We read with great interest the report by Issa et al.1 describing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-associated pancytopenia. Infection with SARS-CoV-2 and the resulting Corona virus disease (COVID-19) can affect virtually any organ of the human body, including the bone marrow. We report a case of pancytopenia associated with COVID-19 infection. While this case shares similarities with that reported previously,1 there are also differences which merit consideration.
A 49-year-old man was diagnosed in 2014 with follicular lymphoma grade 3A, stage IVA (Lugano) with involvement of the bone marrow. The patient had normal blood work and was followed without treatment. In 2017, transformation to diffuse large B-cell lymphoma, stage IVB, was diagnosed on bone marrow biopsy and he received immunochemotherapy. End-of-treatment positron emission tomography–computed tomography showed mixed response and bone marrow biopsy found no lymphoma cells, but grade 3 fibrosis.
Relapse of diffuse large B-cell lymphoma was confirmed in April 2019. Salvage chemotherapy followed by high-dose chemotherapy with autologous stem cell support resulted in complete remission. Bone marrow biopsy before autologous stem cell support contained no lymphoma or fibrosis. In October 2019 and January 2020, blood work was normal and a computed tomography scan in January 2020 still showed a complete remission.
In April 2020, the patient was admitted with fever and symptoms of an upper respiratory tract infection. Throat swab was positive for COVID-19. He was discharged after a few days, only to be admitted again 10 days later with continuous fever and cough.
The blood work at the time of second hospitalization showed, for the first time, a low platelet count (Figure 1 ). He was still positive for COVID-19 by tracheal suction. With suspicion of immune thrombocytopenia, which has previously been associated with COVID-19,2 the patient was started on immunoglobulin infusions, but never received steroids. He had normal platelets in late January, but then the platelet count steadily declined from the middle of April, coinciding with COVID-19 symptoms. Both neutrophil counts and hemoglobin decreased as well (Figure 1). In addition to immunoglobulin, he was treated with meropenem on suspicion of bacterial superinfection, but despite repeated microbiological examination of blood, urine, mouth wash and tracheal secretions, no other microbiological agents were found apart from SARS-CoV-2.
Figure 1.
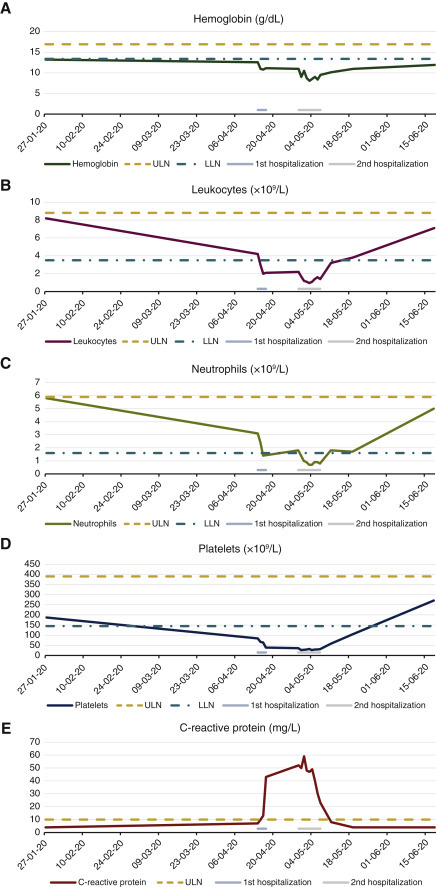
Temporal evolution of (A) hemoglobin, (B) leukocyte count, (C) neutrophil count, (D) platelets and (E) C-reactive protein.
Upper limit of normal (ULN) and lower limit of normal (LLN) according to local laboratory standards are indicated with the dotted lines. Periods of hospitalization are marked with the gray horizontal lines.
Bone marrow biopsy to investigate the cause of pancytopenia found nonspecific reactive changes, with no sign of lymphoma, fibrosis or myelodysplasia. RT-PCR analysis of bone marrow aspirate was negative for SARS-CoV-2.
After the patient's infection resolved, his cytopenia improved. At his most recent outpatient visit, platelets, leukocytes and neutrophils had all normalized and only slight anemia remained.
Compared with the case of COVID-19-associated pancytopenia reported by Issa et al.,1 this case was characterized by a much milder clinical course, an inability to detect COVID-19 in the bone marrow aspirate and a temporally limited duration of pancytopenia matching the duration of infection. As such, pancytopenia in the setting of patients with secondary immunodeficiency with COVID-19 may resemble the type of secondary bone marrow suppression seen in other cases of viral infection.
The patient has consented to the writing of this case report.
Acknowledgments
Funding
None declared.
Disclosure
The authors have declared no conflicts of interest.
References
- 1.Issa N., Lacassin F., Camou F. First case of persistent pancytopenia associated with SARS-CoV-2 bone marrow infiltration in an immunocompromised patient. Ann Oncol. 2020;31(10):1418–1419. doi: 10.1016/j.annonc.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zulfiqar A.A., Lorenzo-Villalba N., Hassler P., Andrès E. Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med. 2020;382(18):e43. doi: 10.1056/NEJMc2010472. [DOI] [PMC free article] [PubMed] [Google Scholar]


