Abstract
Data envelopment analysis (DEA) is a powerful nonparametric engineering tool for estimating technical efficiency and production capacity of service units. Assuming an equally proportional change in the output/input ratio, we can estimate how many additional medical resource health service units would be required if the number of hospitalizations was expected to increase during an epidemic outbreak. This assessment proposes a two-step methodology for hospital beds vacancy and reallocation during the COVID-19 pandemic. The framework determines the production capacity of hospitals through data envelopment analysis and incorporates the complexity of needs in two categories for the reallocation of beds throughout the medical specialties. As a result, we have a set of inefficient healthcare units presenting less complex bed slacks to be reduced, that is, to be allocated for patients presenting with more severe conditions. The first results in this work, in collaboration with state and municipal administrations in Brazil, report 3772 beds feasible to be evacuated by 64% of the analyzed health units, of which more than 82% are moderate complexity evacuations. The proposed assessment and methodology can provide a direction for governments and policymakers to develop strategies based on a robust quantitative production capacity measure.
1. Introduction
The past months scourged the world with a novel coronavirus identified as the cause of a pneumonia outbreak first detected in Wuhan, province of Hubei, China. The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is responsible for a declared worldwide pandemic having more than a million confirmed cases and dozens of thousands of deaths, keeping a quick spread [1, 2]. The prompt virus outbreak causes a much bigger problem than lethality: a large number of infected patients require hospitalization and intensive care due to complications worsening the clinical condition. When several patients need such intensive care at the same time, the hospitals and other health service units with limited resources end up overloaded. As a result, the health systems collapse due to the unavailability of beds, ventilators, and technical resources for new hospital admissions, fatigue, and overloading health teams. Thus, hospital beds acquisition and evacuation are crucial to increase the response capacity to face the crisis [3].
Data envelopment analysis is a powerful nonparametric mathematical programming tool for the technical efficiency estimation of many service units in different economic activities, such as financial institutions and educational and health systems [4–7]. Hospitals are a wide source of efficiency assessments. Some of the most relevant results provide the potential for health improvement based on the expansion of results (e.g., hospitalizations, patient recoveries, performed surgeries, medical prescriptions, among others) or based on the contraction of resources (e.g., nurses, assistants, physicians, infected patients (nondiscretionary), beds, equipment, among others). Such prospects are possible through the envelopment of data, which estimates the industry's efficient production capacity.
This study introduces a novel application to provide an optimal number of hospital beds technically feasible to be evacuated and allocated for urgent hospitalizations through best practices, applicable during the COVID-19 crisis. The methodology is based on the Brazilian Healthy Complexity of Needs prioritization and can be extended to any health system with a similar or different classification of disease and medical specialties.
2. Literature
The increasing pressure on limited resources of health systems during the pandemic has highlighted the need for efficiency-based tools and methodologies to offer new combined perspectives on how to use the hospital's facilities, resources, and capabilities optimally. Ordu et al. [8, 9] develop an interesting decision support tool for modelling capacity constraints, and allocating hospitals' resources, combining discrete event simulation and forecasting techniques. The application in the accident and emergency department captures the outpatient demand for each specialty by age and first/followup referrals and the entire service pathway on different scenarios. Similar approaches aiming at providing increased operational efficiency and high-quality patient care are claimed to offer a considerable improvement in the hospitals' capacity response and average patient length of stay [10, 11]. A measure for the required number of optimal emergency beds, however, is a limitation acknowledged by the authors in these and other operations approach.
The nonparametric frontier estimations of data envelopment analysis can aid managers and policymakers in attaining such a prospect. The weight optimization based on pairwise evaluations scales the used resources and generated products of each service unit, providing a robust measure for the technical efficiency, which can be adapted for inverse output/input relations [12], exogenous or nondiscretionary resources [13–15], and time-series self-evaluations [16–18]. As a result, an estimation for the optimal production capacity for any size service unit is available for decision-making. In the case of hospitalizations, this optimal capacity measure can be translated into an efficient number of hospital beds, equipment, costs, or human resources required for the production of health using internments (hospitalizations) as a proxy for this product.
This instrument, besides offering a relative measure for hospitals' technical efficiency based on the maximum, yet feasible, production configuration, can determine peers of efficiency for benchmarking performance metrics and identifying opportunities for improvement and support resource allocation schemas based on production slacks. Many assessments of health efficiency follow this avenue, for instance, the recommendations of Kounetas and Papathanassopoulos [19] regarding the efficiency of Greek hospitals and Zare et al. [20] using a hybrid data envelopment analysis and game theory methodology for performance measurement in health service units. This interesting perspective of frontier estimations can provide the optimal number of resources to be (re-) allocated from inefficient units through best practices during epidemic crises.
The most common variables considered in modelling the production technology of health systems are the number of beds for hospitalizations, personal protective equipment (PPE) and other technical equipment, drugs, human capital (physicians, nurses, unlicensed assistants, and other staff), hospital infrastructure, costs of service (in many categories), and funding as inputs, and medical prescriptions, number of hospitalizations, outpatient procedures, inverse mortality rate, patients discharged, number of surgeries, and testing as outputs [6,19–26]. Nevertheless, different combinations of output/input can be used in assessments of hospitals' performance, depending on the problem statement and purpose. For instance, Hadad et al. [21] show an interesting nonconventional evaluation which resorts to life expectancy and infant survival rate as the parameters for the health product in two efficiency models, considering the physicians' density, inpatient bed density, expenditures, gross domestic product (GDP), and fruit and vegetable consumption, adding a different perspective in the efficiency assessment.
