Abstract
Background
Advanced heart failure therapies such as left ventricular assist device (LVAD) implantation require intricate follow-up and complex care. We sought to explore the burden of psychosocial risk factors among LVAD patients and their impact on post-implant outcomes using Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS).
Methods
Adult patients in INTERMACS requiring durable LVAD between 2008–2017 were included. Individuals were determined to have psychosocial risk if they had one of the following: 1) limited social support; 2) limited cognition; 3) substance abuse (alcohol and/or drug); 4) severe psychiatric disease (including major depression and/or other major psychiatric diagnosis), and 5) repeated non-compliance. Univariate and multivariate Cox proportional hazard regression models were used to analyze predictors of survival and complications.
Results
15,403 continuous-flow LVAD recipients were included. 3163 (20.5%) had one or more psychosocial risk factors. The most prevalent psychosocial risk factor was substance abuse in 1941 (12.6%) recipients. Patients with psychosocial risk factors were significantly younger at LVAD implant, less likely to be white, and less likely to be female compared to those without psychosocial risk, p <0.001 for all. Patients with psychosocial risk were significantly more likely to receive an LVAD as destination therapy, p <0.001. In adjusted models, patients with psychosocial risk were at increased hazards for device-related infection, gastrointestinal bleeding, pump thrombosis, and readmission and reduced hazards for cardiac transplantation (p<0.05 for all). There was no statistically significant difference in survival on pump support or stroke.
Conclusions
Psychosocial risk is an important component of patient selection for advanced heart failure therapies. Addressing these specific components may help improve access to advanced therapies and post-LVAD outcomes.
Keywords: left ventricular assist device, psychosocial assessment, social support, medication compliance
Introduction
Advanced heart failure therapies including continuous-flow left ventricular assist device (LVAD) implantation offer patients improved survival as well as quality of life.1 Yet, these therapies are both medically complicated and require significant patient engagement with frequent follow-up appointments, intricate medication regimens including therapeutic oral anticoagulation, and device management.2,3 Therefore, candidate selection requires a comprehensive medical assessment as well as a multidisciplinary determination of psychosocial risk.2,4–6 According to the 2018 International Society for Heart and Lung Transplantation (ISHLT) Consensus recommendations for the psychosocial evaluation of adult cardiothoracic transplant candidates and candidates for long-term mechanical circulatory support, candidates should be evaluated for treatment adherence, mental health and substance use history, cognitive status, coping abilities, and social support as these may affect long-term outcomes.7 Objective psychosocial assessment tools for transplant candidacy have been developed including the Stanford Integrated Psychosocial Assessment for Transplant (SIPAT),8–10 Psychosocial Assessment of Candidates for Transplantation (PACT),11 and the Transplant Evaluation Rating Scale (TERS)12,13 which have since been applied to LVAD recipients.14–18 However, these retrospective studies have been limited by their small sample size and inadequate power to assess impact on outcomes.19 The current study sought to explore the burden of psychosocial risk factors among LVAD patients and their impact on post-implant outcomes using the multicenter Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS).
Methods
Patient Population
The INTERMACS database was queried to identify adult patients (≥ 18 years old) who received durable continuous-flow mechanical circulatory support from 2008 through 2017. Patients who had received right ventricular mechanical circulatory support alone or total artificial heart were excluded. The data used in the study are available to other researchers for purposes of reproducing the results or replicating the procedure via data request from the National Heart, Lung, and Blood Institute Biological Specimen and Data Repository Information Coordination Center. The Columbia University Irving Medical Center Institutional Review Board approved this study.
Definition of Psychosocial Risk
We selected variables in five domains that have been previously described to be associated with psychosocial risk in advanced heart failure patients: 1) cognitive function; 2) adherence; 3) psychopathology; 4) social support, and 5) substance abuse.2 These domains are included in validated psychosocial assessment tools such as the SIPAT,14,15,20 PACT,16,17 and the TERS18 which have been previously studied in LVAD recipients. Unfortunately, these objective psychosocial assessment tools require detailed survey data that is unavailable in the INTERMACS registry.
Relevant variables coded in the INTERMACS registry include limited social support, history of alcohol abuse, history of illicit drug use, limited cognitive understanding, repeated noncompliance, severe depression, and other major psychiatric illness. Individuals were determined to have psychosocial risk for the purposes of this analysis if they had one of the following: 1) limited social support; 2) limited cognitive understanding; 3) substance abuse (alcohol and/or drug); 4) psychiatric disease (including severe depression and/or other major psychiatric diagnosis), and 5) repeated non-compliance. Narcotic dependence was not included in history of substance abuse given the degree of missing data. Other relevant demographic and social variables were included such as education, marital status, working for income, tobacco use, and others.
Statistical Analysis
Descriptive analyses were conducted for all baseline variables and are presented as means and SDs for continuous variables and numbers and percentages for categorical variables. Differences between groups were quantified using the independent t-test and chi-square test when appropriate. Kaplan-Meier survival estimates were used to assess post-LVAD implant outcomes, with log-rank testing used to compare groups. Univariate and multivariate Cox proportional hazard regression models were used to analyze predictors of LVAD outcomes, including survival on pump support, cardiac transplantation, device-related infection gastrointestinal (GI) bleeding, device thrombosis (suspected or confirmed), stroke (ischemic or hemorrhagic), and rehospitalization for any cause. Patients were censored if they were transplanted or explanted without new device implant. The last date of follow-up for all patients was October 2017. The multivariate model was adjusted for age, gender, race, heart failure etiology, body surface area (BSA), year of implant, history of right ventricular assist device (RVAD) use, pump type (axial vs. centrifugal), INTERMACS profile, device strategy (destination therapy vs bridge to transplant or recovery), creatinine, bilirubin, and albumin levels, all factors which have been known to be associated with post-transplant or post-LVAD outcomes. All P values were reported as 2-sided tests with p<0.05 considered statistically significant. SPSS Statistics, Version 25.0 (Armonk, NY: IBM) was used to perform statistical analysis.
