Abstract
Law and policy differences help explain why, as HIV-related science has advanced swiftly, some countries have realised remarkable progress on AIDS while others see expanding epidemics. We describe the structure and findings of a new dataset and research platform, the HIV Policy Lab, which fills an important knowledge gap by measuring the HIV-related policy environment across 33 indicators and 194 countries over time, with online access and visualisation. Cross-national indicators can be critical tools in international governance—building social power to monitor state behaviour with the potential to change policy and improve domestic accountability. This new and evolving effort collects data about policy through review of legal documents, official government reports and systematic review of secondary sources. Alignment between national policy environments and global norms is demonstrated through comparison with international public health guidance and agreements. We demonstrate substantial variation in the content of law and policies between countries, regions and policy areas. Given progress in basic and implementation science, it would be tempting to believe most countries have adopted policies aligned with global norms, with a few outliers. Data show this is not the case. Globally, alignment is higher on clinical and treatment policies than on prevention, testing and structural policies. Policy-makers, researchers, civil society, finance agencies and others can use these data to better understand the policy environment within and across countries and support reform. Longitudinal analysis enables evaluation of the impact of laws and policies on HIV outcomes and research about the political drivers of policy choice.
Keywords: HIV, health policy, AIDS, tuberculosis
Summary box.
Data can be generated to measure and visualise national HIV-related law and policy environments for most countries in the world, enabling comparative analysis across countries and against international scientific and human rights norms.
Significant variation exists in the content of HIV-related laws and policies between countries, regions and policy areas—with substantial gaps between national policy environments and global norms.
Globally, alignment is higher on clinical and treatment policies than on prevention, testing and structural policy areas.
Monitoring state behaviour by tracking and comparing HIV-related policies could be used to increase accountability, address structural barriers and better understand why some countries have seen rapid reductions in AIDS deaths and new HIV infections while others see flat or growing epidemics.
Introduction
In recent years, the science of ending AIDS has advanced rapidly—demonstrating effective biomedical and structural interventions. Evidence on treatment as prevention, pre-exposure prophylaxis (PrEP), newer antiretroviral medicines and many other examples have rapidly changed what constitutes the best practices.1–4 Research has also shown how best to deliver interventions—differentiating service delivery, making self-testing available, eliminating criminalisation of key populations.5–8 Despite the progress of science, however, the global AIDS response is not on track to reach globally agreed targets.9 This can be understood, in part, through the gap between science and policy, which remains significant in many contexts.
Governments bring their understanding of best practices to scale through law and policy-making. Scholars have described the ‘legal determinants’ of health and the ‘triangle of rules’ that define health systems.10 11 In the global AIDS response, a wide range of mechanisms have been created to disseminate scientific information and support translation into laws and policies, including technical guidance from UNAIDS and the WHO and funding for implementation through mechanisms like the Global Fund to Fight AIDS, tuberculosis (TB) and Malaria. Nonetheless, data described below show substantial policy differences persist between countries. A small but growing literature in legal epidemiology shows an empirical link between laws and policies and health outcomes.12 For example, eliminating parental consent policies has been linked to increased rates of HIV testing.13 Countries where sex work is not criminalised have significantly lower HIV prevalence among sex workers.14 Medical, mining and criminal policies have been linked to TB rates.15 And countries with a constitutional right to health have better health outcomes than those without.16 Studies have also explored the drivers of HIV policy choice. The degree of ethnic cleavages and time leaders expect to be in power have both been shown to drive policy choice in countries.17 18 Existing research on the impact of policy represent only a small fraction of HIV-related policies for which we might expect variation to matter—from which antiretrovirals are used and whether PrEP is available to people facing HIV risk to rights protections and policies around human resources for health. Despite the centrality of policy environments to HIV outcomes, there is no global, longitudinal dataset that comprehensively measures variations in HIV laws/policies across countries.
