Abstract
Several techniques have been described for bone block augmentation as a treatment for posterior shoulder instability, including intra-articular distal tibial allograft and extra-articular iliac crest autograft. Although indications are not yet well defined, these bone augmentation procedures are considered in patients with glenoid bone loss, increased glenoid retroversion, previous failed posterior soft-tissue repair, and insufficient posterior capsulolabral tissue. In patients with posterior glenoid bone loss, the senior author (P.J.M.) recommends intra-articular glenoid reconstruction with a fresh distal tibial osteoarticular allograft. In patients with insufficient posterior capsulolabral tissue, the senior author prefers an extra-articular iliac crest autograft to buttress the posterior soft-tissue restraints. This technique guide outlines extra-articular iliac crest autograft treatment for recurrent posterior shoulder instability in patients with insufficient posterior soft tissues due to prior failed surgery. After an open capsulolabral repair is performed using suture anchors, the bone block is placed extra-articularly on the posterior glenoid neck.
Posterior shoulder instability accounts for 2% to 5% of patients with shoulder instability.1,2 Symptoms typically develop insidiously, with pain being the most common complaint.3 This pathology frequently occurs in people who are subjected to recurrent posteriorly directed forces of the glenohumeral joint, such as football players or weight lifters.4 Arthroscopic posterior capsulolabral repair with suture anchors has become the gold standard in most patients without significant bone loss.5,6 Dekker et al.7 recently characterized bone loss in the setting of posterior instability, concluding that bony defects are associated with specific changes in concavity, slope, and version and are commonly oriented in the posteroinferior direction.8 Critical bone loss or pathologic glenoid version has not yet been defined in posterior shoulder instability.9,10 When posterior instability is associated with failure of soft-tissue reconstruction and/or glenoid bone loss is significant, bone block augmentation should be considered11 (Table 1).
Table 1.
Indications for Posterior Glenoid Augmentation With Iliac Crest Autograft
| Poor-quality posterior capsular tissue |
| Significant posterior laxity |
| Failed previous soft-tissue stabilization with recurrent instability |
| Posterior instability with glenoid dysplasia |
| Traumatic posterior bony Bankart lesion (<15%) |
| Large reverse Hill-Sachs lesion |
Although promising early outcomes have been reported with posterior bone block augmentation,12,13 there remains a paucity of literature regarding appropriate indications and long-term follow-up. Traditionally, posterior bone block augmentation has been performed open; however, recently, various arthroscopic techniques have been described. Open bone block augmentation has shown reliable and successful patient-reported outcomes in both short- and mid-term studies.14, 15, 16 Initial revision rates for the arthroscopic technique as high as 36.8% have been reported; these have been attributed to a steep learning curve.12 Furthermore, the open approach for bone block augmentation in the treatment of anterior instability has been shown to achieve significantly lower graft impaction angles, which may be associated with more favorable force-dependent bony remodeling and better central positioning of the humeral head within the glenoid cavity.17
The goal of this Technical Note is to describe the principal author's (P.J.M.) technique for treating posterior shoulder instability in the setting of failed soft-tissue stabilization, poor-quality posterior capsulolabral tissue, and hyperlaxity with extra-articular iliac crest autograft posterior glenoid bony augmentation.
