Abstract
Background:
Nearly half of all pregnancies in the United States each year are unintended, with the highest rates observed among non-Hispanic black and Hispanic women. Little is known about whether variations in unintended pregnancy and contraceptive use across racial and ethnic groups persist among women Veteran VA-users who have more universal access than other populations to health care and contraceptive services.
Objectives:
The objectives of this study were to identify history of unintended pregnancy and describe patterns of contraceptive use across racial and ethnic groups among women Veterans accessing VA primary care.
Study Design:
Cross-sectional data from a national random sample of women Veterans (n=2302) ages 18-44 who had accessed VA primary care in the previous 12 month were used to assess history of unintended pregnancy (pregnancies reported as either ‘unwanted’ or having occurred ‘too soon’). Any contraceptive use at last sex (both prescription and non-prescription methods) and prescription contraceptive use at last sex were assessed in the subset of women (n=1341) identified as being at risk for unintended pregnancy. Prescription contraceptive methods include long acting reversible contraceptive methods (intrauterine devices (IUDs) and subdermal implants), hormonal methods (pill, patch, ring, and injection), and female or male sterilization; non-prescription methods include barrier methods (e.g., condoms, diaphragm), fertility-awareness methods, and withdrawal. Multivariable logistic regression models were used to examine the relationship between race/ethnicity with unintended pregnancy and contraceptive use at last sex.
Results:
Overall, 94.4% of women Veterans at risk of unintended pregnancy used any method of contraception at last sex. IUDs (18.9%), female surgical sterilization (16.9%), and birth control pills (15.9%) were the three most frequently used methods across the sample. IUDs were the most frequently used method for Hispanic, non-Hispanic White, and other non-Hispanic women, while female surgical sterilization was the most frequently used method among non-Hispanic black women. In adjusted models, Hispanic women (aOR=1.60, 95%CI:1.15,2.21) and non-Hispanic black women (aOR=1.84, 95%CI:1.44,2.36) were significantly more likely than non-Hispanic white women to report any history of unintended pregnancy. In the subcohort of 1341 women at risk of unintended pregnancy, there were no significant racial/ethnic differences in use of any contraception at last sex. However, significant differences were observed in the use of prescription methods at last sex. Hispanic women (aOR=0.51, 95%CI:0.35,0.75) and non-Hispanic black women (aOR=0.69, 95%CI:0.51,0.95) were significantly less likely than non-Hispanic white women to have used prescription contraception at last sex.
Conclusions:
Significant racial and ethnic differences exist in unintended pregnancy and contraceptive use among women Veterans using VA care, suggesting the need for interventions to address potential disparities. Improving access to and delivery of patient-centered reproductive goals assessment and contraceptive counseling that can address knowledge gaps while respectfully considering individual patient preferences is needed to support women Veterans’ decision-making and ensure equitable reproductive health services across VA.
Keywords: reproductive health equity, ECUUN, race, VA, family planning
Introduction
Increasing women’s access to contraception, with the ultimate goal of helping women achieve their reproductive goals, is an ongoing public health objective in the United States.1 Healthcare systems and public health officials have focused on rates of unintended pregnancy (pregnancies reported as either ‘unwanted’ or ‘mistimed’)2,3 as an indicator of this access and the degree to which women’s reproductive goals are met. Although the meaning and measurement of unintended pregnancy has been subject to ongoing conceptual critique because of its potentially limited ability to capture the complex nature of women’s thoughts and feelings about pregnancy4 and diverse perspectives on the salience and desirability of pregnancy planning,5 it nonetheless remains a useful metric with which to gauge women’s ability to access contraception and/or achieve their reproductive goals and to provide comparisons across time and subpopulations.
Nearly half of all pregnancies in the United States each year are unintended, with the highest rates observed among non-Hispanic black and Hispanic women.3,6 Though the underlying causes of racial and ethnic differences in unintended pregnancy rates are not fully understood,7 differential patterns of contraceptive use has been identified as a potential proximate determinant.8,9 Past research has suggested that non-Hispanic black women in the US are less likely than non-Hispanic white or Hispanic women to use any contraceptive method10,11 and highly effective methods such as long acting reversible contraception (LARC; i.e. intrauterine device (IUD) or subdermal implant).10,12 Black and Hispanic women may also be more likely than white women to experience gaps in contraceptive use that increase the risk of unintended pregnancy.13,14 However, analyses of more recent data from the National Survey of Family Growth suggest changes over time, highlighting increased LARC use overall among non-Hispanic black and Hispanic women15 resulting in no significant differences in LARC use by racial or ethnic group membership.12 Improved understanding of variations in contraceptive use across racial and ethnic groups will offer a baseline from which to evaluate system-based efforts to better meet the reproductive health needs of diverse populations.
As the largest integrated healthcare system in the U.S. and with a large population of racial and ethnic minority women, the Veterans Administration (VA) healthcare system offers an ideal setting for further investigation into racial and ethnic differences in contraceptive use. The number of women Veterans accessing VA healthcare has doubled since 2000, with women Veterans of reproductive age representing the fastest growing group: 7.5% of Veteran VA patients are women, 43% of whom are between the ages of 18 and 44.16 Female VA users also represent a vulnerable population, with a high prevalence of mental illness and medical comorbidities16–18 and disproportionately (42%) from racial and ethnic minority groups.16
Overall rates of contraceptive use and unintended pregnancy among women Veterans served by the VA are similar to those in the U.S. population,19 but racial and ethnic variation in these rates have not previously been reported. Previous research examined racial and ethnic differences in women Veterans’ knowledge about contraception20 and contraceptive preferences and beliefs,21 as well as associations between perceived race-based discrimination and contraceptive use.22 However, whether racial and ethnic differences in contraceptive use patterns and unintended pregnancy exist among women VA-users, who have relatively uniform access to healthcare and to the full range of contraceptive methods, remains unknown. The objective of the current study was therefore to describe variations in unintended pregnancy and contraceptive use among women Veteran VA enrollees across racial and ethnic groups. This study fills a gap in the literature on women Veterans’ health and offers evidence to help achieve the VA’s mission to ensure that all women Veterans receive high quality, equitable reproductive health care.
Materials and Methods
Study design and sample.
