Abstract
Flexor hallucis longus tendon release for surgical treatment of functional hallux limitus–associated conditions is described. This release is obtained by arthroscopic correction of the tendon's blockage, which is located at the retrotalar pulley. The procedure restores the ability for dorsiflexion of the first toe in ankle dorsiflexion (positive stretch test result). Such movement was not possible before, causing a modified gait pattern and affecting the biomechanics of the foot and leg. This explains why the procedure creates favorable changes concerning foot dynamics by restoration not only of the normal tendon glide but also of the normal mobility of the subtalar joint.
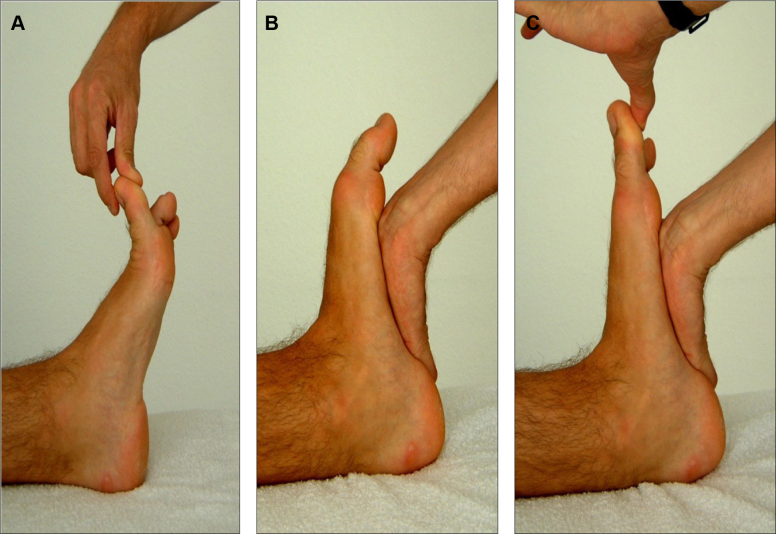
Flexor hallucis longus (FHL) tendon release for surgical treatment of functional hallux limitus–associated conditions1 is described in this technical note. The diagnostic test of functional hallux limitus is called the “stretch test” (Fig 1). A positive test result identifies the tendon's blockage, which is located at the retrotalar pulley2,3 (Fig 2).
Fig 1.
Flexor hallucis longus stretch test. The patient is in the prone position. (A) Sagittal clinical view of medial side of left ankle and foot. The ankle is in plantar flexion. Full range of motion of the first metatarsophalangeal joint is verified. (B) The ankle is maintained in dorsiflexion by applying pressure at the metatarsal heads. (C) When the ankle is forced into passive dorsiflexion and there is an inability to dorsiflex the first metatarsophalangeal joint, the test result is positive.
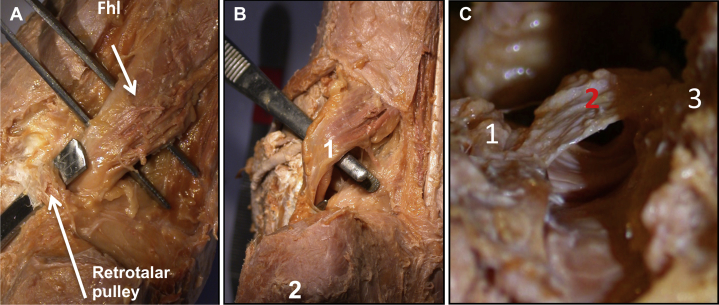
Fig 2.
Anatomic location of impingement in retrotalar tunnel. An anatomic sample of the right foot in the prone position is shown from a sagittal view. (A) Posterior view of flexor hallucis longus (FHL) muscle and tendon with pulley. (B) Posterior view of FHL muscle and tendon without pulley. (1, FHL tendon; 2, calcaneus.) (C) Retrotalar tunnel with pulley visualized from below (FHL tendon removed). (1, posterior medial tubercle; 2, retrotalar pulley; 3, posterior lateral tubercle.)