The ability to monitor state behaviour has become a critical tool in international governance.19 Understanding policy choices in other countries reveals private information that can help governments make better informed decisions.20 Indicators that provide for comparison between states also constitutes an exercise of ‘social power’, with the potential to change important policies and increase the ability of domestic actors to hold leaders accountable to international standards.21 22
We describe a new dataset, index and research/advocacy platform which fills this information gap by rigorously tracking HIV policies adopted at the country level longitudinally. A public dataset and visualisation tool, the HIV Policy Lab, are available online at www.hivpolicylab.org and track 33 key indicators of HIV-related law and policy across 194 countries over multiple years. Policies are benchmarked against global norms and classified by alignment to these norms. Here, we describe the tool and initial findings about the substantial degree of variation in HIV-related policies between countries, surprising after decades of policy dissemination efforts. Researchers, civil society, policy-makers, funders and national and international officials can use this dataset to better understand the policy environment and as a tool for law and policy reform. There are also important unanswered questions about the impact of policies and how policies work differently in different contexts. What works in a randomised controlled trial often cannot be simply translated into national-level policy.23
Building data on HIV policies
The HIV Policy Lab dataset quantitatively represents the HIV-related law and policy environment in a given country, enabling policy actors and researchers to compare across countries. We draw on the methods of policy surveillance—the systematic, scientific collection and analysis of laws of public health significance over time24 25—bringing it into a cross-national comparative context. A variety of qualitative methods including development of coding rules, comparative legal interpretation, policy analysis and content analysis are deployed in constructing the dataset.26–28
We conducted a broad survey of the hundreds of policy topics related to HIV, then narrowed these to a set of key indicators reflecting the scope of the broader HIV policy environment. Building from both theory and good practice, we chose indicators to be valid and meaningful to end users, sensitive and specific to the underlying phenomenon being measured, easily interpreted and which allowed international comparison as well as consistency over time.29 An extensive consultation process included review of international normative guidance and subject-specific, cross-sectoral focus groups with clinicians, social and biomedical scientists, national policy-makers, international organisations, financing agencies, communities of people living with HIV and other civil society groups. Based on the outcomes of those consultations, we identified 33 indicators of the HIV policy environment, 16 of which have subindicators, across four areas: treatment, testing and prevention, structural and health systems policies. For each of the indicators, a coding schema was developed to translate information about the content of the laws and policies into data,30 as summarised in table 1.
Table 1.
HIV policy indicators
| Indicator number | Name | Coding question |
| Clinical/treatment: policies related to HIV treatment and clinical services | ||
| CT1 | Treatment Initiation | Do national guidelines on when to initiate HIV treatment align with international recommendations? |
| CT2 | Same-day treatment start | Do national HIV treatment guidelines offer the possibility to start antiretrovial therapy (ART) the same day as HIV diagnosis? |
| CT3 | Treatment regimen | Does the first-line antiretrovial (ARV) regimen included in national HIV treatment guidelines align with international recommendations? |
| CT4 | Differentiated service delivery | Do national HIV guidelines incorporate differentiated service delivery for stable patients? |
| CT5 | Viral load testing | Do national guidelines on frequency of viral load monitoring align with international recommendations? |
| CT6 | Paediatric diagnosis and treatment | Do national guidelines for paediatric testing and treatment align with international recommendations? |
| CT7 | Migrant access to healthcare | Do national laws/policies allow all migrants access to HIV and primary healthcare services, regardless of their immigration status? |
| CT8 | TB diagnosis | Does national policy include use of rapid diagnostic tests (eg, rapid molecular tests, lateral flow urine lipoarabinomannan assay (LF-LAM)) as the initial diagnostic test for TB in “People Living With HIV/AIDS” (PLHIV)? |
| Testing/prevention: policies related to HIV testing, biomedical and sociobehavioural HIV prevention | ||
| TP1 | Self-testing | Does national law/policy allow for self-testing? |
| TP2 | Index testing w/ protections | Do national HIV guidelines incorporate index testing/partner notification, while prioritising robust protections for patient confidentiality? |
| TP3 | Compulsory testing | Does national law/policy prohibit compulsory HIV testing? |
| TP4 | Age restrictions on testing and treatment | Can adolescents access HIV testing and treatment without parental consent? |
