Highlights
-
•
Spontaneous pneumothorax due to COVID-19 may happen in never-ventilated patients.
-
•
Due to persistence, these pneumothoraces may need surgery for bulla resection.
-
•
Endothelitis as seen in other organs may contribute to prolonged healing.
Keywords: COVID-19, Pneumothorax, Thoracoscopy
Abstract
Introduction
Patients with COVID-19 infection and severe lung parenchyma alterations may need mechanical ventilation with subsequent pneumothorax and eventually persistent air leak in case of pre-existing lung disease.
Presentation of case
This report presents the case of a never-ventilated 58 years old male patient without pre-existing, underlying lung disease demonstrating severe lung parenchyma changes due to COVID-19-pneumonia. He suffered from recurrent bilateral spontaneous pneumothoraces, which were successfully treated with bilateral thoracoscopy and resections of the destroyed lung areas. Notably, he has already been under treatment with anticoagulation due to portal thrombosis 8 years ago.
Discussion
Although especially know from patients under mechanical ventilation, this patient suffered from spontaneous pneumothorax without ever been ventilated. Probably due to the severe vascular inflammatory changes and focal endothelitis like also seen in other organs of COVID-19 patients, the pneumothorax may lead to a prolonged air leak, which needs surgical therapy. The patients pre-existing anticoagulation therapy may prevented him from a mere severe course.
Conclusion
Early surgical therapy may be considered in COVID-19 patients with persistent air leak, even if not mechanically ventilated. Simultaneously, the role of early anticoagulation needs further investigation.
1. Introduction
Increasing reports about lung parenchyma alterations in SARS-CoV-2 patients are emerging [[1], [2], [3], [4], [5]]. Radiological and histological findings suggest inflammatory interstitial changes as seen in cryptogenic organizing pneumonia (COP [4,5]). In case of mechanical ventilation, iatrogenic pneumothorax with chest tube management might occur [2]. A recent report describes two cases of COVID-19 patients with persistent air leak under mechanical ventilation, where thoracoscopic bleb resection was performed [6]. While pneumothorax has been described as rare clinical manifestation in COVID-19 patients [[1], [2], [3]], to our knowledge no reports about persistent air leaks in non-ventilated patients with no pre-existing underlying lung disease like emphysema or blebs have been presented yet. According to our observations in these cases, early thoracoscopy might be indicated.