Preoperative Planning
A complete history and physical examination are essential. The Kim and jerk tests are helpful physical examination maneuvers in the evaluation of posterior instability. The Kim test involves the patient sitting with the examiner applying an axial force through the patient's elbow with the arm in 90° of abduction. The patient's arm is then elevated diagonally upward while a downward and posteriorly directed force is applied to the upper arm. Pain indicates a positive test finding. The jerk test is also performed in the sitting position with the same starting arm position and axial load, with the arm in slightly more internal rotation. Then, the arm is moved across the body in the horizontal plane. A positive result occurs when the humeral head subluxates posteriorly over the glenoid and a clunk is felt; then, when the arm is brought back into abduction, a “jerk” occurs when the humerus reduces. Imaging studies are also essential, including radiographs (4 views—anteroposterior in external and internal rotation, axillary, and scapular Y-view) and magnetic resonance imaging (MRI), to assess labral pathology, capsular injury and laxity, glenoid version, glenoid bone loss, and impaction fractures (i.e. reverse Hill-Sachs lesions), as well as other concomitant pathology. Although not yet well defined in the literature, typical indications for extra-articular posterior glenoid augmentation are recurrent posterior shoulder instability in the setting of prior failed soft-tissue stabilization with poor-quality posterior capsulolabral tissue and significant posterior laxity without glenoid bone loss or a large reverse Hill-Sachs lesions (Table 1). The senior author's indication for extra-articular posterior glenoid augmentation is recurrent posterior instability with less than 15% bone loss and insufficient posterior soft tissues. When intra-articular bone loss is present, the senior author prefers to perform an intra-articular glenoid reconstruction using a fresh distal tibial osteoarticular allograft. When extreme retroversion is encountered, a corrective glenoid osteotomy is preferred. This article will highlight the technique for glenoid reconstruction using an extra-articular iliac crest autograft posterior glenoid augmentation.
Surgical Technique
Diagnostic Arthroscopy
The patient is positioned in the lateral decubitus position to allow access to both the iliac crest and posterior shoulder (Fig 1). A thorough dynamic examination is then performed with the patient under anesthesia. The complete surgical technique is depicted in Video 1. First, a standard posterior viewing portal is created 2 cm inferior and 1 cm medial to the posterolateral acromial border. Under direct visualization, a standard anterior portal is created in the rotator interval. A diagnostic arthroscopy is then performed to evaluate for concomitant pathology, including labral tears, capsular injury, posterior glenoid bone loss, and articular cartilage disruption (e.g. reverse Hill-Sachs lesion).
Fig 1.

The patient is positioned in the lateral decubitus position with the operative shoulder (left shoulder) and ipsilateral iliac crest prepared and draped. The operative extremity is secured in an arm holder (arrow).
Posterior Glenoid Rim Exposure and Preparation
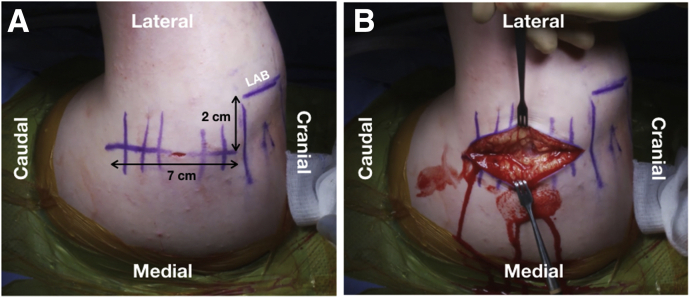
A posterior approach to the glenohumeral joint is performed. A vertical, posteriorly based incision is made at the inferior acromial margin, 2 cm medial to the lateral edge, and is extended distally approximately 7 cm (Fig 2). Dissection is carried down to the deltoid fascia, and the fascia is split with care for later closure. By use of electrocautery, the deltoid muscle is split parallel to its fibers. Reflection of the deltoid exposes the teres minor and infraspinatus fascia deep to the muscle. The interval between the teres minor and infraspinatus is then developed, using a combination of blunt dissection and electrocautery, to gain exposure to the posterior glenohumeral capsule, which is commonly of poor quality or patulous.
Fig 2.
Left shoulder in lateral decubitus position. Skin landmarks and incisions are marked to gain access to the posterior glenohumeral joint. (A) A vertical, posterior mark is made at the inferior margin of the acromion, 2 cm medial to the lateral edge, and extended distally approximately 7 cm. (B) The skin incision is made and is carried down through the subcutaneous tissue. (LAB, lateral acromial border.)
A posterior capsular incision is performed parallel to the glenoid rim and labrum, leaving a cuff for later repair. Dissection can be extended both superiorly and inferiorly to gain further exposure. The medial limb of the capsule is then tagged using a No. 2 suture, and a narrow Fukuda retractor is placed in the joint to retract the humeral head. A Cobb elevator is used to elevate the capsule off the glenoid neck to allow appropriate visualization. In addition to a poor-quality or patulous capsule, the posterior labrum is often deficient between the 6- and 10-o'clock positions.
