Abstract
A 45-year-old man was admitted to the Emergency Department with fatigue and muscular weakness. Soon after hospital admission, he developed “torsades de pointe” and was successfully resuscitated. The admission laboratory investigations had revealed a profound hypokalemia (1.65 mmol/L). The patient had a long-term use of alcohol-free “pastis” in an attempt to reduce his chronic ethanol consumption. As the beverage likely contained a significant amount of liquorice, the diagnosis of glycyrrhizin chronic intoxication was suspected. The diagnosis of liquorice-related pseudohyperaldosteronism was assessed by normal plasma aldosterone levels and low plasma renin activity. Intravenous and oral supplementation of potassium was required for 5 days, and the patient had an uneventful follow-up.
1. Introduction
Liquorice root (Glycyrrhiza gabra) is one of the oldest plants used in some traditional medicines. The major bioactive principle is glycyrrhizic acid which has been shown to inhibit (after intestinal hydrolysis to glycyrrhetic acid) the enzyme 11-β-hydroxysteroid dehydrogenase. This could result to pseudohyperaldosteronism with hypokalemia, hypertension, and metabolic alkalosis. Liquorice is widely present in food and additives leading to a possible chronic intoxication. We describe an unusual case complicated by “torsades de pointe” and cardiac arrest following the chronic ingestion of an alcohol-free “pastis” beverage.
2. Case Report
A 45-year-old Caucasian man presented to our Emergency Department for asthenia, muscular weakness, polydipsia, and severe hypertension. His medical history revealed arterial hypertension and chronic alcohol consumption. He was currently treated with amlodipine, perindopril, and vitamin B supplementation. According to the relatives, the patient ingested daily a large amount of an alcohol-free “pastis” beverage in an attempt to reduce ethanol consumption. At physical examination, arterial blood pressure was 240/120 mmHg, heart rate 75/min cardiac and pulmonary auscultation was normal, and a mild lower limb edema was noted. Admission laboratory investigations are summarized in Table 1 and were remarkable for hypokalemia (1.65 mmol/L, Nl 3.5-5). Liver function tests were nearly normal with AST 42 UI/L (nl < 40), ALT 38 UI/L (nl < 41), alacaline phosphate 115 UI/L (nl 40-129), and gamma GT 102 UI/L (nl 10-71). Total bilirubin was 0.7 mg/dL (nl < 1.1). Fifteen minutes after hospital admissions, the patient experienced an episode of “torsades de pointe” rapidly evolving to cardiac arrest. Short (2 min) cardiopulmonary resuscitation included a 200 J asynchrone defibrillation and the administration of 1 mg of intravenous epinephrine. Postcardiac arrest arterial blood gas did not show any severe metabolic acidosis: pH 7.49, pCO2 48 mmhg (nl 35-45), PO2 75 mmHg (nl 75-104), and bicarbonate 32 mmol/L (nl 28-32).
Table 1.
Pertinent laboratory findings.
| Parameter | Value | Normal value |
|---|---|---|
| Plasma | ||
| Plasma sodium | 144 | 135-145 mmol/L |
| Plasma potassium | 1.65 | 3.5-5 mmol/L |
| Plasma chloride | 101 | 95-105 mmol/L |
| Plasma bicarbonate | 43 | 22-29 mmol/L |
| Plasma creatine kinase | 2270 | <210 UI/L |
| Plasma creatinine | 0.80 | 0.70-1.20 mg/dL |
| Plasma glucose | 12 | 3.3-5.5 mmol/L |
| Urine | ||
| Urinary sodium | 156 | mmol/24 h |
| Urinary potassium | 80 | mmol/24 h |
| Plasma renin activity | ||
| Supine | <0.04 | 0.04-0.52 pmol/L/s |
| Upright | 0.43 | 0.28-1.06 pmol/L/s |
| Supine plasma aldosterone | 106 | 22-477 pmol/L |
Postcardiac arrest electrocardiogram (ECG) revealed an irregular sinus rhythm associated with diffuse repolarization abnormalities; the QTc interval was 410 msec. The patient was transferred to the ICU for further monitoring and continuous intravenous potassium administration through a central venous line for 2 days. Oral supplementation was started on day 3, and the patient was discharged to the general ward. Hormonal workup revealed normal supine plasma aldosterone levels accompanied by very low plasma renin activity. The patient was discharged four days later. At 6-month follow-up, the patient had a normal blood pressure and kalaemia after having stopped liquorice-based beverages.