2. Presentation of case
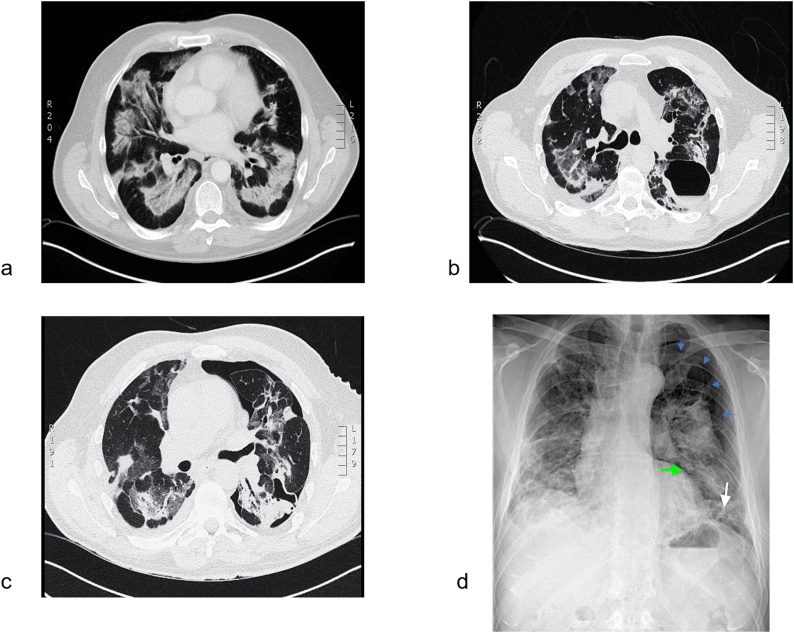
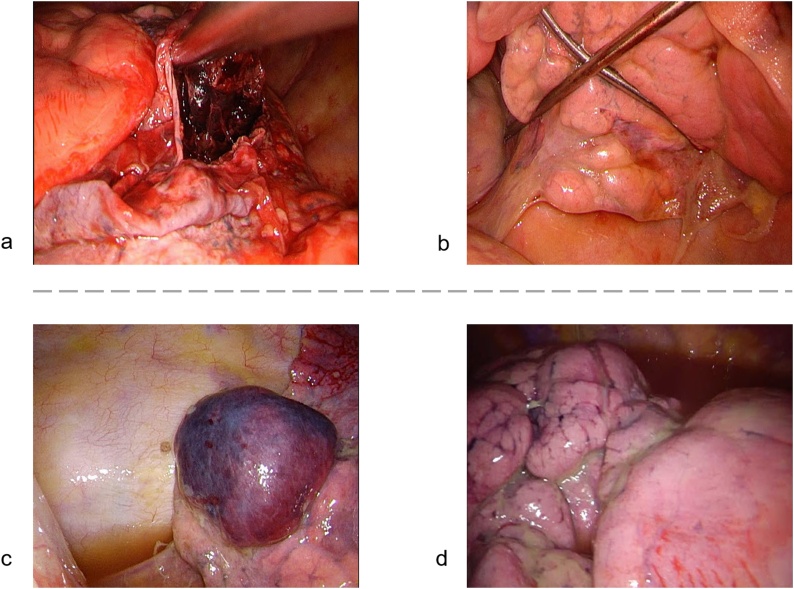
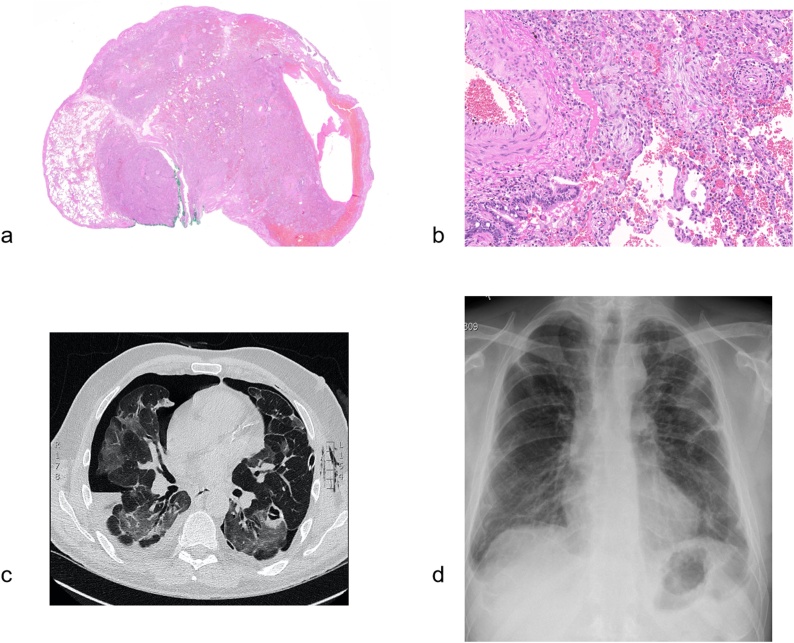
A 58 year-old police officer was admitted to a regional hospital for a severe dry cough and progressive discomfort. Besides arterial hypertension, adipositas (BMI 30.7 kg/m2) and portal vein thrombosis 8 years ago treated with consecutive oral anticoagulation, the patient was otherwise healthy. This never-smoker had no underlying symptomatic lung disease. Subsequently, he was diagnosed with COVID-19 after a CT scan (Fig. 1a) showed typical COVID-19 associated findings including ground-glass consolidation and crazy-paving pattern although two nasopharyngeal swabs showed negative PCR results. An antibody and nasopharyngeal swab test on day 3 after hospitalization confirmed the diagnosis. The patient had a prolonged course of disease with recurrent sub-febrile temperatures, fluctuating inflammatory blood parameters, anosmia and dysgeusia, constant oxygen dependency and increasing inflammatory changes on CT scan (Fig. 1b). 22 days later a singular dose of tocilizumab 800 mg was administered followed by a fast subjective improvement of the patient’s clinical condition. However, on day 26 he developed a spontaneous pneumothorax on his left side (Fig. 1c), which was initially drained with a 12-French chest tube. Four days later a second tube was placed due to an inadequately expanded lung. After initial re-expansion, the patient suffered from recurrent pneumothorax 5 days later (Fig. 1d). With recurrent episodes of air leak, the patient was transferred to us. We inserted a larger chest tube (28 French), leading to pulmonary re-expansion which, however, lasted only for 24 h. We performed an exploratory thoracoscopy on the left side (10 days after initial pneumothorax). A bulla-like lesion filled with hematoma on segment 6 (Fig. 2a) was observed. The entire lung was covered with a thin layer of fibrin deposits and showed several cauliflower-like scarred lesions, possibly corresponding to the COP like lesions seen on CT (Fig. 2b). The hematoma was resected with reinforced stapling devices and two chest tubes were placed. Six days later the patient developed a spontaneous pneumothorax on the right side (Fig. 3c) and was directly scheduled for thoracoscopy. No active air leak was found, but the lower lobe showed again a bulla-like hematoma (Fig. 2c). Scarred lesions were found on the lower and middle lobe (Fig. 2d). The hematoma was resected. The histology of the resected material from both sides showed fibrotic tissue, fibrinous inflammatory changes, intra-alveolar hemorrhage and reactive mesothelial changes as well as endothelitis (Fig. 3a and b).