Data for this study are part of the larger Examining Contraceptive Use and Unmet Need (ECUUN) Study, which assessed women Veterans’ contraceptive use, pregnancy history, and experiences with VA reproductive healthcare. The study included a telephone-based, cross-sectional survey with a national random sample of women Veteran VA users ages 18-44 who had accessed VA primary care in the previous 12 months. Potentially eligible participants were mailed a study packet, including an invitation, a study brochure, and a postage-paid reply card, and asked to express interest in participating or to opt out via either the reply card or by calling the toll-free study telephone number. Recipients who did not opt-out and those who expressed interest were then called and invited to participate. If interested, potential participants underwent eligibility screening and provided verbal consent over the phone; enrolled and consented participants then engaged in a 45-60 minute computer-assisted telephone interview, and were compensated $30 for their time. All interviews took place between April 2014 and January 2016. The University of Pittsburgh and the VA Pittsburgh Institutional Review Boards approved all study procedures.
Invitations were mailed to 8,198 women; 2,769 women were screened and enrolled, and 2,302 surveys were completed, for a response rate of 83% among enrolled participants and an overall response rate of 28%. A comparison using VA administrative data of participants to non-participants from the sampling frame revealed no significant differences in age, race/ethnicity, marital status, income, presence of medical and mental illness, and geographic region (standardized differences ranging from 0.07 – 0.13), suggesting that the overall ECUUN sample is representative of the larger population of women VA users of reproductive age.
Measures
The outcomes of interest for this study included any history of unintended pregnancy, use of any method of contraception at last heterosexual intercourse, and use of prescription method (vs non-prescription method or no method) at last heterosexual intercourse. We assessed any history of unintended pregnancy in the full cohort (n=2302). Participants were asked two questions to assess the intention status of each reported pregnancy; per standard convention,2,3 pregnancies were classified as either “unwanted”, occurring at the “right time”, “too late”, or “too soon” (other choices included “didn’t care” or “didn’t know”). Pregnancies reported as either “unwanted” or having occurred “too soon” were considered unintended.19
From the 2,302 women Veterans who completed the survey, a subset of 1,341 women were identified as being at risk for unintended pregnancy at the time of the survey. Women were considered at risk for unintended pregnancy if they had been sexually active with a male partner in the past year, had no history of hysterectomy or infertility, and were not pregnant, within 6 weeks postpartum, or currently trying to get pregnant. Any contraceptive use (both prescription and non-prescription methods) and prescription contraception use at last sex were assessed only in the at-risk cohort. We assessed prescription contraceptive method use separately from any contraceptive method use because prescription methods are typically more effective at preventing pregnancy than non-prescription methods and require direct interaction with a healthcare provider. Prescription contraceptive methods include LARC (IUDS and subdermal implants), hormonal methods (pill, patch, ring, and injection), and female or male sterilization; non-prescription methods include barrier methods (e.g., condoms, diaphragm), fertility-awareness methods, and withdrawal. National studies typically report contraceptive use as ‘current’ if used in the month prior to assessment;12 for these analyses, we chose instead to report contraceptive use at last heterosexual sex (even if more than one month prior to the survey interview) in order to capture women Veterans’ behavior at the time of risk. Women who reported using more than one method at last sex were classified as using a prescription method if any of the multiple reported methods was a prescription method.
The independent variable of interest was self-reported race/ethnicity. Participants were asked to choose one or more groups that described their racial background (options included White, Black, Asian, Pacific Islander/Native Hawaiian, American Indian/Native Alaskan, and Other (please specify)). If more than one group was chosen, participants were then asked whether they identified with one of the selected racial groups more than the other(s). If they identified a primary group, participants were categorized as a member of that group; if they did not identify with one group more than another, participants were categorized as ‘multiple races.’ For analysis, the broad list of racial/ethnic categories was collapsed into non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic other (includes multiracial, Asian, Pacific Islander, and Native American women).
Based on a priori theoretical associations with contraceptive use and unintended pregnancy, we examined covariates including age, education, marital status, annual household income, parity, having additional non-VA insurance, history of medical conditions that might impact contraceptive method selection (e.g. hypertension, obesity, diabetes), history of mental health conditions (e.g. depression, post-traumatic stress disorder, schizophrenia, anxiety), and history of military sexual trauma. Geographic region was determined using VA administrative data.
Data Analysis
We compared participant demographic characteristics for the full study cohort and the cohort at-risk for unintended pregnancy by race/ethnicity using ANOVA for continuous variables and chi-square tests for categorical variables. We described the types of contraceptive methods used by race/ethnicity. We then compared outcome variables (any unintended pregnancy for the full cohort, any contraceptive use at last sex and prescription contraceptive use at last sex for the subset of women at risk of unintended pregnancy) across racial/ethnic groups using chi-square tests or Fisher’s exact tests. Multivariable logistic regression models were used to examine associations between race/ethnicity and each outcome variable, adjusting for all covariates. Unadjusted and adjusted odds ratios (ORs and aORs) and 95% confidence intervals (CIs) are reported. Statistical analyses were performed using IBM SPSS v25,23 with statistical significance set at p < 0.05.
Results
Unintended Pregnancy (full cohort, n=2302).
Sample characteristics for the full cohort are presented in Table 1. Among these women Veterans, 51.6% were non-Hispanic white, 28.9% non-Hispanic black, 12.4% Hispanic, and 7.1% non-Hispanic ‘other.’ More than half were parous (63.6%) and had a college education (53%); less than half had an annual income of at least $40,000 (47.7%) or were married (41.1%). Non-Hispanic black (30.4%) and Hispanic women (27%) were more likely to be single than were non-Hispanic white women (18.7%); non-Hispanic black women (9.1% and 13.1%, respectively) were also less likely than white women (12.5% and 16.6%, respectively) to have an annual household income in the top two income brackets.
Table 1.