Most hospitals, in general, during the last weeks, and especially intensive care units (ICUs) and emergency departments (EDs) are constantly required to cope with a recurrent daily-based crisis ignited by the novel coronavirus outbreak. Gul & Guneri [27] and Gul et al. [28] discuss the importance of these sectors, dedicated to patients in need of urgent and commonly complex care, in a comprehensive review of literature and evaluation. In addition to the impact on these sectors, the pandemic has affected other specialties that are not directly related to the treatment of respiratory syndromes, where the resource becomes committed in order to prevent the collapse of an entire health system. In most assessments, different conditions and specialties are taken into consideration in several hospital departments, which brings a real contribution of hybrid models to the strategic planning of health service units.
The different specialties carried out by health service units are subject to different and varied heterogeneous factors that are connected to institutional arrangements, population characteristics, location, and socioeconomic or environmental determinants. The linear programming scales the differences through the output/input ratio of each health unit by comparing small units with a benchmark in the efficiency frontier presenting similar input-to-output configuration. Nevertheless, such heterogeneity has a considerable subjective value in the decision maker's perspective, which, despite the objective programming techniques, requires value judgments and preference elicitations on different decision criteria. Multiple criteria methodologies, for instance, Pergher & Vaccaro [29] outranking model based on the Electre Tri, Mendonça et al. [30], grey theory approach for risk assessments, and many others [31–36], can be relevant adapting on this prospect.
3. Methodology
The technical efficiency is traditionally understood as a ratio between the generated outputs and used inputs of a production process. Charnes et al. [37] and Banker et al. [38] through a mathematical linear dual formulation for multiple outputs/inputs configurations in the efficiency problem introduced the so-called data envelopment analysis (DEA). Today, this is the most common approach to assess the efficiency and productivity of many decision-making units (DMUs) in the number of surveys, applications, methodologies, and computational developments [39, 40]. The mathematical programming provides, among other results, the optimal amount of resources to save or products to increase so that an inefficient service unit becomes efficient.
The multidimensional production structure of hospitals and healthcare centres, however, requires a meticulous approach to define which resources need to be reduced in order to improve the health results. According to Lin & Kuo [41], different patient's complexity relies on different health service providers for different clinical specialties, which may jeopardize the slack reduction consistency in the technical efficiency analysis because potential performance improvements in hospitalizations by equally reducing the hospital beds, for instance, for all specialties, may be neither feasible nor coherent for each particular hospital context. An interesting solution is suggested by Ferreira and Marques [42]. According to this study, there is no need for complexity adjustment if one accounts for the operational environment surrounding the hospital. Conditional frontier analysis [15, 43] can add an interesting perspective by considering those environmental determinants in the frontier estimation.
An alternative avenue through a two-step methodology is proposed in this assessment. Estimations for the beds' evacuation is proposed by prioritizing the slack reduction according to the complexity of needs on the most common medical specialties to provide support for bed reallocations during an epidemic crisis. The first step consists of applying nonparametric frontier estimations for the full production capacity of the health service units (the maximum feasible production configuration for each hospital) based on hospital admissions as the main output and hospital beds as one of the many discretionary resources. Similar to many assessments of health systems efficiency, the number of beds is considered a proxy for hospital capital [31–36, 44]. That way, depending on the scale of operations and keeping everything else constant, the lower the usage of this resource, the higher the efficiency for the health service unit. Following similar resource optimization approaches [45, 46], the objective in this assessment is to provide an optimal number of beds to be evacuated and allocated for potential COVID-19 cases, instead of reduction.
For the second step, the optimal number of beds to be reallocated (based on best practices) are prioritized according to the complexity of needs for each medical specialty. The complexity of needs in the Brazilian Health System is the degree of complexity each health problem presents and the requirement for specialized knowledge. There are three categories: basic care, moderate complexity, and high complexity. Each category is defined in Table 1.
Table 1.
Complexity of needs categories.
| Basic care: the first level is characterized by a set of actions and practices using low-density technologies to solve health issues of greater frequency but low severity, including a list of simpler and cheaper procedures. The procedures in this category are capable of meeting most of the community's common health problems. |
|
|
| Moderate complexity: composed of actions and services aiming at meeting the main public health issues whose assistance in the clinical practice requires the availability of specialized professionals and the usage of technological resources for diagnostic, support, and treatment. |
|
|
| High complexity: common for more severe health issues; this category is characterized by a set of procedures involving high technology and high cost, aiming at providing access to highly specialized knowledge and qualified services. |
Hospitalizations have moderate (εlow) or high (εhigh) complexity of needs admissions. Consider a set of j=1,2,3,…, m health service units using xi|i=1,2,3,…, n hospital inputs to produce yr|r=1,2,3,…, s outputs. Consider “o” the service unit under evaluation and “ε,” the sum of both moderate and high complexity of needs hospitalizations, a proxy for the prioritization of beds evacuation. The optimal feasible contraction (evacuations) of high complexity hospitalization beds is as follows:
| (1) |
The optimal feasible contraction (evacuations) of moderate complexity beds is as follows:
| (2) |
where θ∗=min(θ)|(∑j=1mzjxji ≤ θxoi; ∑j=1mzjyjr ≥ yor; ∑j=1mzj=1&zj ≥ 0) is the efficiency score for the production technology under variable returns to scale [9, 14].