To relieve this impingement, we use the technique described in this article. It restores the ability for dorsiflexion of the first toe in ankle dorsiflexion. Because this movement was not possible before, it caused a modified gait pattern and affected the biomechanics of the foot and leg.4, 5, 6, 7 This explains why the procedure creates favorable changes concerning foot dynamics by restoration not only of the normal tendon glide but also of the normal mobility of the subtalar joint.3 Our minimally invasive approach was tested on more than 700 feet and allows for early mobilization with minor complications.8
Surgical Technique
Surgery is performed with the patient in the prone position under general or epidural anesthesia by 1 surgeon and 1 assistant. The feet should extend just beyond the operating table, and the operative foot is elevated slightly. Standard arthroscopic equipment is used, including low-pressure, low-flow pump systems and a Synergy 5.5-mm endoscope (Arthrex, Naples, FL) with a 30° angle.
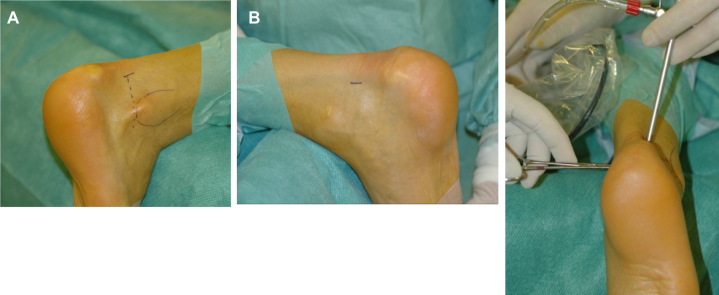
We work with a classic 2-portal endoscopic approach: 1 posterolateral portal for the camera and 1 posteromedial portal for the instruments9,10 (Fig 3). Performing dissection using the ArthroCare Super Turbovac 90 wand handpiece (Smith & Nephew Endoscopy, Andover, MA), we visualize the posterolateral tubercle of the talus and the subtalar joint. Then, starting from a central position, we move upward, medial, and anterior against the medial talar wall, until the first fibers of the pulley are identified by their pearly color. When the pulley is moved forward, the FHL tendon can be seen and its inability to glide properly can be assessed.
Fig 3.
Classic 2-portal endoscopic approach. The patient is in the prone position, and the right foot is exposed. (A) Creation of posterolateral portal at level of tip of lateral malleolus, just lateral to Achilles tendon. Following the initial 0.5-cm skin incision, a mosquito clamp is used to split the subcutaneous tissue in a way that prevents injury to the adjacent sural nerve branches. The clamp should be directed toward the interdigital space between the first 2 toes. The bone surface is palpated with the tip of the clamp, which is subsequently removed and replaced by the scope obturator in the same direction. (B, C) The posteromedial portal is created at the mid distance between the medial malleolus and the Achilles tendon border. Following the skin incision, a mosquito clamp is introduced and directed toward the obturator and forward to the Achilles tendon. When the mosquito clamp touches the shaft of the obturator, it has to be opened to create a space at the posterior aspect of the talus that is needed for the outflow.
Good visualization is mandatory but is sometimes difficult to achieve. Fluoroscopy can help to visualize the subtalar joint in difficult cases, especially when the posterolateral tubercle is prominent. A single sagittal view with the probe in contact with bone is enough to obtain the landmarks. Dissection is guided by the talar wall and has to start from lateral to medial to minimize the risk of neurovascular lesions. The ArthroCare device has to be continuously in contact with the bone. To assess nerve stimulation, the assistant holds the foot on its plantar surface.
Resection of the pulley is achieved using the ArthroCare device, directing it from anterior to posterior and from upward to downward. This release concerns only the retrotalar pulley and not the retinaculum of the calcaneal tunnel.