Results
Baseline Characteristics
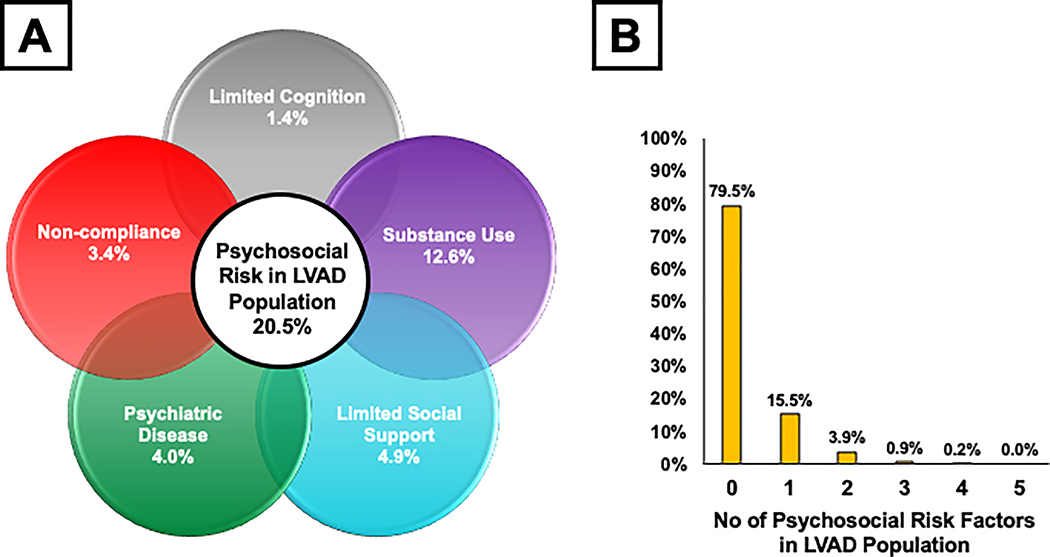
Among eligible participants in the INTERMACS registry, 15,403 individuals received a continuous-flow left ventricular assist device in the INTERMACS registry from 2008 to 2017 were included in the analysis (Table 1). Within this population, 3163 (20.5%) had one or more psychosocial risk factor. The most prevalent psychosocial risk factor was substance abuse in 1941 (12.6%) of LVAD recipients [alcohol abuse in 1211(7.9%) and drug abuse in 1167 (7.6%)] with limited social support being the second most prevalent in 759 (4.9%) of the study population (Figure 1A). The majority of patients with psychosocial risk had only one of the five risk factors (Figure 1B).
Table 1.
Baseline Clinical Characteristics by Psychosocial Risk Status
| Variable | Overall (n=15403, 100%) | Psychosocial Risk (n=3163, 20.5%) | No Psychosocial Risk (n=12240, 79.5%) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age at Implant | 56.9 ± 13.0 | 52.3 ± 12.9 | 58.1 ± 12.7 | <0.001 |
| Female Gender, n(%) | 3322 (21.6) | 577 (18.2) | 2745 (22.4) | <0.001 |
| Race, n(%) | <0.001 | |||
| White, | 10151 (65.9) | 1838 (58.1) | 8313 (67.9) | |
| African American | 3787 (24.6) | 1005 (31.8) | 2782 (22.7) | |
| Asian | 254 (1.6) | 36 (1.1) | 218 (1.8) | |
| American Indian | 116 (0.8) | 34 (1.1) | 82 (0.7) | |
| Pacific Islander | 53 (0.3) | 19 (0.6) | 34 (0.3) | |
| Other | 688 (4.5) | 163 (5.2) | 525 (4.3) | |
| Unknown | 417 (2.7) | 86 (2.7) | 331 (2.7) | |
| Ethnicity | ||||
| Hispanic | 1019 (6.6) | 233 (7.4) | 786 (6.4) | 0.137 |
| Blood Type O, n(%) | 7177 (46.6) | 1458 (46.1) | 5719 (46.7) | 0.384 |
| BMI (kg/m2) | 28.5 ± 6.8 | 28.4 ± 7.0 | 28.6 ± 6.8 | 0.406 |
| BSA (m2) | 2.05 ± 0.30 | 2.05 ± 0.30 | 2.05 ± 0.30 | 0.261 |
| Ischemic Etiology of HF | 6873 (44.6) | 1202 (38.0) | 5671 (46.3) | <0.001 |
| Social Factors | ||||
| Marital Status | <0.001 | |||
| Single | 2986 (19.4) | 970 (30.7) | 2016 (16.5) | |
| Married | 9513 (61.8) | 1405 (44.4) | 8108 (66.2) | |
| Domestic Partner | 1825 (11.8) | 560 (17.7) | 1265 (10.3) | |
| Divorced/Seperated | 514 (3.3) | 108 (3.4) | 406 (3.3) | |
| Widowed | 252 (1.6) | 66 (2.1) | 186 (1.5) | |
| Unknown | 313 (2.0) | 54 (1.7) | 259 (2.1) | |
| Education Level | <0.001 | |||
| None | 29 (0.2) | 9 (0.3) | 20 (0.2) | |
| Grade school | 382 (2.5) | 121 (3.8) | 261 (2.1) | |
| High school | 5062 (32.9) | 1276 (40.3) | 3786 (30.9) | |
| College/Tech school | 2872 (18.6) | 627 (19.8) | 2245 (18.3) | |
| Associate/Bachelor | 1920 (12.5) | 278 (8.8) | 1642 (13.4) | |
| Post-graduate | 802 (5.2) | 98 (3.1) | 704 (5.8) | |
| Not applicable | 12 (0.1) | 1 (0.0) | 11 (0.1) | |
| Unknown | 4324 (28.1) | 753 (23.8) | 3571 (29.2) | |
| Working for Income | 2502 (16.2) | 410 (13.0) | 2092 (17.1) | <0.001 |
| HIV | 48 (0.3) | 16 (0.5) | 32 (0.3) | 0.028 |
| Narcotic Dependence | 100 (0.6) | 72 (2.3) | 28 (0.2) | <0.001 |
| Device-related factors | ||||
| Device type | 0.483 | |||
| LVAD | 14800 (96.1) | 3046 (96.3) | 11754 (96.0) | |
| LVAD + RVAD | 603 (3.9) | 117 (3.7) | 486 (4.0) | |
| LVAD type | <0.001 | |||
| Centrifugal | 4396 (28.5) | 731 (23.1) | 3665 (29.9) | |
| Axial | 11007 (71.5) | 2432 (76.9) | 8575 (70.1) | |
| Device Strategy | <0.001 | |||
| Transplant listed | 3866 (25.1) | 520 (16.4) | 3346 (27.3) | |
| Transplant eligible | 4204 (27.3) | 961 (30.4) | 3243 (26.5) | |
| Destination Therapy | 7232 (47.0) | 1661 (52.5) | 5571 (45.5) | |
| Bridge to recovery | 49 (0.3) | 12 (0.4) | 37 (0.3) | |
| Other | 52 (0.3) | 9 (0.3) | 43 (0.4) | |
| INTERMACS Profile | <0.001 | |||
| Profile 1 | 2655 (17.3) | 567 (21.4) | 2088 (17.2) | |
| Profile 2 | 5288 (34.5) | 1146 (36.4) | 4142 (34.0) | |
| Profile 3 | 5117 (33.4) | 1072 (34.1) | 4045 (33.2) | |
| Profile 4 – 7 | 2260 (14.8) | 361 (11.5) | 1899 (15.6) | |
| NYHA Class IV | 12025 (78.1) | 2613 (82.6) | 9412 (76.9) | <0.001 |
| 6MWT > 300m | 1101 (32.9) | 223(31.9) | 878 (33.2) | 0.541 |
| IV Inotropes | 5421 (35.2) | 1179 (37.3) | 4242 (34.7) | 0.001 |
| IABP | 4234 (27.5%) | 923 (29.2) | 3311 (27.1) | 0.017 |
| ECMO | 865 (5.6%) | 180 (5.7) | 685 (5.6) | 0.837 |
| Mechanical Ventilation | 1120 (7.3%) | 249 (7.9) | 871 (7.1) | 0.144 |
| Dialysis | 412 (2.7) | 88 (2.8) | 324 (2.6) | 0.675 |
| Comorbid Conditions | ||||
| Severe diabetes, n(%) | 1503 (9.8) | 366 (11.6) | 1137 (9.3) | <0.001 |
| Active Smoking, n(%) | 715 (4.6) | 297 (9.4) | 418 (3.4) | <0.001 |
| Pulmonary HTN | 3390 (22.0) | 914 (28.9) | 2476 (20.2) | <0.001 |
| VD, n(%) | 712 (4.6) | 163 (5.2) | 549 (4.5) | 0.111 |
| CHF Therapy | ||||
| Beta Blocker | 7376 (47.9) | 1392 (44.0) | 5984 (48.9) | <0.001 |
| ACE Inhibitor | 3501 (22.7) | 728 (23.0) | 2773 (22.7) | <0.001 |
| Angiotensin Receptor Blocker | 1328 (8.6) | 200 (6.3) | 1128 (9.2) | 0.031 |
| Aldosterone antagonist | 5937 (38.5) | 1276 (40.3) | 4661 (38.1) | <0.001 |
| Loop Diuretic | 12866 (83.5) | 2680 (84.7) | 10186 (83.2) | 0.047 |
| AICD | 12089 (78.5) | 2420 (76.5) | 9669 (79.0) | <0.001 |
6MWT = 6 minute walk test; ACE = angiotensin-converting enzyme; AICD = automated implantable cardioverter-defibrillator; BMI = body mass index; BSA = body surface area; ECMO = extracorporeal membrane oxygenation; HF = heart failure; HIV = human immunodeficiency virus; IABP = intra-aortic balloon pump; HTN = hypertension; LVAD = left ventricular assist device; RVAD = right ventricular assist device; PVD = peripheral vascular disease
Figure 1. The Burden of Psychosocial Risk Factors in INTERMACS.
