ABSTRACT
Background
Eating disorders affect 13% of females and contribute to functional impairment and mortality, but few studies have identified risk factors that prospectively correlate with future onset of anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), and purging disorder (PD). Identifying risk factors specific to each eating disorder is critical for advancing etiologic knowledge and designing effective prevention programs.
Objectives
This study examined whether weight suppression (the difference between a person's highest past weight at their adult height and their current weight) correlates with future onset of AN, BN, BED, and PD.
Methods
Data from 1165 young women with body image concerns (mean ± SD age: 21.9 ± 6.4 y) who completed annual diagnostic interviews over a 3-y follow-up period were examined. Logistic regression models evaluated the relation of baseline weight suppression to onset risk of each eating disorder controlling for age, dietary restraint, and intervention condition.
Results
Elevated weight suppression predicted future onset of AN (OR: 1.36; 95% CI: 1.03, 1.80), BN (OR: 1.34; 95% CI: 1.11, 1.62), PD (OR: 1.46; 95% CI: 1.23, 1.74), and any eating disorder (OR: 1.32; 95% CI: 1.12, 1.56), but not BED (OR: 1.10; 95% CI: 0.89, 1.37). Highest past weight correlated with future onset of BN and PD but not onset of AN, BED, or any eating disorder, and baseline current weight was inversely related to future AN onset only, implying that women with the largest difference between their highest past weight and current weight are at greatest risk of eating disorders.
Conclusions
The results provide novel evidence that weight suppression correlates with future onset of eating disorders characterized by dietary restriction or compensatory weight control behaviors and suggest weight-suppressed women constitute an important risk group to target with selective prevention programs.
These trials were registered at clinicaltrials.gov as NCT01126918 and NCT01949649.
Keywords: risk factors, prospective, weight suppression, anorexia nervosa, bulimia nervosa, binge eating disorder, purging disorder, young women
See corresponding editorial on page 907.
Introduction
Eating disorders affect 13% of females and are characterized by chronicity, distress, impairment, and mortality. It is critical to identify risk factors that predict future onset of each type of eating disorder, because this should advance etiologic knowledge, guide the development of effective prevention programs, and elucidate high-risk subgroups to target with selective prevention programs. One novel potential risk factor is weight suppression, which reflects the difference between highest past weight at adult height and current weight (1). Weight suppression predicted presence of questionnaire-assessed bulimic syndromes at 10-y follow-up (2), but has not yet been shown to predict diagnostic interview–assessed eating disorders, the gold-standard method for assessing eating disorders. Weight suppression theoretically increases the reward value of food, based on evidence that a longer time since last caloric intake correlated with greater reward region (putamen, orbitofrontal cortex) response to high-calorie food images, expected tastes of high-calorie foods, and tastes of high-calorie foods (3) and experimentally manipulated acute caloric deprivation increased reward region (amygdala) response to high-calorie food images (4). However, longer-term weight loss induced by exercise, dietary, and gastric bypass surgery interventions reduced reward region (striatal, putamen, insula) responsivity to high-calorie food images (5–7).
No study to our knowledge has examined whether weight suppression predicts future onset of interview-assessed AN, BN, BED, or PD. Identifying risk factors specific to each type of eating disorder is critical for advancing etiologic knowledge for this class of psychiatric conditions and designing effective prevention programs. Reported dieting has predicted future onset of any eating disorder (8, 9), BN (10, 11), BED (11), and PD (11, 12). It is possible that weight suppression will predict future eating disorder onset because it identifies individuals who have entered a prolonged period of negative energy balance necessary for sustained weight loss. We controlled for reported dieting in the models to determine if weight suppression has unique predictive effects. We also examined whether highest past weight and current weight predicted future onset of eating disorders to determine whether 1 of the 2 constituent variables used to calculate weight suppression had a stronger prospective relation than weight suppression. One reason few studies have examined risk factors that predict future onset of specific eating disorders is that the incidence is low, making it difficult to collect a sample large enough to provide sufficient power. One solution is to use a high-risk design wherein participants at elevated risk of the disorders of interest are followed longitudinally. Thus, we combined data from 2 large selective eating disorder prevention trials that involved adolescent girls and young women at risk of eating disorders due to body image concerns and which used parallel recruitment and assessment procedures to increase sensitivity.