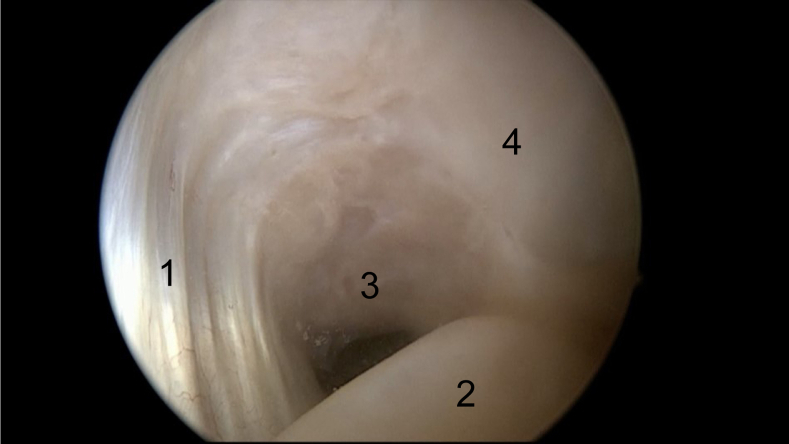
The restoration of the normal tendon glide is then assessed clinically while dorsiflexing the great toe in ankle dorsiflexion. Surgically, the result of the release can be assessed by pulling the tendon backward with the probe. This manipulation allows visualization of the tunnel in front of the tendon and the space created by the release (Fig 4). Synovial remnants situated at the lower part of the retrotalar tunnel are excised if deemed necessary. In case of a posterior bony overgrowth adding to the conflict by limitation of the tendon glide or the presence of an os trigonum, resection using the Synergy Shaver handpiece (Arthrex) with a 3.8-mm blade might follow to a certain degree depending on the preoperative clinical and imaging assessment. Finally, the subtalar joint is examined for normal and unrestricted motion.
Fig 4.
Visualization of retrotalar space: arthroscopic superior-inferior view of medial side of ankle. The patient is in the prone position during the intervention. Assessment of the space created by resection of the pulley is performed, and the possible need to excise synovial remnants or bony overgrowth to maximize the space is evaluated. (1, retrotalar pulley; 2, flexor hallucis longus tendon; 3, retrotalar tunnel; 4, talus.)
A distal location of the musculotendinous junction or a hypertrophic muscular belly predisposes to impingement in the tunnel and needs special care. Therefore, in some cases, it is not sufficient to release the pulley to obtain a free glide of the tendon. If a bony bump at the medial side of the posterolateral tubercle prevents the glide of the muscle backward, bony resection is mandatory. The arthroscopic view will then confirm the improvement in the tendon glide. This anatomic condition was present in 25% of cases in our series.4
After completion of the procedure, the portals are closed with sutures. Special care is needed to avoid incorporating the nervous branches in the sutures. Finally, a compression dressing is applied around the ankle joint.
Table 1 summarizes the pearls and pitfalls of this procedure, and Table 2 outlines its advantages and disadvantages. Video 1 shows and explains the whole intervention.
Table 1.
Pearls and Pitfalls
| The surgeon should ensure a good outflow. |
| Radiologic landmarks can be obtained by fluoroscopy if necessary. |
| Dissection should be carried out step by step in contact with bone. |
| The surgeon should work laterally to the FHL tendon (the nerve bundle is medial). |
| Nerve stimulation is checked by holding the foot (assistant). |
| The surgeon should ensure that the pulley is completely released (lower part). |
| The surgeon should check whether a bony bump is involved in impingement; excessive resection should be avoided. |
| The skin must be sutured very carefully to preserve the nerve branches. |
NOTE. A summary of essential information based on experience or observation is provided. The items listed are helpful to deal with problems that could be encountered while carrying out the described arthroscopic technique and to be aware of its risk-benefit balance.
FHL, flexor hallucis longus.
Table 2.
Advantages and Disadvantages
| The procedure has a short duration and there is no need of a tourniquet. |
| Since the biomechanical chain of the lower limb is restored, the benefits are not limited to the operative area alone. |
| The procedure allows quick rehabilitation of patients, notably athletes. |
| There is a minimal risk of complications and residual pain. |
| An experienced surgeon is needed to limit complications and to carry out an efficient arthroscopic intervention. |
NOTE. A summary of essential information based on experience or observation is provided. The items listed are helpful to deal with problems that could be encountered while carrying out the described arthroscopic technique and to be aware of its risk-benefit balance.