This schematic highlights the five domains used to characterize psychosocial risk: social support, cognition, substance use, psychopathology, and non-compliance (Panel A). The respective frequency of various psychosocial risk factors in the INTERMACS database is also shown. In Panel B, a bar graph highlights that the majority of patients with psychosocial risk had only one of the five risk factors.
Patients with psychosocial risk factors were significantly younger at LVAD implant (52.3±12.9 vs. 58.1±12.7 years), less likely to be white [1838(58.1%) vs. 8313 (67.9%)], and less likely to be female [577(18.2%) vs. 2745(22.4%) compared to those without psychosocial risk, p <0.001 for all. They were significantly more likely to be active smokers [297(9.4%) vs. 418(3.4%), p<0.001] and less likely to be working for income [410(13.0%) vs. 2092 (17.1%), p<0.001]. Patients in the psychosocial risk group were also significantly more likely to be seropositive for human immunodeficiency virus [16(0.5%) vs. 32(0.3%), p = 0.028] as well as be dependent on narcotics [72(2.3%) vs. 28(0.2%), p<0.001]. Individuals with psychosocial risk were significantly less likely to be married [1405(44.4%) vs. 8108 (66.2%), p <0.001] and less likely to have a college degree [278(8.8%) vs. 1642 (13.4%), p <0.001] with associate/bachelor degrees.
In addition, those with psychosocial risk factors were overall sicker patients: they were significantly more likely to be New York Heart Association Class IV [2613(82.6%) vs. 9412(76.9%), p<0.001] and INTERMACS profile 1 at the time of implant [567(21.4%) vs. 2088 (17.2%), p<0.001]. Similarly, they were significantly more likely to be on intravenous inotropes [1179 (37.3%) vs. 4242 (34.7%),p = 0.001] and intra-aortic balloon pump therapy [923 (29.2%) vs. 3311 (27.1%), p = 0.017] prior to LVAD implant than those patients without psychosocial risk. This was also reflected by statistically significantly higher central venous pressures, pulmonary artery diastolic pressure and pulmonary capillary wedge pressure, although these differences are likely not clinically significant (Supplemental Table 1). There were no statistically significant differences in the use of extracorporeal membrane oxygenation, mechanical ventilation, and dialysis between groups.
With regard to device strategy, patients with psychosocial risk were significantly more likely to receive an LVAD as destination therapy [1661(52.5%) vs. 5571 (45.5%)] and significantly less likely to be listed for transplant [520(16.4%) vs. 3346 (27.3%)], p<0.001 for both.
Post-Implant Outcomes
At the end of the follow-up period, 11,740 individuals (76.2%) remained alive on pump support. Patients with high psychosocial risk paradoxically had improved survival on LVAD support in unadjusted univariate analysis. However, when adjusted for clinical risk factors, psychosocial risk was not significantly associated with survival on pump support [HR 0.99 (95% CI 0.91–1.09, p = 0.90](Table 2). Other major psychiatric disease was significantly associated with worsened survival [HR 1.38 (95% CI 1.07–1.77), p = 0.012].
Table 2.