Methods
Participants and procedures
We combined data from 2 eating disorder prevention effectiveness trials (13, 14) (NCT01126918 and NCT01949649; see Supplemental Figures 1 and 2 for participant flow charts for those studies), resulting in a sample of 1165 young women (mean ± SD age: 21.9 ± 6.44 y). Sixty-four percent of the combined sample were European American, 12% Asian, 5% African American, 5% Hispanic, 2% American Indian, and 1% Pacific Islander, and 11% were biracial per self-report. Because individuals with threshold compared with subthreshold eating disorders showed similar functional impairment, emotional distress, and treatment care (15) and subthreshold eating disorders fall under the Other Specified Feeding and Eating Disorders category in Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 (16), we predicted onset of threshold or subthreshold variants of each eating disorder in the same model. Supplemental Table 1 provides the operationalization of threshold and subthreshold levels of AN, BN, BED, and PD.
Design of randomized prevention trials
Mailings and fliers recruited female students for trials evaluating body acceptance interventions at colleges. There was only 1 inclusion criterion: answering affirmatively when asked about the presence of body image concerns during a phone screen. We sought to exclude participants who met criteria for DSM-IV (17) AN or BN. Informed consent was obtained from participants. Participants in Trial 1 were randomly assigned to clinician-led Body Project groups or an educational brochure control condition. Participants in Trial 2 were randomly assigned to clinical-led Body Project groups, peer-led Body Project groups, the Internet-delivered eBody Project, or an eating disorder education video control condition. Participants in both trials completed surveys and interviews at baseline and at 1-, 6-, 12-, 24-, and 36-mo follow-ups. Interviews were conducted in person, but were done over the phone if the participants moved away during follow-up (<10% of the participants). The Oregon Research Institute Institutional Review Board granted ethical approval for both trials.
Measures
Weight suppression
At baseline, participants were weighed and reported their past highest weight at adult height. Following convention, weight suppression was calculated as the difference between participants’ previous highest self-reported weight at their adult height and their measured weight at baseline in kilograms (1). Weight recalled after a 15-y period correlates with measured weight from that time (r = 0.87) (18).
BMI
BMI (in kg/m2) was used to reflect height-adjusted body weight. Height was measured to the nearest 1 mm using portable stadiometers. Weight was assessed to the nearest 0.1 kg using digital scales with participants wearing light indoor clothing without shoes or coats. Age- and sex-adjusted BMI centiles were used to determine whether participants met criteria for AN. BMI has shown convergent validity (r = 0.80–0.90) with direct measures of body fat (19) and predictive validity for future onset of AN (11).
Dietary restraint
The Dutch Restrained Eating Scale (20) assesses the frequency of dieting behaviors. It has shown internal consistency (α = 0.95); 2-wk test–retest reliability (r = 0.82); convergent validity with self-reported (but not objectively measured) caloric intake; predictive validity for future BN, BED, and PD onset; and sensitivity to intervention effects (11, 20–22).
Thin-ideal internalization
The Ideal-Body Stereotype Scale—Revised assessed thin-ideal internalization (14). It has shown internal consistency (α = 0.91), 2-wk test–retest reliability (r = 0.80), predictive validity for bulimic symptom onset, and sensitivity to intervention effects (14).
Body dissatisfaction
The Body Dissatisfaction Scale (14) assessed dissatisfaction with 9 body parts. It has shown internal consistency (α = 0.94), 3-wk test–retest reliability (r = 0.90), predictive validity for eating disorder onset, and sensitivity to intervention effects (14).
Negative affect
Different measures of negative affect were used in each trial and were standardized to permit analyses of the combined data set. In Trial 1 negative affect was assessed with the 21-item Beck Depression Inventory (23), which has shown internal consistency (α = 0.73–0.95), 1-wk test–retest reliability (r = 0.93), convergent validity with clinician ratings of depressive symptoms (mean r = 0.75), and sensitivity to intervention effects (13, 23). In Trial 2 negative affect was assessed with the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale—Revised (24), which has shown internal consistency (α = 0.95), 3-wk test–retest reliability (r = 0.78), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (14).
Eating pathology
The semistructured Eating Disorder Diagnostic Interview (EDDI) (11) assessed eating disorder symptoms over the past 3 mo at baseline and since the previous interview at follow-up assessments on a month-by-month basis over a 3-y follow-up period. DSM-5 (16) criteria for eating disorders, as operationalized in (11), were used (see Supplemental Table 1). EDDI eating disorder diagnoses have shown 1-wk test–retest reliability (κ = 0.79) and interrater agreement (κ = 0.71) for the eating disorder diagnostic criteria used in the present study based on randomly selected subsets of the data examined herein, as well as sensitivity to eating disorder prevention programs (e.g., 14).