| TP5 | PrEP | Does national policy make pre-exposure prophylaxis (PrEP) available to eligible populations in accordance with WHO guidelines? |
| TP6 | Harm reduction | Does national/law policy incorporate key harm reduction strategies? |
| TP7 | Comprehensive sexuality education | Does national policy require that comprehensive sexuality education be taught in primary and secondary schools? |
| TP8 | Prisoners prevention | Are both condoms/lubricants and needle/syringe programmes available to prisoners as a matter of policy? |
| Structural: policies related to structural-legal drivers of HIV | ||
| S1 | Same-sex criminalisation | Are consensual same-sex sexual acts decriminalised in law? |
| S2 | Sex work criminalisation | Is sex work decriminalised under national law? |
| S3 | Drug use criminalisation | Is personal drug possession/use decriminalised? |
| S4 | HIV exposure criminalisation | Does national law avoid criminalising and prosecuting people for HIV exposure/ transmission? |
| S5 | Non-discrimination protections | Do national/laws policies include protections from discrimination on the basis of sexual orientation, gender identity, and HIV status? |
| S6 | National human rights institutions | Is there an independent national human rights institution to which violations can be reported in compliance with the Paris principles? |
| S7 | Constitutional right to health | Is there an enforceable right to health in the national constitution? |
| S8 | Girls education | Is there a national policy in place to encourage secondary school retention among girls? |
| S9 | Gender-based violence | Does the law explicitly address domestic violence with enforceable penalties? |
| S10 | Civil society | Does national law/policy facilitate open participation by civil society in the AIDS response? |
| Health systems: policies related to financing and management of the health system | ||
| HS1 | Task shifting | Does national law/policy allow for nurses or other non-physicians to initiate HIV treatment? |
| HS2 | Health financing | Does national law/policy prioritise sustainable financing for the public health system? |
| HS3 | Universal health coverage (UHC) | Does the national universal health insurance scheme include medications for HIV treatment and PrEP? |
| HS4 | User fees | Are public healthcare services available without user fees at the point of service? |
| HS5 | Access to medicines | Does national law/policy take advantage of ‘TRIPS flexibilities’ for affordable medicines (ie, compulsory licensing/public non-commercial use, parallel import, and Least Developed Country transition provisions)? |
| HS6 | Unique identifiers w/ data protections | Does country have unique identifiers for continuity of care across multiple facilities while protecting patients' privacy? |
| HS7 | Data sharing | Is it country policy to publicly share disaggregated HIV data on a regular basis? |
TB, tuberculosis.
Data on national policies is generated via three approaches. First, we gathered a large number of primary sources (ie, national laws and policy documents) through academic, civil society, and international organisation networks, as well as internet searches. The text of laws and policies was coded using a ‘directed content analysis’ approach and a dual-coder strategy with tests for intercoder reliability, using native speakers as the primary coder for the majority of texts.24 27 31 Second, information formally submitted by governments to UNAIDS and the WHO through the Global AIDS Monitoring (GAM) framework were also coded.32 Information from the GAM National Commitments and Policy Instrument questionnaire is shared publicly33 and include information from governments every 2 years, with partial answers in interim years, and information from local civil society and non-governmental organisations on a set of complementary policy issues. This information is validated for internal consistency and completeness by UNAIDS and WHO—with illogical responses corrected, countries contacted in cases of missing data, and validation against primary sources for selected laws and policies.
We also conducted a meta-analysis of other published sources of information about policies in the public sphere, including United Nations, nongovernmental organisation (NGO) and academic sources. We selected authoritative data sources recommended by academic, international organisation, and civil society experts, allowing for a better understanding of the legal landscape. For example, data on criminalisation are collected by the HIV Justice Network and Global Network of Sex Work Projects, data on laws towards lesbian, gay, bisexual, transgender and intersex (LGBTI) communities from the International Lesbian, Gay, Bisexual, Trans and Intersex Association, information on the use of intellectual property flexibilities from the Medicines Law & Policy database, and data on PrEP from PrEP Watch. The PEPFAR Sustainability Index Dashboard incorporated assessment from US government staff on key policy issues. A full list of sources and citations are listed as online supplemental appendix A. Finally, these sources were augmented with an expert survey distributed to leaders from international organisations, civil society, and clinical, donor, and government institutions to collect information where data were not publicly accessible. By collecting and coding data from multiple sources, it is possible to triangulate information, include the most up-to-date data available.