Characteristics of women Veterans by race/ethnicity, full cohort (n = 2302)
| Total | Hispanic (n=285, %) | NH White (n=1188, %) | NH Black (n=665, %) | NH Other (n=164, %) | p-value | |
|---|---|---|---|---|---|---|
| Age | < 0.001 | |||||
| 20-24 | 3.0 | 2.1 | 3.5 | 2.4 | 3.0 | |
| 25-29 | 16.7 | 23.2 | 17.9 | 12.0 | 15.9 | |
| 30-34 | 29.9 | 32.3 | 30.1 | 28.3 | 30.5 | |
| 35-39 | 25.4 | 22.8 | 24.7 | 26.5 | 30.5 | |
| 40-45 | 25.0 | 19.6 | 23.7 | 30.8 | 20.1 | |
| Marital Statusa | < 0.001 | |||||
| Single | 23.3 | 27.0 | 18.7 | 30.4 | 20.9 | |
| Married | 41.1 | 42.1 | 45.5 | 32.8 | 41.1 | |
| Unmarried but cohabiting | 8.9 | 9.8 | 10.9 | 4.7 | 10.4 | |
| DSW | 26.7 | 21.1 | 24.9 | 32.1 | 27.6 | |
| Annual Household Incomeb | 0.018 | |||||
| < $20,000 | 20.3 | 19.0 | 20.5 | 19.4 | 24.2 | |
| $20,000 - $39,999 | 31.9 | 35.2 | 30.3 | 32.5 | 36.0 | |
| $40,000 - $59,999 | 22.1 | 23.6 | 20.0 | 25.9 | 19.3 | |
| $60,000 - $79,999 | 10.9 | 10.2 | 12.5 | 9.1 | 8.1 | |
| ≥ $80,000 | 14.7 | 12.0 | 16.6 | 13.1 | 12.4 | |
| Education | 0.412 | |||||
| HS / trade school | 8.6 | 10.2 | 8.9 | 7.7 | 7.3 | |
| Some college | 38.3 | 35.4 | 39.5 | 36.8 | 40.9 | |
| College | 39.4 | 43.5 | 38.6 | 39.8 | 37.2 | |
| Master’s degree or higher | 13.6 | 10.9 | 13.0 | 15.6 | 14.6 | |
| Parityc | 0.002 | |||||
| 0 | 36.4 | 36.8 | 39.9 | 30.2 | 35.4 | |
| 1 | 24.1 | 23.5 | 23.0 | 25.8 | 26.2 | |
| 2 | 25.4 | 25.3 | 25.5 | 25.5 | 25.0 | |
| 3 | 10.2 | 11.9 | 8.0 | 13.9 | 8.5 | |
| ≥ 4 | 3.8 | 2.5 | 3.6 | 4.5 | 4.9 | |
| Has additional Non-VA Insurance | 52.1 | 51.2 | 54.1 | 50.2 | 46.3 | 0.161 |
| ≥1 Medical condition | 56.2 | 52.3 | 54.2 | 61.7 | 54.9 | 0.008 |
| ≥1 Mental health condition | 68.7 | 66.0 | 72.5 | 64.4 | 64.0 | 0.001 |
| History of military sexual trauma | 55.0 | 56.5 | 56.9 | 49.6 | 59.8 | 0.010 |
| Geographic location | <0.001 | |||||
| Northeast | 8.7 | 7.7 | 9.8 | 6.0 | 13.4 | |
| Midwest | 17.8 | 9.5 | 25.2 | 10.7 | 7.9 | |
| South | 53.1 | 54.7 | 42.0 | 74.7 | 43.3 | |
| West | 20.4 | 28.1 | 23.1 | 8.6 | 35.4 | |
NH, non-Hispanic; SD, standard deviation; DSW, divorced, separated, widowed; HS, high school
Missing under the Hispanic ethnicity question was coded as non-Hispanic and missing race was coded as other race.
P-values calculated using Pearson’s chi-square test
n=2 missing;
n=25 missing;
n=5 missing
More than half (57.2%) of women reported a history of unintended pregnancy; prevalence was highest among non-Hispanic black women (66.8% of black women had at least one unintended pregnancy), and lowest among non-Hispanic white women (50.8%). Results of unadjusted and adjusted logistic regression models are shown in in Table 2. After controlling for age, marital status, education, income, parity, non-VA insurance, history of medical or mental illness, history of military sexual trauma, and geographic region, women from each racial and ethnic minority group remained significantly more likely than non-Hispanic white women to have had an unintended pregnancy in their lifetime; non-Hispanic black women having the highest likelihood (aOR = 1.81, 95% CI: 1.39, 2.36), followed by Hispanic women (aOR = 1.58, 95% CI: 1.13, 2.19) and other non-Hispanic women (aOR = 1.58, 95% CI: 1.04, 2.34).
Table 2.
Associations between race/ethnicity and history of any unintended pregnancy, full cohort
| Model 1 – Univariate (n=2297) | Unadjusted | ||
|---|---|---|---|
| Any unintended pregnancy n (%)+ | OR (95% CI) | p value | |
| Race/Ethnicity | <0.001 | ||
| Hispanic | 171 (60.0) | 1.450 (1.115, 1.886) | 0.006 |
| NH Black | 442 (66.8) | 1.942 (1.594, 2.367) | < 0.001 |
| NH Other | 99 (60.4) | 1.473 (1.056, 2.054) | 0.023 |
| NH White | 603 (50.8) | (ref) | - |
| Model 2 – Multivariate (n=2270) | Adjusted | ||
| aOR (95% CI) | p value | ||
| Race/Ethnicity | <0.001 | ||
| Hispanic | 170 (59.9) | 1.575 (1.132, 2.191) | 0.007 |
| NH Black | 438 (66.9) | 1.805 (1.393, 2.364) | < 0.001 |
| NH Other | 97 (60.6) | 1.576 (1.040, 2.339) | 0.032 |
| NH White | 597 (51.0) | (ref) | - |
| Age | |||
| 20-24 | 26 (39.4) | 0.902 (0.482, 1.689) | 0.748 |
| 25-29 | 170 (44.7) | 0.928 (0.677, 1.272) | 0.641 |
| 30-34 | 384 (56.8) | (ref) | - |
| 35-39 | 336 (58.1) | 0.750 (0.568, 0.991) | 0.043 |
| 40-45 | 386 (67.7) | 1.145 (.856, 1.532) | 0.360 |
| Marital Status | |||
| Single | 220 (41.6) | 1.398 (1.020, 1.915) | 0.037 |
| Married | 562 (60.3) | (ref) | - |
| Unmarried but cohabiting | 102 (50.0) | 1.383 (0.932, 2.053) | 0.108 |
| Divorced / Separated / Widowed | 418 (69.1) | 1.688 (1.263, 2.257) | < 0.001 |
| Education | |||
| High school / technical school | 120 (60.9) | 1.001 (0.676, 1.484) | 0.995 |
| Some college | 513 (59.0) | 0.977 (0.767, 1.245) | 0.852 |
| College | 502 (56.0) | (ref) | - |
| Master’s degree or higher | 167 (54.2) | 0.955 (0.688, 1.325) | 0.781 |
| Household Income | |||
| < $20,000 | 235 (51.2) | (ref) | - |
| $20,000 - $39,999 | 453 (62.5) | 1.162 (0.859, 1.570) | 0.330 |
| $40,000 - $59,999 | 284 (56.5) | 0.766 (0.543, 1.080) | 0.129 |
| $60,000 - $79,999 | 146 (58.6) | 1.031 (0.668, 1.590) | 0.892 |
| ≥ $80,000 | 184 (55.1) | 0.750 (0.493, 1.143) | 0.181 |
| Parity | |||
| 0 | 181 (22.0) | (ref) | - |
| 1 | 369 (67.2) | 8.016 (6.148, 10.451) | < 0.001 |
| 2 | 464 (80.3) | 17.778 (13.104, 24.118) | < 0.001 |
| 3 | 209 (89.7) | 35.699 (21.909, 58.169) | < 0.001 |
| 4 or more | 79 (90.8) | 43.308 (19.940, 94.065) | < 0.001 |
| Has additional non-VA insurance | 682 (57.8) | 0.916 (0.733, 1.144) | 0.440 |
| > 1 Medical Condition | 786 (61.5) | 0.925 (0.745, 1.149) | 0.481 |
| > 1 Mental Health Condition | 944 (60.4) | 1.472 (1.160, 1.868) | < 0.001 |
| History of military sexual trauma | 744 (59.7) | 1.170 (0.943, 1.453) | 0.154 |
| Geographic location | |||
| Northeast | 99 (50.0) | 0.721 (0.496, 1.047) | 0.086 |
| Midwest | 224 (55.0) | 0.939 (0.701, 1.258) | 0.674 |
| South | 736 (61.1) | (ref) | - |
| West | 243 (52.8) | 0.934 (0.710, 1.229) | 0.627 |
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval; NH, non-Hispanic.