Fig. 1.
The progression of SARS-CoV2 previous to being transferred to our department. a) CT-scan showing focal consolidation with ground-glass peribronchovascular changes. b) CT-scan 1 month later showing perilobular consolidation and reverse Halo-sign, similar to organizing pneumonia and newly appeared cystic lesions. c) CT-scan showing spontaneous pneumothorax. d) X-ray image showing the extend of pneumothorax (blue arrows) and two chest tubes (green and white arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Fig. 2.
Intraoperative images from the two first thoracoscopies. On the left side: a) prominent ruptured bulla (consecutively resected). b) adhesions and cauliflower like rearrangement of lung tissue. Procedure 2 on the right side: c) blood filled bulla (consecutively resected). d) cauliflower like rearrangement of lung tissue.
Fig. 3.
a) Microscopic picture of the resected lung tissue with defined area of atelectatic lung with intra-aleveolar hemorrhage and subpleural hematoma. (Hematoxylin Eosin staining (HE), 50× magnification). b) residual endotheliitis in small and medium sized vessel and intra-alveolar polypoid fibroblast plugs specifying organizing pneumonia (HE, 200× magnification). c) CT-scan showing spontaneous pneumothorax on the right side and residual ground-glass opacities. d) final X-ray about 5 weeks after hospitalization showing a fully re-expanded lung.
Left-sided redo-thoracoscopy with wedge resection and implantation of an indwelling permanent pleura catheter was performed 18 days after surgery due to persisting air leak. The patient was dismissed into rehabilitation in an improved general state of health after almost 2 months of hospitalization in total, without significant air leak indicated by the attached drainage system.
The indwelling permanent pleura catheter was removed in an outpatient setting 30 days after dismissal from the hospital and after successful rehabilitation. He had almost fully recovered and was about to start working again. The final X-ray after removal of the permanent pleural catheter showed a fully expanded lung (Fig. 3d). This case presentation is performed following the SCARE guidelines [6].