bmjgh-2020-003695supp001.pdf (67.8KB, pdf)
We focus on the content of the law and policy in a country—not on how, or to what degree, that policy has been implemented. Policy as written has been described as a distinct ‘triangle’ from implementation in health systems10—and separating them enables both creation of comparable data and the opportunity to assess where implementation issues (instead of policy) may explain outcomes.
Each policy indicator is benchmarked against international normative instruments including guidance from UNAIDS, the WHO, and international rights agreements (collectively referred to below as global norms). For example, on when to start antiretroviral treatment, policies were coded and compared with WHO guidance,34 while on issues of criminalisation policies were compared with the Global Commission on HIV and the Law.35 The full set of indicators is listed in table 1 and a full set of coding rules are described in online supplemental appendix B. The process of developing indicators of governance and policy compared with global norms is highly contested.36 With this in mind, the questions were crafted so that data both show alignment with global norms and provides empirical information to study if and how policies are linked to health outcomes.
bmjgh-2020-003695supp002.pdf (98.3KB, pdf)
For each indicator, a coding question and coding rule were developed about the content of a country’s policies27—intended to provide a specific, measurable indicator. Each policy indicator was coded on a binary scale of 0 or 1. For example, national policy same-day initiation of HIV treatment options were no (0) or yes (1). Some questions allowed for a ‘partial’ code of 0.5—used for complex indicators including some composed of two or three subindicators. Sex work, for example, might be coded fully criminalised (0), partial when buying and selling sex are not criminalised but organising sex work is, and not criminalised (1) where all three elements are not (1). On PrEP, meanwhile, the two-part indicator includes approval of antiretrovirals for prophylactic use and whether those at substantial risk are eligible—with a partial score given if only one subindicator is adopted. All indicators are weighted equally. While it is likely that some policies are more important than others, we currently lack empirical evidence as to which matter more, with these data meant to enable research on this question. Therefore, the scores are best interpreted as individual country/year observations and a count of the policies aligned with global norms and not as a weighted model of the policy environment.
A custom data architecture with corresponding ontology and taxonomy was developed to capture these data and support integration, comparison, and analysis with longitudinal epidemiological data. All data sources are documented, including update frequency.
To visualise the overall law and policy environment, and for the four policy areas, a continuous scoring metric is created. For all indicators for which there are data, the total of adopted and partially adopted is divided by the number of indicators scored, then multiplied by 100 to create the continuous policy area score. Only countries that had data collected on at least one-third of all indicators for the policy area are included. This scoring metric is reflected in a qualitative assignment by quintile based on how aligned each country’s policy environment is with global norms. The result is longitudinal data with country-year observations which can be rolled up into composite measures of the HIV policy environment and visualised.