Percent values may not add up to 100 due to rounding
Contraceptive Use (at-risk cohort, n=1341).
Sample characteristics of the at-risk cohort are presented in Table 3. Among the 1341 women identified as being at-risk of unintended pregnancy, 52.3% were non-Hispanic white, 27.8% non-Hispanic black, 12.6% Hispanic, and 7.2% non-Hispanic ‘other’ More than half were parous (68.6%), had a college education (52.9%), and an annual income of at least $40,000 (52.3%), and nearly half (47.7%) were married. Some significant racial and ethnic differences were observed. Hispanic (26%) and non-Hispanic black women (28.4%) were more likely than non-Hispanic white women (16.4%) to be single, and non-Hispanic black women (23.7%) were less likely to be nulliparous than non-Hispanic white women (36.2%).
Table 3.
Characteristics of women Veterans at-risk for unintended pregnancy& by race/ethnicity (n=1431)
| Total | Hispanic (n=169, %) | NH White (n=702, %) | NH Black (n=373, %) | NH Other (n=97, %) | p-value | |
|---|---|---|---|---|---|---|
| Age | 0.010 | |||||
| 20-24 | 3.9 | 1.8 | 4.7 | 3.5 | 3.1 | |
| 25-59 | 18.7 | 26.0 | 19.7 | 13.4 | 19.6 | |
| 30-34 | 32.4 | 33.7 | 33.8 | 30.8 | 26.8 | |
| 35-39 | 25.1 | 22.5 | 24.2 | 28.2 | 24.7 | |
| 40-45 | 19.8 | 16.0 | 17.7 | 24.1 | 25.8 | |
| Marital Statusa | < 0.001 | |||||
| Single | 21.1 | 26 | 16.4 | 28.4 | 18.8 | |
| Married | 43.6 | 46.2 | 48.1 | 33.8 | 43.8 | |
| Unmarried but cohabiting | 8.7 | 6.5 | 10.4 | 5.6 | 12.5 | |
| DSW | 26.6 | 21.3 | 25.1 | 32.2 | 25 | |
| Annual Household Incomeb | 0.071 | |||||
| < $20,000 | 20.5 | 16.6 | 21.7 | 20 | 21.1 | |
| $20,000 - $39,999 | 31.7 | 34.9 | 29.5 | 33.5 | 35.8 | |
| $40,000 - $59,999 | 21.6 | 25.4 | 18.9 | 25.1 | 21.1 | |
| $60,000 - $79,999 | 11.4 | 11.8 | 12.3 | 9.7 | 10.5 | |
| ≥ $80,000 | 14.7 | 11.2 | 17.6 | 11.6 | 11.6 | |
| Education | 0.454 | |||||
| HS / trade school | 7.9 | 7.7 | 8.3 | 8.0 | 7.9 | |
| Some college | 39.2 | 37.3 | 39.7 | 37.3 | 39.2 | |
| College | 39.9 | 46.2 | 39 | 39.4 | 39.9 | |
| Master’s degree or higher | 13.0 | 8.9 | 13 | 15.3 | 13 | |
| Parityc | 0.001 | |||||
| 0 | 31.4 | 30.8 | 36.2 | 23.7 | 26.8 | |
| 1 | 24.8 | 26.6 | 22.5 | 28.2 | 24.7 | |
| 2 | 28.0 | 27.2 | 28.8 | 27.4 | 25.8 | |
| 3 | 11.6 | 12.4 | 9.1 | 15.1 | 14.4 | |
| ≥ 4 | 4.3 | 3.0 | 3.3 | 5.6 | 8.2 | |
| Has additional Non-VA Insurance | 50.9 | 47.9 | 52.4 | 50.1 | 47.4 | 0.614 |
| ≥1 Medical condition | 53.3 | 47.9 | 50.7 | 60.6 | 53.6 | 0.008 |
| ≥1 Mental health condition | 66.0 | 60.9 | 71.1 | 59.8 | 61.9 | 0.001 |
| History of military sexual trauma | 52.7 | 53.8 | 56.3 | 44.2 | 57.7 | 0.002 |
| Geographic location | <0.001 | |||||
| Northeast | 7.9 | 4.1 | 9.5 | 5.1 | 13.4 | |
| Midwest | 18.2 | 8.3 | 26.2 | 10.7 | 6.2 | |
| South | 53.0 | 57.4 | 41.0 | 75.6 | 45.4 | |
| West | 20.9 | 30.2 | 23.2 | 8.6 | 35.1 | |
NH, non-Hispanic; SD, standard deviation; DSW, divorced, separated, widowed; HS, high school
Missing under the Hispanic ethnicity question was coded as non-Hispanic and missing race was coded as other race.
Women were considered at risk of unintended pregnancy if they had been sexually active with a man in the last year, had not had a hysterectomy, and were not infertile, pregnant, postpartum, or trying to get pregnant
P-values calculated using Pearson’s chi-square test
n=1 missing;
n=15 missing;
n=2 missing
Contraceptive methods used at last sex are shown in Figure 1. Overall, 94.4% of women Veterans at risk of unintended pregnancy used any method of contraception at last sex. IUDS (18.9%), female surgical sterilization (16.9%), and birth control pills (15.9%) were the three most frequently used methods across the sample; IUDs were the most frequently used method for Hispanic, non-Hispanic White, and other non-Hispanic women, while female surgical sterilization was the most frequently used method among non-Hispanic black women.