Statistical methods
Data were missing from 5%, 10%, 7%, 10%, and 17% of participants at the 1-, 6-, 12-, 24-, and 36-mo follow-ups, respectively. Attrition at all follow-ups was significantly associated with only higher baseline dietary restraint (Cohen's d ranged from 0.17 to 0.43). We used multiple imputation to impute plausible values for the study variables using predictive mean matching (25). In our missing data model we included only the variables in our statistical models, but no other auxiliary variables because no other variables correlated at r > 0.40 with either weight suppression or BMI (26). We created 50 imputed data sets using the mice package (version 3.6.0) (27) in R version 3.6.1 (R Core Team) (28). We included intervention condition as a control variable in all analyses to reduce the possibility that condition affected our estimate of the relation between weight suppression and future onset of eating disorders.
For each of the 5 eating disorder outcomes considered, we excluded participants who had an eating disorder at baseline or whose eating disorder status at baseline was unknown. This resulted in 4 (1 threshold and 3 subthreshold), 75 (37 threshold and 38 subthreshold), 47 (28 threshold and 19 subthreshold), 21 (16 threshold and 5 subthreshold), and 146 (82 threshold and 64 subthreshold) participants being excluded from the AN, BN, BED, PD, and any eating disorder models, respectively, because they had that eating disorder at baseline. For AN, 8 (0.69%) participants had unknown baseline status, whereas for BN, BED, and PD only 1 (0.09%) participant for each eating disorder had an unknown baseline status. We excluded participants who met the criteria for the eating disorders examined in each model at baseline to ensure that elevated weight suppression occurred before onset of the eating disorders, as recommended by methodologists (29). We did not impute eating disorder diagnoses at baseline because it could have generated unequal sample sizes across the imputed data sets owing to the fact that we excluded participants with the disorder at baseline for which we were predicting onset; the procedure used for pooling parameter estimates from the imputed samples requires that the imputed samples are the same size. We had sample sizes of 1118, 1065, 1090, 1114, and 989 participants for the AN, BN, BED, PD, and any eating disorder models, respectively. For each of the outcomes separately, we fit a logistic regression model with weight suppression (standardized) as the predictor to each of the 50 imputed data sets and pooled the parameter estimates across the models using Rubin's rules (30). We also investigated whether highest past weight and current weight at baseline (both standardized) predicted future onset of eating disorders with logistic regression models, in an effort to determine whether 1 of the 2 constituent variables used to calculate weight suppression had a stronger prospective relation than weight suppression. All models controlled for age and dietary restraint, which were included as continuous covariates, and intervention condition, which was modeled with a series of dummy coded vectors (e.g., Body Project prevention program = 1, all other conditions = 0).
Results
Descriptive analyses
Table 1 shows a breakdown of the study participants’ age, ethnicity, and level of education by BMI status categories at baseline. The majority of participants (n = 704) were considered to have healthy weight (BMI < 25), followed by overweight (n = 289, BMI between 25 and 30) and obese (n = 164, BMI > 30) participants. The participants with normal body weight were on average younger than the overweight and obese participants. The 3 groups were similar ethnically, with the exception that participants with a normal body weight were more likely to identify as Asian than were overweight participants (2 times) and obese participants (4 times). Conversely, obese participants were more likely to identify as black/African American than were overweight participants (nearly 2 times) and normal-weight participants (nearly 3 times). Normal body weight participants were more educated than overweight and obese participants because the former had a higher percentage of college graduates and women with advanced degrees.
TABLE 1.