Mapping and comparing HIV policies
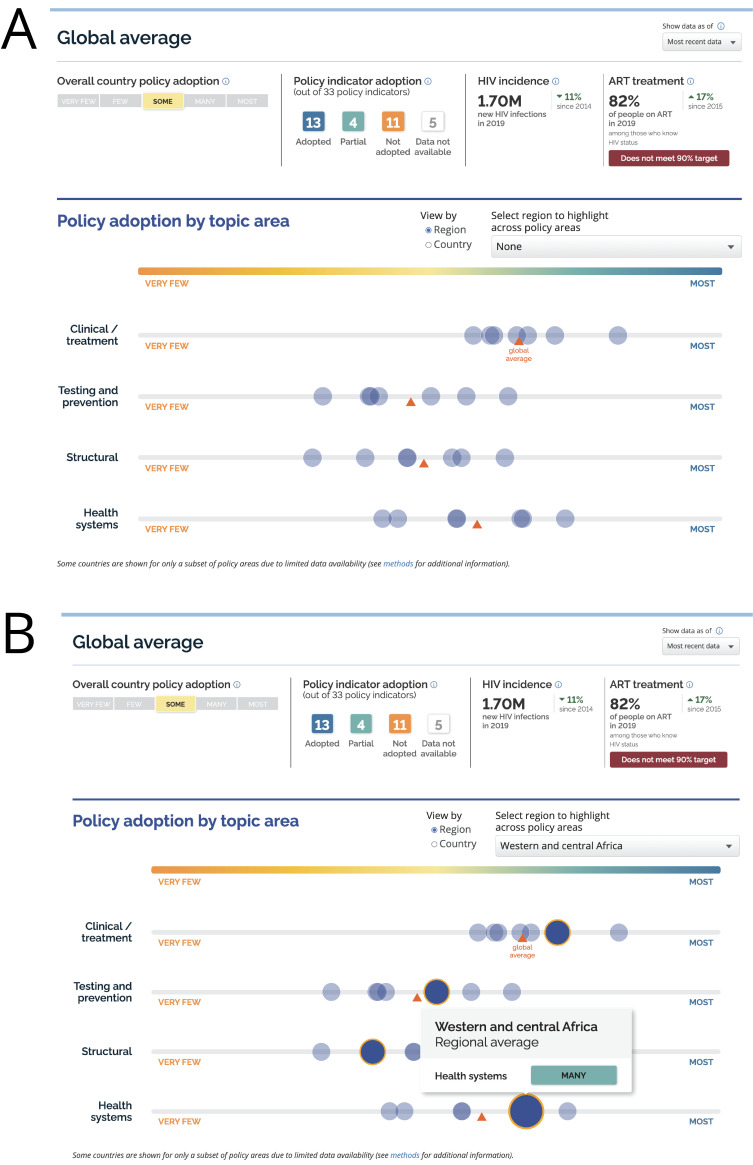
As shown in figure 1A, we collated polices by country to allow comparative analysis of the policy environment. Data have been collected and integrated starting in 2017 and can be explored by year, by policy area, and by indicator to better understand the distribution of policies globally.
Figure 1.
HIV policies adopted by country (most recent available data).
Overall the data show that, even with significant efforts to support evidence-based policy-making, there remains a significant gap between international norms and national policies. There is also very significant variation in the content of law and policies, and the degree to which the align with international norms, between countries and across policy areas.
For example, as shown in figure 1B, C, the majority of countries have aligned their policies in the clinical and treatment area with global norms. Notable data exceptions include areas in the Middle East and Northern Africa. By contrast, many more countries having adopted only a few of the policies aligned with global norms in the testing and prevention area.
Figure 2A illustrates the global and regional average for policy adoption, with each blue circle representing a region oriented along the qualitative indicator of progress. Globally, scores are highest on average for the clinical and treatment policy area and lowest for testing and prevention. As shown in figure 2, each region can be highlighted to show relative progress across each policy area. Figure 2B, for example, shows that countries in the West & Central African region have HIV clinical/treatment policies which are more closely aligned with international norms than the global average; however, their structural polices (eg, criminalisation, gender and human rights) are less aligned with global norms than average.
Figure 2.
Average HIV-related policy adoption.
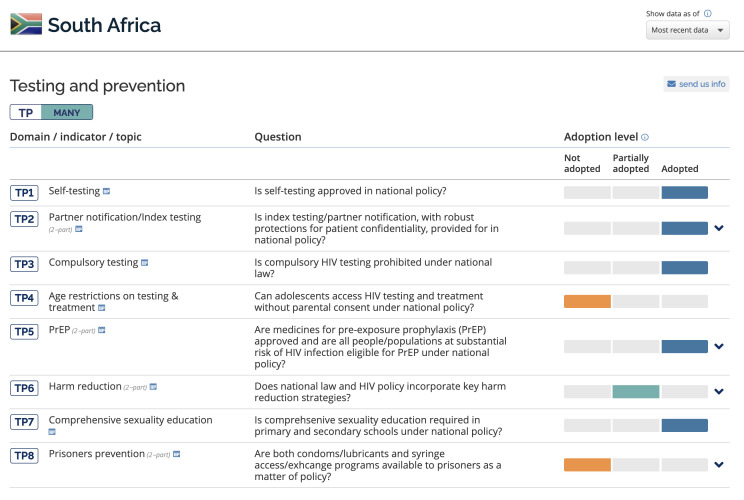
The HIV Policy Lab site provides access to the coding rules and underlying basis for each indicator score available at a country level along with sources for each answer, including underlying legal documents. Figure 3 and figure 4 shows South Africa’s HIV-related policy environment visualised and compared with other countries. As shown in figure 3A on the South African detail on the global map, South Africa has aligned most of the policies in our dataset with global normative advice. In particular, the country’s clinical/treatment and health systems policies largely align with global norms, with testing and structural policies less aligned, but still reflect a high level of adoption of global best practices. For each country, progress towards meeting key targets for HIV incidence rates and ART treatment are included to provide context highlighting the importance of policy choice.