Hazard Ratio Estimates for LVAD Outcomes by Psychosocial Risk
| LVAD Outcomes | Unadjusted Cox Regression | Adjusted Cox Regression* | ||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Survival on pump support | ||||
| Any Psychosocial Risk | 0.84 (0.77 – 0.92) | <0.001 | 0.99 (0.91 – 1.09) | 0.902 |
| Limited Social Support | 0.90 (0.77 – 1.05) | 0.182 | 0.96 (0.81 – 1.13) | 0.608 |
| Limited Cognition | 0.81 (0.63 – 1.05) | 0.107 | 0.84 (0.64 – 1.11) | 0.213 |
| Substance Abuse | ||||
| ETOH Abuse | 0.82 (0.72 – 0.93) | 0.002 | 0.96 (0.84 – 1.10) | 0.533 |
| Drug Use | 0.68 (0.59 – 0.79) | <0.001 | 0.97 (0.83 – 1.14) | 0.703 |
| Psychiatric Disease | ||||
| Severe Depression | 0.89 (0.72 – 1.10) | 0.272 | 0.95 (0.76 – 1.19) | 0.653 |
| Other Major Psychiatric Dx | 1.08 (0.85 – 1.37) | 0.529 | 1.38 (1.07 – 1.77) | 0.012 |
| Non-Compliance | 0.94 (0.78 – 1.13) | 0.515 | 1.16 (0.95 – 1.40) | 0.137 |
| Cardiac Transplantation | ||||
| Any Psychosocial Risk | 0.82 (0.76 – 0.90) | <0.001 | 0.85 (0.80 – 0.91) | <0.001 |
| Limited Social Support | 0.68 (0.57 – 0.81) | <0.001 | 0.82 (0.68 – 0.99) | 0.038 |
| Limited Cognition | 0.67 (0.51 – 0.89) | 0.005 | 0.66 (0.49 – 0.89) | 0.006 |
| Substance Abuse | ||||
| ETOH Abuse | 0.93 (0.83 – 1.05) | 0.249 | 0.88 (0.77 – 0.99) | 0.041 |
| Drug Use | 0.95 (0.84 – 1.07) | 0.392 | 0.84 (0.74 – 0.96) | 0.011 |
| Psychiatric Disease | ||||
| Severe Depression | 0.82 (0.66 – 1.01) | 0.066 | 0.81 (0.64 – 1.02) | 0.068 |
| Other Major Psychiatric Dx | 1.12 (0.88 – 1.41) | 0.357 | 1.10 (0.86 – 1.41) | 0.444 |
| Non-Compliance | 0.62 (0.50 – 0.78) | <0.001 | 0.68 (0.54 – 0.86) | 0.001 |
| Device Related Infection | ||||
| Any Psychosocial Risk | 1.40 (1.28 – 1.54) | <0.001 | 1.29 (1.17 – 1.43) | <0.001 |
| Limited Social Support | 1.57 (1.35 – 1.84) | <0.001 | 1.44 (1.22 – 1.69) | <0.001 |
| Limited Cognition | 1.22 (0.94 – 1.59) | 0.132 | 1.22 (0.92 – 1.61) | 0.161 |
| Substance Abuse | ||||
| ETOH Abuse | 1.30 (1.14 – 1.49) | <0.001 | 1.26 (1.09 – 1.45) | 0.002 |
| Drug Use | 1.43 (1.25 – 1.63) | <0.001 | 1.24 (1.07 – 1.44) | 0.004 |
| Psychiatric Disease | ||||
| Severe Depression | 1.22 (0.97 – 1.53) | 0.083 | 1.12 (0.88 – 1.42) | 0.345 |
| Other Major Psychiatric Dx | 1.62 (1.26 – 2.08) | <0.001 | 1.46 (1.12 – 1.90) | 0.006 |
| Non-Compliance | 1.58 (1.31 – 1.90) | <0.001 | 1.37 (1.13 – 1.67) | 0.002 |
| Gastrointestinal Bleeding | ||||
| Any Psychosocial Risk | 0.98 (0.90 – 1.06) | 0.532 | 1.20 (1.11 – 1.31) | <0.001 |
| Limited Social Support | 0.96 (0.82 – 1.11) | 0.555 | 1.06 (0.91 – 1.24) | 0.467 |
| Limited Cognition | 1.13 (0.91 – 1.05) | 0.267 | 1.24 (0.99 – 1.56) | 0.058 |
| Substance Abuse | ||||
| ETOH Abuse | 1.02 (0.90 – 1.14) | 0.794 | 1.22 (1.08 – 1.38) | 0.002 |
| Drug Use | 0.74 (0.65 – 0.85) | <0.001 | 1.08 (0.93 – 1.24) | 0.325 |
| Psychiatric Disease | ||||
| Severe Depression | 1.08 (0.89 – 1.30) | 0.432 | 1.26 (1.03 – 1.53) | 0.023 |
| Other Major Psychiatric Dx | 0.88 (0.68 – 1.13) | 0.319 | 1.17 (0.90 – 1.53) | 0.223 |
| Non-Compliance | 1.10 (0.93 – 1.31) | 0.250 | 1.40 (1.17 – 1.67) | <0.001 |
| Device Thrombosis (Suspected or Confirmed) | ||||
| Any Psychosocial Risk | 1.27 (1.14 – 1.41) | <0.001 | 1.19 (1.06 – 1.33) | 0.002 |
| Limited Social Support | 1.27 (1.05 – 1.53) | 0.013 | 1.19 (0.98 – 1.45) | 0.087 |
| Limited Cognition | 1.10 (0.81 – 1.50) | 0.544 | 1.06 (0.77 – 1.47) | 0.723 |
| Substance Abuse | ||||
| ETOH Abuse | 1.05 (0.89 – 1.24) | 0.539 | 1.08 (0.91 – 1.29) | 0.363 |
| Drug Use | 1.37 (1.18 – 1.60) | <0.001 | 1.19 (1.01 – 1.41) | 0.038 |
| Psychiatric Disease | ||||
| Severe Depression | 1.40 (1.10 – 1.77) | 0.006 | 1.27 (0.99 – 1.63) | 0.061 |
| Other Major Psychiatric Dx | 1.57 (1.19 – 2.07) | 0.002 | 1.37 (1.01 – 1.85) | 0.042 |
| Non-Compliance | 1.43 (1.16 – 1.77) | <0.001 | 1.29 (1.03 – 1.62) | 0.024 |
| Stroke (Ischemic or Hemorrhagic) | ||||
| Any Psychosocial Risk | 1.02 (0.92 – 1.12) | 0.765 | 1.11 (0.99 – 1.24) | 0.067 |
| Limited Social Support | 0.97 (0.80 – 1.17) | 0.726 | 0.98 (0.80 – 1.20) | 0.846 |
| Limited Cognition | 1.00 (0.75 – 1.35) | 0.959 | 0.96 (0.70 – 1.32) | 0.788 |
| Substance Abuse | ||||
| ETOH Abuse | 1.01 (0.87 – 1.18) | 0.853 | 1.15 (0.98 – 1.35) | 0.084 |
| Drug Use | 0.89 (0.76 – 1.05) | 0.169 | 1.00 (0.84 – 1.19) | 0.976 |
| Psychiatric Disease | ||||
| Severe Depression | 0.88 (0.67 – 1.15) | 0.349 | 0.89 (0.67 – 1.18) | 0.420 |
| Other Major Psychiatric Dx | 1.12 (0.83 – 1.51) | 0.467 | 1.15 (0.84 – 1.59) | 0.380 |
| Non-Compliance | 1.28 (1.04 – 1.56) | 0.018 | 1.38 (1.11 – 1.71) | 0.004 |
| Hospital Readmission | ||||
| Any Psychosocial Risk | 1.08 (1.03 – 1.13) | 0.002 | 1.14 (1.08 – 1.19) | <0.001 |
| Limited Social Support | 1.06 (0.98 – 1.15) | 0.169 | 1.13 (1.04 – 1.24) | 0.005 |
| Limited Cognition | 1.00 (0.87 – 1.14) | 0.948 | 1.09 (0.94 – 1.26) | 0.263 |
| Substance Abuse | ||||
| ETOH Abuse | 1.06 (0.99 – 1.14) | 0.071 | 1.11 (1.03 – 1.19) | 0.005 |
| Drug Use | 1.03 (0.96 – 1.11) | 0.373 | 1.09 (1.01 – 1.17) | 0.022 |
| Psychiatric Disease | ||||
| Severe Depression | 1.20 (1.07 – 1.33) | 0.001 | 1.18 (1.06 – 1.33) | 0.004 |
| Other Major Psychiatric Dx | 1.42 (1.25 – 1.62) | <0.001 | 1.40 (1.22 – 1.60) | <0.001 |
| Non-Compliance | 1.04 (0.94 – 1.15) | 0.439 | 1.10 (0.99 – 1.22) | 0.085 |
ETOH = alcohol
Adjusted for age, gender, race, BSA, implant year, HF etiology, RVAD use, pump type (axial vs. centrifugal), INTERMACS Class, device strategy (destination vs. bridge), creatinine, bilirubin, and albumin levels.