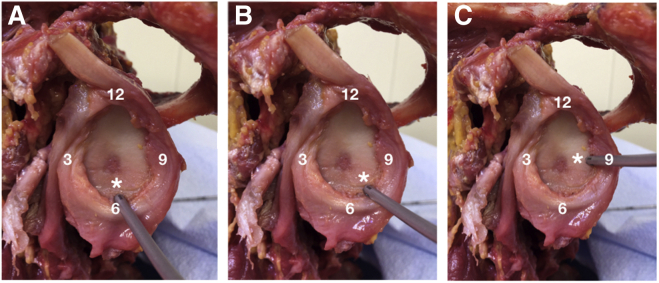
If the labrum is of sufficient quality for repair, we place 1.8-mm all-suture anchors (FiberTak; Arthrex, Naples, FL) on the glenoid. In this case, 3 anchors were placed, one each at the 6-o'clock position, 7:30 clock-face position, and 9-o'clock position (Fig 3). The labral repair is facilitated by passing the sutures from the anchors around the capsulolabral complex with a free needle and then tying them in a horizontal mattress fashion. The free limbs are kept for later capsular closure and imbrication.
Fig 3.
Dissected cadaveric shoulder showing proper placement of 1.8-mm knotless all-suture anchors (3 anchors) used to complete the soft-tissue repair of the posterior labrum on the glenoid: drill guide placed at 6-o'clock position (asterisk) (A), 7:30 clock-face position (asterisk) (B), and 9-o'clock position (asterisk) (C).
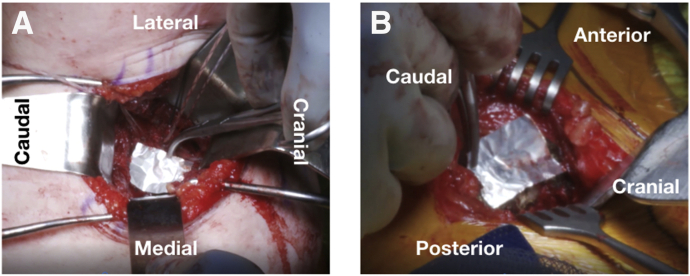
A key elevator and a 5.0-mm bone cutting burr are used to prepare the posterior glenoid for placement of the posterior extra-articular bone block. The glenoid is carefully decorticated to a bleeding bed to facilitate bone-to-bone healing with the tricortical graft. Care must be taken to avoid over-resection. A ruler is used to determine the size of the glenoid defect, and a template (e.g. aluminum foil from suture packaging) is created to facilitate appropriate sizing (Fig 4A).
Fig 4.
(A) Left shoulder in lateral decubitus position. A template (aluminum foil from suture packaging) is used to determine the size of the glenoid defect and the appropriate size of the iliac graft to harvest. (B) Left iliac crest in lateral decubitus position. The aluminum foil template is used to size the iliac crest graft before harvest.
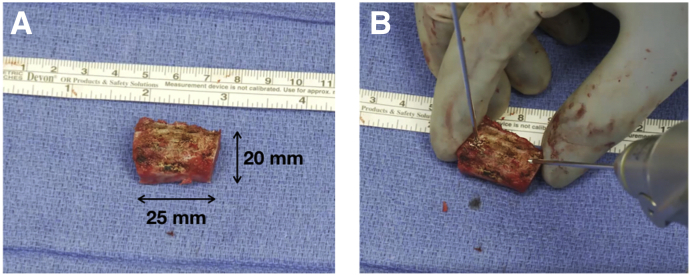
Tricortical Iliac Crest Bone Graft Harvest
The tricortical iliac crest autograft is harvested from the ipsilateral anterior iliac crest using the technique described by Warner et al.18 Appropriate sizing of the graft is determined using the previously created template (Fig 4B). On the basis of the previous measurements, a 25 × 20–mm graft was harvested in this case (Fig 5A). The graft is then appropriately contoured with a rongeur to allow proper fit on the glenoid neck. Two threaded K-wires are placed at the superior and inferior aspects of the graft to facilitate handling and positioning (Fig 5B).
Fig 5.