Equations (1) and (2) state that the optimal number for beds evacuation of high complexity admissions depends on the number of evacuated beds of moderate complexity. In other words, the optimal number for beds evacuation of high complexity hospitalizations is the remaining feasible contraction of beds after all moderate complexity admissions are evacuated. As an example, considering an efficiency score θ∗ = 0.8, the service unit may improve efficiency by producing the same result using (1–0.8) = 20% fewer resources. Considering 100 hospital beds allocated to admissions of both low and high complexity of needs as the discretionary input |εlow = 15 and εhigh = 85, the number of beds to be evacuated having moderate complexity is EvA− =εlow=15 beds and the number of beds to be evacuated having high complexity is the remaining EvA+ =ε(1 − θ) − εlow=20 − 15=5 beds.
Adding (1) and (2) into the DEA formulation, we can infer the optimal number for beds evacuation (EvA) based on the complexity of needs prioritization:
| (3) |
Full concepts and definitions concerning the complexity of needs assistance in the Brazilian Health System and a list with the related medical specialties are available in [47].
4. Data
In the first step of the evaluation, an input-oriented variable returns to scale model is conducted. Pernambuco's State Secretariat for Budgeting and Planning (SEPLAG) provided data regarding 373 from the 1136 health services units in the state. For this assessment, we have selected the 88 most important hospitals and healthcare centres based on the volume of hospitalizations. Due to data limitations, the number of doctors, surgeons, and general physicians is not considered in the analysis. For most medical specialties, ward rounds for inpatient care by physicians occur once a day or after a week, depending on the patient treatment plan or condition. This context let us assume that the inclusion or removal of these professionals may not shift the efficiency prospects compared to nurses and other health staff which are in direct contact with hospitalizations. The inputs are the number of nurses, nursing assistants, and licensed healthcare technicians and the cost of hospitalizations and the sum of hospital beds for three categories (specialties): medical clinics (comprehensive care for individuals aging over 12 years, in critical or semicritical conditions, and who do not need surgical treatment), surgical clinics (reserved for preoperative and postoperative care), and obstetrics. The output is the number of hospital internments (hospitalizations).
Table 2 and Figure 1 report the main descriptive statistics. Costs refer only to hospitalizations expenditure considering the three specialties. On average, R$ 8,073,821 (about US$ 1.5 million) is spent per health unit in hospitalizations for a typical year. Nursing assistants and nursing technicians are two professional categories working in outpatient sectors usually performing basic care planned by the nurse, such as administration of medicines, vaccines, dressings, performing patient hygiene, and sterilization of medical equipment. Due to the similarity of both categories, they were aggregated into one input named “assistants and technicians”.
Table 2.
Variables and descriptive statistics.
| Variables | Min. | 1st Qu. | Median | Mean | 3rd Qu. | Max. | Std. Dev. | |
|
| ||||||||
| Inputs | Assistants and technicians | 4.0 | 27.5 | 75.5 | 185.6 | 212.2 | 1409.0 | 271.54 |
| Nurses | 1.00 | 7.00 | 15.50 | 61.95 | 79.50 | 617.00 | 96.98 | |
| Hospital beds | 11.00 | 41.75 | 72.50 | 140.77 | 155.00 | 1075.00 | 181.54 | |
| Costs | 28388 | 225080 | 1804658 | 8073821 | 5137736 | 101663545 | 17038427 | |
|
| ||||||||
| Output | Hospitalizations | 74.0 | 527.8 | 2530.0 | 5252.0 | 7625.8 | 41678.0 | 7155.14 |
Figure 1.
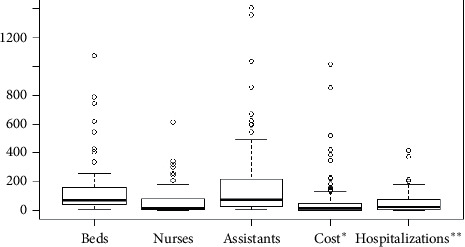
Boxplots visualization. ∗Hospitalization costs (expenditure) in 100000. ∗∗Number of hospitalizations in 100.
In general, the 88 most important health units in the state sums 16336 of those professionals, 5452 nurses, and 12388 beds, spent more than R$ 710 million (about US$ 132 million) in one year, and were responsible for 462175 hospitalizations and 5252 hospitalizations per unit on average. This means 0.07% (88 hospitals) were responsible for 27.02% of all hospitalizations in the state. Figure 1 illustrates the descriptive statistics in boxplots visualizations. Most of the outliers are public hospitals characterized by a high demand for health services.