Characteristics of study participants at baseline1
| Healthy weight (n = 704) | Overweight (n = 289) | Obese (n = 164) | |
|---|---|---|---|
| Age, y | 21.0 ± 4.7 | 22.1 ± 6.9 | 25.3 ± 10.0 |
| Ethnicity | |||
| White | 63.7 | 65.9 | 61.6 |
| Black/African American | 3.3 | 5.6 | 8.5 |
| Asian | 16.2 | 8.7 | 3.7 |
| Hispanic | 4.0 | 6.6 | 7.9 |
| American Indian/Alaskan Native | 1.1 | 1.7 | 3.7 |
| Native Hawaiian/Pacific Islander | 0.4 | 0.7 | 1.2 |
| Biracial | 11.1 | 10.5 | 13.4 |
| Other | 0.1 | 0.3 | 0.0 |
| Education | |||
| Grade school graduate | 2.1 | 1.4 | 4.3 |
| Some high school | 1.4 | 2.1 | 1.2 |
| High school graduate | 6.4 | 9.2 | 13.6 |
| Some college | 12.2 | 17.7 | 28.4 |
| College graduate | 37.8 | 30.4 | 33.3 |
| Advanced degree | 40.0 | 39.2 | 19.1 |
1Values are mean ± SD or n (%). Healthy weight, overweight, and obese correspond to BMI (in kg/m2) <24.9, 25–29.9, and >30, respectively.
Participants’ self-reported previous highest weight ranged from 40.8 to 182.8 kg (mean ± SD: 72.9 ± 17.6 kg), whereas their current weight ranged from 38.9 to 153.9 kg (mean ± SD: 68.1 ± 15.9 kg). Participants’ self-reported previous highest weight was strongly correlated with their current weight (r = 0.93), suggesting very similar rank ordering on these variables. Weight suppression in the sample ranged from 0 to 70.7 kg (mean ± SD: 4.8 ± 6.5 kg), with 186 participants (16.1%) currently at their highest weights. Weight suppression was uncorrelated with baseline BMI (r = 0.05) and dietary restraint (r = 0.05), providing evidence that weight suppression is a distinct construct. Weight suppression did not correlate significantly with thin-ideal internalization (r = −0.08), body dissatisfaction (r = 0.06), or negative affect (r = 0.08).
Over a 3-y follow-up period, 18 participants showed future onset of AN, 79 showed onset of BN, 75 showed onset of BED, 60 showed onset of PD, and 133 showed onset of any of these eating disorders. Preliminary analyses confirmed that, as observed previously (15), participants with threshold eating disorders did not differ significantly from participants with subthreshold eating disorders in terms of negative affect, psychosocial functioning, and mental health treatment (P > 0.10). Weight suppression at baseline was 8.3 kg for participants who showed onset of AN, 7.1 kg for participants who showed onset of BN, 5.6 kg for participants who showed onset of BED, 8.7 kg for participants who showed onset of PD, and 6.5 kg for participants who showed onset of any eating disorder, compared with 4.4 kg for participants who did not show onset of any eating disorder. These data suggest that most participants were in a state of moderate weight suppression.
Relation of weight suppression to incidence of eating disorder onset over 3-y follow-up
Table 2 presents parameter estimates from the logistic regression models, including ORs and 95% CIs. Because we standardized weight suppression and the other predictors before modeling, the OR can be interpreted such that, in the case of AN, for a 1-SD increase in weight suppression, the odds of developing AN increased by a factor of 1.36 (OR: 1.36) while holding age, dietary restraint, and condition constant. The other ORs can be interpreted similarly. Weight suppression was significantly associated with the odds for future onset of AN, BN, PD, and any eating disorder. The ORs ranged from 1.32 for any eating disorder to 1.46 for PD. However, weight suppression was not associated with the odds of future onset of BED. We also confirmed that all of the significant effects remained significant and the nonsignificant effects remained nonsignificant when we controlled for baseline BMI. And although we report weight suppression as the difference between highest past weight and current weight, relative weight suppression (31), defined as this difference divided by highest past weight, also yielded similar associations (the 2 variables were correlated: r = 0.94).
TABLE 2.
Parameter estimates from the logistic regression models testing the relation of weight suppression and dietary restraint to future onset of eating disorders over a 3-y follow-up period1
| Eating disorder | OR (95% CI) | P value |
|---|---|---|
| Anorexia nervosa | 1.36 (1.03, 1.80) | 0.031 |
| Bulimia nervosa | 1.34 (1.11, 1.62) | 0.002 |
| Binge eating disorder | 1.10 (0.89, 1.37) | 0.371 |
| Purging disorder | 1.46 (1.23, 1.74) | <0.001 |
| Any eating disorder | 1.32 (1.12, 1.56) | 0.001 |
1All models included an intercept term and controlled for age (continuous variable), intervention (categorical variable), and dietary restraint (continuous variable). ORs (95% CIs) and P values correspond to the ORs and associated 95% CIs and the P values from the pooled results.