(A) A 25 × 20–mm iliac tricortical autograft is harvested. (B) Two threaded K-wires are placed into the superior and inferior aspects of the graft to allow easier handling and positioning.
Iliac Crest Bone Graft Posterior Bone Block Fixation
The graft is positioned flush with the glenoid and held manually in place (Fig 6A). Two 3.5-mm drill holes are placed in the graft; then the graft is positioned in the appropriate location on the glenoid. The glenoid is drilled with a 2.5-mm drill, and two 3.5-mm fully threaded stainless-steel cortical screws are placed through the graft approximately 1 cm apart, securing the graft by using a lag by application technique (Fig 6 B and 6 C). It is important to make sure that the graft is positioned flush to 1 mm lateral to the native glenoid and that there is good apposition between the posterior glenoid neck and the free tricortical autograft bone.
Fig 6.
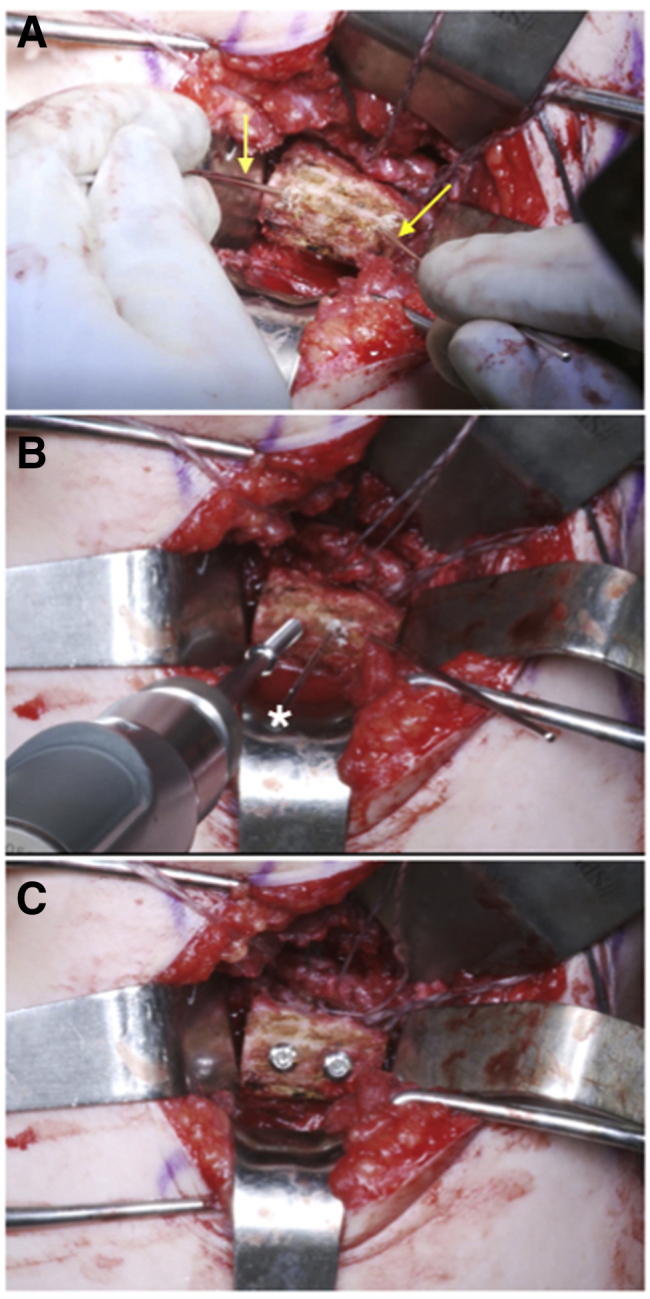
Left shoulder in lateral decubitus position. (A) The tricortical iliac crest autograft is positioned flush with the glenoid and held manually in place with 2 K-wires (arrows). (B) A 3.5-mm fully threaded stainless-steel cortical screw is inserted through the inferior 3.5-mm drill hole. A preliminary K-wire (asterisk) is placed through the center of the graft to minimize rotation during graft fixation. (C) The graft is fixated in the appropriate position flush to 1 mm lateral to the native glenoid with two 3.5-mm stainless-steel screws.