5. Results and Discussion
Tables 3 and 4 summarize the main results. We have 26 hospitals working at full capacity in the state, serving as peers (benchmarks) for the remaining inefficient health units. These units are producing the maximum possible admissions a hospital can produce during a year given the current production technology, equipment, and human resource. It is worth mentioning that, for some of the ranked hospitals, the efficiency comes at the cost of quality due to the high demand for health services and overcrowded public hospitals. The total of 3772 beds are feasible to be evacuated and reallocated for new COVID-19 cases in one year considering the remaining inefficient units formalization of new service protocols, postponing surgeries and decreasing the patient length of stay in hospitals through best practices from the peers, of which 2883 are related to moderate hospitalizations and 889 high complex cases. Table 4 has the remaining hospitals and their potential for bed evacuation during the crisis.
Table 3.
Efficient hospitals at full capacity of admissions.
| Health service units | Beds | Peering |
|
| ||
| IMIP | 1075 | N/A |
| Hospital Da Restauração | 790 | 9 units |
| Hospital Otavio De Freitas | 620 | N/A |
| Hospital Getulio Vargas | 545 | 2 units |
| Hospital Barao De Lucena | 340 | 1 unit |
| Hospital Dom Malan | 259 | 8 units |
| Hospital Miguel Arraes | 173 | 4 units |
| Hospital Pelopidas Silveira | 170 | 3 units |
| HMR Dra Merces P. Cunha | 150 | 43 units |
| HM Santa Maria | 146 | 7 units |
| HR Fernando Bezerra | 98 | 3 units |
| CH Dr Jose E. De Moura | 91 | 15 units |
| HMC C. S. Bom Jesus | 70 | 18 units |
| IBVASF | 67 | 4 units |
| HI Palmira Sales | 62 | 19 units |
| Casa De Saúde São Jose | 59 | 2 units |
| PM Pr. Barros Lima | 57 | 7 units |
| Mat. Dr Luiz Leite | 42 | 4 units |
| Hospital Ermirio Coutinho | 41 | 11 units |
| HMM. Olimpio M G. Lins | 26 | 20 units |
| UM Kyola | 23 | 24 units |
| Hosp. Genezio F. Xavier | 22 | 1 unit |
| UM Dr Jose M. Monteiro | 16 | 15 units |
| UM Jose Dantas Filho | 15 | 2 units |
| HM Alice Figueira | 14 | 13 units |
| UM Maria Eliziaria Paes | 11 | 5 units |
Table 4.
Hospitals with potential for bed evacuations.
| DMU | Efficiency | Beds | Evacuations |
|
| |||
| 1 | 0.078 | 744 | 686 |
| 2 | 0.586 | 425 | 176 |
| 3 | 0.268 | 191 | 140 |
| 4 | 0.427 | 234 | 134 |
| 5 | 0.619 | 255 | 97 |
| 6 | 0.511 | 197 | 96 |
| 7 | 0.277 | 128 | 92 |
| 8 | 0.352 | 142 | 92 |
| 9 | 0.812 | 407 | 76 |
| 10 | 0.668 | 210 | 70 |
| 11 | 0.653 | 198 | 69 |
| 12 | 0.675 | 193 | 63 |
| 13 | 0.561 | 138 | 61 |
| 14 | 0.664 | 180 | 61 |
| 15 | 0.566 | 130 | 56 |
| 16 | 0.875 | 426 | 53 |
| 17 | 0.601 | 125 | 50 |
| 18 | 0.686 | 150 | 47 |
| 19 | 0.543 | 81 | 37 |
| 20 | 0.685 | 115 | 36 |
| 21 | 0.619 | 90 | 34 |
| 22 | 0.668 | 96 | 32 |
| 23 | 0.408 | 52 | 31 |
| 24 | 0.662 | 82 | 28 |
| 25 | 0.535 | 52 | 24 |
| 26 | 0.615 | 61 | 23 |
| 27 | 0.690 | 74 | 23 |
| 28 | 0.772 | 98 | 22 |
| 29 | 0.605 | 56 | 22 |
| 30 | 0.499 | 44 | 22 |
| 31 | 0.629 | 59 | 22 |
| 32 | 0.670 | 59 | 19 |
| 33 | 0.643 | 54 | 19 |
| 34 | 0.692 | 60 | 18 |
| 35 | 0.655 | 51 | 18 |
| 36 | 0.666 | 50 | 17 |
| 37 | 0.874 | 130 | 16 |
| 38 | 0.59 | 39 | 16 |
| 39 | 0.697 | 46 | 14 |
| 40 | 0.810 | 71 | 13 |
| 41 | 0.893 | 108 | 12 |
| 42 | 0.933 | 173 | 12 |
| 43 | 0.723 | 38 | 11 |
| 44 | 0.896 | 111 | 11 |
| 45 | 0.925 | 148 | 11 |
| 46 | 0.745 | 37 | 9 |
| 47 | 0.892 | 88 | 9 |
| 48 | 0.691 | 24 | 7 |
| 49 | 0.886 | 61 | 7 |
| 50 | 0.844 | 32 | 5 |
| 51 | 0.979 | 244 | 5 |
| 52 | 0.810 | 21 | 4 |
| 53 | 0.840 | 26 | 4 |
| 54 | 0.895 | 32 | 3 |
| 55 | 0.920 | 42 | 3 |
| 56 | 0.898 | 20 | 2 |
| 57 | 0.902 | 20 | 2 |
| 58 | 0.966 | 39 | 1 |
| 59 | 0.974 | 35 | 1 |
| 60 | 0.979 | 31 | 1 |
| 61 | 0.987 | 61 | 1 |
| 62 | 0.978 | 22 | 0 |