Figure 1. Percent of women using each contraceptive method* at last sex by race/ethnicity (among women at risk for unintended pregnancy).
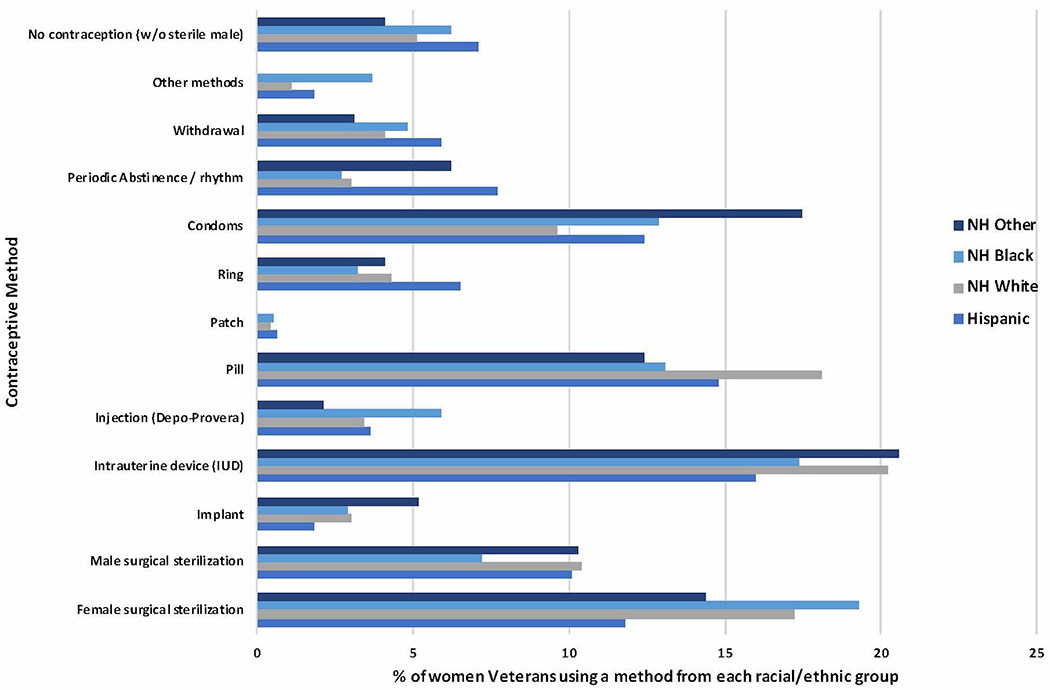
*Data are most effective contraceptive method used at last sex
Associations between race/ethnicity and contraceptive use at last sex are presented for the at-risk cohort in Tables 4 & 5. The proportion of women using any method of contraception at last sex was similar across race/ethnicity group, ranging from 93% to 96%. Prescription contraceptive use was highest among non-Hispanic white women (77.1%), and lowest among Hispanic black women (65.1%). After adjusting for potential confounders, there were no significant racial/ethnic differences in use of any contraception at last sex. However, significant differences were observed in the use of prescription methods at last sex. After adjusting for age, marital status, education, income, parity, non-VA insurance, history of medical or mental illness, history of military sexual trauma, and geographic region, Hispanic women (aOR = 0.54, 95% CI: 0.37, 0.77), non-Hispanic black women (aOR = 0.68, 95% CI: 0.51, 0.90), and other non-Hispanic women (aOR = 0.62, 95% CI: 0.39, 1.00) were significantly less likely than non-Hispanic white women to have used prescription contraception at last sex.
Table 4.
Associations between race/ethnicity and any contraceptive use at last sex, at-risk& cohort
| Model 1 – Univariate (n=1341) | Unadjusted | ||
|---|---|---|---|
| Any contraceptive use at last sex n (%)+ | OR (95% CI) | p value | |
| Race/Ethnicity | 0.653 | ||
| Hispanic | 157 (92.9) | 0.708 (0.360, 1.393) | 0.317 |
| NH Black | 350 (93.8) | 0.821 (0.479, 1.408) | 0.474 |
| NH Other | 93 (95.9) | 1.259 (0.438, 3.617) | 0.669 |
| NH White | 666 (94.9) | (ref) | - |
| Model 2 – Multivariate (n=1323) | Adjusted | ||
| aOR (95% CI) | p value | ||
| Race/Ethnicity | 0.436 | ||
| Hispanic | 157 (92.9) | 0.595 (0.289, 1.1223) | 0.158 |
| NH Black | 346 (93.8) | 0.712 (0.390, 1.300) | 0.269 |
| NH Other | 90 (95.7) | 1.108 (0.371, 3.311) | 0.855 |
| NH White | 657 (95.1) | (ref) | |
| Age | |||
| 20-24 | 46 (90.2) | 0.442 (0.144, 1.357) | 0.154 |
| 25-29 | 235 (94.8) | 0.761 (0.342, 1.690) | 0.502 |
| 30-34 | 414 (96.5) | (ref) | - |
| 35-39 | 309 (93.1) | 0.462 (0.231, 0.924) | 0.029 |
| 40-45 | 246 (93.5) | 0.476 (0.223, 1.017) | 0.055 |
| Marital Status | |||
| Single | 267 (94.7) | 1.823 (0.850, 3.908) | 0.123 |
| Married | 537 (93.7) | (ref) | - |
| Unmarried but cohabiting | 112 (95.7) | 1.906 (0.687, 5.285) | 0.215 |
| Divorced / Separated / Widowed | 334 (95.2) | 1.555 (0.786, 3.073) | 0.204 |
| Education | |||
| High school / technical school | 100 (94.3) | 0.623 (0.236, 1.643) | 0.338 |
| Some college | 483 (93.2) | 0.515 (0.285, 0.928) | 0.027 |
| College | 507 (95.8) | (ref) | - |
| Master’s degree or higher | 160 (94.1) | 0.748 (0.335, 1.669) | 0.478 |
| Household Income | |||
| < $20,000 | 253 (93.4) | (ref) | - |
| $20,000 - $39,999 | 405 (96.4) | 1.858 (0.892, 3.867) | 0.098 |
| $40,000 - $59,999 | 268 (93.4) | 1.063 (0.501, 2.257) | 0.873 |
| $60,000 - $79,999 | 145 (96.0) | 1.621 (0.552, 4.764) | 0.380 |
| ≥ $80,000 | 179 (92.3) | 0.877 (0.341, 2.253) | 0.784 |
| Parity | |||
| 0 | 385 (93.0) | (ref) | - |
| 1 | 308 (94.2) | 1.560 (0.816, 2.984) | 0.179 |
| 2 | 363 (97.3) | 4.120 (1.830, 9.277) | 0.001 |
| 3 | 141 (92.2) | 1.402 (0.633, 3.106) | 0.405 |
| 4 or more | 53 (94.6) | 2.331 (0.635, 8.564) | 0.202 |
| Has additional non-VA insurance | 634 (94.3) | 1.049 (0.615, 1.792) | 0.860 |
| > 1 Medical Condition | 668 (94.2) | 1.005 (0.600, 1.684) | 0.986 |
| > 1 Mental Health Condition | 823 (93.9) | 0.683 (0.385, 1.211) | 0.182 |
| History of military sexual trauma | 656 (94.0) | 0.900 (0.541, 1.498) | 0.686 |
| Geographic location | |||
| Northeast | 100 (95.2) | 1.256 (0.468, 3.372) | 0.651 |
| Midwest | 233 (95.9) | 1.382 (0.659, 2.900) | 0.392 |
| South | 657 (93.7) | (ref) | - |
| West | 260 (94.9) | 1.151 (0.601, 2.204) | 0.672 |
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval; NH, non-Hispanic.