Capsulorrhaphy With Capsular Closure
Sutures from the previously placed anchors in the native glenoid are used to advance the capsule in a pants-over-vest manner, making the graft extra-articular and allowing the capsule to be plicated. The capsule is then reinforced with interrupted figure-of-8 No. 2 sutures.
Posterior Closure
The wound is copiously irrigated, and the fascia between the infraspinatus and teres minor is closed. The deltoid fascia and skin are then closed in a layered fashion. Table 2 summarizes the key procedural steps.
Table 2.
Key Procedural Steps
| Patient placement in lateral decubitus position |
| Diagnostic arthroscopy |
| Open, posterior approach to shoulder with vertical incision |
| Split of deltoid muscle parallel to its fibers using electrocautery |
| Development of interval between infraspinatus and teres minor using electrocautery |
| Posterior capsulotomy parallel to glenoid rim, preserving labral attachment to glenoid |
| Posterior labral repair using 1.8-mm knotted all-suture anchors |
| Extra-articular glenoid preparation using key elevator and burr |
| Sizing of bone graft using suture packaging foil template |
| Harvest of tricortical iliac crest autograft |
| Insertion of K-wires for handling and placement on glenoid neck |
| Fixation of graft flush with glenoid articular surface using two 3.5-mm screws |
| Capsulorrhaphy in pants-over-vest manner to make autograft extra-articular |
| Capsular reinforcement with figure-of-8 sutures |
| Layered closure |
Postoperative Rehabilitation
The operative extremity is protected in a sling for 6 weeks. Postoperative rehabilitation focuses on early gradual passive range of motion without excessive loading of the posterior capsule. At 6 weeks, if radiographs show proper graft and screw placement, active motion is permitted (Fig 7). Strengthening commences at 8 to 10 weeks postoperatively. Full unrestricted activity is typically permitted at 6 months after surgery, after full strength and motion have been restored and radiographic findings remain satisfactory. Pearls and pitfalls of open posterior glenoid augmentation with iliac crest autograft are shown Table 3.
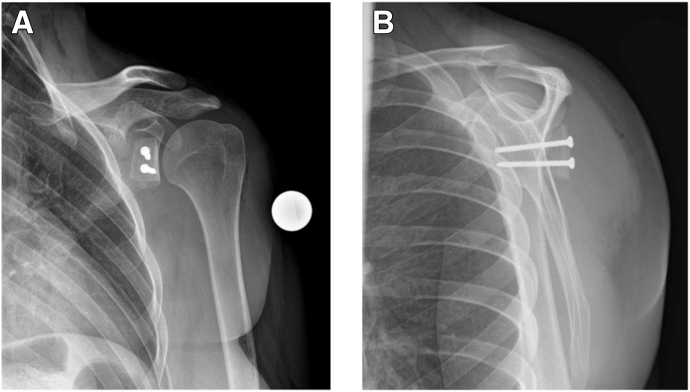
Fig 7.
Postoperative radiographs of a left shoulder showing proper placement of the bone graft and fixation hardware, without signs of loosening or failure. (A) Anteroposterior glenoid (Grashey) view. (B) Scapular Y-view.
Table 3.
Pearls and Pitfalls of Open Posterior Glenoid Augmentation With Iliac Crest Autograft
| Pearls |
| Appropriate dissection between infraspinatus and teres minor |
| Vertical capsulotomy allowing later repair |
| Capsulolabral repair |
| Appropriate graft placement—K-wires allow handling |
| Placement of graft flush to 1 mm lateral to joint |
| Pitfalls |
| Inadequate exposure |
| Inappropriate screw trajectory |
| Neurovascular injury |
Discussion
Posterior shoulder instability has become increasingly recognized as an under-reported but important pathology, particularly in athletes.3 Arthroscopic capsulolabral repair has become the standard of care; however, open bone grafting techniques play an important role, although their indications have not yet been clearly defined.6 Reported recurrence rates of posterior shoulder arthroscopic capsulolabral repair range from 3.4% to 35%, whereas the largest series published, comprising 297 shoulders, reported a 6.4% revision rate.6,19 Taking into consideration the large range of failure rates and varying pathologies regarding glenoid bone loss and glenoid version, posterior bone block procedures have an important role in treatment.