Figure 2 illustrates the overall production capacity with the efficiency frontier estimation by the envelopment of data under a variable returns to scale technology. In the visualization of Figure 2, the inputs in the x label are aggregated by simple summing with no specific weight for this aggregation. One should be alerted that a multiple-input to one output plot may not necessarily place the multiefficient health service units on the two-dimensional frontier, serving only illustration purposes. The traditional radial variable returns to scale model can be the most interesting option for the objective of incorporating the complexity of needs in a second step defining the feasible options for resource evacuation among the specialties. Because of the characteristic of data (beds available by medical specialties), we can prioritize the reduction of beds (and related resources uniformly) according to the complexity of their specialty. The points on the frontier represent the efficient hospitals reported in Table 3, which are benchmarks for best practices. The remaining inefficient units (under the frontier) in this illustration become efficient either by producing more hospitalizations with the same level of used inputs or by reducing the used inputs keeping hospitalizations at the same level or by a combination of both. In the input-oriented model of this assessment, efficiency is obtained by reducing (and reallocating) the number of beds keeping the same amount of hospitalization. This can be possible by applying some of the benchmark strategies for reducing the length of stay. In this representation, the most inefficient unit (the most distant point from the frontier) is one of the most important private hospitals in the state, having a considerable number of available beds for reallocation in a typical year.
Figure 2.
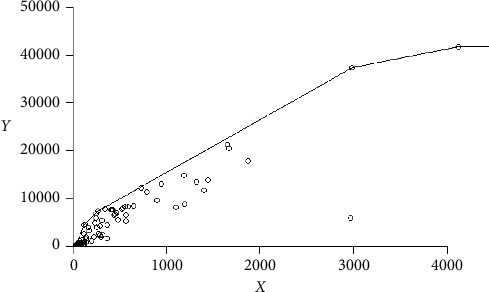
Efficiency frontier.
Table 5 reports the main prospects for the assessment. The evacuation of hospital beds are prioritized according to the complexity of needs for the many medical specialties each health service units operate. The monthly estimates are evacuation projections based on the efficient production capacity of hospitals, which can be used during the pandemic critical months. Twenty-three out of the 57 health service units with potential for bed evacuations do not require high complexity evacuations. Twenty out of the 57 require less than 50% high complexity evacuations. This methodology helps the policymaker concentrate attention on the hospital with the best potential and less critical services to evacuate and reallocate beds and related resources through best practices referred from the benchmarking peers of the evaluation.
Table 5.
Potential for bed evacuations according to the complexity of needs.
| DMU | Moderate complexity(%) | High complexity(%) | Monthlyestimate |
|
| |||
| 1 | 100 | 83 | 57 |
| 2 | 94 | 0 | 15 |
| 3 | 100 | 67 | 12 |
| 4 | 60 | 0 | 11 |
| 5 | 58 | 0 | 8 |
| 6 | 68 | 0 | 8 |
| 7 | 100 | 51 | 8 |
| 8 | 100 | 57 | 8 |
| 9 | 55 | 0 | 6 |
| 10 | 70 | 0 | 6 |
| 11 | 65 | 0 | 6 |
| 12 | 100 | 4 | 5 |
| 13 | 100 | 7 | 5 |
| 14 | 100 | 31 | 5 |
| 15 | 0 | 43 | 5 |
| 16 | 39 | 0 | 4 |
| 17 | 100 | 26 | 4 |
| 18 | 51 | 0 | 4 |
| 19 | 100 | 28 | 3 |
| 20 | 100 | 18 | 3 |
| 21 | 100 | 28 | 3 |
| 22 | 100 | 12 | 3 |
| 23 | 100 | 51 | 3 |
| 24 | 100 | 32 | 2 |
| 25 | 100 | 27 | 2 |
| 26 | 100 | 29 | 2 |
| 27 | 100 | 12 | 2 |
| 28 | 86 | 0 | 2 |
| 29 | 100 | 31 | 2 |
| 30 | 100 | 0 | 2 |
| 31 | 100 | 24 | 2 |
| 32 | 100 | 19 | 2 |
| 33 | 100 | 17 | 2 |
| 34 | 100 | 47 | 2 |
| 35 | 100 | 18 | 1 |
| 36 | 100 | 12 | 1 |
| 37 | 23 | 0 | 1 |
| 38 | 100 | 30 | 1 |
| 39 | 100 | 24 | 1 |
| 40 | 43 | 0 | 1 |
| 41 | 2 | 0 | 1 |
| 42 | 9 | 0 | 1 |
| 43 | 16 | 0 | 1 |
| 44 | 16 | 0 | 1 |
| 45 | 100 | 3 | 1 |
| 46 | 100 | 1 | 1 |
| 47 | 49 | 0 | 1 |
| 48 | 100 | 5 | 1 |
| 49 | 100 | 3 | 1 |
| 50 | 0 | 10 | 1 |
| 51 | 21 | 0 | 1 |
| 52 | 68 | 0 | 1 |
| 53 | 24 | 0 | 1 |
| 54 | 9 | 0 | 1 |
| 55 | 26 | 0 | 1 |
| 56 | 38 | 0 | 1 |
| 57 | 16 | 0 | 1 |
| 58 | 88 | 0 | 1 |
| 59 | 100 | 8 | 1 |
| 60 | 78 | 0 | 1 |
| 61 | 100 | 17 | 1 |
| 62 | 53 | 0 | 1 |
6. Conclusions
The assessment provided a framework for the application of nonparametric frontier methods of the DEA family to estimate the technically feasible capacity of hospitalizations, which, combined with prioritization methodologies for medical specialties such as the cmplexity of needs in Brazil, can disclose valuable support for policymakers to prevent an eventual collapse of health systems during the COVID-19 epidemic crisis. The methodology can be adapted to other localities, or decision criteria, providing a systematic approach for resource allocation through hospitals during the pandemic.