Figure 3.
South Africa HIV-related policies.
Figure 4.
Country score card: testing and prevention policies in South Africa.
The dataset is publicly available and public participation is encouraged—with data gaps highlighted and users invited to contribute updated data and documents. Critical for any research resource, all data on the site are available for search, filter and download. Additionally, users are able to access the detailed codebook to allow deeper analysis.
Translating policy data into action
Despite remarkable progress, the world is significantly off track from UN-agreed HIV goals.9 Policy plays an important role. New HIV infections have fallen by 38% in eastern and southern Africa between 2010 and 2019, for example, compared with a remarkable 72% increase in eastern Europe and central Asia.9 As shown in figure 1C, many countries in eastern and southern Africa have aligned many or most of their policies on prevention with global norms while quite a few countries in eastern Europe and central Asia have not.
Significant policy reform remains important in HIV. After decades of the global AIDS response and scientific advance, it would be tempting to believe that most countries have adopted the ‘right’ policies, with a few outliers. Our data show that this is not the case. Significant work is needed to improve the HIV-related policy environment in countries across the world.
These data highlight situations where national policies may be aligned with normative guidance, yet HIV outcomes remain poor—opening opportunities to explore how policy is implemented and financed, and whether policies operate as expected, particularly when transferred from international bodies to diverse local communities. HIV funding can have greater impact where policy environments are supportive. Financing agencies like the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund could better consider the policy environment when making grants, set targets for countries to improve, and fund advocacy and policy reform efforts.
One notable positive is the alignment of many countries on clinical policies. The WHO, UNAIDS and PEPFAR have put significant effort into supporting policy reform in this area (explicit guidance, funding national-level guidelines development and implementation training) with important results. We can learn from this to inform broader policy change.
An important next step will be national consultations with civil society, communities living with and affected by HIV, and policy-makers to support the use of the Policy Lab as a tool for advocacy and to drive policy implementation where needed. Data can bring transparency and make it obvious where some countries have not enacted science-based policies. Comparisons with neighbouring countries can be a powerful political motivator. Ordinal and categorical rankings are possible—but require further theoretical and empirical work to address concerns about validity from similar efforts.37 Policy, however, often changes only after concerted and strategic advocacy.38 Differentiated service delivery has often been adopted at the behest of people living with HIV; PrEP polices have changed when young women or gay men have demanded access. Engagement of activists and public health leaders is a necessary ingredient for these data to have impact.
Conclusion
Policy surveillance through the HIV Policy Lab offers a new way to understand, explore and explicitly compare the HIV-related law and policy environments of countries around the world—transforming policies into data and tracking them over time. The tool provides access to critical new data and an evidence basis to study what policies work, where and under what conditions. Many countries are currently significantly off track in global goals to end AIDS as a public health threat by 2030 and policy is one reason. Obvious correlations can be seen in our visualisations between policy and progress against AIDS. Deeper empirical work is needed, though, to understand how the policy environment is helping or hindering the AIDS response. Having a more robust understanding of which policies are having the most impact, for good or ill, would help focus and prioritise the global effort to mobilise political will. This dataset provides the raw material to enable this sort of cross-national analysis with longitudinal, country-level observations across most countries in the world. Enacting HIV-related policy is, in and of itself, an intervention—and on issues ranging from antiretroviral treatment protocols to HIV self-testing to criminalisation and imposition of user fees at the point of care it can and should be rigorously evaluated.