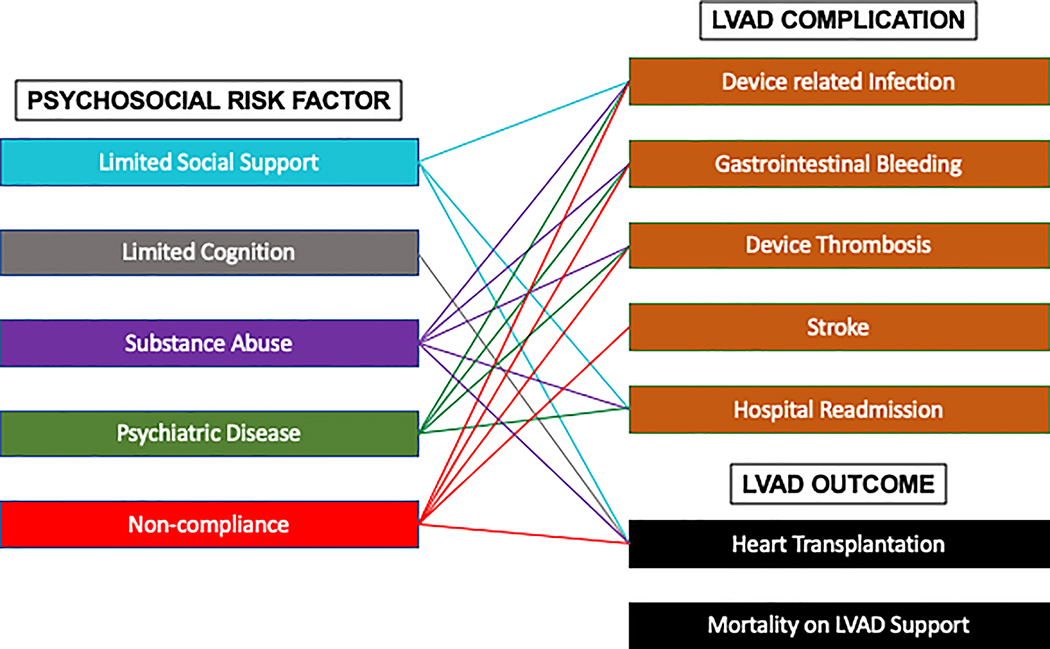
Device-related infections occurred in 2363 (15.3%) individuals. Any psychosocial risk was significantly associated with increased hazards for device-related infection in the unadjusted and adjusted regression model [HR 1.29 (95% CI 1.17–1.43), p <0.001]. When each individual risk factor was examined, the subpopulations with limited social support, substance abuse, other major psychiatric diagnosis, and history of non-compliance independently were each significantly associated with increased hazards for device-related infections (p<0.05 for all) (Table 2, Figure 2).
Figure 2. Psychosocial Risk Domains and Associated Outcomes.
Network diagram is shown displaying associations between each domain of psychosocial risk to LVAD complications and outcomes
During the study period, gastrointestinal bleeding occurred in 3775 (24.5%) individuals while pump thrombosis occurred in 1870 (12.1%). Psychosocial risk was significantly associated with increased hazards for GI bleeding [adjusted HR 1.20 (95% CI 1.11–1.31), p <0.001]. This was driven by increased hazards of GI bleeding among patients with alcohol abuse, severe depression and a history of non-compliance (p < 0.05 for all). Patients with psychosocial risk factors were also at significantly increased hazards for device thrombosis (suspected or confirmed) [adjusted HR 1.19 (95% CI 1.06–1.33), p = 0.002]. This was driven by increased hazards among those with drug use, other major psychiatric disease, and a history of non-compliance (p <0.05 for all).
There were 2279 (14.8%) individuals with ischemic or hemorrhage stroke during the study period. There was no statistically significant association with risk of stroke (ischemic or hemorrhagic) among patients with any psychosocial risk in an adjusted Cox regression model [HR 1.11 (95% CI 0.99–1.24, p = 0.07]. However, non-compliance was associated with a significantly increased risk of stroke [HR 1.38 (95% CI 1.11–1.71, p = 0.004].
Hospital readmissions were common, occurring in 11,323 (73.5%) patients throughout the study period. In addition, patients with psychosocial risk factors had significantly increased hazards for all-cause hospital readmission [adjusted HR 1.14 (95% CI 1.08–1.19), p <0.001]. Nearly all subpopulations were at significantly increased hazards for hospital readmissions with the exception of limited cognition and history of non-compliance where no statistically significant associations were seen.
Approximately one in four patients received cardiac transplantation [n =3738 (24.2%)]. Patients with psychosocial risk factors were significantly less likely to undergo cardiac transplantation [adjusted HR 0.85 (95% CI 0.80–0.91), p < 0.001]. At 3-year follow-up, the incidence of transplant was 41.0% in the no psychosocial risk group, compared to 35.9% in the group with at least one psychosocial risk factor (log rank p <0.001).
Additive Impact of Multiple Psychosocial Risk Factors
An additional analysis was performed to assess the impact of the number of psychosocial risk factors on outcomes. In patients with 2 or more psychosocial risk factors, the hazards of cardiac transplantation were significantly lower [adjusted HR 0.72 (95% CI 0.61–0.87), p < 0.001] compared to those without psychosocial risk (Table 3). The hazards of device-related infection, gastrointestinal bleeding, device thrombosis, and hospital readmission were all significantly higher in the group with 2 or more psychosocial risk factors. Survival on pump support was still not significantly different, even among the subgroup with 2 or more psychosocial risk factors [adjusted HR 0.94(95% CI 0.79–1.12), p = 0.49]. Patients with 2 or more psychosocial risk factors had significantly higher risk of driveline infection compared to patients with only 1 psychosocial risk factor [adjusted HR 1.22 (95% CI 0.80–0.91), p = 0.034, Supplemental Table 2).
Table 3.