Unlike anterior shoulder instability, critical bone loss has yet to be defined in posterior shoulder instability. One indication is posterior glenoid bone loss. In a 2016 study by Mauro et al.,9 a smaller glenoid bone width was the only MRI measurement that resulted in poorer outcome scores. In a study by Bradley et al.,5 decreased glenoid bone width was also determined to be a risk factor for revision. The unique characteristics of posterior bone loss have recently been described. A study of 40 young patients with posterior shoulder instability evaluated computed tomography and MRI and concluded that posterior glenoid bone loss involves loss of glenoid concavity, is posterior sloping, and is characterized by increased retroversion.8 The location of posterior bone loss was also studied by the same group by evaluating 71 three-dimensional computed tomography scans. This group found that bone loss occurred 30° off the long axis of the glenoid in the posteroinferior direction from the 6:44 to 9:28 clock-face position.7 This pathology differs from bone loss seen in anterior shoulder instability, which is abrupt and parallel to the long axis of the glenoid. Therefore, the knowledge we have regarding anterior instability and bone loss cannot be extrapolated to that of posterior pathology. This leads to complex decision making in posterior instability patients.
Glenoid version may also play a role in treatment decision making and the use of posterior bone block procedures. Owens et al.10 published a prospective series of 714 military athletes and reported that glenoid retroversion was the strongest risk factor for the development of posterior shoulder instability: A 17% increased risk was seen with each 1° increase in retroversion. Mechanism of injury may also play a role in bony morphology and therefore treatment. In a study comparing posterior shoulder instability in 20 traumatic and 12 atraumatic patients, there was no difference in return to play or redislocation; however, those with an atraumatic mechanism had greater retroversion and worse functional outcome scores.20 Therefore, atraumatic posterior instability may be more likely to necessitate bone block procedures.
Grafts can be placed intra- or extra-articularly. The senior author prefers to use an iliac crest extra-articular autograft, as shown in this article, in patients with an insufficient posterior capsule and poor-quality soft tissue, without glenoid bone loss. The capsulolabral complex is repaired to the native glenoid, and the graft is fixed to the glenoid extra-articularly. The senior author's indication for extra-articular posterior glenoid augmentation is recurrent posterior instability with less than 15% bone loss and insufficient posterior soft tissues. In patients with more relevant (>15%) posterior glenoid bone loss, an intra-articular graft (fresh distal tibial allograft) is used to widen the glenoid track and to restore the articular cartilage. One of the first studies evaluating distal tibial allograft for posterior shoulder instability reported excellent outcomes after 2 years.21
The senior author finds posterior glenoid augmentation useful for patients with symptomatic posterior shoulder instability with an insufficient posterior capsulolabral complex and previous failed posterior capsulolabral repair. Although critical bone loss and critical glenoid retroversion have not yet been defined in the literature, the senior author prefers to treat these conditions with either glenoid reconstruction using fresh distal tibial allograft (posterior glenoid bone loss >15%) or corrective glenoid osteotomy (retroversion >20°). A study of 11 cadaveric shoulders evaluated different amounts of glenoid bone loss and its repair. They reported that a defect over 20% resulted in continued instability after labral repair. Although this is the best study to date, it is now known that posterior glenoid bone loss is not abrupt and parallel to the long axis of the glenoid as was tested in this model.22 Future studies are required to determine the critical amount of bone loss and the amount of pathologic retroversion in a clinically accurate model.