Discussion
Our minimally invasive approach entails a minimal tissue detachment and a focused and limited dissection of the hindfoot anatomic area, thus minimizing the potential complications that could arise. The most common complication is nerve injury to the sural and saphenous nerves. This can lead to neuroma formation, requiring a subsequent intervention.8 Another complication can be deep or superficial wound infection; treatment is conducted nonoperatively.11, 12, 13
Tissue attachments are preserved, and bony resection is as minimized as possible. Therefore, we use repetitive controls of the tendon's ability to glide. Excessive resection could lead to muscle weakness or a fracture of the lateral rim.14
However, this procedure's safety is easily warranted if the surgical steps are thoroughly followed, and the overall complication rate is very low.11, 12, 13, 14 Furthermore, this technique provides a good alternative to the already existing open surgical approaches for FHL release and represents the first technique described to address the issue of FHL conflict during its passage through the retrotalar tunnel.15, 16, 17, 18, 19 It not only addresses a local tendon problem but also restores the normal functional anatomy of the foot by drastically improving local and remote biomechanics.5
The arthroscopically assisted section of the retrotalar pulley and the subsequent re-establishment of the tendon glide restore the subtalar mobility and allow the kinetic chain of the lower extremity to regain its natural dynamic balance, as we observed in our series. Our technique has been validated by using a gait-analysis assessment preoperatively, as well as postoperatively. Our results have clearly illustrated substantial favorable changes concerning foot dynamics in gait, thus highlighting the efficacy and consistency of our technique.4 We have also shown that this technique results not only in restoration of the normal tendon glide but also in restoration of the normal mobility of the subtalar joint.3,8 In today's world with an ongoing demand for better surgical results, especially in patients who practice sports activities, this technique constitutes a safe and efficacious treatment option that ensures high patient satisfaction.
Acknowledgment
The authors acknowledge Lucien Delapraz, Human Resources business partner, Centre Orthopédique d’Ouchy, Lausanne.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic technique. The medial side of the right foot is exposed with the patient in prone position. We can see the clinical signs of functional hallux limitus: plantar hyperkeratosis on the great toe and on the fifth metatarsal head, being a result of the absence of support on the first metatarsal head, as well as walking on the outer edge of the foot. The pen drawing shows the pathway of the flexor hallucis longus and its conflict at the retrotalar pulley. A classic 2-portal endoscopic approach is used to visualize the subtalar joint: posterolateral portal for the camera and posteromedial portal for the instruments. The first step is the creation of the posterolateral portal at the level of the tip of the lateral malleolus, just lateral to the Achilles tendon. Following the initial 0.5-cm skin incision, a mosquito clamp is used to split the subcutaneous tissue in a way that prevents injury to the adjacent sural nerve branches. The clamp should be directed toward the interdigital space between the first 2 toes. The bone surface is palpated with the tip of the clamp, which is subsequently removed and replaced by the arthroscope in the same direction. Next, the posteromedial portal is made at the mid distance between the medial malleolus and the Achilles tendon border. Following the skin incision, a mosquito clamp is introduced and directed toward the obturator and forward to the Achilles tendon. When the mosquito clamp touches the shaft of the arthroscope, it has to be opened to create a space at the posterior aspect of the talus that is needed for the outflow. It is important to stay behind the vessels and nerves. The posterolateral tubercle of the talus and the subtalar joint are visualized by dissecting the fatty tissue and the talocalcaneal ligament. It is not mandatory to expose the ankle joint. Then, the dissection starts from a central position and moves to an upward, medial, and anterior direction against the medial talar wall, until the first fibers of the pulley are identified by their pearly color. When the pulley is moved forward, the flexor hallucis longus tendon can be seen and its inability to glide properly can be assessed. Resection of the pulley is achieved by use of the ArthroCare device with a direction from anterior to posterior and from upward to downward. Special caution is taken not to stimulate the posterior tibial nerve with an adequate orientation of the ArthroCare device. Once the pulley is resected, restoration of the normal tendon glide is assessed clinically while dorsiflexing the great toe in ankle dorsiflexion. Surgically, the result of the release can be assessed by pulling the tendon backward with the probe. This maneuver allows visualization of the tunnel in front of the tendon and the space created by the release. Synovial remnants situated at the lower part of the retrotalar tunnel are excised if deemed necessary. In case of a posterior bony overgrowth adding to the conflict by limitation of the tendon glide or the presence of an os trigonum, resection might follow to a degree according to the preoperative clinical and imaging assessment. The subtalar joint is examined for normal and unrestricted motion by passive mobilization.