Additive Impact of Psychosocial Risk Factors on LVAD Outcomes
| LVAD Outcomes | Unadjusted Cox Regression | Adjusted Cox Regression* | ||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Survival on pump support | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 0.87 (0.79 – 0.96) | 0.004 | 1.01 (0.91 – 1.12) | 0.842 |
| 2+ Psychosocial Risk Factors | 0.76 (0.64 – 0.89) | 0.001 | 0.94 (0.79 – 1.12) | 0.495 |
| Cardiac Transplantation | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 0.87 (0.79 – 0.95) | 0.002 | 0.86 (0.78 – 0.95) | 0.003 |
| 2+ Psychosocial Risk Factors | 0.70 (0.59 – 0.82) | <0.001 | 0.72 (0.60 – 0.86) | <0.001 |
| Device Related Infection | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 1.31 (1.18 – 1.46) | <0.001 | 1.23 (1.10 – 1.37) | <0.001 |
| 2+ Psychosocial Risk Factors | 1.40 (1.28 – 1.54) | <0.001 | 1.49 (1.27 – 1.76) | <0.001 |
| Gastrointestinal Bleeding | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 0.97 (0.89 – 1.06) | 0.546 | 1.18 (1.07 – 1.29) | 0.001 |
| 2+ Psychosocial Risk Factors | 0.98 (0.85 – 1.14) | 0.803 | 1.29 (1.11 – 1.51) | 0.001 |
| Device Thrombosis (Suspected or Confirmed) | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 1.21 (1.07 – 1.36) | 0.002 | 1.15 (1.01 – 1.31) | 0.031 |
| 2+ Psychosocial Risk Factors | 1.47 (1.23 – 1.76) | <0.001 | 1.32 (1.09 – 1.59) | 0.005 |
| Stroke (Ischemic or Hemorrhagic) | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 1.03 (0.92 – 1.15) | 0.656 | 1.12 (1.00 – 1.27) | 0.059 |
| 2+ Psychosocial Risk Factors | 0.98 (0.81 – 1.19) | 0.864 | 1.06 (0.86 – 1.30) | 0.585 |
| Hospital Readmission | ||||
| 0 Psychosocial Risk Factor | … | … | … | … |
| 1 Psychosocial Risk Factor | 1.06 (1.00 – 1.12) | 0.022 | 1.12 (1.06 – 1.18) | <0.001 |
| 2+ Psychosocial Risk Factors | 1.12 (1.03 – 1.22) | 0.006 | 1.21 (1.11 – 1.32) | <0.001 |
Discussion
The current study examines the burden of psychosocial risk factors among patients who have received LVADs and its association with post-implant outcomes. The important findings include: 1) One or more psychosocial risk factors was present in approximately 20% of LVAD recipients; 2) Patients with psychosocial risk were more likely to be young, non-white, men with more severe cardiac disease; and 3) Patients with psychosocial risk were at increased hazards for device-related infection, gastrointestinal bleeding, pump thrombosis, and hospital readmission compared to those without psychosocial risk, with particular risk factors contributing to different outcomes. However, overall psychosocial risks were not significantly associated with survival or stroke. Taken together, these findings highlight the adverse outcomes associated with psychosocial risk and the need for programs to address these factors to improve both LVAD outcomes and access to heart transplantation.
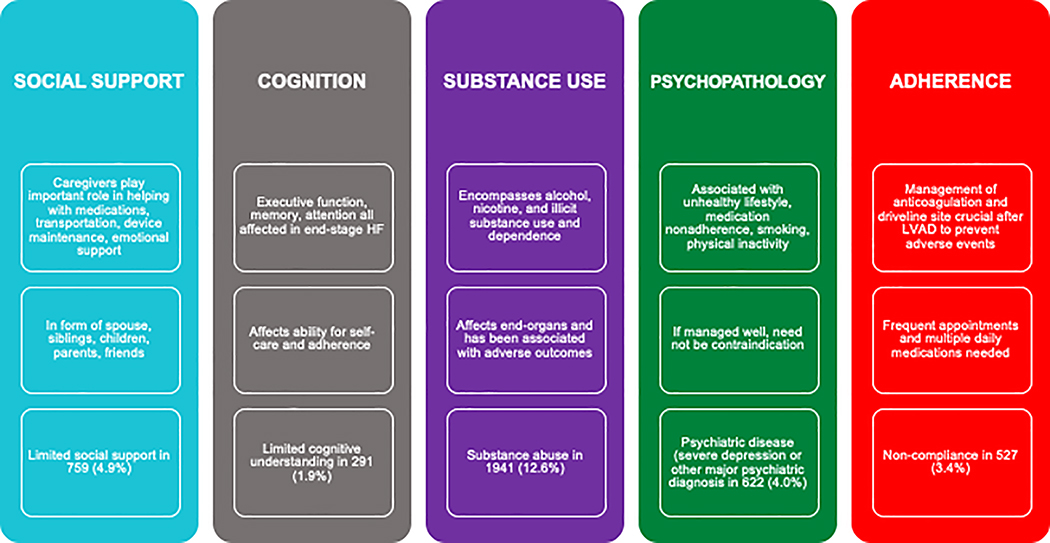
In our study, one in five LVAD recipients had at least one marker of elevated psychosocial risk. Our definition of psychosocial risk incorporated five distinct domains, all of which are mentioned in the 2018 ISHLT consensus statement,7 and are captured in previously validated objective psychosocial assessments such as the SIPAT,14,15,20 PACT,16,17 and the TERS (Figure 3).18 The most common risk factor was substance abuse, followed by limited social support, severe psychiatric disease, non-compliance, and limited cognition. Notably, the majority of patients with psychosocial risk had only one psychosocial risk factor with a small minority having two or three of the five risk factors. This likely reflects that patients would not have been deemed appropriate candidates if they had multiple co-existing risk factors.
Figure 3. The Five Domains of Psychosocial Risk.
This schematic further summarizes the five components of psychosocial risk evaluated in the current study. Connections were made between risk factors and outcomes if the adjusted hazard ratios were statistically significant. The multivariate model used was adjusted for age, gender, race, heart failure etiology, body surface area (BSA), year of implant, history of right ventricular assist device (RVAD) use, pump type (axial vs. centrifugal), INTERMACS profile, device strategy (destination therapy vs bridge to transplant or recovery), creatinine, bilirubin, and albumin levels.
Patients with psychosocial risk were significantly more likely to be young, non-white, men with more severe cardiac disease. They were more likely to require inotrope therapy as well as IABP therapy prior to LVAD implant. Yet, patients with psychosocial risk were significantly more likely to receive an LVAD as destination therapy and significantly less likely to be listed for transplant. One can suspect that many of these patients would medically be candidates for transplant given their age, acuity of illness, and preserved end-organ function. As the most common psychosocial risk factor in our analysis was substance use, we hypothesize that this likely precluded their candidacy in addition to active smoking which was significantly higher in the psychosocial risk group. We have previously demonstrated that LVAD recipients of lower socioeconomic status have similar demographics (young, non-white), less likely to be married, more likely to have public insurance, and less likely to be employed.21 Notably, in this analysis, socioeconomic status did not significantly impact post-LVAD outcomes. Furthermore, substance use disorders nationally are most commonly seen in young men.22,23 This highlights the need for screening and implementation of effective psychologic and medical treatments for substance use disorders in this population.24 With effective treatment and close follow-up, these patients may become candidates for heart transplantation in the future.
Following LVAD implant, patients with psychosocial risk were at increased hazards for multiple device-related complications. After adjusting for a number of patient-specific and device-specific factors, patients with psychosocial risk remained at significantly increased hazards for device-related infection, gastrointestinal bleeding, pump thrombosis, and hospital readmission compared to those without psychosocial risk. Prior studies which have evaluated retrospectively psychosocial risk in LVAD recipients have found mixed results, but have been limited by small sample sizes. For example, Halkar and colleagues used the PACT to retrospectively examine 230 LVAD patients and found no associations between psychosocial risk and readmissions, pump thrombosis, driveline infections, GI bleeding, or survival.17 Of note, 97% of the study population had PACT scores in the range of “acceptable to excellent candidate.” On the other hand, Maltby and colleagues16, found a significant association between lower psychosocial risk and readmissions after LVAD implant with no differences in survival, a finding also replicated in other studies.25,26 However, given the increased risk of other complications, these patients likely have worse quality of life. One strength of our analysis was the significantly larger sample size which gave us adequate power to explore these associations.