Making law and policy transparent gives policy-makers important information about what their neighbours are doing to fight AIDS. It helps people and organisations to hold national leaders accountable to international standards. Measurement is only the first step, however. Engaging with activists and policy-makers to support policy reform and progress over the medium term is necessary for impact. Where measurement, transparency and advocacy, many more lives can be saved and HIV infections averted in this time of scarce resources and complex global politics.
Footnotes
Handling editor: Seye Abimbola
Twitter: @MMKavanagh, @mplngr
Contributors: Empirical work was conceptualised by all authors. MK, RS, and EG drafted the paper. All authors edited and approved submitted version. MP and SE led data collection and structuring. VB and TE led work on NCPI survey which makes up part of the data.
Funding: This study was funded by United States Agency for International Development.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Mugo NR, Ngure K, Kiragu M, et al. Prep for Africa: what we have learnt and what is needed to move to program implementation. Curr Opin HIV AIDS 2016;11:80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyrer C, Birx DL, Bekker L-G, et al. The Vancouver consensus: antiretroviral medicines, medical evidence, and political will. Lancet 2015;386:505–7. 10.1016/S0140-6736(15)61458-1 [DOI] [PubMed] [Google Scholar]
- 3.Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med 2015;372:509–18. 10.1056/NEJMoa1402269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV, 2018. Available: http://www.who.int/hiv/pub/guidelines/ARV2018update/en/ [Accessed 10 Aug 2020].
- 5.El-Sadr WM, Harripersaud K, Rabkin M. Reaching global HIV/AIDS goals: What got us here, won't get us there. PLoS Med 2017;14:e1002421. 10.1371/journal.pmed.1002421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimsrud A, Bygrave H, Doherty M, et al. Reimagining HIV service delivery: the role of differentiated care from prevention to suppression. J Int AIDS Soc 2016;19:21484. 10.7448/IAS.19.1.21484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makofane K, Beck J, Lubensky M, et al. Homophobic legislation and its impact on human security. African Security Review 2014;23:186–95. 10.1080/10246029.2014.913832 [DOI] [Google Scholar]
- 8.Njau B, Covin C, Lisasi E, et al. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health 2019;19:1289. 10.1186/s12889-019-7685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNAIDS 2020 global AIDS update: seizing the moment. Geneva: UNAIDS, 2020. https://www.unaids.org/en/resources/documents/2020/global-aids-report [Google Scholar]
- 10.Abimbola S. Health system governance: a triangle of rules. BMJ Glob Health 2020;5:e003598. 10.1136/bmjgh-2020-003598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gostin LO, Monahan JT, Kaldor J, et al. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet 2019;393:1857–910. 10.1016/S0140-6736(19)30233-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramanathan T, Hulkower R, Holbrook J, et al. Legal epidemiology: the science of law. J Law Med Ethics 2017;45:69–72. 10.1177/1073110517703329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kranzer K, Meghji J, Bandason T, et al. Barriers to provider-initiated testing and counselling for children in a high HIV prevalence setting: a mixed methods study. PLoS Med 2014;11:e1001649. 10.1371/journal.pmed.1001649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reeves A, Steele S, Stuckler D, et al. National sex work policy and HIV prevalence among sex workers: an ecological regression analysis of 27 European countries. Lancet HIV 2017;4:e134–40. 10.1016/S2352-3018(16)30217-X [DOI] [PubMed] [Google Scholar]
- 15.Basu S, Stuckler D, McKee M. Addressing institutional amplifiers in the dynamics and control of tuberculosis epidemics. Am J Trop Med Hyg 2011;84:30–7. 10.4269/ajtmh.2011.10-0472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kavanagh MM. The right to health: institutional effects of constitutional provisions on health outcomes. Stud Comp Int Dev 2016;51:328–64. 10.1007/s12116-015-9189-z [DOI] [Google Scholar]