Women were considered at risk of unintended pregnancy if they had been sexually active with a man in the last year, had not had a hysterectomy, and were not infertile, pregnant, postpartum, or trying to get pregnant
Percent values may not add up to 100 due to rounding
Table 5.
Associations between race/ethnicity and prescription contraceptive use at last sex, at-risk& cohort
| Model 1 – Univariate (n=1341) | Unadjusted | ||
|---|---|---|---|
| Prescription contraceptive use at last sex n (%)+ | OR (95% CI) | p value | |
| Race/Ethnicity | 0.002 | ||
| Hispanic | 110 (65.1) | 0.536 (0.372, 0.770) | 0.001 |
| NH Black | 260 (69.7) | 0.676 (0.508, 0.901) | 0.007 |
| NH Other | 67 (69.1) | 0.624 (0.388, 1.004) | 0.052 |
| NH White | 541 (77.1) | (ref) | - |
| Model 2 – Multivariate (n=1323) | Adjusted | ||
| aOR (95% CI) | p value | ||
| Race/Ethnicity | 0.005 | ||
| Hispanic | 110 (65.1) | 0.519 (0.351, 0.768) | 0.001 |
| NH Black | 259 (70.2) | 0.737 (0.534, 1.019) | 0.065 |
| NH Other | 65 (69.1) | 0.604 (0.364, 1.001) | 0.050 |
| NH White | 537 (77.7) | (ref) | - |
| Age | |||
| 20-24 | 36 (70.6) | 0.901 (0.456, 1.779) | 0.764 |
| 25-29 | 172 (69.4) | 0.863 (0.590, 1.263) | 0.448 |
| 30-34 | 332 (77.4) | (ref) | - |
| 35-39 | 231 (69.6) | 0.597 (0.422, 0.844) | 0.004 |
| 40-45 | 200 (76.0) | 0.780 (0.527, 1.155) | 0.214 |
| Marital Status | |||
| Single | 178 (63.1) | 0.680 (0.460, 1.003) | 0.052 |
| Married | 457 (79.8) | (ref) | - |
| Unmarried but cohabiting | 89 (76.1) | 1.028 (0.617, 1.712) | 0.916 |
| Divorced / Separated / Widowed | 247 (70.4) | 0.755 (0.530, 1.076) | 0.120 |
| Education | |||
| High school / technical school | 79 (74.5) | 1.073 (0.644, 1.789) | 0.787 |
| Some college | 382 (73.7) | 1.045 (0.773, 1.412) | 0.775 |
| College | 386 (73.0) | (ref) | - |
| Master’s degree or higher | 124 (72.9) | 0.965 (0.635, 1.465) | 0.865 |
| Household Income | |||
| < $20,000 | 172 (63.5) | (ref) | - |
| $20,000 - $39,999 | 325 (77.4) | 1.820 (1.271, 2.605) | 0.001 |
| $40,000 - $59,999 | 205 (71.4) | 1.260 (0.844, 1.882) | 0.258 |
| $60,000 - $79,999 | 119 (78.8) | 1.666 (0.974, 2.851) | 0.062 |
| ≥ $80,000 | 150 (77.3) | 1.393 (0.820, 2.366) | 0.220 |
| Parity | |||
| 0 | 275 (66.4) | (ref) | - |
| 1 | 216 (66.1) | 0.955 (0.682, 1.339) | 0.791 |
| 2 | 318 (85.3) | 2.713 (1.822, 4.039) | < 0.001 |
| 3 | 120 (78.4) | 1.845 (1.131, 3.009) | 0.014 |
| 4 or more | 42 (75.0) | 1.587 (0.790, 3.188) | 0.194 |
| Has additional non-VA insurance | 514 (76.5) | 1.185 (0.899, 1.561) | 0.229 |
| > 1 Medical Condition | 531 (74.9) | 1.088 (0.830, 1.427) | 0.540 |
| > 1 Mental Health Condition | 649 (74.1) | 0.951 (0.711, 1.271) | 0.733 |
| History of military sexual trauma | 520 (74.5) | 1.102 (0.843, 1.440) | 0.478 |
| Geographic location | |||
| Northeast | 80 (76.2) | 1.241 (0.745, 2.067) | 0.407 |
| Midwest | 185 (76.1) | 1.150 (0.796, 1.660) | 0.456 |
| South | 499 (71.2) | (ref) | - |
| West | 207 (75.5) | 1.244 (0.881, 1.756) | 0.215 |
OR, odds ratio; aOR, adjusted odds ratio; CI, confidence interval; NH, non-Hispanic.
Women were considered at risk of unintended pregnancy if they had been sexually active with a man in the last year, had not had a hysterectomy, and were not infertile, pregnant, postpartum, or trying to get pregnant
Percent values may not add up to 100 due to rounding
Comment
Principal Findings.
In this nationally representative survey of women Veterans of reproductive age using VA healthcare, we found significant racial and ethnic differences in women Veterans’ history of unintended pregnancy and contraceptive use that mirror observed differences in the general U.S. population. Women Veterans from racial or ethnic minority groups were more likely than non-Hispanic white women to have ever had an unintended pregnancy in their lifetime and less likely than non-Hispanic white women to have used prescription contraception at last sex.
Results.