3. Discussion
Differential diagnosis of severe hypokalemia is very important as it mainly conditions the best therapeutics in ED. It includes decrease intake (starvation, clay ingestion), cell redistribution (metabolic alkalosis; treatments such as insulin, β-2-agonists, or α-2-antagonists; B12 vitamin or folic acid; parenteral nutrition…), and increased loss (mineralocorticoid excess including liquorice or Tobacco chewing, vomiting, renal tubular acidosis, and diabetic keto-acidosis). The patients' vitamin B was without B12. High levels of intravenous KCl were administered to him during in ED and ICU stay.
Hypokalemia, of chronic installation, can be very severe and associated with cramps, paresthesia, and heart rate disturbances such as ventricular fibrillation or “torsades de pointe.” Severe hypokalemia can also induce rhabdomyolysis as illustrated in our patient [1].
There was no liver failure as total bilirubin was only very lightly elevated and under the toxic range (0.7 mg/dL, nl < 1.1), but gamma-glutamyltransferase was elevated probably mainly due to chronic alcohol abuse.
Diagnosis can be made by low plasma aldosterone concentration, very low plasma renin levels, and disturbed urinary (Na/K) electrolytes [2]. Hypernatremia and metabolic alkalosis are inconstant [3].
Glycyrrhizin is a terpene extracted from the liquorice root. Natural liquorice juice contains 5 to 20% of glycyrrhizin. It is mainly used as a sweetener, its sweet power being 30 to 50 times greater than saccharose which explains its use in confectionery and beverages such as “pastis” as in the present observation.
Glycyrrhizin intoxication is mainly due to excessive and prolonged consumption of liquorice based pastry or cocktails. Chronic ingestion of 65-165 g liquorice confectionary can still cause symptoms, even if there is probably some interindividual susceptibility to glycyrrhetic acid. In 2005, the Food and Drug Administration (FDA) has implemented the World Health Organization recommendations of maximum glycyrrhizin concentrations in food and beverages [4]. They are illustrated in Table 2.
Table 2.
Limitations for the use of liquorice and its derivatives in foods.
| Food category | Maximum allowable levels of glycyrrhizin content in food (%) |
|---|---|
| Hard candy | 16 |
| Soft candy | 3.1 |
| Chewing gum | 1.1 |
| Vitamins or mineral dietary supplements | 0.5 |
| Nonalcoholic beverages | 0.15 |
| Herbs and seasonings | 0.15 |
| Plant protein products | 0.15 |
| Alcoholic beverages | 0.10 |
| All other foods except sugar substitutes | 0.10 |
| Baked goods | 0.05 |
Liquorice has a mineralocorticoid action through its glycyrrhetic derivative which inhibits type 2 11-β-hydroxysteroid dehydrogenase (Figure 1) and furthers renal transformation of cortisol to cortisone. Cortisol is free to bind to mineralocorticoid receptors mimicking hyperaldosteronism with severe hypokalemia, water, and salt retention [5].
Figure 1.
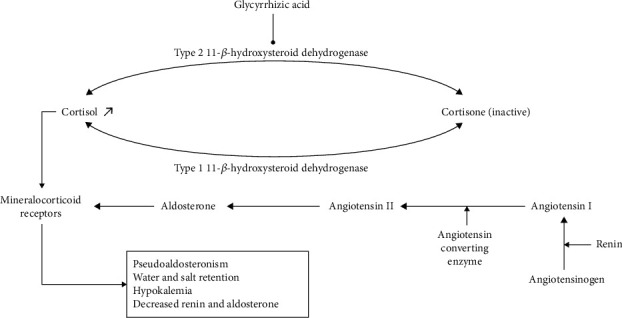
Both cortisol and aldosterone bind with equal affinity to mineralocorticoid receptors that are activated predominantly with aldosterone. Type 2 11-β-hydroxysteroid dehydrogenase (11-βHSD) converts cortisol to its inactive form, cortisone, and evokes corticosteroid specificity. By inhibitory effects of Glycyrrhiza glabra and glycyrrhizin on type 2 11-βHSD, the mineralocorticoid receptors are activated by cortisol, leading to accumulation of glucocorticoids with anti-inflammatory and mineralocorticoid properties, hypokalemia, and mineralocorticoid-related hypertension.
