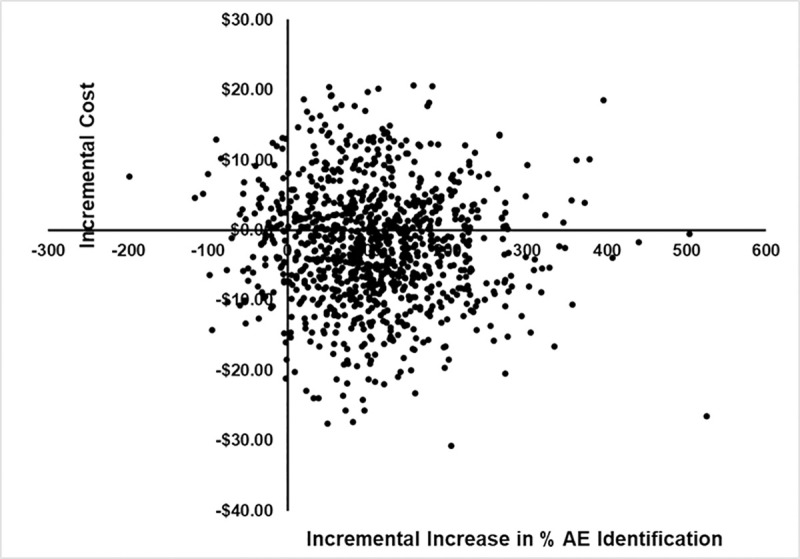
AE–Adverse event.
Discussion
2wT for VMMC follow-up appeared to increase AE ascertainment at reduced cost as compared to SoC. Although VMMC, itself, is cost-effective for HIV prevention, sustainability of VMMC programs will depend on innovations for cost-containment as donor funding expires and programs revert to Ministry funding in VMMC-priority countries. In this cost-effectiveness analysis of an mHealth intervention, 2wT was less costly and more effective in identifying AEs with dramatically reduced healthcare worker workload as compared to the SoC with in-person visits. VMMC programs in high-priority countries should consider this 2wT mHealth interventions to reduce the overall costs per VMMC while maintaining VMMC quality. The adoption of 2wT could contribute positively to long-term sustainability of VMMC programs.
The results of the probabilistic sensitivity analyses (Fig 3) showed that there was more uncertainty as to the impact of 2wT to reduce cost (as shown by the substantial distribution of cost-effectiveness pairs in the vertical (cost) plane of the ICE scatter plot) compared to its impact to increase effectiveness (as shown by the limited distribution of cost-effectiveness pairs in the horizontal (effectiveness) plane of the ICE scatter plot). As shown in Fig 3, there was a very small proportion of cost-effectiveness pairs in the north-west and south-west quadrants of the cost-effectiveness plans, suggesting a great deal of certainty as to the impact of 2wT to increase effectiveness. This suggests that there is more room for further innovation in cost-containment which may be easier achieved than innovation in effectiveness, in this case identifying adverse events. Such innovation to reduce costs, through for instance gains in efficiency in administering the 2wT program, will hasten the achievement of long-term sustainability of VMMC programs.
We used the payer perspective to assess the cost-effectiveness of 2wT. In Zimbabwe, the payer is the government, the MoHCC, which would likely bear the future costs of sustaining the VMMC program. However, broader potential benefits of 2wT should not be discounted. From a societal perspective, 2wT is likely to be even more economically attractive given that it would save client costs associated with in-person post-VMMC visits (e.g. transportation and missed wages). 2wT would also be expected to increase demand for VMMC by reducing the financial disincentives and perceived inconvenience of routine VMMC post-operative visits. For providers, less time on in-person follow-up reviews could free them to perform more VMMCs or other clinic duties.