Previous research suggests that observed differences in unintended pregnancy and contraceptive use may be partially explained by significant racial and ethnic variation in women’s contraceptive preferences and beliefs. Women from racial and ethnic minority groups have consistently been identified as more likely to report preferences for contraceptive features that align with non-prescription methods;8,9,21 these preferences may be related to concerns about contraceptive safety,24,25 personal control over whether and when to use the method,8 or lifestyle and relationship factors (such as affordability or the desire for a method not to alter a woman’s menstrual cycle).8 Racial and ethnic minority women are also more likely to express fatalistic views about pregnancy, i.e., the belief that pregnancy happens when it is supposed to happen4, irrespective of contraceptive use.9,21
Racial and ethnic differences in unintended pregnancy and contraceptive use may also be related to documented differences in contraceptive knowledge. In both non-Veteran9,25,26 and Veteran20 populations, racial and ethnic minority women have been found to have lower overall contraceptive knowledge than non-Hispanic white women; since knowledge is critical for informed contraceptive choice, lower levels of knowledge may be influencing minority women Veterans’ use (or non-use) of specific methods at last sex. A separate analysis using data from the ECUUN study suggests that women Veterans with greater contraceptive knowledge were more likely to use a LARC method (vs. non-prescription methods or no method) and were more likely to express strong preferences for method effectiveness, which is significantly associated with greater likelihood of both LARC and hormonal method (i.e., prescription method) use.27 These prior findings on racial and ethnic variation in contraceptive preferences, beliefs, and knowledge together suggest the need for individualized, culturally-responsive contraceptive counseling that allows women Veterans to inform their preferences for specific contraceptive method features with accurate knowledge about those methods.
Another possible contributor to racial and ethnic differences in unintended pregnancy and contraceptive use may be women’s previous interactions with reproductive health services. A study of reproductive aged Black women found that 67% reported one or more instances of discrimination in the family planning or reproductive health care context, and that perceived discrimination was associated with more negative attitudes toward prescription contraception.28 In a second study, 37% of Black respondents reported perceiving race-based pressure from providers to choose a specific contraceptive method.29 Previously published research from the ECUUN study found that more than 1 in 10 minority women reported perceptions of race-based discrimination when receiving care in VA, and that women who reported perceived race-based discrimination were less likely to use prescription contraceptive methods.22 Qualitative data among women Veterans also suggest that Black women are more likely to report perceiving or fearing judgement of their reproductive choices by health care providers, which may hinder their ability to access contraceptive services.30
Clinical & Research Implications.
Despite all women Veteran VA users having the same access to VA reproductive healthcare, our finding on persistent racial and ethnic differences in contraceptive use suggest that access is only one component of the complex and highly personal process of contraceptive decision-making. Implementing patient-centered contraceptive counseling that enables providers and patients to consider a variety of individual experiences and influences on women Veterans’ decision-making may encourage all women Veterans to make informed, preference-concordant contraceptive choices while at the same time supporting VA’s mission to assure health equity for all Veterans. Future research should explore interventions that facilitate provision of high-quality, patient-centered family planning care, with the goal of guiding VA efforts to provide comprehensive reproductive health care that is both gender- and culturally-sensitive.32
Strengths & Limitations.
A few limitations must be considered when interpreting the results of this study. First, we do not have a sufficiently large sample of women who identify as American Indian/Alaska Native, Asian, or Native Hawaiian/Other Pacific Islander to explore differences among these groups. Second, the ECUUN study’s overall response rate is 28%, raising potential concerns about the generalizability of our findings. However, the similarity of participants to non-participants in terms of relevant demographic or clinical characteristics suggests that the ECUUN sample is largely representative of reproductive-aged women Veterans who use VA primary care. Relatedly, our findings cannot be generalized to women Veterans who do not use VA for health care. Compared to women Veteran non-users of VA, VA-users are more likely to be a member of a racial or ethnic minority and to have lower socioeconomic status, lack private medical insurance, and to have worse overall health on all health-related measures.31 Despite these limitations, this study provides new insight into racial and ethnic differences in contraceptive use in a national sample of women Veterans who use VA for primary care.
Conclusions.
Our findings suggest that racial and ethnic differences in both unintended pregnancy and prescription contraceptive use seen in the general US population also exist in this study’s sample of women Veterans. A growing body of research suggests that these differences may be rooted in modifiable deficiencies in care provided to women from racial or ethnic minority groups. These findings highlight the need for provider- and system-level efforts to ensure that all women Veterans have access to equitable, patient-centered contraceptive counseling that addresses knowledge gaps, respectfully considers individual patient experiences and context, and actively connects women to appropriate resources both within and outside of VA.
Condensation:
This nationally representative survey of women Veterans of reproductive age who use VA healthcare identified significant racial and ethnic differences in history of unintended pregnancy and contraceptive use.
AJOG at a Glance:
Why was the study conducted? To improve our understanding of variations in unintended pregnancy and contraceptive use among women Veterans across racial and ethnic groups.
What are the key findings? Women Veterans from racial or ethnic minority groups were more likely than non-Hispanic white women to have ever had an unintended pregnancy in their lifetime and less likely than non-Hispanic white women to have used prescription contraception at last sex.
What does this study add to what is already known? This is the first study to examine whether racial and ethnic differences in contraceptive use patterns and unintended pregnancy exist in the VA, where access to the full range of contraceptive methods is more uniform than in other healthcare settings.
Acknowledgments
Funding: This study was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development (VA Merit Award IIR 12-124, PI: Sonya Borrero). Dr. Deirdre Quinn is supported by a post-doctoral fellowship through the Department of Veterans Affairs (VA) Office of Academic Affiliations and the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System. Dr. Lisa Callegari is supported by a VA Health Services Research and Development Career Development Award (14-412). Colleen Judge-Golden is supported by the National Center For Advancing Translational Sciences of the National Institutes of Health (Award Number TL1TR001858, PI: Wishwa Kapoor).
Footnotes
Publisher's Disclaimer: Disclaimer: The opinions expressed in this work are the authors’ and do not reflect those of the Department of Veterans Affairs, or the U.S. government.
Disclosures: The authors report no competing financial interests.
References
- 1.Office of Disease Prevention and Health Promotion (ODPHP). Family Planning. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/family-planning. Published 2018. Accessed December 11, 2018.