Notably, the hazard ratios for most outcomes were similar, indicating an approximately 20% increased risk of complications in patients with only one psychosocial risk factor. Yet, this may be an acceptable risk when compared to withholding of LVAD therapy altogether in these higher risk patients who are typically young with severe heart failure syndrome, particularly when we found no difference in survival on pump support. The risk of these complications nearly doubled in patients with 2 or more risk factors. In addition, we may be able to mitigate these risks by developing systems of support, providing access to addiction medicine, and broader mental health resources for our patients. These may also help to improve their candidacy for organ transplantation.
We also found that different psychosocial variables may be more associated with specific outcomes in the LVAD population. These variables may differ from heart transplant recipients. For example, increased GI bleeding was primarily observed in subpopulations of patients with alcohol abuse, severe depression and a history of non-compliance whereas pump thrombosis was driven primarily by those with major psychiatric disease other than depression, drug use, and history of non-compliance. This is not surprising given that alcohol abuse can lead to the development of coagulopathy as well as mucosal injury leading to increased bleeding.27 Typically, there is an inverse relationship between bleeding and clotting. However, we found an increased hazards for both GI bleeding and pump thrombosis among those with a history of non-compliance, reflecting an inability to maintain therapeutic oral anticoagulation perhaps developing both sub- and supratherapeutic internationalized normalized ratio values.28
Our study has limitations that should be acknowledged. Perhaps the most significant limitation is the fact that INTERMACS only includes patients who have received an LVAD implant; therefore, it does not include psychosocial risk for those who were not deemed eligible for the therapy. This study was a retrospective analysis using registry data. Furthermore, there may be center-specific differences regarding how patients were coded as having limited social support, limited cognitive understanding, or repeated non-compliance. These can be challenging to define and therefore, may be subject to biases. For example, perhaps non-white individuals are more likely to be coded for specific risk factors when compared to white individuals due to unconscious biases. In addition, for substance abuse, it is unclear when this occurred in relation to the timing of VAD implant. Information regarding rehabilitation treatments were not available nor was information regarding neurocognitive assessments. This highlights the importance of using formal psychosocial assessment tools in future multicenter studies.
In conclusion, patients with psychosocial risk factors are at risk for adverse outcomes and complications after LVAD implantation. Five broad categories including social support, cognition, substance use, psychopathology, and non-compliance may each predict their own set of post-LVAD complications. However, these factors exist within a broader societal, cultural, and economic context. Therefore, in order to ensure equitable access to advanced heart failure therapies, we must also address these factors through developing interventions in future studies.
Supplementary Material
What is new?
Nearly 1 in 5 left ventricular assist device recipients have psychosocial risk factors such as limited social support, limited cognition, substance abuse, severe psychiatric disease, or non-compliance. Psychosocial risk is not associated with increased mortality on LVAD support. However, patients with psychosocial risk are at increased risk for device-related infection, gastrointestinal bleeding, pump thrombosis, and hospital readmission and are significantly less likely to receive cardiac transplantation.
What are the clinical implications?
When evaluating advanced heart failure patients for left ventricular assist device therapy, special attention should be paid to psychosocial risk factors that may impact long-term complications on pump support. Psychosocial risk alone should not be an absolute contraindication to device therapy given lack of increased mortality in this population. Through developing systems of support, broader mental health resources, and access to addition medicine, we can help improve these outcomes as well as their candidacy for heart transplantation on device support.
Acknowledgments
Sources of Funding: None
Non-Standard Abbreviations and Acronyms
- LVAD
left ventricular assist device
- INTERMACS
Interagency Registry for Mechanically Assisted Circulatory Support
- ISHLT
International Society for Heart and Lung Transplantation
- PACT
Psychosocial Assessment of Candidates for Transplantation
- SIPAT
Psychosocial Assessment for Transplant
- TERS
Transplant Evaluation Rating Scale (TERS)
Footnotes
Disclosure Statement: None
References
- 1.Mehra MR, Goldstein DJ, Uriel N, Cleveland JC, Yuzefpolskaya M, Salerno C, Walsh MN, Milano CA, Patel CB, Ewald GA, Itoh A, Dean D, Krishnamoorthy A, Cotts WG, Tatooles AJ, Jorde UP, Bruckner BA, Estep JD, Jeevanandam V, Sayer G, Horstmanshof D, Long JW, Gulati S, Skipper ER, O’Connell JB, Heatley G, Sood P, Naka Y, MOMENTUM 3 Investigators. Two-Year Outcomes with a Magnetically Levitated Cardiac Pump in Heart Failure. N Engl J Med. 2018;378:1386–1395. [DOI] [PubMed] [Google Scholar]
- 2.Bui QM, Allen LA, LeMond L, Brambatti M, Adler E. Psychosocial Evaluation of Candidates for Heart Transplant and Ventricular Assist Devices: Beyond the Current Consensus. Circ: Heart Failure [Internet]. 2019. [cited 2019 Nov 14];12 Available from: https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.119.006058 [DOI] [PubMed]
- 3.Givertz MM. Cardiology patient pages: ventricular assist devices: important information for patients and families. Circulation. 2011;124:e305–311. [DOI] [PubMed] [Google Scholar]
- 4.Petty M, Bauman L. Psychosocial issues in ventricular assist device implantation and management. J Thorac Dis. 2015;7:2181–2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eshelman AK, Mason S, Nemeh H, Williams C. LVAD destination therapy: applying what we know about psychiatric evaluation and management from cardiac failure and transplant. Heart Fail Rev. 2009;14:21–28. [DOI] [PubMed] [Google Scholar]