References
- 1.Durrant B., Chockalingam N. Functional hallux limitus: A review. J Am Podiatr Med Assoc. 2009;99:236–243. doi: 10.7547/0980236. [DOI] [PubMed] [Google Scholar]
- 2.Tzioupis C., Oliveto A., Grabherr S., Vallotton J., Riederer B. Identification of the retrotalar pulley of the flexor hallucis longus tendon. J Anat. 2019;235:757–764. doi: 10.1111/joa.13046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vallotton J., Echeverri S., Dobbelaere-Nicolas V. Functional hallux limitus or rigidus caused by a tenodesis effect at the retrotalar pulley: Description of the functional stretch test and the simple hoover cord maneuver that releases this tenodesis. J Am Podiatr Med Assoc. 2010;100:220–229. doi: 10.7547/1000220. [DOI] [PubMed] [Google Scholar]
- 4.Tzioupis CC, Diehl S, Boulos K, Aminian K, Rouhani H, Vallotton J. multi-segment model study to evaluate the sagittal plane blockade in patients with functional hallux limitus (FHL): Results after endoscopic tenolysis of the flexor hallucis longus at the retrotallar pulley. Presented at the 14th Congress of the European Federation of National Associations of Orthopaedics and Traumatology, Istanbul, Turkey, June 5-8, 2013.
- 5.Dananberg H.J. Sagittal plane biomechanics. American Diabetes Association. J Am Podiatr Med Assoc. 2000;90:47–50. doi: 10.7547/87507315-90-1-47. [DOI] [PubMed] [Google Scholar]
- 6.Dananberg H.J. Gait style as an etiology to chronic postural pain. Part I. Functional hallux limitus. J Am Podiatr Med Assoc. 1993;83:433–441. doi: 10.7547/87507315-83-8-433. [DOI] [PubMed] [Google Scholar]
- 7.Dananberg H.J. Gait style as an etiology to chronic postural pain. Part II. Postural compensatory process. J Am Podiatr Med Assoc. 1993;83:615–624. doi: 10.7547/87507315-83-11-615. [DOI] [PubMed] [Google Scholar]
- 8.Vallotton J. [Functional hallux limitus (FHL): A new explanation for overuse pathologies] Rev Med Suisse. 2014;10:2333–2337. [in French] [PubMed] [Google Scholar]
- 9.van Dijk C.N., Scholten P.E., Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. doi: 10.1053/jars.2000.19430. [DOI] [PubMed] [Google Scholar]
- 10.Scheibling B., Koch G., Clavert P. Cadaver study of anatomic landmark identification for placing ankle arthroscopy portals. Orthop Traumatol Surg Res. 2017;103:387–391. doi: 10.1016/j.otsr.2016.09.026. [DOI] [PubMed] [Google Scholar]
- 11.Deng D.F., Hamilton G.A., Lee M. Complications associated with foot and ankle arthroscopy. J Foot Ankle Surg. 2012;51:281–284. doi: 10.1053/j.jfas.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Miyamoto W., Takao M., Matsushita T. Hindfoot endoscopy for posterior ankle impingement syndrome and flexor hallucis longus tendon disorders. Foot Ankle Clin. 2015;20:139–147. doi: 10.1016/j.fcl.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Galla M., Lobenhoffer P. Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg. 2011;17:79–84. doi: 10.1016/j.fas.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Pereira H., Vuurberg G., Stone J., Lui T.H. Ankle tendoscopy: State of the art. J ISAKOS. 2017;2:332–338. [Google Scholar]
- 15.Monteagudo M., Maceira E., Martinez de Albornoz P. Foot and ankle tendoscopies: Current concepts review. EFORT Open Rev. 2017;1:440–447. doi: 10.1302/2058-5241.160028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kennedy J.G., van Dijk P.A., Murawski C.D. Functional outcomes after peroneal tendoscopy in the treatment of peroneal tendon disorders. Knee Surg Sports Traumatol Arthrosc. 2016;24:1148–1154. doi: 10.1007/s00167-016-4012-6. [DOI] [PubMed] [Google Scholar]
- 17.Vega J., Redo D., Savin G., Malagelada F., Dalmau-Pastor M. Anatomical variations of flexor hallucis longus tendon increase safety in hindfoot endoscopy. Knee Surg Sports Traumatol Arthrosc. 2017;25:1929–1935. doi: 10.1007/s00167-017-4465-2. [DOI] [PubMed] [Google Scholar]