- 2.Mosher WD, Jones J, Abma JC. Intended and Unintended Births in the United States: 1982–2010. Natl Heal Stat Rep. 2012;55(55):1–27. http://www.cdc.gov/nchs/data/nhsr/nhsr055.pdf. [PubMed] [Google Scholar]
- 3.Finer LB, Zolna MR. Declines in intended and unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–852. doi: 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borrero S, Nikolajski C, Steinberg JR, et al. It just happens: A qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception. 2015;91(2):150–156. doi: 10.1016/j.contraception.2014.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aiken ARA, Borrero S, Callegari LS, Dehlendorf C. Rethinking the pregnancy planning paradigm: Unintended conceptions or unrepresentative concepts? Perspect Sex Reprod Heal. 2016;48(3):147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim TY, Dagher RK, Chen J. Racial/Ethnic Differences in Unintended Pregnancy: Evidence from a National Sample of U.S. Women. Am J Prev Med. 2016;50(4):427–435. doi: 10.1016/j.amepre.2015.09.027 [DOI] [PubMed] [Google Scholar]
- 7.Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gynecol. 2010;202(3):214–220. doi: 10.1016/j.ajog.2009.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception. 2016;93(5):406–411. doi: 10.1016/j.contraception.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 9.Rocca CH, Harper CC. Do Racial and Ethnic Differences in Contraceptive Attitudes and Knowledge Explain Disparities In Method Use? Perspect Sex Reprod Health. 2012;44(3):150–158. doi: 10.1363/4415012 [DOI] [PubMed] [Google Scholar]
- 10.Dehlendorf C, Park SY, Emeremni CA, Comer D, Vincett K, Borrero S. Racial/ethnic disparities in contraceptive use: Variation by age and women’s reproductive experiences. Am J Obstet Gynecol. 2014;210(6):526.e1–526.e9. doi: 10.1016/j.ajog.2014.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mosher W, Jones J, Abma J. Nonuse of contraception among women at risk of unintended pregnancy in the United States. Contraception. 2015;92(2):170–176. doi: 10.1016/j.contraception.2015.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniels K, Abma JC. Current Contraceptive Status Among Women Aged 15–49: United States, 2015–2017. NCHS Data Brief. 2018;(327):1–7. https://www.cdc.gov/nchs/data/databriefs/db327_tables-508.pdf#3. [PubMed] [Google Scholar]
- 13.Frost JJ, Singh S, Finer LB. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect Sex Reprod Heal. 2007;39(2):90–99. doi: 10.1363/3909007 [DOI] [PubMed] [Google Scholar]
- 14.Frost JJ, Darroch JE. Factors Associated with Contraceptive Choice and Inconsistent Method Use, United States, 2004. Perspect Sex Reprod Health. 2008;40(2):94–104. doi: 10.1363/4009408 [DOI] [PubMed] [Google Scholar]
- 15.Kavanaugh ML, Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception. 2018;97(1):14–21. doi: 10.1016/j.contraception.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frayne SM, Phibbs CS, Saechao F, et al. Sourcebook: Women Veterans in the Veterans Health Administration. Vol. 4 Washington, DC; 2018. [Google Scholar]
- 17.Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42(5):473–480. doi: 10.1016/j.amepre.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 18.Carter A, Borrero S, Wessel C, et al. Racial and Ethnic Health Care Disparities Among Women in the Veterans Affairs Healthcare System: A Systematic Review. Women’s Heal Issues. 2016. doi: 10.1016/j.whi.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 19.Borrero S, Callegari LS, Zhao X, et al. Unintended Pregnancy and Contraceptive Use Among Women Veterans: The ECUUN Study. J Gen Intern Med. 2017;32(8):900–908. doi: 10.1007/s11606-017-4049-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenfeld E, Callegari LS, Sileanu FE, et al. Racial and ethnic disparities in contraceptive knowledge among women veterans in the ECUUN study. Contraception. 2017;96(1):54–61. doi: 10.1016/j.contraception.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Callegari LS, Zhao X, Schwarz EB, Rosenfeld E, Mor MK, Borrero S. Racial/ethnic differences in contraceptive preferences, beliefs, and self-efficacy among women veterans. Am J Obstet Gynecol. 2017;216(504):e1–10. doi: 10.1016/j.ajog.2016.12.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macdonald S, Hausmann LRM, Sileanu FE, Zhao X, Mor MK, Borrero S. Associations between Perceived Race-based Discrimination and Contraceptive Use among Women Veterans in the ECUUN Study. Med Care. 2017;55(9):S43–S49. doi: 10.1097/MLR.0000000000000746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corp IBM. IBM SPSS Statistics for Macintosh, Version 25.0. 2017. [Google Scholar]
- 24.Hodgson EJ, Collier C, Hayes L, Curry LA, Fraenkel L. Family planning and contraceptive decision-making by economically disadvantaged, African-American women. Contraception. 2013;88(2):289–296. doi: 10.1016/j.contraception.2012.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74(2):125–132. doi: 10.1016/j.contraception.2006.02.010 [DOI] [PubMed] [Google Scholar]
- 26.Craig AD, Dehlendorf C, Borrero S, Harper CC, Rocca CH. Exploring young adults’ contraceptive knowledge and attitudes: Disparities by race/ethnicity and age. Women’s Heal Issues. 2014;24(3):e281–e289. doi: 10.1016/j.whi.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Callegari L, Rosenfeld E, Zhao X, Mor M, Schwarz E, Borrero S. Relationships between contraceptive preferences, knowledge and use among women veterans In: Contraception. Vol 96 Elsevier Inc.; 2017:286–287. doi: 10.1016/j.contraception.2017.07.093 [DOI] [Google Scholar]
- 28.Thorburn S, Bogart LM. African American Women and Family Planning Services: Perceptions of Discrimination. Women Health. 2005;42(1):23–39. doi: 10.1300/J013v42n01_02 [DOI] [PubMed] [Google Scholar]
- 29.Bird ST, Bogart LM. Birth control conspiracy beliefs, perceived discrimination, and contraception among African Americans: an exploratory study. J Health Psychol. 2003;8(2):263–276. http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106546949&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- 30.Callegari LS, Tartaglione E V., Magnusson SL, et al. Understanding Women Veterans’ Family Planning Counseling Experiences and Preferences to Inform Patient-Centered Care. Women’s Heal Issues. 2019;29(3):283–289. doi: 10.1016/j.whi.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 31.Washington DL, Yano EM, Simon B, Sun S. To use or not to use: What influences why women veterans choose VA health care. J Gen Intern Med. 2006;21(SUPPL. 3):11–18. doi: 10.1111/j.1525-1497.2006.00369.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frayne S, Phibbs C, Saecho F, et al. Sourcebook: Women Veterans in the Veterans Health Administration. Vol. 3 Washington DC; 2014. [Google Scholar]