Intoxication is often suspected when arterial hypertension appears to be refractory to medical treatment in patients who are acknowledging liquorice consumption. Efficacy of angiotensin converting enzyme inhibitors is often limited in this setting by the too low plasma renin levels [5, 6].
Glycyrrhizin intoxication may lead in some patients to severe cardiac arrhythmias. In a review on nine patients with severe liquorice intoxication, six developed cardiac arrest [7]. The patients survived after successful resuscitation. Acute heart failure with pulmonary edema has also been described [8].
Evolution is usually favourable within 30 days of liquorice weaning. Mineralocorticosteroid effect can last 6 months because of long glycyrrhizin half-life and the time needed for normalization of renin-angiotensin-aldosterone pathway [4].
4. Conclusion
The association of severe hypokalemia and hypertension should draw the attention to a possible liquorice intoxication, in the absence of other evident causes of drug-induced hypokalemia. Thorough patient's history and the determination of renin and aldosterone plasma levels are the cornerstone of the diagnosis. Treatment includes potassium supplementation and spironolactone as well as stopping glycyrrhizin uptake [9, 10].
Conflicts of Interest
No competing interests exist.
References
- 1.Horwitz H., Jimenez-Solem E., Petersen L. W., Woeien V. A. Hypokalemia and rhabdomyolysis. Journal of Pharmacology and Pharmacotherapeutics. 2015;6(2):98–99. doi: 10.4103/0976-500X.155488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farese R. V., Biglieri E. G., Shackleton C. H. L., Irony I., Gomez-Fontes R. Licorice-induced hypermineralocorticoidism. The New England Journal of Medicine. 1991;325(17):1223–1227. doi: 10.1056/NEJM199110243251706. [DOI] [PubMed] [Google Scholar]
- 3.Card W. I., Strong J. A., Tompsett S. L., Mitchell W., Taylor N. R. W., Wilson J. M. G. Effects of liquorice and its derivatives on salt and water metabolism. The Lancet. 1953;261(6762):663–668. doi: 10.1016/s0140-6736(53)91801-7. [DOI] [PubMed] [Google Scholar]
- 4.Epstein M. T., Espiner E. A., Donald R. A., Hughes H. Effect of eating liquorice on the renin-angiotensin aldosterone axis in normal subjects. British Medical Journal. 1977;1(6059):488–490. doi: 10.1136/bmj.1.6059.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luchon L., Meyrier A., Paillard F. Hypokalemia without arterial hypertension by licorice poisoning. Néphrologie. 1993;14(4):177–181. [PubMed] [Google Scholar]
- 6.Brunin J. L., Bories P., Ampelas M., Mimran A., Michel H. Pseudohyperaldosteronism induced by alcohol-free aniseed aperitif in alcoholic cirrhotic patients. Gastroentérologie Clinique et Biologique. 1984;8(10):711–714. [PubMed] [Google Scholar]
- 7.Omar H. R., Komarova I., El-Ghonemi M., et al. Licorice abuse: time to send a warning message. Therapeutic Advances in Endocrinology and Metabolism. 2012;3(4):125–138. doi: 10.1177/2042018812454322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson H. J., Harrison F. S., Nicholson J. T. Cardiac abnormalities due to licorice intoxication. Pennsylvania Medicine. 1971;74(3):51–54. [PubMed] [Google Scholar]
- 9.Bannister B., Ginsburg R., Shneerson J. Cardiac arrest due to liquoriceinduced hypokalaemia. British Medical Journal. 1977;2(6089):738–739. doi: 10.1136/bmj.2.6089.738-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Food and Drug Administration limitations for the use of licorice and its derivatives in foods World Health Organization. US FAD; 2005. [Google Scholar]