Posterior shoulder bone block procedures play an important role in patients with significant glenoid bone loss and retroversion. An iliac crest extra-articular graft, as described in this article, is preferred in patients with recurrent posterior instability owing to insufficient-quality posterior capsule and soft tissue without bone loss. Future studies are needed to define critical bone loss in posterior shoulder instability and refine indications for posterior bone block procedures.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.P.E. receives personal fees from Steadman Philippon Research Institute (SPRI), outside the submitted work. Current paid employee at SPRI. SPRI exercises special care to identify any financial interests or relationships related to research conducted here. During the past calendar year, SPRI has received grant funding or in-kind donations from Arthrex, Department of DefenseOffice of Naval Research, DJO, MLB, Ossur, Siemens, Smith & Nephew, and XTRE. P-C.N. receives fellowship support from Arthrex, outside the submitted work. P.J.M. is a consultant for Arthrex, Medibridge, and Springer Publishing; receives royalties from Arthrex, Medibridge, and Springer Publishing; receives grant support from Arthrex; receives stock from VuMedi; and reports that his institution receives funding from Smith & Nephew, Siemens, and Össur, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step illustration of open capsulorrhaphy with extra-articular posterior glenoid augmentation with iliac crest autograft in a patient's left shoulder in the lateral decubitus position. Posterior labral deficiency is observed between the 6- and 10-o'clock positions. Three 1.8-mm knotless all-suture anchors (FiberTak) are placed at the 6-o'clock position, 7:30 clock-face position, and 9-o'clock position. A soft-tissue labral repair is accomplished by passing sutures through the capsulolabral complex with a free needle and then tying them in horizontal mattress fashion. A 25 × 20–mm tricortical bone graft is harvested from the iliac crest in the standard fashion and fixed flush on the posterior glenoid using two 3.5-mm fully threaded stainless-steel cortical screws in a lag by application technique. Subsequent capsulorrhaphy is performed by advancing the capsule in a pants-over-vest manner, placing the bone graft extra-articular and allowing the capsule to be plicated.
References
- 1.Owens B.D., Duffey M.L., Nelson B.J., DeBerardino T.M., Taylor D.C., Mountcastle S.B. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168–1173. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 2.Zacchilli M.A., Owens B.D. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92:542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 3.Bernhardson A.S., Murphy C.P., Aman Z.S., LaPrade R.F., Provencher M.T. A prospective analysis of patients with anterior versus posterior shoulder instability: A matched cohort examination and surgical outcome analysis of 200 patients. Am J Sports Med. 2019;47:682–687. doi: 10.1177/0363546518819199. [DOI] [PubMed] [Google Scholar]
- 4.Arner J.W., McClincy M.P., Bradley J.P. Arthroscopic stabilization of posterior shoulder instability is successful in American football players. Arthroscopy. 2015;31:1466–1471. doi: 10.1016/j.arthro.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Bradley J.P., Arner J.W., Jayakumar S., Vyas D. Risk factors and outcomes of revision arthroscopic posterior shoulder capsulolabral repair. Am J Sports Med. 2018;46:2457–2465. doi: 10.1177/0363546518785893. [DOI] [PubMed] [Google Scholar]
- 6.Bradley J.P., McClincy M.P., Arner J.W., Tejwani S.G. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: A prospective study of 200 shoulders. Am J Sports Med. 2013;41:2005–2014. doi: 10.1177/0363546513493599. [DOI] [PubMed] [Google Scholar]
- 7.Dekker T.J., Peebles L.A., Goldenberg B.T., Millett P.J., Bradley J.P., Provencher M.T. Location of the glenoid defect in shoulders with recurrent posterior glenohumeral instability. Am J Sports Med. 2019;47:3051–3056. doi: 10.1177/0363546519876282. [DOI] [PubMed] [Google Scholar]
- 8.Beaulieu-Jones B.R., Peebles L.A., Golijanin P. Characterization of posterior glenoid bone loss morphology in patients with posterior shoulder instability. Arthroscopy. 2019;35:2777–2784. doi: 10.1016/j.arthro.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Mauro C.S., McClincy M.P., Bradley J.P. Effect of glenoid version and width on outcomes of arthroscopic posterior shoulder stabilization. Am J Sports Med. 2016;44:941–947. doi: 10.1177/0363546516631738. [DOI] [PubMed] [Google Scholar]