Investigating the components of weight suppression
We also investigated the 2 constituent elements of weight suppression. Specifically, we explored the associations of both highest past weight and current weight with eating disorder outcomes, in separate models because of the high correlation between these variables (r = 0.93), which would lead to unstable parameter estimates due to multicollinearity. Highest past weight was significantly associated with future onset of BN (OR: 1.28, t = 2.21, df = 1042.86, P = 0.027) and PD (OR: 1.29, t = 2.11, df = 1102.88, P = 0.035), controlling for age, dietary restraint, and condition, but not with AN, BED, or any eating disorder. Current weight was inversely related to future onset of AN (OR: 0.26, t = −2.98, df = 1107.89, P = 0.003), but was not associated with future onset of BN, BED, PD, or any eating disorder controlling for age, dietary restraint, and condition.
Discussion
Weight suppression was common in this sample of young women with body image concerns. On average, participants were 4.8 kg below their highest past weight and 84% reported weight suppression. The mean weight suppression (4.8 kg) was higher than observed in community samples (2.7 kg) (32), but lower than observed in outpatient (9.6 kg) (1) and residential treatment (12.0 kg) (33) clinical samples. Weight suppression did not correlate with dietary restraint, BMI, thin-ideal internalization, body dissatisfaction, or negative affect, suggesting that it captures a distinct construct that does not overlap with established eating disorder risk factors (8–12, 34).
We examined whether weight suppression correlated with future onset of specific eating disorders or any eating disorder, which has not to our knowledge been examined previously. Weight suppression correlated with future onset of AN, BN, PD, and any eating disorder, but not BED. Thus, weight suppression was correlated with eating disorders characterized by dietary restriction and compensatory weight control behaviors, but not BED, which is characterized by only binge eating. Results suggest that weight suppression increases the odds for behaviors designed to produce weight loss. The prospective effects were moderate in magnitude. Participants who showed future onset of each eating disorder or any eating disorder exhibited about twice the amount of weight suppression (7.9 kg) as participants who did not show disorder onset (4.6 kg).
The prospective effects for weight suppression on future eating disorders occurred controlling for dietary restraint, providing further evidence that weight suppression captures a distinct risk process. Dietary restraint correlated with future onset of BN, BED, PD, and any eating disorder, but not AN, which converges with findings from an independent sample (8, 12), a partially independent sample that contained 32% of participants in the present report (11), and studies conducted by independent teams (9, 10, 34). The evidence that dietary restraint did not correlate with future onset of AN converges with findings from an independent sample (35) and the partially independent sample that contained 32% of the participants in the present sample (11). Dietary restraint showed stronger relations to future eating disorder onset than did weight suppression.
It was surprising that dietary restraint and weight suppression were uncorrelated, but that both increased risk of future eating disorder onset. Studies have consistently revealed that individuals with high compared with low dietary restraint scores do not consume fewer calories per objective measures of caloric intake, such as doubly labeled water estimates of caloric intake and unobtrusively observed caloric intake (e.g., 21, 36–38). Indeed, individuals with high compared with low dietary restraint scores have not been shown to lose weight over time. Thus, there is no evidence that individuals with dietary restraint scores enter into the negative energy balance necessary for weight loss (39). In contrast, individuals high in weight suppression apparently do enter into a prolonged period of negative energy balance, which is necessary for their current weight to be less than their past highest weight (39). It will be critical to determine what it is about individuals with high dietary restraint scores that increases risk of future eating disorder onset, given that it does not appear to be a negative energy balance.
We examined whether current weight and highest past weight correlated with future onset of specific eating disorders or any eating disorder to determine if the prospective relations were driven by the 2 constituent variables used to calculate weight suppression. Highest past weight correlated with future onset of BN and PD, but not AN, BED, or any eating disorder. These results converge with evidence that overeating, which is presumably a key driver of the highest past weight, correlates with future onset of BN, BED, and PD (11). Lower baseline weight correlated with future onset of AN, but not future onset of BN, BED, PD, or any eating disorder. This single prospective relation converges with evidence that a low BMI correlated with future onset of AN, but not the other eating disorders (11, 35), and is consistent with evidence that lifetime AN correlated with a low birth weight (40), a low BMI at age 6 y (41), a low BMI at age 5–10 y (42), and undereating at age 10 y (43). Collectively, results suggest that a negative energy balance that produces a low BMI at baseline and a history of a positive energy balance show weaker relations to future onset of these eating disorders than does weight suppression. This pattern of findings implies that it is the process of losing a significant amount of weight after gaining excess body weight that increases the risk of subsequent eating disorder onset. These findings make a novel contribution to the literature because this is, as far as we know, the first study to test whether the 2 variables used to calculate weight suppression correlate with future onset of various eating disorders.