A valuable extension for the assessment of the health service units technical efficiency is the frontier estimation based on time-series production data instead of pairwise comparisons. Due to the many particular differences regarding the production technology of hospitals, an approach based on internal rather than industrial capacity can be more deductive and coherent.
Another interesting value can be added by the definition of beds' evacuation based on multiple decision criteria besides the complexity of needs. Important clinical aspects of hospital internments such as the gravity of diseases, flexibility for resource transfer among the medical specialties, and substitution potential can orientate decisions of managers and policymakers closer to each health unit reality. In addition, the usage of fuzzy data for the assessment of network system such as a hospital can aid valuable support [48]. This analysis can provide a direction for public administrations to perform some of their strategies based on an objective quantitative production capacity measure and support subjective decision-making with the inclusion of such aspects.
An extension of the current application investigating the efficiency evolution and the hospitalization efficacy against COVID-19 can be very useful for policymakers. A time-series evaluation, as suggested by Nepomuceno et al. [49], can be performed using time-series data regarding the period before and after the implementation of beds reallocation schema based on each specialty complexity of needs. The first results of this assessment were disclosed to state authorities, hoping to contribute to how to mitigate the drastic effects of the current crisis in the available resources.
Acknowledgments
The authors acknowledge Pernambuco's State Secretariat for Budgeting and Planning (SEPLAG) for the provision of data and valuable suggestions. The authors acknowledge the funding support from the Brazilian National Council for Scientific and Technological Development (CNPq).
Data Availability
Readers can access the data related to the findings of this study upon request.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. The Lancet. 2020;395(10226):764–766. doi: 10.1016/s0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coronavirus COVID-19 global cases by the center for systems science and engineering (CSSE) at johns hopkins coronavirus resource center, https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf, 2020.
- 3.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? The Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berger A. N., Humphrey D. B. Efficiency of financial institutions: international survey and directions for future research. European Journal of Operational Research. 1997;98(2):175–212. doi: 10.1016/s0377-2217(96)00342-6. [DOI] [Google Scholar]
- 5.Nepomuceno T. C. C., Daraio C., Costa A. P. C. S. Combining multi-criteria and directional distances to decompose non-compensatory measures of sustainable banking efficiency. Applied Economics Letters. 2020;27(4):329–334. doi: 10.1080/13504851.2019.1616051. [DOI] [Google Scholar]
- 6.Ibrahim M. D., Daneshvar S. Efficiency analysis of healthcare system in Lebanon using modified data envelopment analysis. Journal of Healthcare Engineering. 2018;2018 doi: 10.1155/2018/2060138.2060138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banker R. D., Conrad R. F., Strauss R. P. A comparative application of data envelopment analysis and translog methods: an illustrative study of hospital production. Management Science. 1986;32(1):30–44. doi: 10.1287/mnsc.32.1.30. [DOI] [Google Scholar]
- 8.Ordu M., Demir E., Tofallis C., Gunal M. A novel healthcare resource allocation decision support tool: a forecasting-simulation-optimization approach. Journal of the Operational Research Society. 2020 doi: 10.1080/01605682.2019.1700186. [DOI] [Google Scholar]
- 9.Ordu M., Demir E., Tofallis C. A decision support system for demand and capacity modelling of an accident and emergency department. Health Systems. 2020;9(1):31–56. doi: 10.1080/20476965.2018.1561161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oh C., Novotny A. M., Carter P. L., Ready R. K., Campbell D. D., Leckie M. C. Use of a simulation-based decision support tool to improve emergency department throughput. Operations Research for Health Care. 2016;9:29–39. doi: 10.1016/j.orhc.2016.03.002. [DOI] [Google Scholar]
- 11.Demir E., Southern D., Verner A., Amoaku W. A simulation tool for better management of retinal services. BMC Health Services Research. 2018;18(1):p. 759. doi: 10.1186/s12913-018-3560-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nepomuceno K. T. C., Nepomuceno T. C. C., Sadok D. Measuring the internet technical efficiency: a ranking for the world wide web pages. IEEE Latin America Transactions. 2020;18(6):1119–1125. doi: 10.1109/TLA.2020.9099750. [DOI] [Google Scholar]