From a bilateral and multilateral donor perspective, principally that of the major VMMC donor, the United States’ President's Emergency Plan for AIDS Relief (PEPFAR), the cost savings per VMMC using 2wT for follow-up is approximately $2.10. This amount is substantial if applied to the nearly 19 million VMMCs performed in the last 10 years. Additionally, the study showed a cost savings of $2.92 on in-person clinic visits. Applying this across the health sector, where relevant, would suggest a substantial potential reduction in the cost of VMMC in Zimbabwe and elsewhere. Furthermore, the internal ZAZIC program expenditure analysis conducted to comply with PEPFAR reporting requirements, estimated that from a programmatic perspective, the cost of service delivery within the overall ZAZIC program is 66% of the total cost of a VMMC–with 12% spent on demand creation and an additional 22% spent on management [32]. Therefore, a $2.10 reduction in follow-up costs could be shifted to other areas of service delivery and potentially allow for more VMMCs.
We may have underestimated the potential positive impact of 2wT on VMMC program cost savings. 2wT was implemented as a RCT in a routine VMMC setting. Therefore, the study does not provide a complete picture of the cost saving impact of 2wT. For instance, the 2wT nurse responsible for client communication was also part of other trial activities and provided VMMC services for a limited number of patients. It is possible that dedicated nurses for 2wT in high-volume sites or increasing numbers of patients enrolled in 2wT may have led to even greater cost savings.
There are several limitations of this analysis and its interpretation. First 2wT savings may differ in other contexts. Although 2wT reduces costs as compared to standard in-clinic follow-up in Zimbabwe, the amount of savings would depend on the specific staffing structure in other contexts. In settings with different human resources or implementation models, cost savings and the impact of 2wT on personnel distribution and use could differ. Secondly, we selected quality of care as the outcome—cost per AE yield. Although this is a critical indicator of patient safety, it does not immediately lend itself to comparison across interventions in the health sector. However, the 85% clinic workload reduction observed between the 2wT and the SoC should be a convincing measure of the impact of 2wT to reduce health resources utilization, helping demonstrate the potential economic advantages of 2wT in the broader healthcare system context. Finally, we did not include the costs of 2wT design, development, and maintenance in our analysis from the payer perspective, and we did not factor in the standard computers and Android phones for system operation. While we assumed that the marginal cost of inheriting an existing system by a government would be minimal on a per VMMC client basis, there may be significant periodic costs of upgrades and system maintenance. At scale, however, the capital and operating costs would be distributed across all circumcisions and would represent conservatively, at most, $.25 per VMMC by our estimates.
Conclusion
This economic evaluation of a novel application of mHealth found that 2wT-based VMMC follow-up reduced provider workload while maintaining quality of care. By dramatically decreasing unnecessary visits, 2wT saved costs, increasing the potential for program sustainability. We conclude that in the ongoing context of extreme resource constraints in high-priority countries, 2wT is a cost-effective method to improve AE ascertainment and maintain the quality of VMMC care. Further expansion and testing of 2wT for VMMC follow-up is warranted.
Acknowledgments
The authors wish to acknowledge the contributions of the 2wT study team: Christina Mauhy, Mujinga Tshimanga, Wendy Mutepfe, and Patricia Tapiwa Gundidza. We would also like to thank the Zimbabwe VMMC teams at Seke South and Norton clinics as well as Zimbabwe Ministry of Health and Child Care for their participation and collaboration.
Data Availability
Primary data analyzed for this paper may be found at https://zenodo.org/record/3953043#.XxYa7ihKguU.