- 17.Lieberman ES. Boundaries of contagion: how ethnic politics have shaped government responses to AIDS. Princeton University Press, 2009. [Google Scholar]
- 18.Dionne KY. The role of executive time horizons in state response to AIDS in Africa. Comparative Political Studies, 2010. [Google Scholar]
- 19.Kelley JG, Simmons BA. Politics by number: indicators as social pressure in international relations. Am J Pol Sci 2015;59:55–70. 10.1111/ajps.12119 [DOI] [Google Scholar]
- 20.Dobbin F, Simmons B, Garrett G. The global diffusion of public policies: social construction, coercion, competition, or learning? Annu Rev Sociol 2007;33:449–72. 10.1146/annurev.soc.33.090106.142507 [DOI] [Google Scholar]
- 21.Honig D, Weaver C. A race to the top? the aid transparency index and the social power of global performance indicators. Int Organ 2019;73:579–610. 10.1017/S0020818319000122 [DOI] [Google Scholar]
- 22.Dai X. International institutions and national policies. Cambridge University Press, 2007. [Google Scholar]
- 23.Smith K. Beyond evidence based policy in public health: the interplay of ideas. Springer, 2013. [Google Scholar]
- 24.Burris S, Hitchcock L, Ibrahim J, et al. Policy surveillance: a vital public health practice comes of age. J Health Polit Policy Law 2016;41:1151–73. 10.1215/03616878-3665931 [DOI] [PubMed] [Google Scholar]
- 25.Marks-Sultan G, Tsai F-J, Anderson E, et al. National public health law: a role for who in capacity-building and promoting transparency. Bull World Health Organ 2016;94:534–9. 10.2471/BLT.15.164749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Melton J, Elkins Z, Ginsburg T, et al. On the Interpretability of law: lessons from the decoding of national Constitutions. Br J Polit Sci 2013;43:399–423. 10.1017/S0007123412000361 [DOI] [Google Scholar]
- 27.Prior L. Content analysis. The Oxford Handbook of qualitative research, 2014: 359–79. [Google Scholar]
- 28.Nelken D. Comparative legal research and legal culture: facts, approaches, and values. Annu Rev Law Soc Sci 2016;12:45–62. 10.1146/annurev-lawsocsci-110615-084950 [DOI] [Google Scholar]
- 29.Brown D. Good practice guidelines for indicator development and reporting : Third World forum on statistics: knowledge and policy. Busan, Korea, 2009: 27–30. [Google Scholar]
- 30.Saldaña J. Coding and analysis strategies In: The Oxford Handbook of qualitative research, 2014. [Google Scholar]
- 31.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 32.UNAIDS Global AIDS monitoring 2020 — indicators for monitoring the 2016 political Declaration on ending AIDS, 2019. Available: https://www.unaids.org/en/resources/documents/2019/Global-AIDS-Monitoring [Accessed 18 Jul 2020].
- 33.UNAIDS Laws and policies analytics. Available: http://lawsandpolicies.unaids.org/ [Accessed 11 Aug 2020].
- 34.World Health Organization (WHO) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2nd Ed Geneva: WHO, 2016. [PubMed] [Google Scholar]
- 35.Global Commission on HIV and the Law Report: Risks, Rights & Health, 2012. Available: http://www.hivlawcommission.org/index.php/report [Accessed 28 May 2013].
- 36.Apaza CR. Measuring governance and corruption through the worldwide governance indicators: Critiques, responses, and ongoing scholarly discussion. Political Science and Politics, 2009: 139–43. [Google Scholar]
- 37.Razavi A, Erondu N, Okereke E. The global health security index: what value does it add? BMJ Glob Health 2020;5:e002477. 10.1136/bmjgh-2020-002477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russell A, Luba M, Mwehonge K, et al. Civil society demand for accountability to achieve the 90-90-90 targets: lessons from eastern and southern Africa. Curr Opin HIV AIDS 2019;14:41–5. 10.1097/COH.0000000000000516 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-003695supp001.pdf (67.8KB, pdf)
bmjgh-2020-003695supp002.pdf (98.3KB, pdf)