- 13.Saquetto T. C., Araujo C. A. Efficiency evaluation of private hospitals in Brazil: a two-stage analysis. Revista De Administração Mackenzie. 2019;20(5) doi: 10.1590/1678-6971/eramr190183. [DOI] [Google Scholar]
- 14.Seljak J., Kvas A. Three-stage data envelopment analysis as a tool for nurse leader performance appraisals: case study. SAGE Open. 2015;5(1) doi: 10.1177/2158244015577666. [DOI] [Google Scholar]
- 15.Nepomuceno T. C. C., Santiago K. T. M., Daraio C., Costa A. P. C. S. Exogenous crimes and the assessment of public safety efficiency and effectiveness. Forthcoming in Annals of Operations Research. 2020 [Google Scholar]
- 16.Nepomuceno T. C. C., Costa A. P. C. Resource allocation with time series DEA applied to Brazilian federal saving banks. Economics Bulletin. 2019;39(2):1384–1392. [Google Scholar]
- 17.Nepomuceno T. C. C., De Carvalho V. D. H., Costa A. P. C. S. Time-series directional efficiency for knowledge benchmarking in service organizations. Proceedings of the World Conference on Information Systems and Technologies; April 2020; Budva, Montenegro. Springer; pp. 333–339. [DOI] [Google Scholar]
- 18.Baldemor M. Time series and data envelopment analysis on the performance efficiency of Dmmmsu-South La union campus. International Journal of Scientific Engineering and Research. 2018;4(4):5–10. [Google Scholar]
- 19.Kounetas K., Papathanassopoulos F. How efficient are Greek hospitals? a case study using a double bootstrap DEA approach. European Journal of Health Economics. 2013;14(6):979–994. doi: 10.1007/s10198-012-0446-z. [DOI] [PubMed] [Google Scholar]
- 20.Zare H., Tavana M., Mardani A., Masoudian S., Kamali Saraji M. A hybrid data envelopment analysis and game theory model for performance measurement in healthcare. Health Care Management Science. 2019;22(3):475–488. doi: 10.1007/s10729-018-9456-4. [DOI] [PubMed] [Google Scholar]
- 21.Hadad S., Hadad Y., Simon-Tuval T. Determinants of healthcare system’s efficiency in OECD countries. European Journal of Health Economics. 2013;14(2):253–265. doi: 10.1007/s10198-011-0366-3. [DOI] [PubMed] [Google Scholar]
- 22.Kaveski S., Degenhart L., Vogt M., Hein N. Efficiency of the service of the municipalities associated with SUS in mato grosso do sul southwest. Administração Pública e Gestão Social. 2015;7(4):197–205. doi: 10.21118/apgs.v7i4.760. [DOI] [Google Scholar]
- 23.Bahrami M. A., Rafiei S., Abedi M., Askari R. Data envelopment analysis for estimating efficiency of intensive care units: a case study in Iran. International Journal of Health Care Quality Assurance. 2018;31(4):276–282. doi: 10.1108/ijhcqa-12-2016-0181. [DOI] [PubMed] [Google Scholar]
- 24.Kocisova K., Gavurova B., Behun M. The importance of implementing environmental variables in the process of assessment of healthcare efficiency through DEA (1) Ekonomicky Casopis. 2019;67(4):367–387. [Google Scholar]
- 25.Li C., Sun M., Shen J. J., Cochran C. R., Li X., Hao M. Evaluation on the efficiencies of county-level Units for Disease Control and Prevention in China: results from a national survey. Tropical Medicine & International Health. 2016;21(9):1106–1114. doi: 10.1111/tmi.12753. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez-De Julian S., Trillez-Araujo S., Uso-Talamantes R., Caballer Tarazona V., Saurí-Ferrer M. I., Trillo J. L. Efficiency assessment in primary healthcare units of a health district. Value in Health. 2018;21(3):p. S318. doi: 10.1016/j.jval.2018.09.1899. [DOI] [Google Scholar]
- 27.Gul M., Guneri A. F. A comprehensive review of emergency department simulation applications for normal and disaster conditions. Computers and Industrial Engineering. 2015;83:327–344. doi: 10.1016/j.cie.2015.02.018. [DOI] [Google Scholar]
- 28.Gul M., Fuat Guneri A., Gunal M. M. Emergency department network under disaster conditions: the case of possible major Istanbul earthquake. Journal of the Operational Research Society. 2019;71(5):733–747. doi: 10.1080/01605682.2019.1582588. [DOI] [Google Scholar]
- 29.Pergher I., Vaccaro G. L. R. Work in process level definition: a method based on computer simulation and electre tri. Production. 2014;24(3):536–547. doi: 10.1590/S0103-65132013005000067. [DOI] [Google Scholar]
- 30.Mendonça Silva M., Poleto T., Camara e Silva L., Henriques De Gusmao A. P., Cabral Seixas Costa A. P. A grey theory based approach to big data risk management using FMEA. Mathematical Problems in Engineering. 2016;2016:15. doi: 10.1155/2016/9175418.9175418 [DOI] [Google Scholar]