Funding Statement
Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under Award Number R21TW010583. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. The Lancet. 2007;369(9562):657–66. [DOI] [PubMed] [Google Scholar]
- 2.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS medicine. 2005;2(11):e298 10.1371/journal.pmed.0020298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–56. Epub 2007/02/27. 10.1016/S0140-6736(07)60312-2 . [DOI] [PubMed] [Google Scholar]
- 4.Njeuhmeli E, Forsythe S, Reed J, Opuni M, Bollinger L, Heard N, et al. Voluntary Medical Male Circumcision: Modeling the Impact and Cost of Expanding Male Circumcision for HIV Prevention in Eastern and Southern Africa. PLOS Medicine. 2011;8(11):e1001132 10.1371/journal.pmed.1001132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uthman OA, Popoola TA, Uthman MM, Aremu O. Economic evaluations of adult male circumcision for prevention of heterosexual acquisition of HIV in men in sub-Saharan Africa: a systematic review. PloS one. 2010;5(3):e9628 10.1371/journal.pone.0009628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piatti-Fünfkirchen M, Lindelow M, Yoo K. What Are Governments Spending on Health in East and Southern Africa? Health Systems & Reform. 2018;4(4):284–99. 10.1080/23288604.2018.1510287 [DOI] [PubMed] [Google Scholar]
- 7.Clemens MA, Pettersson G. New data on African health professionals abroad. Human Resources for Health. 2008;6(1):1 10.1186/1478-4491-6-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olakunde BO, Adeyinka DA, Ozigbu CE, Ogundipe T, Menson WNA, Olawepo JO, et al. Revisiting aid dependency for HIV programs in Sub-Saharan Africa. Public Health. 2019;170:57–60. 10.1016/j.puhe.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 9.Curran K, Njeuhmeli E, Mirelman A, Dickson K, Adamu T, Cherutich P, et al. Voluntary Medical Male Circumcision: Strategies for Meeting the Human Resource Needs of Scale-Up in Southern and Eastern Africa. PLOS Medicine. 2011;8(11):e1001129 10.1371/journal.pmed.1001129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Njeuhmeli E, Opuni M, Schnure M, Tchuenche M, Stegman P, Gold E, et al. Scaling Up Voluntary Medical Male Circumcision for Human Immunodeficiency Virus Prevention for Adolescents and Young Adult Men: A Modeling Analysis of Implementation and Impact in Selected Countries. Clinical Infectious Diseases. 2018;66(suppl_3):S166–S72. 10.1093/cid/cix969 [DOI] [PubMed] [Google Scholar]
- 11.Rech D, Spyrelis A, Frade S, Perry L, Farrell M, Fertziger R, et al. Implications of the fast-evolving scale-up of adult voluntary medical male circumcision for quality of services in South Africa. PLoS One. 2014;9(5):e80577 Epub 2014/05/08. 10.1371/journal.pone.0080577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K, et al. Text Messaging to Improve Attendance at Post-Operative Clinic Visits after Adult Male Circumcision for HIV Prevention: A Randomized Controlled Trial. PloS one. 2012;7(9):e43832 10.1371/journal.pone.0043832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K, et al. Effect of text messaging to deter early resumption of sexual activity after male circumcision for HIV prevention: a randomized controlled trial. Journal of acquired immune deficiency syndromes (1999). 2014;65(2):e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, De Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS (London, England). 2011;25(6):825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeRenzi B, Findlater L, Payne J, Birnbaum B, Mangilima J, Parikh T, et al., editors. Improving community health worker performance through automated SMS. Proceedings of the fifth international conference on information and communication technologies and development; 2012: ACM.
- 16.Perrier T, Dell N, DeRenzi B, Anderson R, Kinuthia J, Unger J, et al., editors. Engaging pregnant women in Kenya with a hybrid computer-human SMS communication system. Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems; 2015: ACM.
- 17.Leiby K, Connor A, Tsague L, Sapele C, Kaonga A, Kakaire J, et al. The impact of SMS-based interventions on VMMC uptake in Lusaka Province, Zambia: a randomized controlled trial. Journal of acquired immune deficiency syndromes (1999). 2016;72(Suppl 4):S269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnabas RV, van Rooyen H, Tumwesigye E, Brantley J, Baeten JM, van Heerden A, et al. Uptake of antiretroviral therapy and male circumcision after community-based HIV testing and strategies for linkage to care versus standard clinic referral: a multisite, open-label, randomised controlled trial in South Africa and Uganda. The lancet HIV. 2016;3(5):e212–e20. 10.1016/S2352-3018(16)00020-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomsen SC, Skinner D, Toefy Y, Esterhuizen T, McCaul M, Petzold M, et al. Voice-Message–Based mHealth Intervention to Reduce Postoperative Penetrative Sex in Recipients of Voluntary Medical Male Circumcision in the Western Cape, South Africa: Protocol of a Randomized Controlled Trial. JMIR research protocols. 2016;5(3):e155 10.2196/resprot.5958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Byabagambi J, Kigonya A, Lawino A, Ssensamba JT, Twinomugisha A, Karamagi-Nkolo E, et al. A Guide to Improving the Quality of Safe Male Circumcision in Uganda 2015. [cited 2016 August 12]. Available from: https://www.usaidassist.org/sites/assist/files/uganda_guide_to_improving_the_quality_of_smc_a4_feb2015_ada.pdf. [Google Scholar]
- 21.World Health Organization Regional Office for Africa. Progress in scaling up voluntary medical male circumcision or HIV prevention in Est and Southern Africa January-December 20122013 October 27, 2014. Available from: http://www.malecircumcision.org/country_updates/documents/Progress%20in%20scaling%20up%20VMMC_Dec2013.pdf.