- 18.Spennacchio P., Cucchi D., Randelli P.S., van Dijk N.C. Evidence-based indications for hindfoot endoscopy. Knee Surg Sports Traumatol Arthrosc. 2016;24:1386–1395. doi: 10.1007/s00167-015-3965-1. [DOI] [PubMed] [Google Scholar]
- 19.Rungprai C., Tennant J.N., Phisitkul P. Disorders of the flexor hallucis longus and os trigonum. Clin Sports Med. 2015;34:741–759. doi: 10.1016/j.csm.2015.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic technique. The medial side of the right foot is exposed with the patient in prone position. We can see the clinical signs of functional hallux limitus: plantar hyperkeratosis on the great toe and on the fifth metatarsal head, being a result of the absence of support on the first metatarsal head, as well as walking on the outer edge of the foot. The pen drawing shows the pathway of the flexor hallucis longus and its conflict at the retrotalar pulley. A classic 2-portal endoscopic approach is used to visualize the subtalar joint: posterolateral portal for the camera and posteromedial portal for the instruments. The first step is the creation of the posterolateral portal at the level of the tip of the lateral malleolus, just lateral to the Achilles tendon. Following the initial 0.5-cm skin incision, a mosquito clamp is used to split the subcutaneous tissue in a way that prevents injury to the adjacent sural nerve branches. The clamp should be directed toward the interdigital space between the first 2 toes. The bone surface is palpated with the tip of the clamp, which is subsequently removed and replaced by the arthroscope in the same direction. Next, the posteromedial portal is made at the mid distance between the medial malleolus and the Achilles tendon border. Following the skin incision, a mosquito clamp is introduced and directed toward the obturator and forward to the Achilles tendon. When the mosquito clamp touches the shaft of the arthroscope, it has to be opened to create a space at the posterior aspect of the talus that is needed for the outflow. It is important to stay behind the vessels and nerves. The posterolateral tubercle of the talus and the subtalar joint are visualized by dissecting the fatty tissue and the talocalcaneal ligament. It is not mandatory to expose the ankle joint. Then, the dissection starts from a central position and moves to an upward, medial, and anterior direction against the medial talar wall, until the first fibers of the pulley are identified by their pearly color. When the pulley is moved forward, the flexor hallucis longus tendon can be seen and its inability to glide properly can be assessed. Resection of the pulley is achieved by use of the ArthroCare device with a direction from anterior to posterior and from upward to downward. Special caution is taken not to stimulate the posterior tibial nerve with an adequate orientation of the ArthroCare device. Once the pulley is resected, restoration of the normal tendon glide is assessed clinically while dorsiflexing the great toe in ankle dorsiflexion. Surgically, the result of the release can be assessed by pulling the tendon backward with the probe. This maneuver allows visualization of the tunnel in front of the tendon and the space created by the release. Synovial remnants situated at the lower part of the retrotalar tunnel are excised if deemed necessary. In case of a posterior bony overgrowth adding to the conflict by limitation of the tendon glide or the presence of an os trigonum, resection might follow to a degree according to the preoperative clinical and imaging assessment. The subtalar joint is examined for normal and unrestricted motion by passive mobilization.