- 6.Dew MA, DiMartini AF, Dobbels F, Grady KL, Jowsey-Gregoire SG, Kaan A, Kendall K, Young Q-R. The Approach to the Psychosocial Evaluation of Cardiac Transplant and Mechanical Circulatory Support Candidates. Curr Heart Fail Rep. 2019;16:201–211. [DOI] [PubMed] [Google Scholar]
- 7.Dew MA, DiMartini AF, Dobbels F, Grady KL, Jowsey-Gregoire SG, Kaan A, Kendall K, Young Q-R, Abbey SE, Butt Z, Crone CC, De Geest S, Doligalski CT, Kugler C, McDonald L, Ohler L, Painter L, Petty MG, Robson D, Schlöglhofer T, Schneekloth TD, Singer JP, Smith PJ, Spaderna H, Teuteberg JJ, Yusen RD, Zimbrean PC. The 2018 ISHLT/APM/AST/ICCAC/STSW recommendations for the psychosocial evaluation of adult cardiothoracic transplant candidates and candidates for long-term mechanical circulatory support. J Heart Lung Transplant. 2018;37:803–823. [DOI] [PubMed] [Google Scholar]
- 8.Maldonado JR, Dubois HC, David EE, Sher Y, Lolak S, Dyal J, Witten D. The Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT): a new tool for the psychosocial evaluation of pre-transplant candidates. Psychosomatics. 2012;53:123–132. [DOI] [PubMed] [Google Scholar]
- 9.Maldonado JR, Sher Y, Lolak S, Swendsen H, Skibola D, Neri E, David EE, Sullivan C, Standridge K. The Stanford Integrated Psychosocial Assessment for Transplantation: A Prospective Study of Medical and Psychosocial Outcomes. Psychosom Med. 2015;77:1018–1030. [DOI] [PubMed] [Google Scholar]
- 10.Vandenbogaart E, Doering L, Chen B, Saltzman A, Chaker T, Creaser JW, Rourke D, Cheng RW, Fonarow GC, Deng M. Evaluation of the SIPAT instrument to assess psychosocial risk in heart transplant candidates: A retrospective single center study. Heart Lung. 2017;46:273–279. [DOI] [PubMed] [Google Scholar]
- 11.Hitschfeld MJ, Schneekloth TD, Kennedy CC, Rummans TA, Niazi SK, Vasquez AR, Geske JR, Petterson TM, Kremers WK, Jowsey-Gregoire SG. The Psychosocial Assessment of Candidates for Transplantation: A Cohort Study of its Association With Survival Among Lung Transplant Recipients. Psychosomatics. 2016;57:489–497. [DOI] [PubMed] [Google Scholar]
- 12.Twillman RK, Manetto C, Wellisch DK, Wolcott DL. The Transplant Evaluation Rating Scale. A revision of the psychosocial levels system for evaluating organ transplant candidates. Psychosomatics. 1993;34:144–153. [PubMed] [Google Scholar]
- 13.Dieplinger G, Mokhaberi N, Wahba R, Peltzer S, Buchner D, Schlösser HA, Ditt V, von Borstel A, Bauerfeind U, Lange U, Arns W, Kurschat C, Stippel DL, Vitinius F. Correlation Between the Transplant Evaluation Rating Scale (TERS) and Medical Outcomes in Living-Donor Kidney Transplant Recipients: A Retrospective Analysis. Transplant Proc. 2018;50:1276–1280. [DOI] [PubMed] [Google Scholar]
- 14.Bui QM, Braun OO, Brambatti M, Gernhofer YK, Hernandez H, Pretorius V, Adler E. The value of Stanford integrated psychosocial assessment for transplantation (SIPAT) in prediction of clinical outcomes following left ventricular assist device (LVAD) implantation. Heart Lung. 2019;48:85–89. [DOI] [PubMed] [Google Scholar]
- 15.Cagliostro M, Bromley A, Ting P, Donehey J, Ferket B, Parks K, Palumbo E, Mancini D, Anyanwu A, Pawale A, Pinney S, Moss N, Lala A. Standardized Use of the Stanford Integrated Psychosocial Assessment for Transplantation in LVAD Patients. J Card Fail. 2019;25:735–743. [DOI] [PubMed] [Google Scholar]
- 16.Maltby MC, Flattery MP, Burns B, Salyer J, Weinland S, Shah KB. Psychosocial assessment of candidates and risk classification of patients considered for durable mechanical circulatory support. J Heart Lung Transplant. 2014;33:836–841. [DOI] [PubMed] [Google Scholar]
- 17.Halkar M, Nowacki AS, Kendall K, Efeovbokhan N, Gorodeski EZ, Moazami N, Starling RC, Young JB, Lee S, Tang WHW. Utility of the Psychosocial Assessment of Candidates for Transplantation in Patients Undergoing Continuous-Flow Left Ventricular Assist Device Implantation. Prog Transpl. 2018;28:220–225. [DOI] [PubMed] [Google Scholar]
- 18.Yost GL, Bhat G, Ibrahim KN, Karountzos AG, Chandrasekaran M, Mahoney E. Psychosocial Evaluation in Patients Undergoing Left Ventricular Assist Device Implantation Using the Transplant Evaluation Rating Scale. Psychosomatics. 2016;57:41–46. [DOI] [PubMed] [Google Scholar]
- 19.Bruce CR, Delgado E, Kostick K, Grogan S, Ashrith G, Trachtenberg B, Estep JD, Bhimaraj A, Pham L, Blumenthal-Barby JS. Ventricular assist devices: a review of psychosocial risk factors and their impact on outcomes. J Card Fail. 2014;20:996–1003. [DOI] [PubMed] [Google Scholar]
- 20.Sperry BW, Ikram A, Alvarez PA, Perez AL, Kendall K, Gorodeski EZ, Starling RC. Standardized Psychosocial Assessment Before Left Ventricular Assist Device Implantation. Circ Heart Fail. 2019;12:e005377. [DOI] [PubMed] [Google Scholar]
- 21.Clemons AM, Flores RJ, Blum R, Wayda B, Brunjes DL, Habal M, Givens RC, Truby LK, Garan AR, Yuzefpolskaya M, Takeda K, Takayama H, Farr MA, Naka Y, Colombo PC, Topkara VK. Effect of Socioeconomic Status on Patients Supported with Contemporary Left Ventricular Assist Devices. ASAIO J. 2019; [DOI] [PubMed] [Google Scholar]
- 22.Gomes T, Tadrous M, Mamdani MM, Paterson JM, Juurlink DN. The Burden of Opioid-Related Mortality in the United States. JAMA Netw Open. 2018;1:e180217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones CB, Hill ML, Pardini DA, Meier MH. Prevalence and correlates of vaping cannabis in a sample of young adults. Psychol Addict Behav. 2016;30:915–921. [DOI] [PubMed] [Google Scholar]
- 24.Parker R, Armstrong MJ, Corbett C, Day EJ, Neuberger JM. Alcohol and substance abuse in solid-organ transplant recipients. Transplantation. 2013;96:1015–1024. [DOI] [PubMed] [Google Scholar]
- 25.Snipelisky D, Stulak JM, Schettle SD, Sharma S, Kushwaha SS, Dunlay SM. Psychosocial characteristics and outcomes in patients with left ventricular assist device implanted as destination therapy. Am Heart J. 2015;170:887–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lundgren S, Lowes BD, Zolty R, Burdorf A, Raichlin E, Um JY, Poon C. Do Psychosocial Factors Have Any Impact on Outcomes After Left Ventricular Assist Device Implantation? ASAIO J. 2018;64:e43–e47. [DOI] [PubMed] [Google Scholar]
- 27.Andersen IB, Jørgensen T, Bonnevie O, Grønbaek M, Sørensen TI. Smoking and alcohol intake as risk factors for bleeding and perforated peptic ulcers: a population-based cohort study. Epidemiology. 2000;11:434–439. [DOI] [PubMed] [Google Scholar]
- 28.Nassif ME, LaRue SJ, Raymer DS, Novak E, Vader JM, Ewald GA, Gage BF. Relationship Between Anticoagulation Intensity and Thrombotic or Bleeding Outcomes Among Outpatients With Continuous-Flow Left Ventricular Assist Devices. Circ Heart Fail. 2016;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.