- 10.Owens B.D., Campbell S.E., Cameron K.L. Risk factors for posterior shoulder instability in young athletes. Am J Sports Med. 2013;41:2645–2649. doi: 10.1177/0363546513501508. [DOI] [PubMed] [Google Scholar]
- 11.Millett P.J., Clavert P., Hatch G.F., III, Warner J.J. Recurrent posterior shoulder instability. J Am Acad Orthop Surg. 2006;14:464–476. doi: 10.5435/00124635-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz D.G., Goebel S., Piper K., Kordasiewicz B., Boyle S., Lafosse L. Arthroscopic posterior bone block augmentation in posterior shoulder instability. J Shoulder Elbow Surg. 2013;22:1092–1101. doi: 10.1016/j.jse.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Wellmann M., Pastor M.F., Ettinger M., Koester K., Smith T. Arthroscopic posterior bone block stabilization-early results of an effective procedure for the recurrent posterior instability. Knee Surg Sports Traumatol Arthrosc. 2018;26:292–298. doi: 10.1007/s00167-017-4753-x. [DOI] [PubMed] [Google Scholar]
- 14.Struck M., Wellmann M., Becher C., Pastor M.F., Smith T. Results of an open posterior bone block procedure for recurrent posterior shoulder instability after a short- and long-time follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24:618–624. doi: 10.1007/s00167-014-3495-2. [DOI] [PubMed] [Google Scholar]
- 15.Servien E., Walch G., Cortes Z.E., Edwards T.B., O'Connor D.P. Posterior bone block procedure for posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2007;15:1130–1136. doi: 10.1007/s00167-007-0316-x. [DOI] [PubMed] [Google Scholar]
- 16.Levigne C., Garret J., Walch G. Posterior bone block for posterior instability. Tech Shoulder Elbow Surg. 2005;6:26–35. [Google Scholar]
- 17.Ernstbrunner L., Plachel F., Heuberer P. Arthroscopic versus open iliac crest bone grafting in recurrent anterior shoulder instability with glenoid bone loss: A computed tomography-based quantitative assessment. Arthroscopy. 2018;34:352–359. doi: 10.1016/j.arthro.2017.07.034. [DOI] [PubMed] [Google Scholar]
- 18.Warner J.J., Gill T.J., O'Hollerhan J.D., Pathare N., Millett P.J. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34:205–212. doi: 10.1177/0363546505281798. [DOI] [PubMed] [Google Scholar]
- 19.DeLong J.M., Jiang K., Bradley J.P. Posterior instability of the shoulder: A systematic review and meta-analysis of clinical outcomes. Am J Sports Med. 2015;43:1805–1817. doi: 10.1177/0363546515577622. [DOI] [PubMed] [Google Scholar]
- 20.Katthagen J.C., Tahal D.S., Montgomery S.R., Horan M.P., Millett P.J. Association of traumatic and atraumatic posterior shoulder instability with glenoid retroversion and outcomes after arthroscopic capsulolabral repair. Arthroscopy. 2017;33:284–290. doi: 10.1016/j.arthro.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Millett P.J., Schoenahl J.Y., Register B., Gaskill T.R., van Deurzen D.F., Martetschlager F. Reconstruction of posterior glenoid deficiency using distal tibial osteoarticular allograft. Knee Surg Sports Traumatol Arthrosc. 2013;21:445–449. doi: 10.1007/s00167-012-2254-5. [DOI] [PubMed] [Google Scholar]
- 22.Nacca C., Gil J.A., Badida R., Crisco J.J., Owens B.D. Critical glenoid bone loss in posterior shoulder instability. Am J Sports Med. 2018;46:1058–1063. doi: 10.1177/0363546518758015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step illustration of open capsulorrhaphy with extra-articular posterior glenoid augmentation with iliac crest autograft in a patient's left shoulder in the lateral decubitus position. Posterior labral deficiency is observed between the 6- and 10-o'clock positions. Three 1.8-mm knotless all-suture anchors (FiberTak) are placed at the 6-o'clock position, 7:30 clock-face position, and 9-o'clock position. A soft-tissue labral repair is accomplished by passing sutures through the capsulolabral complex with a free needle and then tying them in horizontal mattress fashion. A 25 × 20–mm tricortical bone graft is harvested from the iliac crest in the standard fashion and fixed flush on the posterior glenoid using two 3.5-mm fully threaded stainless-steel cortical screws in a lag by application technique. Subsequent capsulorrhaphy is performed by advancing the capsule in a pants-over-vest manner, placing the bone graft extra-articular and allowing the capsule to be plicated.