3. Discussion
To our knowledge, this is the first reported case of SARS-CoV-2 related pneumothorax treated by thoracoscopic wedge-resection in a patient without pre-existing lung disease or history of mechanical ventilation. Pneumothorax is a rare COVID-19 associated complication with only a few descriptions in current literature [[1], [2], [3]]. Aiolfi et al. have published two cases of thoracoscopic wedge-resection in intubated patients who suffered from pneumothorax as successful surgical intervention after persistent air leakage. Long-term outcome of these cases is unknown [7]. Our case shows a prolonged recovery after delayed wedge resection due to spontaneous pneumothorax directly in contrast to quick recovery after almost immediate surgical intervention to treat pneumothorax on the opposite side.
Histological changes of the resected lung wedge demonstrated typical signs as vascular inflammatory changes, focal endothelitis and signs of an organizing pneumonia with intra-alveolar hemorrhagic areas, which have been previously described in association with COVID-19 infection [4,5]. Whether the phenomenon of the intra-alveolar hemorrhages represents a morphological picture of the viral induced disturbed pulmonary microvasculature or is a result of the necessary anticoagulation therapy, needs to be addressed in further studies [4,5]. As suggested in the literature, and based on the intraoperative images of chronic cauliflower-like lesions in this patient, we assume that the viral-induced pulmonary changes lead to a consequent increased frailty of tissue [1]. In CT scans, lesions are often seen subpleurally and in peripheral location [8], much in accordance with our intraoperative findings.
Notable in our patient is that at no point mechanical ventilation was necessary despite the severe lung tissue alterations. Given the recent findings that SARS-CoV-2’s adhesion to the ACE2 receptor also in endothelia can cause micro-embolism [4], the patient’s continuous therapeutic anticoagulation might have prevented him from suffering a more serious course. Improved outcome in patients who received anticoagulation when showing signs of disseminated intravascular coagulopathy was reported [9].
4. Conclusion
Early surgical intervention as well as early use of anticoagulation in patientsdeserve further investigation.
Disclosure
All authors report no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
In Switzerland, case reports are not required to be voted by the Swiss Ethics. If required, this specific confirmation can be given later. See Informed Consent below.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
-
1.
Conceptualization: CC, LW, IO.
-
2.
Data curation: CC, LW, GH, CA, MH, ZV, TF, IO.
-
3.
Formal analysis: CC, LW, GH, CA, MH, ZV, TF, IO.
-
4.
Funding acquisition: n/a.
-
5.
Investigation & Methodology: CC, LW, GH, CA, MH, ZV, TF, IO.
-
6.
Project administration: CC, IO.
-
7.
Resources: CC, LW, GH, CA, MH, ZV, TF, IO.
-
8.
Software: n/a.
-
9.
Supervision: IO.
-
10.
Validation: CC, LW, IO.
-
11.
Visualization: CC, LW, IO.
-
12.
Writing - original draft: CC, LW.
-
13.
Writing - review & editing: CC, LW, GH, CA, MH, ZV, TF, IO.
Registration of research studies
N/A.
Guarantor
Claudio Caviezel & Isabelle Opitz.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Sun R., Liu H., Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J. Radiol. 2020;21(5):541–544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rohailla S., Ahmed N., Gough K. SARS-CoV-2 infection associated with spontaneous pneumothorax. Can. Med. Assoc. J. 2020 doi: 10.1503/cmaj.200609. cmaj.200609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang W., Gao R., Zheng Y., Jiang L. COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema. J. Travel Med. 2020;27(5) doi: 10.1093/jtm/taaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S.Y. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 2020;15(5):700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2018;(60):132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Aiolfi A., Biraghi T., Montisci A. Management of persistent pneumothorax with thoracoscopy and blebs resection in Covid-19 patients. Ann. Thorac. Surg. 2020 doi: 10.1016/j.athoracsur.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu Q., Guan H., Sun Z. Early CT features and temporal lung changes in COVID-19 pneumonia in Wuhan, China. Eur. J. Radiol. 2020;(January) doi: 10.1016/j.ejrad.2020.109017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020;(March):1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]