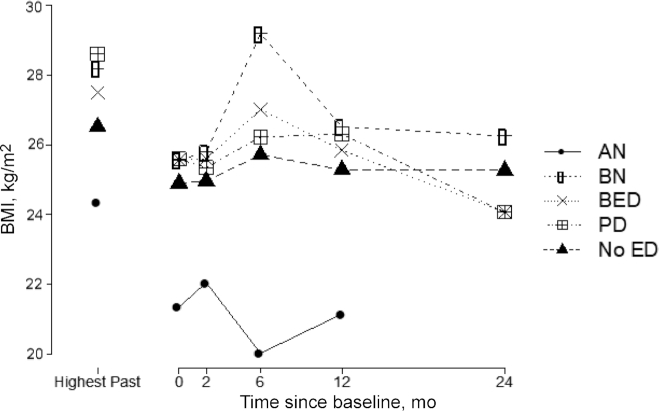
Results suggest that youth who subsequently develop AN typically exhibit weight suppression, yet data from clinical samples suggest that individuals who later develop AN report a history of overweight (31). To better understand the weight history of participants who developed AN in this community-recruited sample, we therefore graphed the average BMI for participants who showed onset of AN, BN, BED, and PD, focusing only on assessments before they showed onset of these eating disorders, and for those who did not develop an eating disorder (Figure 1); participants who later showed AN onset had lower BMI values and a lower past highest BMI than those who remained free of an eating disorder or who developed 1 of the other types of eating disorders.
FIGURE 1.
Highest past BMI and BMI trajectories for participants who subsequently showed onset of threshold or subthreshold levels of each ED compared with participants who did not develop an ED. Month 24 was not included for AN because only 1 participant had not developed AN at that time. AN, anorexia nervosa; BED, binge eating disorder; BN, bulimia nervosa; ED, eating disorder; PD, purging disorder.
Study limitations should be considered. First, all participants were required to report body image concerns, which might constrain generalizability. However, the risk factors identified in high-risk samples (11, 44) are similar to those identified in unselected samples (8–10, 12, 34), suggesting that findings should generalize. In addition, the recruitment methodology resulted in a sample with greater mean weight suppression and increased variance, which would have theoretically increased sensitivity. Second, we relied on self-reported highest past weight, rather than on directly measured historical weight because objectively capturing highest lifetime weight was unfeasible. Fortunately, data suggest that retrospectively reported weight correlates (r = 0.87) with previously measured weight (18). Third, the sample consisted solely of women and results may not apply to the less frequent onset of eating disorders in men. Fourth, as with all prospective analyses, it is always possible that some third variable, whether measured or unmeasured, could explain the observed relations between weight suppression and future onset of eating disorders.
The findings have several clinical implications. First, it might be useful to consider weight-suppressed individuals as a high-risk population worth targeting with selective eating disorder prevention programs. Second, results imply that individuals should be informed that losing excess weight may increase the risk of onset of eating disorders. Third, preventing initial excess weight gain should reduce the risk of future weight suppression and consequent risk of eating disorders. This implication is consistent with the evidence that a prevention program promoting a balance between energy intake and expenditure, which reduced excess weight gain and onset of overweight and obesity, also reduced future onset of eating disorders (13, 22). The fact that most people who gain excess body weight are unable to lose the excess body weight on a lasting basis likewise suggests that prevention of initial excess body weight gain is prudent.
The present results also suggest directions for future research. First, replicating the relation between weight suppression and future onset of eating disorders in independent samples is needed. Second, research should investigate whether most people achieve weight suppression by intentionally entering a negative energy balance necessary for weight loss and evaluate whether the predictive effects of weight suppression differ if weight loss is intentional as opposed to unintentional. Third, future studies should investigate whether the risk of eating disorder onset conveyed by weight suppression fades after a particular duration of time at the suppressed weight. Finally, it would be useful to investigate biological factors that may mediate the relation between weight suppression and future onset of eating disorders, such as elevated reward region responsivity to food cues, elevated signaling of hunger hormones, or lower signaling of satiety hormones.