- 31.Cavalcante C. A. V., Alencar M. H., Lopes R. S. Multicriteria model to support maintenance planning in residential complexes under warranty. Journal of Construction Engineering and Management. 2017;143(4) doi: 10.1061/(asce)co.1943-7862.0001250.04016110 [DOI] [Google Scholar]
- 32.Silva M. M., Costa A. P. C. S., De Gusmão A. P. H. Continuous cooperation: a proposal using a fuzzy multicriteria sorting method. International Journal of Production Economics. 2014;151:67–75. doi: 10.1016/j.ijpe.2014.01.022. [DOI] [Google Scholar]
- 33.Silva L. C. E., Costa A. P. C. S. IT project investments: an analysis based on a sort and rank problem. International Journal of Information Technology & Decision Making. 2014;13(4):699–719. doi: 10.1142/s0219622014500655. [DOI] [Google Scholar]
- 34.Fontana M. E., Morais D. C. Decision model to control water losses in distribution networks. Production. 2016;26(4):688–697. doi: 10.1590/0103-6513.201815. [DOI] [Google Scholar]
- 35.Da Silva J. G., Lopes R. S. An integrated framework for mode failure analysis, delay time model and multi-criteria decision-making for determination of inspection intervals in complex systems. Journal of Loss Prevention in the Process Industries. 2018;51:17–28. doi: 10.1016/j.jlp.2017.10.013. [DOI] [Google Scholar]
- 36.Nepomuceno T. C. C., De Moura J. A., Costa A. P. C. S. Modeling sequential bargains and personalities in democratic deliberation systems. Kybernetes. 2018;47(10):1906–1923. doi: 10.1108/K-03-2018-0144. [DOI] [Google Scholar]
- 37.Charnes A., Cooper W. W., Rhodes E. Measuring the efficiency of decision making units. European Journal of Operational Research. 1978;2(6):429–444. doi: 10.1016/0377-2217(78)90138-8. [DOI] [Google Scholar]
- 38.Banker R. D., Charnes A., Cooper W. W. Some models for estimating technical and scale inefficiencies in data envelopment analysis. Management Science. 1984;30(9):1078–1092. doi: 10.1287/mnsc.30.9.1078. [DOI] [Google Scholar]
- 39.Daraio C., Kerstens K. H., Nepomuceno T. C. C., Sickles R. Productivity and efficiency analysis software: an exploratory bibliographical survey of the options. Journal of Economic Surveys. 2019;33(1):85–100. doi: 10.1111/joes.12270. [DOI] [Google Scholar]
- 40.Daraio C., Kerstens K., Nepomuceno T., Sickles R. C. Empirical surveys of frontier applications: a meta‐review. International Transactions in Operational Research. 2020;27(2):709–738. doi: 10.1111/itor.12649. [DOI] [Google Scholar]
- 41.Lin Y., Kuo R. Patient complexity and services provided of local clinics in Taiwan: how many of them are “primary care” providers? Value in Health. 2018;21:S49–S50. doi: 10.1016/j.jval.2018.07.331. [DOI] [Google Scholar]
- 42.Ferreira D., Marques R. Should inpatients be adjusted by their complexity and severity for efficiency assessment? evidence from Portugal. Health Care Management Science. 2016;19(1):43–57. doi: 10.1007/s10729-014-9286-y. [DOI] [PubMed] [Google Scholar]
- 43.Daraio C., Simar L. Conditional nonparametric frontier models for convex and nonconvex technologies: a unifying approach. Journal of Productivity Analysis. 2007;28(1-2):13–32. doi: 10.1007/s11123-007-0049-3. [DOI] [Google Scholar]
- 44.Omrani H., Shafaat K., Emrouznejad A. An integrated fuzzy clustering cooperative game data envelopment analysis model with application in hospital efficiency. Expert Systems with Applications. 2018;114:615–628. doi: 10.1016/j.eswa.2018.07.074. [DOI] [Google Scholar]
- 45.Ferreira D., Nunes A., Marques R. Doctors, nurses, and the optimal scale size in the Portuguese public hospitals. Health Policy. 2018;122(10):1093–1100. doi: 10.1016/j.healthpol.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 46.Ferreira D., Nunes A., Marques R. Economies of scope in the health sector: the case of Portuguese hospitals. European Journal of Operational Research. 2018;266(2):716–735. doi: 10.1016/j.ejor.2017.09.044. [DOI] [Google Scholar]
- 47.Conselho Nacional De Secretários De Saúde (Brasil) 2007. Assistência de Média e Alta Complexidade no SUS. Conselho Nacional de Secretários de Saúde, Brasília. http://bvsms.saude.gov.br/bvs/publicacoes/colec_progestores_livro9.pdf.
- 48.Ameri Z., Sana S. S., Sheikh R. Self-assessment of parallel network systems with intuitionistic fuzzy data: a case study. Soft Computing. 2019;23(2):12821–12832. doi: 10.1007/s00500-019-03835-5. [DOI] [Google Scholar]
- 49.Nepomuceno T. C. C., De Moura J. A., E Silva L. C., Costa A. P. C. S. Alcohol and violent behavior among football spectators: an empirical assessment of Brazilian’s criminalization. International Journal of Law, Crime and Justice. 2017;51:34–44. doi: 10.1016/j.ijlcj.2017.05.001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Readers can access the data related to the findings of this study upon request.