- 22.Population Services International CoSoE, Central and Southern Africa (COSECSA), U.S. Centers for Disease Control and Prevention. Adverse Event Action Guide for Voluntary Medical Male Circumcision by Surgery or Device. 2016.
- 23.Control CfD, Prevention. Voluntary medical male circumcision-southern and eastern Africa, 2010–2012. MMWR Morbidity and mortality weekly report. 2013;62(47):953 [PMC free article] [PubMed] [Google Scholar]
- 24.Bochner AF, Feldacker C, Makunike B, Holec M, Murenje V, Stepaniak A, et al. Adverse event profile of a mature voluntary medical male circumcision programme performing PrePex and surgical procedures in Zimbabwe. Journal of the International AIDS Society. 2017;(20:21394). Epub 21 February 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feldacker C, Murenje V, Barnhart S, Xaba S, Makunike-Chikwinya B, Holeman I, et al. Reducing provider workload while preserving patient safety via a two-way texting intervention in Zimbabwe’s voluntary medical male circumcision program: study protocol for an un-blinded, prospective, non-inferiority, randomized controlled trial. Trials. 2019;20(1):451 10.1186/s13063-019-3470-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feldacker C, Murenje V, Holeman I, Xaba S, Makunike-Chikwinya B, Korir M, et al. Reducing Provider Workload While Preserving Patient Safety: A Randomized Control Trial Using 2-Way Texting for Postoperative Follow-up in Zimbabwe's Voluntary Medical Male Circumcision Program. Journal of acquired immune deficiency syndromes (1999). 2020;83(1):16–23. Epub 2019/12/07. 10.1097/qai.0000000000002198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feldacker C, Makunike-Chikwinya B, Holec M, Bochner AF, Stepaniak A, Nyanga R, et al. Implementing voluntary medical male circumcision using an innovative, integrated, health systems approach: experiences from 21 districts in Zimbabwe. Global health action. 2018;11(1):1414997 10.1080/16549716.2017.1414997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Econet. Econet Wireless Tariffs (Incl VAT) Harare, Zimbabwe2016 [cited August 2016]. Available from: https://www.econet.co.zw/services/tariffs.
- 29.Babigumira JB, Stergachis A, Veenstra DL, Gardner JS, Ngonzi J, Mukasa-Kivunike P, et al. Potential cost-effectiveness of universal access to modern contraceptives in Uganda. PLoS One. 2012;7(2):e30735 Epub 2012/03/01. 10.1371/journal.pone.0030735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hofer F, Kauczor H-U, Stargardt T. Cost-utility analysis of a potential lung cancer screening program for a high-risk population in Germany: A modelling approach. Lung Cancer. 2018;124:189–98. 10.1016/j.lungcan.2018.07.036 [DOI] [PubMed] [Google Scholar]
- 31.Health Information and Quality Authority. Guidelines for the Economic Evaluation of Health Technologies in Ireland. 2018. Accessed on 0912/2020 at https://tools.ispor.org/PEguidelines/source/HIQA_Economic_Guidelines_2018.pdf.
- 32.President’s Emergency Plan for AIDS Relief (2019) "PEPFAR 2020 Country Operational Plan: Guidance for all PEPFAR Countries. Accessed on 09/15/2020 at https://www.state.gov/wp-content/uploads/2019/08/PEPFAR-Fiscal-Year-2019-Country-Operational-Plan-Guidance.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Primary data analyzed for this paper may be found at https://zenodo.org/record/3953043#.XxYa7ihKguU.