In conclusion, elevated weight suppression was associated with higher odds of future onset of AN, BN, PD, and any eating disorder over a 3-y follow-up period, but did not significantly increase the odds for future onset of BED, suggesting that weight suppression increases the risk of eating disorders characterized by unhealthy weight control behaviors, but not solely binge eating. These relations were independent of dietary restraint and other risk factors that have correlated significantly with future onset of eating disorders.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—ES: led the design and writing of the paper; PR and HS: contributed to the design of the study and writing portions of the text; CD: conducted all analyses and wrote portions of the text; and all authors: read and approved the final manuscript. The authors report no conflicts of interest.
Notes
Supported by National Institute of Mental Health grants MH086582 and MH097720 (to ES).
Supplemental Table 1 and Supplemental Figures 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Data described in the article, code book, and analytic code will be made available upon request to the corresponding author. We did not preregister these analyses because they involved secondary data analyses.
Abbreviations used: AN, anorexia nervosa; BED, binge eating disorder; BN, bulimia nervosa; DSM, Diagnostic and Statistical Manual of Mental Disorders; EDDI, Eating Disorder Diagnostic Interview; PD, purging disorder.
Contributor Information
Eric Stice, Department of Psychiatry and Behavioral Sciences, Stanford University, Stanford, CA, USA.
Paul Rohde, Oregon Research Institute, Eugene, OR, USA.
Heather Shaw, Oregon Research Institute, Eugene, OR, USA.
Chris Desjardins, Saint Michael's College, Colchester, VT, USA.
References
- 1. Butryn ML, Lowe MR, Safer DL, Agras WS. Weight suppression is a robust predictor of outcome in the cognitive-behavioral treatment of bulimia nervosa. J Abnorm Psychol. 2006;115(1):62–7. [DOI] [PubMed] [Google Scholar]
- 2. Keel PK, Heatherton TF. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. J Abnorm Psychol. 2010;119(2):268–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stice E, Burger K, Yokum S. Caloric deprivation increases responsivity of attention and reward brain regions to intake, anticipated intake, and images of palatable foods. Neuroimage. 2013;67:322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leidy HJ, Lepping RJ, Savage CR, Harris CT. Neural responses to visual food stimuli after a normal vs. higher protein breakfast in breakfast-skipping teens: a pilot fMRI study. Obesity (Silver Spring). 2011;19(10):2019–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cornier MA, Melanson EL, Salzberg AK, Bechtell JL, Tregellas JR. The effects of exercise on the neuronal response to food cues. Physiol Behav. 2012;105(4):1028–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deckersbach T, Das SK, Urban LE, Salinardi T, Batra P, Rodman AM, Arulpragasam AR, Dougherty DD, Roberts SB. Pilot randomized trial demonstrating reversal of obesity-related abnormalities in reward system responsivity to food cues with a behavioral intervention. Nutr Diabetes. 2014;4:e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ochner CN, Stice E, Hutchins E, Afifi L, Geliebter A, Hirsch J, Teixeira J. Relation between changes in neural responsivity and reductions in desire to eat high-calorie foods following gastric bypass surgery. Neuroscience. 2012;209:128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rohde P, Stice E, Marti CN. Development and predictive effects of eating disorder risk factors during adolescence: implications for prevention efforts. Int J Eat Disord. 2015;48(2):187–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Santonastaso P, Friederici S, Favaro A. Full and partial syndromes in eating disorders: a 1-year prospective study of risk factors among female students. Psychopathology. 1999;32(1):50–6. [DOI] [PubMed] [Google Scholar]
- 10. Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ. 1999;318(7186):765–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol. 2017;126(1):38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav Res Ther. 2011;49(10):622–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stice E, Rohde P, Butryn ML, Shaw H, Marti CN. Effectiveness trial of a selective dissonance-based eating disorder prevention program with female college students: effects at 2- and 3-year follow-up. Behav Res Ther. 2015;71:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stice E, Rohde P, Shaw H, Gau JM. Clinician-led, peer-led, and internet-delivered dissonance-based eating disorder prevention programs: acute effectiveness of these delivery modalities. J Consult Clin Psychol. 2017;85(9):883–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2013;122(2):445–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 17. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed Text revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 18. Troy LM, Hunter DJ, Manson JE, Colditz GA, Stampfer MJ, Willett WC. The validity of recalled weight among younger women. Int J Obes Relat Metab Disord. 1995;19(8):570–2. [PubMed] [Google Scholar]
- 19. Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatr. 1998;132(2):204–10. [DOI] [PubMed] [Google Scholar]
- 20. van Strien T, Frijters JER, van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. Int J Eat Disord. 1986;5(4):747–55. [Google Scholar]
- 21. Stice E, Cooper JA, Schoeller DA, Tappe K, Lowe MR. Are dietary restraint scales valid measures of moderate- to long-term dietary restriction? Objective biological and behavioral data suggest not. Psychol Assess. 2007;19(4):449–58. [DOI] [PubMed] [Google Scholar]
- 22. Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. J Consult Clin Psychol. 2008;76(2):329–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100. [Google Scholar]
- 24. Watson D, Clark LA. Affects separable and inseparable: on the hierarchical arrangement of the negative affects. J Pers Soc Psychol. 1992;62(3):489–505. [Google Scholar]
- 25. van Buuren S. Flexible imputation of missing data. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2018. [Google Scholar]
- 26. Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–76. [DOI] [PubMed] [Google Scholar]
- 27. van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Soft. 2011;45:3. [Google Scholar]
- 28. R Core Team. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 29. Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–56. [DOI] [PubMed] [Google Scholar]
- 30. Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 2002. [Google Scholar]
- 31. Lowe MR, Piers AD, Benson L. Weight suppression in eating disorders: a research and conceptual update. Curr Psychiatry Rep. 2018;20(10):80. [DOI] [PubMed] [Google Scholar]
- 32. Lowe MR, Marti CN, Lesser EL, Stice E. Weight suppression uniquely predicts body fat gain in first-year female college students. Eat Behav. 2019;32:60–4. [DOI] [PubMed] [Google Scholar]
- 33. Lowe MR, Davis W, Lucks D, Annunziato R, Butryn M. Weight suppression predicts weight gain during inpatient treatment of bulimia nervosa. Physiol Behav. 2006;87(3):487–92. [DOI] [PubMed] [Google Scholar]
- 34. Dakanalis A, Clerici M, Bartoli F, Caslini M, Crocamo C, Riva G, Carra G. Risk and maintenance factors for young women's DSM-5 eating disorders. Arch Womens Ment Health. 2017;20(6):721–31. [DOI] [PubMed] [Google Scholar]
- 35. Stice E, Bohon C. Eating disorders. Hoboken, NJ: Wiley and Sons; 2013. [Google Scholar]
- 36. Martin CK, Williamson DA, Geiselman PJ, Walden H, Smeets M, Morales S, Redmann S Jr. Consistency of food intake over four eating sessions in the laboratory. Eat Behav. 2005;6(4):365–72. [DOI] [PubMed] [Google Scholar]
- 37. Rolls BJ, Castellanos VH, Shide DJ, Miller DL, Pelkman CL, Thorwart ML, Peters JC. Sensory properties of a nonabsorbable fat substitute did not affect regulation of energy intake. Am J Clin Nutr. 1997;65(5):1375–83. [DOI] [PubMed] [Google Scholar]
- 38. Stice E, Sysko R, Roberto CA, Allison S. Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite. 2010;54(2):331–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hill JO, Wyatt HR, Peters JC. Energy balance and obesity. Circulation. 2012;126(1):126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cnattingius S, Hultman CM, Dahl M, Sparen P. Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch Gen Psychiatry. 1999;56(7):634–8. [DOI] [PubMed] [Google Scholar]
- 41. Tyrka AR, Waldron I, Graber JA, Brooks-Gunn J. Prospective predictors of the onset of anorexic and bulimic syndromes. Int J Eat Disord. 2002;32(3):282–90. [DOI] [PubMed] [Google Scholar]
- 42. Yilmaz Z, Gottfredson NC, Zerwas SC, Bulik CM, Micali N. Developmental premorbid body mass index trajectories of adolescents with eating disorders in a longitudinal population cohort. J Am Acad Child Adolesc Psychiatry. 2019;58(2):191–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nicholls DE, Viner RM. Childhood risk factors for lifetime anorexia nervosa by age 30 years in a national birth cohort. J Am Acad Child Adolesc Psychiatry. 2009;48(8):791–9. [DOI] [PubMed] [Google Scholar]
- 44. Jacobi C, Fittig E, Bryson SW, Wilfley D, Kraemer HC, Taylor CB. Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychol Med. 2011;41(9):1939–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.